Abstract
Background:
Health counseling before marriage can be a most worthwhile and satisfying aspect of preventive medicine. It is important in genetic diagnosis and the prevention of hereditary, sexually transmitted and other infectious diseases.
Objectives:
To determine the acceptance of the concept of Premarital Health Counseling (PMHC), and to identify some factors, which may efect this acceptance among Saudis who attend Primary Health Care Center in Riyadh, Kingdom of Saudi Arabia (KSA), 1417H.
Methods:
The present study is a cross-sectional one with a selected sample of Saudis who attended the Primary Health Care Centers in Riyadh during the year 1417H. A multistage sampling and equal allocation stratified sampling within was used to select 484 persons comprising an equal number of males and females, married and single above the age of 18 years. A pre-designed pre-tested questionnaire sheet was used to collect the required data, which were then tabulated and statistically analyzed.
Results:
The study indicated that 364 (75.2%) of the study population accepted the concept of Premarital Health Counseling. PMHC was positively affected by the advancing age, experience of marriage, educational level and well-understood Islamic-health related issues. Out f those who accepted the concept, 273 (75%) agreed on the exchange of PMHC certificates between couples to be married and 152 (42%) agreed on the implementation of legislation on PMHC. Also, 298 (82%) of them wanted PMHC to be confidential and 168 (46%) agreed to the concept despite its cost. As regards the location of PMHC, most of participants who agreed to PMHC would prefer it to be given at governmental establishments.
Recommendations:
The study recommended the implementation of PMHC in Saudi Arabia, since it was accepted by the study population. However, further studies should be carried out to determine the details to be incorporated in the PMHC, their implementation and legislation on demographic basis of the Saudi community. Also, a community health education program for PMHC has to be devised in collaboration with Islamic leaders.
Keywords: Attitudes, Premartial Health Counseling, Premarital counseling, Saudi Arabia
INTRODUCTION
The operational definition used in this study for Premarital Health Counseling (PMHC) would involve a consultation during which history would be taken and medical examination as well as laboratory investigations done for persons planning to marry, in order to screen for inherited and communicable diseases.
Health counseling before marriage can be a worthwhile and a most satisfying aspect of preventive medicine.1 One important aspect of PMHC is genetic counseling.2 This reduces the number of offspring that may be affected by a disorder, by defining the need for treatment (e.g. phenylketonurea) or assisting the couple to decide whether or not to avoid pregnancy in presence of a high risk of abnormality.3
The issue of PMHC is of great importance in Saudi Arabia because of high prevalence (55%) of consanguineous marriages.4–6 Offspring of these marriages may have such diseases as hereditary hearig impairment, mental retardation, autosomal recessive osteopetrosis and blood disorders such as thalassaemia.7,8 Furthermore, the risk of bearing a child with a birth defect in these marriages is approximately 6-8% for each pregnancy, a figure which is double the reported incidence of serious birth defects or mental retardation in the population at large.9 Premarital exposure to some infectious diseases such as hepatitis B virus, and rubella during pregnancy which are easily prevented by premarital vaccination may result in physical or mental disorders in the newborn.10,11
The objective of the study was to determine the acceptance of the concept of PMHC and to identify some factors , which may influence the acceptance among Saudi who attended Primary Health Care Center in Riyadh city, KSA, 1417H.
METHODOLOGY
The present study is a cross-sectional one, conducted in 13 (20%) Primary Health Care Centers (PHCCs) located in Riyadh city selected by systematic random sampling. The study sample was a total of 484 persons consisting of an equal number of Saudi males and females, married and single above the age of 18 years. Multistage sampling, and equal allocation stratified sampling within, was used to estimate the size of the study sample, using the following equation, N=Z2,pq/D2 (N=the maximum sample size required, D=A 95% - CI is desired with d=0.05,12). To ensure a reliable study, the following formula is used: N=(Za/2/ CI)2 + 3 where Za/2=1.96, CI=95%, and width 0.1.
