Abstract
Community-based participatory research (CBPR) with disability communities is directed toward facilitating full inclusion of individuals with disabilities and disability community organizations in all aspects of the research process. Within the CBPR framework, academic-disability community partners may value and wish to use experimental designs to test interventions. Being aware of and proactively addressing barriers and challenges to inclusion in the areas of human resources, training, productivity, accommodation, and inadequate funding for disability community organizations are critical for success. Some of the strategies discussed in this paper for addressing these challenges include creating redundant systems, providing benefits counseling and individualized payment options for employment, designing trainings to be disability friendly, and carefully considering selection of partners in light of available community resources.
Keywords: community-based participatory research, disability community, disability research
Community-based participatory research (CBPR) is an inquiry framework that fosters the creation of practical strategies to fully include individuals with disabilities in research (Mmatli, 2009). CBPR is directed toward engaging researchers and community members as equal partners to generate knowledge that is immediately relevant and accessible to communities, especially those who have historically experienced social and economic marginalization (Bricher, 2000; Israel, Schulz, Parker, & Becker, 1998; Minkler, 2005). This aim and its underlying critical and participatory epistemology drive a commitment within the academic-community partnership to develop strategies that empower community members to participate fully and not be limited to an advisory or “token” role. (Kliewer & Biklen, 2000; Lord & Church, 1998; Zimmerman, Tilly, Cohen, & Love et al, n.d.). This type of equal partnership with full participation, voice, and power in the research process, from beginning to end, constitutes full inclusion. Active facilitation of full inclusion of individuals with disabilities in CBPR requires that all partners systematically address the social and physical barriers to participation and employment often faced by members of disability communities (Bricher, 2000; Mmatli, 2009). For the purposes of this paper, disability community is defined as individuals with physical disabilities and their consumer-led disability advocacy and service organizations.
Because the nature of disability often affects the ability to work and requires disability accommodation, the challenges of achieving full inclusion and participation of community members in all aspects of a CBPR project go well beyond those frequently cited in the general CBPR literature (e.g., distrust of researchers, inadequate time for relationship building; Block, Skeels, & Keys, 2006; Lord & Church, 1998). Moreover, the extent of disability community participation required to meet CBPR standards places the frequency and magnitude of disability-related challenges at a level that is much higher than is typically found in traditional (i.e., researcher-directed) research. These disability-related challenges may be particularly acute in CBPR experimental research studies that include multiple activities with interventions or data collection at fixed time-points. Thus, our purpose in this paper is to prepare researchers and the disability community to address challenges to full inclusion of individuals with disabilities in CBPR generally and in experimental CBPR in particular effectively.
In this paper we discuss key challenges that have significantly affected the work of our academic-disability community partnership in two experimental CBPR studies. We describe the background and context of our academic-disability community partnership and the collaborative development of the two experimental CBPR projects. We then describe our experiences with disability-specific challenges and recommend strategies for overcoming barriers in five areas including: (a) human resources; (b) training; (c) disability and productivity; (d) disability accommodation; and (e) inadequate funding for disability community organizations. Although use of these strategies is particularly critical in experimental CBPR for the reasons described above, they may be applied in any research seeking to promote inclusion of individuals with disabilities. Figures at the end of each section highlight the key points related to awareness of challenges, planning, and the benefits of proposed inclusion strategies.
Partnership and Studies
Origins of Our Academic-Disability Community Partnership
The principal investigator (PI; the first author) and co-investigator (the third author) have worked together for more than 10 years on multiple disability community-placed projects. This community-placed work resulted in the formation of community relationships that provided a foundation for the development of an academic-disability community partnership. Consistent with a collaborative approach, our academic-disability community partnership was formalized during a series of town meetings held for the purpose of identifying disability community health priorities (Cheadle, Senter, Solomon, Beery, & Schwartz, 2005). The town meetings were held at various community locations and primarily attended by women with physical disabilities. Through this information-gathering process, depression in women with physical disabilities was identified as a major community concern, and the partners set out to consider how the community might effectively address this health problem. Guiding principles included collaboration, accessibility of all aspects of the projects to individuals across physical disability types, and development of interventions that enable community control over future implementation (Israel et al., 1998; White, Nary, & Froehlich, 2001). Two ongoing CBPR studies: Reflection, Insight, and Self-Empowerment (RISE) and Healing Pathways, were born out of this collaboration.
Study Aims
The specific aims of the RISE study are to: (a) strengthen and expand an existing academic-disability community partnership; (b) develop a peer-implemented group therapy intervention for treatment of depression in women with physical disabilities; and (c) assess the feasibility of the intervention. This work provided a foundation for the Healing Pathways study. The specific aims of the Healing Pathways study are to (a) modify an existing program to develop a strengths-based cognitive behavioral group therapy intervention for treatment of depression in women with physical disabilities (Ridgeway, McDiarmid, Davidson, Bayes, & Ratzlaff, 2002; Zinbarg, Mashal, Black, & Fluckiger, 2010), and (b) conduct an efficacy trial using a wait-list control design. The RISE/Healing Pathways academic-disability community partners include two universities, individuals with disabilities from two rural and two urban communities, and a wide array of disability community organizations in these same areas. Although numerous disability community organization partners supported research recruitment efforts, key disability community organizations such as the HASL Independent Abilities Center (HASL, formerly known as the Handicap Awareness and Support League) had a higher degree of engagement. Greater engagement occurred when data collection and intervention activities took place at partner locations and included disabled employees of those organizations as paid team members.
