Abstract
Objective: To evaluate the prevalence of primary iris and/or ciliary body cysts in eyes with shallow anterior chamber and their effect on the narrowing of the anterior chamber angle. Methods: Among the general physical check-up population, subjects with shallow anterior chambers, as judged by van Herick technique, were recruited for further investigation. Ultrasound biomicroscope (UBM) was used to detect and measure the cysts located in the iris and/or ciliary body, the anterior chamber depth (ACD), the angle opening distance at 500 μm (AOD500), and the trabecular-iris angle (TIA). A-scan ultrasonography was used to measure the ocular biometry, including lens thickness, axial length, lens/axial length factor (LAF), and relative lens position (RLP). The effect of the cyst on narrowing the corresponding anterior chamber angle and the entire angle was evaluated by the UBM images, ocular biometry, and gonioscopic grading. The eye with unilateral cyst was compared with the eye without the cyst for further analysis. Results: Among the 727 subjects with shallow anterior chamber, primary iris and ciliary body cysts were detected in 250 (34.4%) patients; among them 96 (38.4%) patients showed unilateral single cyst, 21 (8.4%) patients had unilateral double cysts, and 42 (16.8%) patients manifested unilateral multiple and multi-quadrants cysts. Plateau iris configuration was found in 140 of 361 (38.8%) eyes with cysts. The mean size of total cysts was (0.6547±0.2319) mm. In evaluation of the effect of the cyst size and location on narrowing the corresponding angle to their position, the proportion of the cysts causing corresponding angle narrowing or closure among the cysts larger than 0.8 mm (113/121, 93.4%) was found to be significantly higher than that of the cysts smaller than 0.8 mm (373/801, 46.6%), and a significant higher proportion was also found in the cysts located at iridociliary sulcus (354/437, 81.0%) than in that at the pars plicata (131/484, 27.1%). In evaluating the effect of the cyst on the entire anterior chamber angle, the eyes with multiple and multi-quadrants cysts manifested significant narrowing of the entire anterior chamber angle as compared with the eyes without cysts, based on the data analysis in comparison of TIA, AOD500, and gonioscopic grading evaluation. The unilateral single or double cysts in the eyes had no significant effect on narrowing of anterior chamber angle as compared with eyes without cysts. The iris and/or ciliary body cysts did not seem to affect the axial length, ACD, lens thickness, RLP, LAF. Conclusions: The prevalence of primary iris and ciliary body cyst was 34.4% in the subjects with shallow anterior chamber. The cysts larger than 0.8 mm, locating at iridociliary sulcus, or multiple and extensive cysts were inclined to cause the angle narrowing or closure.
Keywords: Iris and ciliary body cyst, Ultrasound biomicroscope, Shallow anterior chamber
1. Introduction
Primary iris and ciliary body cysts are congenital cystic lesions, which occur in the iris or the ciliary body with a normal localization at the iridociliary junction or pars plicata (Lois et al., 1998). Histological studies showed the cysts to be fluid-filled cavities with an epithelial cell wall (Shields et al., 1984). It is difficult to detect cysts by slit-lamp biomicroscopy or gonioscopy due to their hidden location. Ultrasound biomicroscopy (UBM) plays an important role in examining the anterior segment anatomy, including retro-iridian structures and ciliary processes, owing to its high resolution and noninvasive nature (Conway et al., 2005; Gündüz et al., 2007; Ang et al., 2008). Therefore, it has been used widely to evaluate the cysts and other lesions (Kunimatsu et al., 1999; Marigo et al., 1999; McWhae et al., 2007; Minavi and Holdeman, 2007).
The width of the anterior chamber angle depends on several factors including the level of iris insertion, the profile of peripheral iris, and the location of ciliary body (He et al., 2006; Dorairaj et al., 2007). The cysts at the iridociliary junction or pars plicata identified by UBM can lead to anterior displacement of the iris root or anterior rotation of the ciliary body, accordingly cause narrow angle and even angle-closure glaucoma (Kuchenbecker et al., 2000; Badlani et al., 2003; Ritch et al., 2003; Crowston et al., 2005; Xiao et al., 2006; Dada et al., 2011). However, to our best knowledge, there have been no reports addressing the clinical relevance between cysts and shallow anterior chamber. Ocular biometric parameters such as anterior chamber depth (ACD), lens thickness, and axial length have rarely been investigated in the previous case reports about patients diagnosed with angle-closure glaucoma secondary to iris cysts. In the present study, we included 727 subjects with shallow anterior chambers in routine health check-ups and observed the prevalence of primary iris and ciliary body cysts in these subjects. By investigating the ocular biometric parameters in bilateral eyes of patients, our study indicates a possible involvement of cysts in the development of angle-closure glaucoma.