A pre-designed pre-tested questionnaire sheet was used to collect the required data. Cronbach's Coefficient Alpha, with standardized variable method, was used to measure the internal consistency and reliability of the questionnaire items.14 It was found to be 0.7.15 The author interviewed all participants, and the definition of PMHC was stated in Arabic to them. The questionnaire covered independent (age, sex, etc) and dependent variables (attitudes on medical, social, and religious ideas pertaining to PMHC).
Summated ratings (Likert's scale) was used to assist the study group attitudes toward PMHC. Five grades were used for the attitude scale, strongly agreed, agreed, neutral, diagreed, and strongly disagreed. Desirable attitudes were given scores of five and four.15 The median of scores one to five was used to determine the end attitude of the participants (agreed, disagreed, etc.).
After complete data collection, it was tabulated and statistically analyzed.
RESULTS
As table 1 shows, the majority of participants 364 (75.2%) accepted the concept of PMHC. Others, including participants who were neutral or did not accept PMHC totaled 120 (24.8%). Generally, those who accepted PMHC had a higher mean age (31.89 ± 9.74) than those who didn’t (28.7 ± 11.12) (p<0.003). The lowest percentage of acceptances (40%) was found among those aged less than 20 years. On the other hand, the highest percentage was found among those aged 30-34 and 35-39 years. These differences were found to be statistically significant. Acceptance was not affected by sex, (Table 2).
Table 1.
Participants’ acceptance of PMHC by age in Riyadh city, 1417H
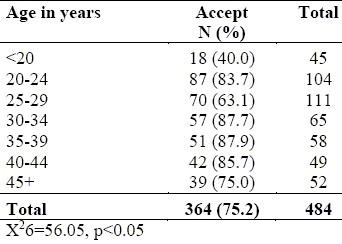
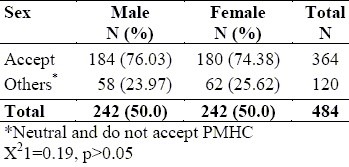
Table 2.
Distribution of participants by acceptance of PMHC and sex in Riyadh city, 1417H
Experience of marriage significantly affected the participants’ acceptance of PMHC. Out of those who had been married more than once, 62 (89.9%) accepted the PMHC compared to only 111 (62.4%), among those who had no experience of marriage (p<0.05), (Table 3).
Table 3.
Distribution of participants by social characteristics and PMHC acceptance in Riyadh city, 1417H
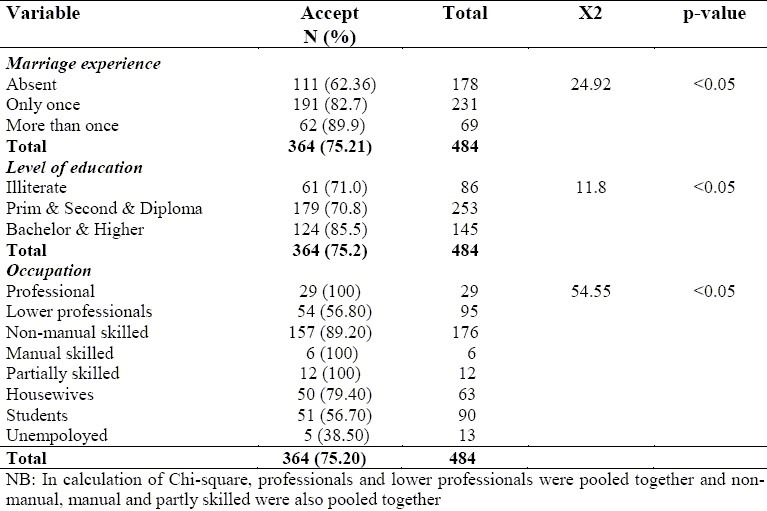
Concerning educational level, the highest percentage of those who accepted PMHC was found among the highly educated individuals 124 (85.5%), compared to 61 (71%) among illiterate participants (Table 3).
Relating participants’ acceptance of PMHC to their occupations, a statistical significant difference was found (p<0.05). Unemployed partcipants, students and lower professionals were the least likely to respond positively to PMHC (38.5%, 56.7% and 56.8% respectively) (Table 3).