Composition of Research Teams
We set out to include as many members of the target population (i.e., women with physical disabilities) on our research teams as possible within the timeframes available. We were successful in this goal, with 12 of 14 RISE and 11 of 15 Healing Pathways team members being women with physical disabilities, most of whom also had other co-occurring health conditions. On both studies, team members with physical disabilities assumed primary responsibility for participant recruitment, screening and enrollment, data collection, participant retention, participant safety, and implementation of the intervention. Analysis and dissemination activities are currently underway. Research teams consisted of the investigators, Center for Independent Living (CIL) directors and staff (e.g., HASL), individual disability community members, and students. A CIL is “a consumer-controlled, community-based, cross-disability, nonresidential private nonprofit agency that is designed and operated within a local community by individuals with disabilities and provides an array of independent living services” (Independent Living Research Utilization, 2011). Key roles assumed by team members with physical disabilities have included peer group co-facilitator, personal care assistant, advisory board member, and leader of dissemination and/or follow-up work groups.
Study Designs and Methods
Both studies used mixed methods including focus groups and a randomized control trial of a peer-led group depression intervention with a wait-list control group (n=82 and n=90, respectively). As noted earlier, the target populations for both studies were women with physical disabilities who required some form of accommodation for mobility or sensory impairment or both. To be eligible for participation in either study women also had to have a Center for Epidemiologic Studies Depression (CES-D) Scale cut-off score of 16 or higher (Radloff, 1977).
The RISE intervention was first developed using focus groups and community input including the unpublished personal writings of some women with physical disabilities on the research team. Women's descriptions of their personal experiences with disability and depression directly informed the topics and approaches we incorporated into the intervention. We then assessed the feasibility of the intervention and preliminarily assessed efficacy.
Healing Pathways built on this work by modifying the RISE intervention and conducting an efficacy pilot. Two focus groups were conducted to gather information on strengths-based interventions to support further modifications of the RISE intervention that was then renamed the Healing Pathways program. Focus groups were conducted with therapy groups to support continued improvement of the program. Both studies used level of depressive symptoms as the primary outcome variable. Secondary outcomes for both studies were: self-esteem, coping, healthy lifestyle behaviors, and loneliness. Results from these studies will be forthcoming.
Tensions Involved in Selecting an Experimental Research Design
Researchers have recommended that changes can be made to increase the flexibility of traditional experimental designs in order to make them more adaptive to complex interventions, multi-level outcome variables, and/or multiple and variable implementation settings (Craig et al., 2008; Gross & Fogg, 2001; Preference Collaborative Review Group, 2008). Developing and testing an intervention in a disability community may involve any or all of these elements of complexity. One example of an adaptation of experimental design is to consider participant preference of assignment to control or intervention group as part of the randomization procedure, or to utilize wait-lists for participants in control groups to have access to the intervention at a later time (Gross & Fogg, 2001). These adaptations may have particular applicability in a CBPR experimental study where participants rightfully expect to have a degree of self-determination in the study. Additionally, feasibility studies to address potential vulnerabilities of the study design, intervention, or community-based settings may be useful to make adjustments prior to scaling up the intervention (Craig et al, 2008). Process evaluations can be designed and conducted within the study to assess intervention implementation fidelity, clarify causal mechanisms, or identify contextual factors influencing outcomes (Craig et al., 2008; Gross & Fogg, 2001; Preference Collaborative Review Group, 2008).
These approaches, however, do not enable flexibility of data collection time points. Multilevel modeling (MLM) is a statistical approach that may be used to increase the flexibility of data collection time points in a randomized control trial (Raudenbush, Bryk, & Congdon, 2004). Drawbacks associated with MLM include lack of familiarity with the approach by many reviewers for use in a randomized control and the need for advanced statistical expertise on the research team. When MLM is not the method of analysis used, work on experimental research studies is generally completed at fixed time points, and demands for productivity are high during intervention and data collection periods. Unexpected changes in productivity, which are a common experience for individuals with disabilities, are difficult to accommodate without jeopardizing study results. Thus, tensions may arise when CBPR partners desire both a flexible research design and rigorous testing of an intervention. Nevertheless, experimental design is one that a disability community may value and wish to utilize to test the efficacy of community-led interventions (Krahn, Putnam, Drum, & Powers, 2006). Access to all types of research designs by community choice is consistent with both the participatory philosophy of CBPR and the Americans with Disabilities Act (ADA, 2008; Krahn et al., 2006). Although in some instances incredibly difficult to carry out, experimental design is a form of valuable research to which the disability community deserves access. Being aware of options to increase design flexibility like MLM, and addressing the five challenges to full inclusion in CBPR described here, is critical to ensuring that disability community access to participatory experimental studies is genuine.
