Abstract
Objective:
To evaluate the quality of management of hypertensive patients attending Primary Health Care Center (PHC) in Dammam city and to determine factors that possibly affect it.
Design:
A cross sectional study and direct interview.
Setting:
Dammam city.
Subjects:
All doctors and nurses from a randomly selected sample of Primary Health Care Centers during April 1994.
Main measures:
Measuring the knowledge, attitude and practice of doctors and nurses about hypertension management.
Results:
Hypertension is regarded as an important health problem in Saudi Arabia in the opinion of majority of doctors (80′0) and nurses (69%). Almost half of the doctors and nurses believe that nurses are sufficiently qualified to measure blood pressure of patients. Most of the doctors (96.7%) and nurses (86%) depend merely on face-to-face education of patients Thirty percent of doctors and 34% of nurses think that the care for hypertensive patients in their Primary Health Care Centers is inadequate.
Conclusions and recommendations:
Offering on job training of both physicians and nurses on hypertension management. Producing a well planned protocol on the national level. Implementing a total quality management and medical audit system to PHC centers.
Keywords: Hypertension, Primary care and practice, Saudi Arabia
INTRODUCTION
Hypertension remains a major health problem, causing high mortality and morbidity all over the world. It is considered a major risk factor to both cerebrovascular accidents (CVAs) and coronary artery disease (CAD).
In the USA, mortality data reveal that for every employee killed in an industrial accident, more than 50 die of cardiovascular disease. Hypertension is incriminated as the main underlying cause.1
In Saudi Arabia, hypertension showed a wide range of prevalence, from 4-10%. The difference in these figures is mainly attributed to the variance in methods and criteria utilized to establish the diagnosis.2–5
As this disease can be detected early, primary care physicians and nurses are in an ideal position to improve the diagnosis and control of hypertension.6–10 Screening can be performed easily in PHC centers.
The up-to-date knowledge of the disease, its sequel, and proper management is essential for the primary health care physician. The attitude and practice of physicians and other health care providers towards hypertension and hypertensive patients should be optimized through scientific communication with specialized centers in the Ministry of Health (MOH), University Hospitals and other specialized centers. Such improvement in the knowledge, attitude and practice will definitely improve the care of hypertensive patients and lessen possible complications. Nevertheless, by improving public awareness of such medical problems, primary prevention and early detection plans can be implemented quite efficiently.
This study examined the KAP among physicians and nurses towards hypertension in the PHC centers in Dammam city, the capital of the Eastern Province in the Kingdom of Saudi Arabia (KSA).
MATERIAL AND METHODS
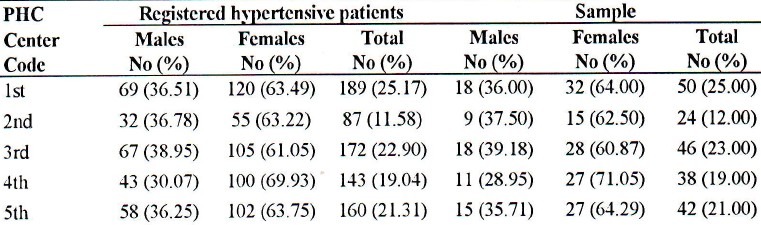
This is part of a major study assessing the quality of care provided to hypertensive patients. From a total of 20 primary health care centers in Dammam, we randomly chose 5 (25%). Two hundred patients (35.5% males and 64.5% females) were randomly and proportionally selected out of 751 patients receiving treatment at 5 PHC centers for more than one year. This sample represents 11% of the total known hypertensive patients registered at Dammam's PHC centers (Table 1).
Table 1.
Sample of hypertensive patient's from Dommam's PHC centers
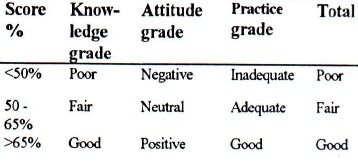
All physicians (30) and nurses (50) in the selected health care centers were approached and interviewed. They represented 40% and 33% of Dammam City PHC centers’ physicians and nurses respectively. To check their knowledge, attitude and practice towards hypertension management, a structural questionnaire was designed for both physicians and nurses. This questionnaire was scored as requested by the authors. The allocation was 40% to knowledge, 35% for practice and 25% for attitude.
RESULTS
Knowledge questions
Hypertension was regarded as an important health problem in Saudi Arabia in the opinion of majority of physicians 24 (80°/,) and nurses 48 (96%). This belief was mainly due to a high number of hypertensive patients encountered during their work. Furthermore, all the physicians and nurses believed that complications of hypertension can be prevented.