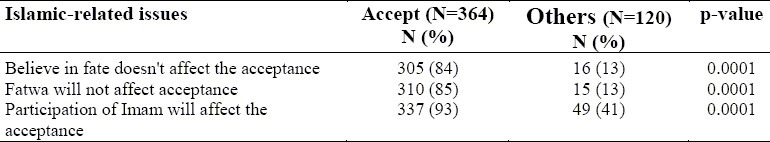
Misunderstood Islamic based issues negatively affected the study population's acceptance of PMHC as 104 persons (87%) of those who did not accept PMHC related attitudes to God's will (p<0.0001). Only 15 (13%) of those who did not accept PMHC did so despite the presence or absence of Fatwa (p<0.0001). Regarding the participation of Imam in a community-based health education program, 337 (93%) of participants who accepted PMHC welcomed the idea, compared to 49 (41%) of those who did not accept PMHC (p<0.0001) (Table 4).
Table 4.
Islamic-related issues affecting acceptance of PMHC in Riyadh city, 1417H
Of the participants who accepted the concept of PMHC, 273 (75%) persons agreed to voluntary exchange health fitness certificate between the couple to be married (p<0.001). In contrast, 212 (58%) rejected mandatory marital health fitness certificate (p<0.001). Confidentiality was the request of 298 (81.87%) participants and nearly 339 (93%) agreed to the inclusion of PMHC in school curricula. The cost of PMHC could hinder its practice among 196 (55%) participants who accepted it (Table 5).
Table 5.
Attitudes of participants accepting PMHC towards factors encouraging its practice in Riyadh city, 1417H
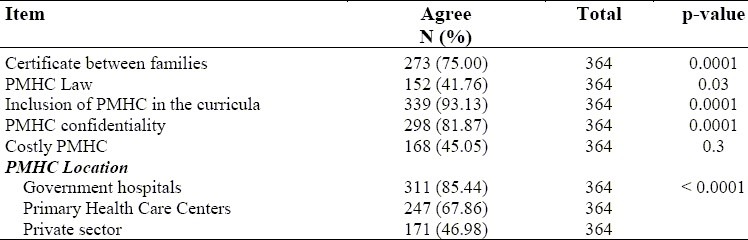
On the questions of the location of PMHC, 311 (85.4%) of the participants who accepted PMHC preferred it to be based in a governmental hospital, and 247 (67.9%) preferred it in PHCCs, in comparison to 171 (46.9%) who preferred it to be in the private sector (p<0.0001).
DISCUSSION
PMHC is a new and interesting health issue that needs to be investigated and discussed, especially in Islamic Arabic cultures, and more precisely in the Saudi community where consanguineous marriage represents more than 50% of all marriages, a rather high rate compared with many other countries.25,26 The present study can be the basis for further investigations of PMHC. Moreover, results discussed in the present study may require further investigations. It is necessary to mentions that, there have been few studies on premarital counseling and premarital medical examination in the Arab world.
The majority of participants 364 (75.2%) accepted the concept of PMHC, and those who accepted it were older than those who rejected it. The group that had the lowest percentage of acceptance of PMHC were aged less than 20 years. This finding can be explained by the fact that more exposure to life's experiences, a higher level of education, and marriage increases interest on health issues, particularly the health of offspring and consequently the acceptance of PMHC. There was no statistical difference on the attitudes on PMHC acceptance between males and females. This may be attributed to the present improvement of te social status of Saudi women e.g., female education, involvement in various occupations, etc.
On the question of marriage, the present study revealed that individuals who had an experience of marriage were significantly more accepting of the PMHC concept than individuals who had never been married. Also, participants who had been married many times were more accepting of the concept of PMHC than those who were still in their first marriage. Participants who had been married at least once have more knowledge and a greater awareness of the spouse's health problems. In addition, participants who were not married were usually younger, and were perhaps less educated and consequently less likely to accept PMHC. Similar findings were reported in Egypt where single people were seen to be the least likely to accept premarital conseling and examination.16
The majority of participants had an educational level above primary schools. This may have played a part in the positive acceptance of PMHC among the study group, as higher education means better knowledge of health matters.
On the participant's occupation, it was revealed that, PMHC acceptance increased among the higher social classes to as much as 100% among professional, in comparison with unemployed participants who had the lowest percentage of PMHC acceptance (38.5%).