Discussion of Five Challenges to Full Inclusion
Human Resources
A major challenge to full inclusion we faced was hiring team members who were women from the disability community receiving disability benefits. Including individuals receiving federal or state-subsidized disability income and other benefits is important for the conduct of CBPR in the disability community. It is critical to recognize the importance of this aspect of inclusivity, while at the same time being prepared for its inherent challenges (Northway, 2010).
Individuals receiving either Supplemental Security Income (SSI) or Social Security Disability Insurance (SSDI) from the U.S. Social Security Administration face significant restrictions on the amount of income they are allowed to earn without losing benefits. Earning any amount over the cap for a specified time period will result in substantial losses to the benefit recipient. This fact has had three tangible effects on our projects. First, it reduced the applicant pool for team positions. Second, it promoted feelings of anxiety and vulnerability among team members receiving benefits (the majority of the team). Third, it necessitated establishment of multiple systems for billing and reimbursement of team members. Each of these effects increased administrative time. A reduced applicant pool translated into greater time needed for recruiting and hiring of employees. Fear of loss of benefits created greater stress and burden for selected team members that in turn affected the entire team. Finally, there was a need for multiple flexible payment systems, which were not readily accessible in the existing university research grants and contracts system (and thus needed to be found or improvised), requiring substantial time investment because these arrangements varied both within and across team members.
Offering pre-employment benefits counseling is an approach that may reduce fear about losing SSI/SSDI lifelines and help eliminate barriers to paid employment on CBPR teams. On our research teams the co-investigator initially offered benefits counseling on an informal basis. The demand for this service proved so great, however, that she was unable to sustain this effort. Planning for greater administrative time and writing a part-time benefits counselor into the budget and/or partnering with an agency that offers this service are possible methods for supporting full inclusion.
Examples of strategies used to address financial issues in our studies included finding ways to pay for volunteer expenses for team members whose benefits restrictions precluded any earned income, placing team members on the regular university payroll system with variable hours, and creating multiple independent contracts. Although crucial, these efforts were burdensome and stressful for both the PI and research grants and contracts support staff who expressed concern that they had “exhausted fringe mechanisms,” “asked for favors,” and “tried to push things through” to create financial access for team members (Alcala-Moss, 2010, p.7). Expecting these challenges and having frank up-front discussions may be helpful in addressing these difficulties. At a national health research policy level, it is worth examining how current health research fiscal structures could be modified to make CBPR, especially of experimental and other high workload and time-sensitive designs, more accessible for disability communities (Figure 1).
Figure 1.
Key Points Regarding Human Resources Challenges
Training
Several authors have identified “learn as we go” as a useful training strategy for CBPR projects in the disability community because it emphasizes the educational component of this approach to research (Minkler et al., 2008; Zimmerman et al., n.d.). Although the flexible, evolving nature of this kind of learning approach may be optimal for preparing and supporting community members to fully participate in CBPR, it is challenging to use this approach when an experimental design is involved. Training for team members involved in traditional experimental designs emphasizes up-front development of the research skills needed to recruit and retain participants, collect and manage data, and maintain intervention fidelity and safety, thus making an evolving “learn as we go” approach challenging to implement. Creating a training plan that addresses CBPR and experimental design goals while accommodating disability is the second CBPR interventional research team challenge (Ochocka, Janzen, & Nelson, 2002).
Despite the clash between “learn as we go” and more structured approaches to training, options for addressing emergent training needs are best considered as part of an overall strategy. In our studies, because a majority of team members had no prior research or clinical training, they looked to the academic investigators to design and implement trainings. Although the academic investigators solicited input regarding the content and structure of trainings, team members had difficulty identifying the amount, level, and specificity of training needed. For both RISE and Healing Pathways, the intervention peer group co-facilitators had to learn not only skills to carry out the research protocol, but also to conduct a manualized group depression intervention. Although most of the disability community members selected to be trained as peer co-facilitators had previous experience with informal support group work in the community, none were trained mental health clinicians. Initial training sessions for both studies were focused on developing research skills for implementation of protocols in a variety of areas including recruitment and retention, data collection and management, intervention fidelity, and safety. Additional training was provided to peer co-facilitators on a variety of topics pertinent to delivery of the intervention. Examples included principles and practice of group therapy, cognitive behavioral therapy, and positive psychology. For RISE, we held a 3-day training retreat for team members and found that the days were too long and the agenda overly full. This was true despite having obtained substantial input from disabled team members regarding the training format in advance. Within 90 minutes of beginning the first day, team members frequently left the room for unscheduled breaks, which made continuity of the training schedule difficult to maintain. We learned that the days we had planned were too long and the number of scheduled breaks too few for team members who were dealing with chronic pain and fatigue related to disability.