Four out of 30 physicians (13%) and 27 out of 50 nurses (45%) gave an incorrect definition of hypertension. The remaining stated either correct or partially correct definitions.
Twenty-seven (90%) physicians stated that they knew the diagnostic criteria for hypertension, whereas only 2 (6.7%) gave the criteria as stipulated by the World Health Organization.
Only 4 out of 30 physicians (13%) were able to mention the names of all anti-hypertension drug groups. The remaining offered incomplete answers.
On being asked about the side effects of the antihypertensive drugs, the majority of physicians 24 (80%) mentioned a few. On the other hand, the remaining 6 (20%) were not able to recall any side effect.
Attitude Questions
Four out of 30 physicians (13%) and 13 out of 50 nurses (26%) stated that the treatment of hypertensive patients should be team work shared by the cardiologist, the PHC physicians and nurses. Others felt that either the cardiologist or the PHC physicians should be responsible for the management.
Health education offered to hypertensive patients was regarded as the responsibility of the PHC center team by 20 (66.7%) of the physicians and 25 (50%,) of the nurses. The remaining cited only one of the health team personnel.
All physicians and 44 nurses (88%) reported that the causes of poor patient compliance were: the lack of patient commitment, inadequate health education, patients’ attendance at other places for treatment; the communication gap between patients and the health center. The lack of confidence in the health team, the underestimation of the seriousness of the disease by the health team was a possible cause. Other reasons like poor patient knowledge, transportation problems for some patients specially for female patients and the long wait in the PHC centers before seeing their physician were cited as a final cause.
In the opinion of PHC physicians and nurses, the follow-up of hypertensive patients after being stabilized, ranges between one week to 2 months.
Thirteen (34.3%) physicians and 28 (5G%) nurses believed that it was the nurse's duty to measure BP, the remaining mentioned one of the other health team personnel.
Practice Questions
All physicians and nurses claimed that they offered health education to their patients on every visit using the face-to-face method.
The level of BP at which a GP should start drug treatment was inconsistent. Six (20%) physicians stated 140/90 mmHg as the level above which they would start drug treatment. Six physicians (20%) gave levels of tip to 160/100. Another group of 4 physicians (13%) said there was no cut-off point since this depended on the age of the patient and 14 physicians (47%) stated that it was according to DBP only, ranging from 110 mmHg.
Reasons for referring hypertensive patients to hospitals were debatable. Some reasons are listed hereunder in order of frequency: uncontrolled hypertension, hyper-tensive emergencies, and the specialist's opinion.
The frequency of performing fundoscopy and 12 lead conventional electrocardiogram was investigated. The majority of physicians (90%) suggested intervals of 1-12 months.
On asking PHC physicians about the anti-hypertensive drugs that should not be given during pregnancy, 12 (40%) said they did not know, and 5 (1G.7%)) physicians gave wrong answers. On the other hand, the remainder gave the names of some but not all drugs.
Hypertension was considered controlled if BP level was 140/90 mmHg or less in the opinion of 6 (20%) physicians, between 120-160 mmHg systolic and 80-100 diastolic in the opinion of the majority, and 2 physicians (6.7%) did not know the answer.
The majority of physicians 28 (93.3%) and nurses 41 (82%) rated their knowledge about hypertension as good.
Nine (30%) physicians and 17 (34%) nurses believed that the care provided for hypertensive patients at their PHC centers was inadequate.
Four (13.3%) physicians and 5 (10%) nurses believed that there is no need for regular maintenance of the BP apparatus, others mentioned variable periods ranging from 1 month to 2 years.
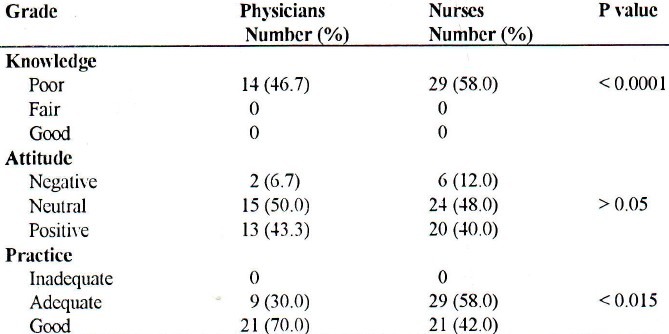
Table 2 shows a comparison between physicians’ and nurses’ KAP scores grading results. There is a statistically significant difference in knowledge and practice, but this was not the case for attitude or for the overall KAP score grading.