The position of Islam is to prevent fetal malformations as far as possible. The Prophet Mohammad, peace be upon him, through many Hadiths directed attention toward inherited matters, and the careful choice of partners for marriage.17 Participation of Islamic leaders in community health education could have an important enhancing role in community acceptance of PMHC, as participation of the Imam and the presence of a religious fatwa can positively change the atttitude of about 53% of those who didn’t accept PMHC (41% and 13% respectively) (Table 4). In Western countries, religious men take part in premarital counseling.18,19 More health education from the Islamic point of view is needed, especially for young inexperienced persons and the uneducated individuals.
Medical examination and laboratory tests are mandatory prior to marriage application20–22 in many countries such as the USA and China because of some important health problems, like STDs, and hereditary diseases. The study showed that, voluntary exchange of marital health fitness certificate, between the two applicants for marriage had a good response among the participants accepting PMHC. However, if PMHC certificate became mandatory the percentage of acceptance would drop. This finding indicates that a community-based health education on the issue of PMHC legislation is necessary. Health education is one of the important means of encouraging the community to accept this idea23 and the inclusion of information of PMHC in the school curricula, could be the basis on which knowledge on health matters pertaining to the PMHC concept and its future acceptance could be built. Moreover, the assurance of the confidentality of information given during PMHC would ensure its continued success.24
Practicing PMHC in governmental establishments is preferred to its being given in the private sectors. This may be due to the high cost involved in private health care sectors, as 54% of participants who accepted the concept were not willing to participate if PMHC were costly.
CONCLUSIONS
The present study revealed that, 364 (75.2%) of study population accepted the concept of PMHC. Advancing age, experience of marriage, educational level and well-understood Islamic-related health issues positively influenced its acceptance. The participants who accepted PMHC concept agreed to the exchange of PMHC certificates between couples to be married but rejected the enforcement of PMHC by legislation. The need for confidentiality was stressed, a preference for its practice at governmental health establishments rather than private hospitals and the cost of the service were considered important.
RECOMMENDATIONS
The following are recommended:
The implementation of PMHC in Saudi Arabic, as it was accepted by the study population.
Execution of further studies to determine what should constitute PMHC, its implementation and its legislation on demographic basis of the Saudi community.
A community-based health education program for PMHC has to be devised in collaboration with Islamic leaders, to raise the level of awareness and acceptance of the community toward the concept of PMHC particularly with the following in mind: (a) that it should be directed mainly to single and young persons; (b) that school curricula should include PMHC education.
PMHC be free of charge in the governmental health institutes, or the cost minimal in the private sector.
The assurance of total confidentiality.
REFERENCES
- 1.Benson RC. Psychologic aspects of gynecologic practice. 5th ed. Beirut, Lebanon: Librairie du liban; 1984. Current obstetric & gynecological diagnosis & treatment. [Google Scholar]
- 2.Last JM, Wallace R. Genetic and Public Heatlh. 13th ed. USA: Prentice-Hall International Inc; 1992. Public health & preventive medicine. [Google Scholar]
- 3.Cassens BJ. Epidemiology, and prevention of selected acute illnesses. 2nd ed. USA: Williams & Wilkins; 1992. Preventive medicine and public health. [Google Scholar]
- 4.Awad HM. Autosomal recessive osteopetrosis. Annals of Saudi Medicine. 1994;14(2):102–6. doi: 10.5144/0256-4947.1994.102. [DOI] [PubMed] [Google Scholar]