Having learned from our experiences on RISE, we redesigned the initial training format and held a “disability friendly” 10 day training retreat for Healing Pathways. This training covered the same topics as the 3-day retreat of the previous RISE study, but incorporated more frequent breaks of longer duration. We calculated the costs of the Healing Pathways retreat at $500 per person per training day ($5000 per person total for the full 10 days) excluding administrative costs, which were substantially more than originally planned. In addition to this 10 day large group training, additional site specific face-to-face and telephone training support was also provided, totaling approximately 100 hours. Finally, team members and peer co-facilitators undertook many additional hours of self-study to complete the training program. Although the training plan was fairly successful, consistent feedback received from team members indicated that the supplemental face-to-face and telephone training support was insufficient to prepare them for the complexity of their roles. Including a larger number of academic researchers on the team to act as research mentors to community members probably would have resulted in a better fit with the “learn as you go” CBPR training model. Yet such a strategy would also substantially increase cost and change the ratio of community members to academic researchers on the team, thereby potentially introducing a new set of challenges.
Several recommendations related to training can be gleaned from this experience. First, an overestimate of time and financial resources for training is preferable to an underestimate. Community members with no prior research or clinical experience may not understand basic concepts. Moreover, because full inclusion necessitates that individuals with disabilities from the community assume critical project roles, high levels of training may be required for some team members as was the case for our peer co-facilitators. Second, costs associated with disability accommodation such as wheelchair accessible transportation and hotel rooms, and providing training materials in special formats are substantial and need to be correctly factored into training costs. These costs will vary depending on the types of disability represented on the team. Third, we recommend training schedules that include frequent long breaks and shorter days. We suggest that blocks of training time longer than 90 minutes be avoided. Finally, team members dealing with chronic pain and fatigue may have difficulty absorbing large amounts of information in a short time. We recommend being prepared to repeat training concepts at multiple time points and to provide multiple options for team members to demonstrate proficiency with the material and skills (Figure 2).
Figure 2.
Key Points Regarding Training Challenges
Challenges Related to Disability and Research Team Productivity
Although discussion of issues related to productivity in the disability community can be politically sensitive, an open and honest approach to discussing and addressing this reality is essential to planning for full inclusion in CBPR. Productivity issues are most likely to present challenges on research studies that do not allow for a flexible and fluid schedule of activities and deadlines, such as is often the case in experimental studies with multiple intervention and data collection time points.
When planning a CBPR intervention study, investigators need to anticipate the number and type of paid team members based on an estimate of the types of knowledge and skills needed as well as the amount of time required for completion of specific tasks. For example, when deciding how many team members are needed to collect data, an estimate of the amount of time required for completion of a data collection interview is an important piece of information for calculating time and costs. In our studies, we found it very difficult to identify accurately how many hours were needed to complete specific research activities because productivity varied widely both within and across team members. Thus, the amount of time required to complete work was never constant. Moreover, we found that team members tended to overestimate what they were able to do.
The physical disabilities and related symptoms of team members affected their level of productivity to a much greater degree than they themselves and other team members anticipated. For example, a team member estimated she could easily manage working 10 hours per week, but later struggled to work 5 hours per week even when provided with reasonable accommodation such as working from home and a flexible work schedule. This type of situation became even more difficult to manage when team members who were in this position, feeling embarrassed or fearing loss of employment, attempted to cover up their performance problems thereby leaving the rest of the team under the impression that work was being completed. The unpredictable waxing and waning nature of primary disabilities, and the onset of secondary health conditions, including hidden conditions such as psychiatric disorders, were at the heart of this issue.
In addition to variability in the total number of hours team members were able to work, the nature and severity of disabilities also influenced the amount of time it took for team members to complete specific activities. Team members had no way to accurately predict during the hiring and training processes, which were often conducted in a group format, how long task completion might take them, making it even more difficult to anticipate and plan the workload. Thus, while it took one team member 45 minutes to complete a post-test with a study participant; another team member took 3 hours to complete the same task. These situations created ongoing stress and discomfort for the entire team. Very often, team members reported pushing themselves beyond their limits. One team member asked, “Are we not acknowledging that we have disability?” (Alcala-Moss, 2010, p.9). Either team members felt pressure to complete work they had committed to, despite experiencing physical or psychiatric symptoms that made it difficult for them to do so, and/or their work was taken up by other team members who in turn became overloaded by repeatedly completing extra work that had been originally assigned to others. The result, all too often, was a thoroughly exhausted team.
An appropriate remedy for this challenge is to build in hiring and training additional team members into the research plan, and to extend the length of the study, thereby providing team members with more time to finish their work. Creation of redundant systems and extending timelines provides breathing room for team members whose physical and/or psychiatric symptoms slow them down and/or whose work speed is slower than others at baseline. These systems also provide back-up for critical functions. To be effective, this remedy requires advanced planning and an appropriate budget (Figure 3).
Figure 3.