Table 2.
Grading of physicians’ and nurses’ KAP scores
Suggestions by PHC physicians and nurses to improve patient care:
More structural and specialized health education for patients.
A hypertensive registry in each PHC center with a system of calling defaulters.
Regular visits by the health education specialist to PHC centers to improve the quality of health education materials and methods.
Continuing medical education courses for the PHC staff to update their knowledge on hypertension.
Improvement in the appointment system for referred cases to hospital.
Home visits for hypertensive patients.
Special hypertension clinic.
A special identification care for hypertensive patients registered in each PHC center.
The ranges and means of scoring for physicians’ and nurses’ KAP questionnaires are shown in Table 3. When KAP results of Physicians’ and nurses’ KAP grading were compared, a significant difference in knowledge and practice was found, but this difference was not obvious for attitude as in Table 4 or overall KAP grading.
Table 3.
Physicians’ and nurses’ KAP range and mean scoring
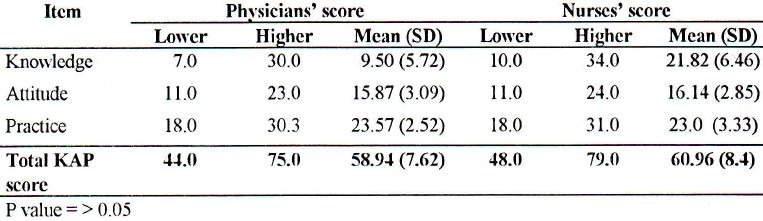
Table 4.
Grading of physicians and nurses
DISCUSSION
The scores of both physicians and nurses regarding basic information about hypertension was low. Such low scores may be related to poor quality of PHC staff, lack of continuous medical education programs and scientific channels between PHC staff and specialized centers. Despite this, higher attitude and practice scores were obtained probably because practice and attitude do not depend on knowledge only but also on other factors including experience. These results coincide with results of a similar study in South Africa.1
There was no significant difference among physicians and nurses in the overall KAP scoring, which could be explained by the unfortunate fact that both groups had little knowledge. This was not the case for physicians with regard to their knowledge about management of hypertension (criteria of diagnosis, levels to start drug therapy, and levels of control). Some physicians gave correct answers, but others gave completely wrong answers which might lead to misdiagnosis and unsatisfactory medical treatment of patients as hypertensive, or the neglect of some hypertensive patients with uncontrolled BP. This agrees with other studies.1,11–21
Both physicians and nurses provided some practical suggestions which are worth considering.
The overall results from this study showed an unsatisfactory KAP among PHC physicians and nurses in Dammam city PHC centers, indicating their inability to provide the desired quality care for this group of patients. Our findings confirm the urgent need to establish a comprehensive training program to all PHC physicians and nurses.
Finally, any effective plan for improving hypertensive management should not exclude some important items such as the following:
Adopting and implementing the latest updated recommendations of the Joint National Committee on Detection, Evaluation and Treatment of High Blood Pressure which are based on years of experience and clinical trials.22
The on-the-job training of both physicians and nurses on hypertension management based on well-planned protocols at the national level. Stressing the role of nurses as an important complementary support would give the physician more time to concentrate on difficult areas.9,10,23
Implementation of quality assurance e.g. continuous monitoring, evaluation and self assessment are mandatory for better management.
A larger scale study may be advisable to evaluate the extent of this problem among PHC physicians and nurses all over the Kingdom. This will elicit more information to plan and implement interventions for the improvement of service.
Efforts for assessing the PHC team to provide better management for hypertensive patients would be advantageous.
ACKNOWLEDGMENT
We would like to thank Dr. Mustafa Abdel Gany, MRCP, Consultant Cardiologist, Fakhry Hospital, for the valuable advice and for helping in questionnaire design. And to all the PHC physicians and nurses for their cooperation.