2. Subjects and methods
2.1. Subjects
This study was approved by the Ethics Committee of the Sir Run Run Shaw Hospital, School of Medicine, Zhejiang University, China and was performed according to the tenets of the World Medical Association’s Declaration of Helsinki. Informed consent was obtained from all subjects. From December 2007 to May 2008, a total of 10 170 healthy Chinese patients visited our health promotion center for regular health check-ups. Among them, 727 subjects, who were found to have shallow anterior chamber and wanted a further evaluation, were enrolled in this study. Any individuals with the history of intraocular surgery or penetrating trauma, anterior segment laser treatment, or glaucoma and uveitis were excluded. The diagnosis of shallow anterior chamber was made based on the peripheral ACD equal to or shallower than a half of the peripheral corneal thickness according to the method of van Herick et al. (1969). Bilateral eyes of 727 patients (285 males and 442 females) with a mean age of (52.5±10.5) years were subjected to regular ocular examination and detailed evaluations with A-scan ultrasonography, gonioscopy, and UBM scans.
2.2. Gonioscopy
All subjects were examined with Goldmann 1-mirror gonioscopy (YZ-214, Vision 6, China) in the dark by a single examiner masked to UBM findings. The circumference of the anterior chamber angle was divided into eight sectors (Fig. 1), and angle widths of all sectors were graded using the Scheie grading system.
Fig. 1.
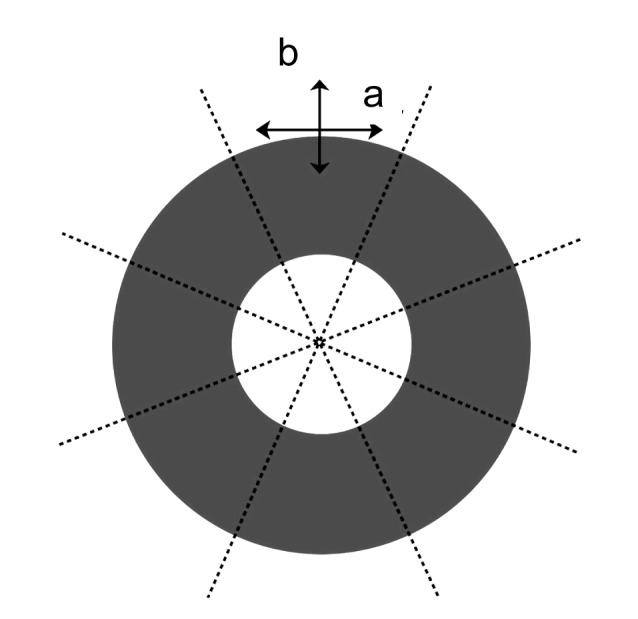
Division of circumference of the ciliary body in each eye into eight sectors
In ultrasound biomicroscopy (UBM), each sector was scanned perpendicularly in transverse (a) and radial (b) positions
2.3. A-scan ultrasonography
Parameters were measured with A-mode ultrasound (P-4000, Sonomed, USA) with the following values recorded for each eye: (1) lens thickness; (2) axial length as the sum of the anterior chamber, lens thickness, and vitreous length; (3) lens/axial length factor (LAF) as the lens thickness to axial length ratio multiplied by 10; and (4) relative lens position (RLP) as the relative position of the center of the lens determined by adding the ACD to half the lens thickness and then dividing the sum by the axial length. The RLP was multiplied by 10 (Marchini et al., 1998).
2.4. Ultrasound biomicroscopy
The examinations were performed using a high-resolution UBM (SW-3200, SUOER, China) with a 68-MHz transducer-probe allowing 5 mm×5 mm tissue penetration and approximately 50-mm resolution. The circumference of the ciliary body in each eye was divided into eight sectors for a complete examination (Fig. 1). All procedures were performed by the same experienced examiner in constant ambient lighting conditions.
Several parameters were measured with UBM with values recorded for each eye. Any cysts detected in UBM were assessed for size (average of the horizontal and vertical diameters in radial position), location, and clock position. ACD was measured from the endothelial surface of the cornea to the anterior surface of the lens. Trabecular-iris angle (TIA) was measured with the apex in the iris recess and the arms of the angle passing through a point on the trabecular meshwork at 500 mm from the scleral spur and the point on the iris perpendicularly opposite. Angle opening distance at 500 μm (AOD500) was the distance between the posterior cornea surface and the anterior iris surface measured on a line perpendicular to the trabecular meshwork at 500 mm from the scleral spur (Shukla et al., 2008).