Key Points Regarding Productivity Challenges
Accommodation
Although disability accommodation is a concept that cuts across other areas described in this paper, because it is so vital to the success of full inclusion, we have chosen to give it a separate section of its own. Full inclusion of individuals with physical disabilities in all aspects of the research process is difficult to achieve without reasonable accommodation related to mobility, pain, fatigue, and related concerns. Reasonable accommodation for individuals with disabilities according to the Americans with Disabilities Act of 1990, As Amended (2008) includes making buildings, facilities, and transportation readily accessible; restructuring work schedules and assignments; modifying equipment, training materials and policies; and other similar accommodations. All reasonable accommodations under the ADA (2008, p. 4) are based on the recognition that individuals with disabilities deserve to “fully participate in all aspects of society” and that failure to provide accommodation to facilitate such inclusion is to “segregate” and “discriminate” against the individual with disability on a par with discrimination on the basis of ethnicity, color, sex, national origin, religion, or age.
Assessing for and meeting accommodation needs both for team members and study participants require substantial time and financial resources. Planning for these costs ahead of time can never be fully accurate because the number and types of accommodations needed cannot be fully predicted. Therefore, we recommend beginning with a reasonable estimate and then conducting ongoing assessments of accommodation needs as the study unfolds. Referral to the ADA (2008) may be helpful in determining what is deemed reasonable; however, ethical obligations to provide accommodation should also be considered (Kliewer & Biklen, 2000).
Examples of accommodations to consider based on our team's experience may include: personal assistant services during groups for some study participants; technical assistance with computers and software programs; providing workbooks in electronic format, on special paper, and with larger font (we used Verdana 14 as the standard font); and special transportation arrangements. For research team members specifically, we suggest also making an effort to match roles and tasks with abilities as an additional accommodation strategy (Lasker, Weiss, & Miller, 2001; Mmatli, 2009). Because the unique characteristics of team members' skills and abilities may not always be clear right away, openness to making changes to essential job functions may be necessary over time. This process will require administrative time for analysis of work patterns and identification of strategies and supports. Although the practice of accommodating each other is generally helpful and necessary, when done informally (i.e., one employee asks another to do part of his or her job), it risks resentment among team members when over-utilized. Dealing with accommodation needs proactively and explicitly, introducing redundant systems for built-in support, and encouraging open and assertive communication are all useful strategies to consider when addressing these issues.
Another important consideration pertaining to accommodation relates to the level of supports provided to study participants in unusual circumstances. We found that adhering to study protocols was a challenge for team members when they were working with study participants who were prior acquaintances or even friends. This is not an unusual occurrence in small, tightly knit communities. In these instances, the extent of the help expected and/or provided may exceed reasonable bounds. An example from RISE occurred with a participant who used marijuana for pain management. In the state of Oregon, where our studies are ongoing, individuals may possess a limited number of marijuana plants or a small amount of harvested marijuana plant material if they have a medical marijuana card signed by an attending physician. There are a limited number of debilitating medical conditions, including severe pain, for which individuals may be authorized to use medical marijuana. The medical marijuana card is registered with the state to protect the individual from criminal prosecution for possession of a controlled substance (Oregon Department of Human Services, 2010). However, in this case, the participant was in possession of marijuana plants without the medical marijuana card. The participant asked for help moving her marijuana plants to avoid detection as a form of “accommodation.” Given the illegality of the situation this assistance was not provided. A second RISE example occurred when a participant was transitioning from a cane to a wheelchair at the same time she was trying to leave a domestic violence situation. Rather than go to a healthcare provider, she asked a peer co-facilitator to help her. The co-facilitator wanted to help the participant, so she assisted the participant in seeking shelter at a local hotel and also obtained and delivered a used wheelchair. The participant decided against keeping the wheelchair, however, and left it in the hotel lobby. The co-investigator discovered this when she went to visit the participant and found the wheelchair with a sign on it with the co-investigator's name indicating that she was responsible to remove it from the premises.
The crux of the issue of providing “unreasonable” accommodation to participants who are friends or acquaintances again can be traced to tensions inherent in CBPR principles and experimental design. Because providing accommodation is a central value of disability culture, flexibility in providing accommodation would seem to be appropriate for a CBPR project in the disability community (Northway, 2010). In contrast, concerns about contamination and confounding variables generally precludes over involvement with participants when using an experimental design. Frequent and ongoing frank discussions about the trade-offs and difficulties involved in negotiating boundaries between the role of community member as friend, and community member as researcher, and the levels of accommodation the team is willing and able to provide to participants are critical to addressing this issue (Figure 4).
Figure 4.