REFERENCES
- 1.Pick WM, Steyn K. Hypertension in family practice. A study of knowledge, attitudes, and practices. S Afr Med J. 1992;82(4):257–9. [PubMed] [Google Scholar]
- 2.Abu Aisha H, Al-Khater A, Al-Omar O, Arafa M, Krimely M. Proceedings of the symposium on Hypertension: Current Concepts and Management. Riyadh: 1985. May 16, The epidemiology of hypertension in a rural community in central Saudi Arabia. [Google Scholar]
- 3.Ahmed AF, Mahmoud ME. The prevalence of hypertension in Saudi Arabia. Saudi Med J. 1992;13(6):548–551. [Google Scholar]
- 4.Al-Shammari SA, Khoja TA, Arafa M. Proceedings of the First Gulf Primary Health Care Conference. Salmanya. Bahrain: Faculty of Medicine, Arabian Gulf University; 1993. Noc. Hypertensive patient's care in primary health care centers in Riyadh: assessment of quality. [Google Scholar]
- 5.Al-Nosha M, El Shabrawy MA, Karrar A. Proceedings of the 5th Scientific Session 1994. Al-Khobar: Saudi Heart Association; 1994. Jan, Arterial hypertension in Saudi Arabia. [Google Scholar]
- 6.Mann KV, Putnam W. Physicians’ perceptions of their role in cardiovascular risk. Prev Med. 1989;15:875–6. doi: 10.1016/0091-7435(89)90053-4. [DOI] [PubMed] [Google Scholar]
- 7.Mead M. Hypertension the GP Perspective. Update. 1988;2:875–6. [Google Scholar]
- 8.Guyther JR, Kochar MS. The family physician's role in detection and control of hypertension. Fam Corn Health. 1981;4(1):21–7. doi: 10.1097/00003727-198105000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Scwartz LL, Raymer JM, Nash CA, Hassan IA, Muenter DT. Hypertension: role of the nurse-therapist. Mayo Clin Proc. 1990;65(1):67–72. doi: 10.1016/s0025-6196(12)62111-9. [DOI] [PubMed] [Google Scholar]
- 10.Jewell D, Hope J. Evaluation of a nurse-run hypertension clinic in general practice. Practitioner. 1988;232:484–7. [PubMed] [Google Scholar]
- 11.Keil U, Spelsberg A, Weiland SK, Hartel U. Physician inquiry in Bochum/Dorimund Stuttgart and Munich, Germany. In: Strasser T, Wilhemsen L, editors. Assessing hypertension control and management. Geneva: WHO; 1993. pp. 103–8. [Google Scholar]
- 12.Fuller A, Lasser U, Schumann V, Siegel M. Physician inquiry in Stuttgart, Germany. In: Strasser T, Wilhemsen L, editors. Assessing hypertension control and management. Geneva: WHO; 1993. pp. 109–14. [Google Scholar]
- 13.Torner I, Soler M. Physician inquiry in Catatonia, Spain. In: Strasser T, Wilhemsen L, editors. Assessing hypertension control and management. Geneva: WHO; 1993. pp. 115–20. [Google Scholar]
- 14.Manek S, Rutherford J, Jackson SH, Turner P. Persistence of divergent dews of hospital staff in detecting and managing hypertension. BMJ. 1984;289:1433–4. doi: 10.1136/bmj.289.6456.1433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fotherby MD, Harper GD, Potter JF. General practitioner's management of hypertension in elderly patients. BMJ. 1992;26(305):750–2. doi: 10.1136/bmj.305.6856.750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Willburn RL. Mild hypertension. Should all patients be treated? Postgrad Med. 1984;76(7):107–13. doi: 10.1080/00325481.1984.11698803. [DOI] [PubMed] [Google Scholar]
- 17.Cooper JR. Management of hypertension in general practice. BMJ. 1981;282:380–2. doi: 10.1136/bmj.282.6273.1380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Barber JH, Beevers DG, Fife R. Blood pressure screening and supervision in general practice. BMJ. 1979;1:843–6. doi: 10.1136/bmj.1.6167.843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mudge P, Jackson C, Pyke J. The management of hypertension in Queensland general practice. Aust Fam Physician. 1990;19:1569–70. [PubMed] [Google Scholar]
- 20.Cove-Smith JR. Hypertension: current prescription policies. Update. 1990;17:1212–6. [Google Scholar]
- 21.Carter BL, Kriesel HT, Steilkraus L, Knudson R. Anti-hypertensive drug prescribing patterns of internist and family physicians. J Fam Pract. 1989;29(3):257–62. [PubMed] [Google Scholar]
- 22.The Joint National Committee on Detection, Evaluation and Treatment of High Blood Pressure. The 5th report of the Joint National Committee on Detection, Evaluation and Treatment of High Blood Pressure (JNCR) Arch Intern Med. 1993;153:154–83. [PubMed] [Google Scholar]
- 23.Bass MJ, Whinney IR, Dormer A. Do family physicians need medical assistants to detect and manage hypertension? CMAJ. 1986;134:1247–55. [PMC free article] [PubMed] [Google Scholar]