- 5.Kasim A, Adnan A. Risk factors of mental retardation in children attending an educationally subnormal/mental school in Dammam, Saudi Arabia. Annals of Saudi Medicine. 1993;13(4):355–9. doi: 10.5144/0256-4947.1993.355. [DOI] [PubMed] [Google Scholar]
- 6.Alwan AS Hamamy H. Riyadh: King Abdulaziz City for Science and Technology; 1993. Hereditary disorders in the Eastern Mediterranean Region of World Health Organisation. Proceedings of the symposium on the medical genetics in the setting of middle eastern population. [Google Scholar]
- 7.El-Hazmi MA. Genetic diseases in Saudi Arabia: A model for national awareness and care programme. Saudi Medical Journal. 1992;13(6):514–20. [Google Scholar]
- 8.Ohlsson A. Better prenatal care in Saudi Arabia. Annals of Saudi Medicine. 1985;5(3):169–75. [Google Scholar]
- 9.Milnnsky A. Baltimore, USA: The John Hopkins University Press; 1992. Hereditary and your family's health. [Google Scholar]
- 10.Hu Z. Observation on prevention of hepatitis B virus transmission between newly-married couples by HbsAg vaccine. Chung, Hua, Liu, Hsing, Ping, Hsueh, Tsa, Chih (abstracts medline search) 1991;12(4):222–5. [PubMed] [Google Scholar]
- 11.Serdula M, mark J, Remington P, Ibara C, White M. Premarital rubella screening program: From identification to vacination of susceptible women in the state of Hawaii. Public Health Rep. 1986;101(3):329–33. [PMC free article] [PubMed] [Google Scholar]
- 12.Daniel WW. 4th ed. New York, USA: John Wiley & Sons; 1987. Biostatistics: A foundation for analysis in health science. [Google Scholar]
- 13.Streiner DL, Norman GR. Oxford UK: Oxford Medical Publication; 1989. Health measurement scales (A practical guide to their development and use) [Google Scholar]
- 14.Holman TB, Larson JH, Harmer SL. The development and predictive validity of a new premarital assessment instrument: The preparation for marriage questionnaire. Family Relations. 1994;43:46–52. [Google Scholar]
- 15.Marion P, Gendel E, Cortese P. California, USA: Mayfield Publishing Company; 1987. Planning and implementing health education in schools. [Google Scholar]
- 16.Eshra D, Dorgham L, El-Sherbeni A. Knowledge, attitudes, and practice towards premarital counseling, and examination. J Egypt Public Health Assoc. 1989;64(1-2):1–15. [PubMed] [Google Scholar]
- 17.Al-Bar MA. Jeddah, KSA: Dar Almanar; 1991. Malformed fetus, and genetic diseases, etiology, signings, and control. [Google Scholar]
- 18.Jones EF, Stahmann RF. Clergy beliefs, preparation, and practice in premarital counseling. The Journal of Postoral Care. 1994;48(2):181. [Google Scholar]
- 19.Steiner P, David K. Involvement of rabbis in counseling, and referral for genetic conditions: result of a survey. Am Hum Genet. 1993;53(5):1359–65. [PMC free article] [PubMed] [Google Scholar]
- 20.Holder WR, Knox JM. Syphilis in pregnancy. Med Clin of North Am. 1972;56(5):1151–60. doi: 10.1016/s0025-7125(16)32341-0. [DOI] [PubMed] [Google Scholar]
- 21.Rutkow IM, Lipton JM. Some negative aspects of state health departments’ policies related to screening for sickle cell anemia. Am J Public Health. 1974;64(3):217–21. doi: 10.2105/ajph.64.3.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Horton R. Western eyes on China's eugenics law. Lancet. 1995;15(346 (8968)):131. [PubMed] [Google Scholar]
- 23.Murphy EA, Chase GA. Chicago, USA: Year Book Medical Publishers INC; 1975. Principles of genetic counseling. [Google Scholar]
- 24.Gostin L, Curran W, Clark M. The cases against compulsory case finding in controlling AIDS - testing, screening and reporting. Am J Law Med. 1987;12(1):7–53. [PubMed] [Google Scholar]
- 25.Al-Abdulkareem AA, Ballal SG. Consanguineous marriage in an urban area of Saudi Arabia: rates and adverse health effects on the offspring. J Community Health. 1998;23(1):75–83. doi: 10.1023/a:1018727005707. [DOI] [PubMed] [Google Scholar]
- 26.Al-Husain M, Al-Bunyan M. Consanguineous marriages in Saudi population and the effect of inbreeding on prenatal and postnatal mortality. Ann Trop Pediatr. 1997;17(2):155–60. doi: 10.1080/02724936.1997.11747879. [DOI] [PubMed] [Google Scholar]