Key Points Regarding Accommodation Challenges
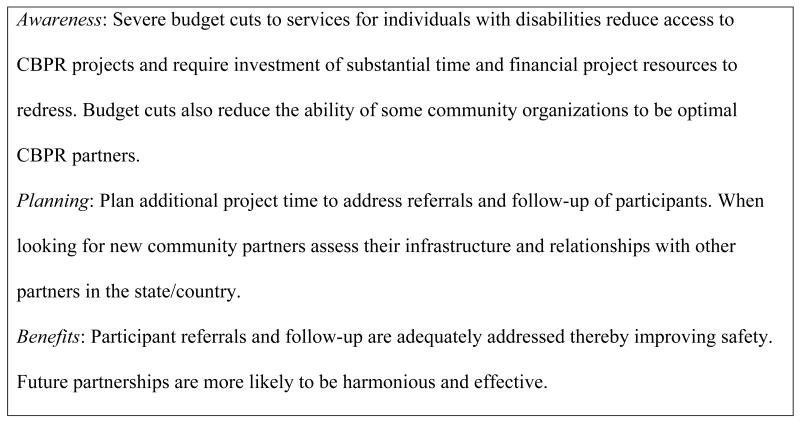
Funding for Disability Community Organizations
The fifth and final challenge we discuss focuses on community-level barriers to full inclusion of persons with disabilities in research. Federal and state funding for disability service agencies and other services that benefit individuals with disabilities has been cut drastically over the past several years with varying effects on different communities. According to the recently released Center on Budget and Policy Priorities report (Johnson, Oliff, & Williams, 2010) beginning in 2008, 31 states have cut public health funding and 29 have cut services for the elderly and disabled. Moreover, sizeable budget gaps are likely to continue to occur for several years. In states and communities where the cuts have been most drastic, barriers to participation in CBPR projects arise.
The first set of barriers occurs when budget cuts create loss of essential services for individuals with disabilities in a particular community. This creates service gaps, reducing referral options and requiring more team follow-up concerning domestic violence and other safety-related concerns. Lack of available services also affects vital systems such as transportation. These community level barriers directly affect community members' ability to participate in CBPR.
A second set of barriers is evident at the agency level. When CIL budgets are cut, tangible effects on employee pay and benefits, employee performance, and turnover can be seen. Administrative staff who are responsible for managing grants and contracts, as well as programs and services are affected, and the quality of their work is often compromised. These combined effects make affected CILs less desirable as research partners, thus limiting their opportunity to access CBPR partnerships.
In addition to reducing service quality, budget cuts create competition among state and other community organizations for meager funds. In Oregon this has resulted in closing of some of the smaller state centers and strained relations between some existing centers as well (Oregon State Independent Living Council, 2005, 2006, 2009). This in turn has influenced decisions about which organizations to partner with for the long-term, resulting in potential exclusion of some communities from CBPR.
Once all of these barriers have been considered and CIL partners selected, unforeseen budget cuts can still affect CIL partners' ability to meet contractual agreements. Two examples from our projects include a lack of CIL funds to advance monies to pay for required travel or participant stipends. We worked with grants and contracts staff at the University to see if there were any ways around these problems. Although we were able to make special arrangements to cover travel, we learned that the University does not have a mechanism that would enable community partners to borrow against the grant. Thus, the PI loaned her personal funds to temporarily cover a portion of the stipends to help the team at distant rural sites move past yet another barrier. Without this loan our rural community partner would not have been able to compensate participants using the same standardized remuneration schedule applied to participants at urban intervention sites, thereby introducing potential bias. Given that the PI had very little contact with participants at rural sites and that standard protocols were implemented at all sites regardless of financial status the team believed that this strategy was appropriate.
Being aware and prepared for each of these community-level challenges in the planning stages of a project is important to help all partners make wise decisions related to protocol development, partnership choices, and resource allocation. Because CBPR is also about capacity building, strategies for supporting partners' ability to provide services and manage grants and contracts may also be part of such projects in the disability community. Finally, academic institutions can be helpful by taking more active roles in supporting CBPR projects and community partners by making research infrastructure both accessible and helpful to underfunded community agencies (Block et al., 2006; Figure 5).
Figure 5.
Key Points Regarding Disability Community Agency Funding Challenges
Conclusions
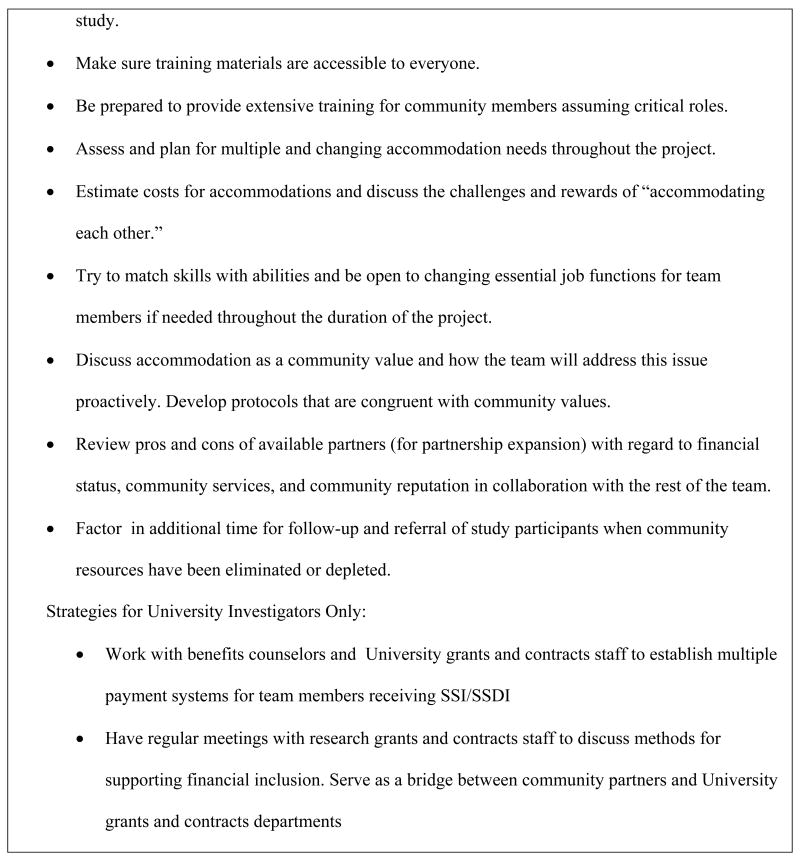
Full inclusion of individuals with disabilities and disability community organizations in research partnerships is key to developing CBPR and other research protocols that reflect the health and social priorities of disability communities. Through our experiences on two experimental CBPR studies, we have learned that there are multiple and quite formidable challenges to achieving full inclusion for individuals with disabilities and disability community organizations. As research partnerships set out to design projects, we recommend starting with an explicit awareness of the potential challenges to full inclusion for individuals with disabilities and for disability community organizations. Additionally, we suggest proactive planning and budgeting for the finances, personnel, and training needed to increase inclusion and decrease barriers for individuals with disabilities. We hope that this paper will help investigators provide evidence to support the need for these disability-related budget items. These efforts of initial planning, along with ongoing evaluation and accommodation, are likely to increase success for CBPR studies by including all the team members without exhausting personnel or financial resources when challenges are encountered during the course of the project.
Figure 6 summarizes the many recommendations embedded in this paper. We suggest using the information in the figure as an inclusion strategy checklist when planning for an experimental CBPR project with a disability community. Although it by no means covers all areas that CBPR researchers are advised to consider, it does provide an important overview of practical realities related to inclusion. Finally, future work is needed to evaluate the effectiveness of these strategies for promoting full inclusion with experimental CBPR projects in disability communities. Cost analysis is also needed to help researchers, community members, and funders make meaningful budget calculations and identify potential areas for budget reductions and efficiencies without sacrificing disability community access to CBPR (Viswanathan, et al., 2004).
Figure 6.
Overview of Strategies for Addressing the Five Challenges
Acknowledgments
This work was funded by the National Institute of Disability and Rehabilitation Research and the National Institute of Mental Health.
Contributor Information
Dena Hassouneh, Email: phillide@ohsu.edu, Oregon Health & Science University, School of Nursing, SN 637, 3455 SW US Veterans Hospital Rd., Portland, Ore. 97239-2941, Phone: 503 494 2714, Fax: 503 494 3878.
Amana Alcala-Moss, Oregon Health & Science University, School of Nursing, Portland, Ore.
E. McNeff, Portland State University, Regional Research Institute, Portland, Ore.
References
- Alcala-Moss A. RISE and Healing Pathways team member interviews: perspectives on CBPR with women with physical disabilities. School of Nursing, Oregon Health & Science University; Portland, Oregon: 2010. Unpublished manuscript. [Google Scholar]
- Americans with Disabilities Act of 1990, As Amended. 2008 Retrieved from http://www.ada.gov/pubs/adastatute08.pdf.
- Block P, Skeels SE, Keys CB. Participatory intervention research with a disability community: A practical guide to practice. International Journal of Disability, Community, & Rehabilitation. 2006;5(1) Retrieved from http://www.ijdcr.ca/VOL05_01_CAN/articles/block.shtml. [Google Scholar]
- Bricher G. Disabled people, health professionals, and the social model of disability: can there be a research relationship? Disability & Society. 2000;15:781–793. [Google Scholar]
- Cheadle A, Senter S, Solomon L, Beery WL, Schwartz PM. A qualitative exploration of alternative strategies for building community health partnerships: Collaboration- versus issue-oriented approaches. Journal of Urban Health. 2005;82:638–652. doi: 10.1093/jurban/jti120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craig P, Dieppe P, Macintyre S, Mitchie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: The new Medical Research Council Guidance. BMJ. 2008;337:a1655. doi: 10.1136/bmj.a1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross D, Fogg L. Clinical trials in the 21st century: The case for participant-centered research. Research in Nursing & Health. 2001;24:530–539. doi: 10.1002/nur.10010. [DOI] [PubMed] [Google Scholar]
- Independent Living Research Utilization. ILRU directory of CILs and SILCs. 2011;33 Retrieved from http://www.ilru.org/html/publications/directory/index.html. [Google Scholar]
- Israel BA, Schulz AJ, Parker EA, Becker AB. Review of community-based research: Assessing partnership approaches to improve public health. Annual Review of Public Health. 1998;19:173–202. doi: 10.1146/annurev.publhealth.19.1.173. [DOI] [PubMed] [Google Scholar]
- Johnson N, Orliff P, Williams E. An update on state budget cuts: At least 46 states have imposed cuts that hurt vulnerable residents and the economy. Center on Budget and Policy Priorities. 2011 Retrieved from http://www.cbpp.org/cms/?fa=view&id=1214.
- Kliewer C, Biklen D. Democratizing disability inquiry. Journal of Disability Policy Studies. 2000;10:186–206. [Google Scholar]
- Krahn GL, Putnam M, Drum CE, Powers L. Disabilities and health: Toward a national agenda for research. Journal of Disability Policy Studies. 2006;17:18–27. [Google Scholar]
- Lasker RD, Weiss ES, Miller R. Partnership synergy: A practical framework for studying and strengthening the collaborative advantage. Milbank Quarterly. 2001;72:179–205. doi: 10.1111/1468-0009.00203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lord J, Church K. Beyond “partnership shock:” Getting to ‘yes’, living with ‘no’. Canadian Journal of Rehabilitation. 1998;12:113–121. [Google Scholar]
- Minkler M. Community-based research partnerships: Challenges and opportunities. Journal of Urban Health. 2005;82(2;Supp 2):ii3–ii12. doi: 10.1093/jurban/jti034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minkler M, Hammel J, Gill CJ, Magasi S, Vásquez VB, Bristo M, Coleman D. Community-based participatory research in disability and long-term care policy: A case study. Journal of Disability Policy Studies. 2008;19:114–126. [Google Scholar]
- Mmatli TO. Translating disability-related research into evidence-based advocacy: The role of people with disabilities. Disability and Rehabilitation. 2009;31:14–22. doi: 10.1080/09638280802280387. [DOI] [PubMed] [Google Scholar]
- Northway R. Participatory research part 2: practical considerations. International Journal of Therapy and Rehabilitation. 2010;17:226–231. [Google Scholar]
- Ochocka J, Janzen R, Nelson G. Sharing power and knowledge: Professional and mental health consumer/survivor researchers working together in a participatory action research project. Psychiatric Rehabilitation Journal. 2002;25:379–387. doi: 10.1037/h0094999. [DOI] [PubMed] [Google Scholar]
- Oregon Department of Human Services. Description of the Oregon Medical Marijuana Act. 2010 Retrieved from http://arcweb.sos.state.or.us/rules/OARs_300/OAR_333/333_008.html.
- Oregon State Independent Living Council. SILC 2004-2005 Annual Report. 2005 Retrieved from http://www.oregon.gov/DHS/vr/silc/annual-rep2005.pdf.
- Oregon State Independent Living Council. SILC 2006 Annual Report. 2006 Retrieved from http://www.oregon.gov/DHS/vr/silc/2006_annualreport.pdf.
- Oregon State Independent Living Council. SILC 2008-2009 Annual Report. 2009 Retrieved from http://www.oregon.gov/DHS/vr/silc/2008-2009_annualreport.pdf.
- Preference Collaborative Review Group. Patients' preferences within randomized trials: Systematic review and patient level meta-analysis. BMJ. 2008;337:a1864. doi: 10.1136/bmj.a1864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Raudenbush SW, Bryk AS, Congdon R. Hierarchical linear and nonlinear modeling. Lincolnwood IL: SSI; 2004. [Google Scholar]
- Ridgeway P, McDiarmid D, Davidson L, Bayes J, Ratzlaff S. Pathways to Recovery: A strengths based recovery self-help workbook. Lawrence, KS: Supported Education Group University of Kansas; 2002. [Google Scholar]
- Viswanathan M, Ammerman A, Eng E, Gartlehner G, Lohr KN, Griffith D, et al. Whitener L. Community-based participatory research: Assessing the evidence. Evidence report/technology assessment No. 99: AHRQ Publication 04-E022-2. Rockville, MD: 2004. [PMC free article] [PubMed] [Google Scholar]
- White GW, Nary DE, Froehlick AK. Consumers as collaborators in research and action. In: Keys CB, Dowrick PW, editors. People with disabilities: Empowerment and community action. New York: Haworth Press; 2001. pp. 15–34. [Google Scholar]
- Zimmerman S, Tilly J, Cohen L, Love K. A manual for community-based participatory research: Using research to improve practice and inform policy in assisted living. n.d. Retrieved from http://www.shepscenter.unc.edu/research_programs/aging/publications/CEAL-UNC%20Manual%20for%20Community-Based%20Participatory%20Research-1.pdf.
- Zinbarg RE, Mashal NM, Black DA, Fluckiger C. The future and promise of cognitive behavioral therapy: A commentary. Psychiatric Clinics of North America. 2010;33:711–727. doi: 10.1016/j.psc.2010.04.003. [DOI] [PubMed] [Google Scholar]