The corresponding anterior chamber angle of the cyst, which is defined as the anterior chamber angle with cyst in the largest vertical diameter on UBM image, was further assessed by comparing AOD500 and TIA with those in the neighboring horizontal and vertical o’clock without cyst. If the AOD500 and TIA were both smaller than the averages, then it is recorded that the corresponding anterior chamber angle narrowed or closed (Figs. 2 and 3). Anterior chamber angle is considered to be closed on UBM image if any contact between the iris and angle wall anterior to the scleral spur is noted. Plateau iris configuration was diagnosed by the presence of a flat or concave iris plane, a sharp angle turn of the posterior iris root before inserting into ciliary body, anteriorly displaced ciliary processes, and a normal central ACD of (3.0±1.0) mm by UBM means (Fig. 4). At least two quadrants had to fulfill the above criteria for an eye to be defined as plateau iris (Stieger et al., 2007).
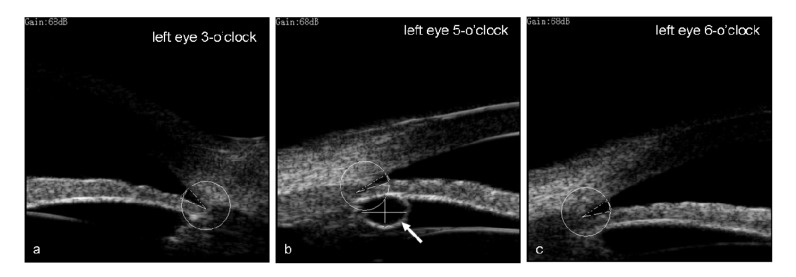
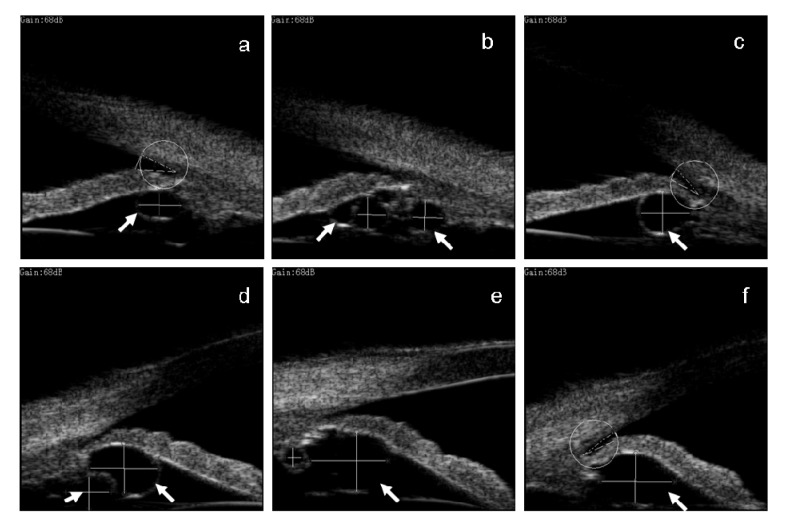
Fig. 2.
Ultrasound biomicroscopy (UBM) images of the left eye 3 (a), 5 (b), and 6 (c) o’clock radial positions in a 47-year-old patient with one cyst (arrow)
AOD500 and TIA: (a) 0.2786 mm and 27°; (b) 0.2104 mm and 14°; (c) 0.2587 mm and 22°. Compared with (a), in (c) the AOD500 and TIA were all smaller than the averages, so it was recorded that the corresponding anterior chamber angle narrowed
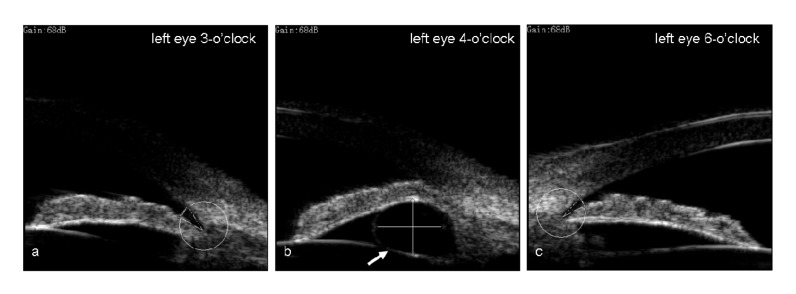
Fig. 3.
Ultrasound biomicroscopy (UBM) images of the left eye 3 (a), 4 (b), and 6 (c) o’clock radial positions in a 41-year-old patient with one cyst (arrow)
Compared to (c), the angle in (b) was closed, and thus it was recorded that the corresponding anterior chamber angle closed
Fig. 4.
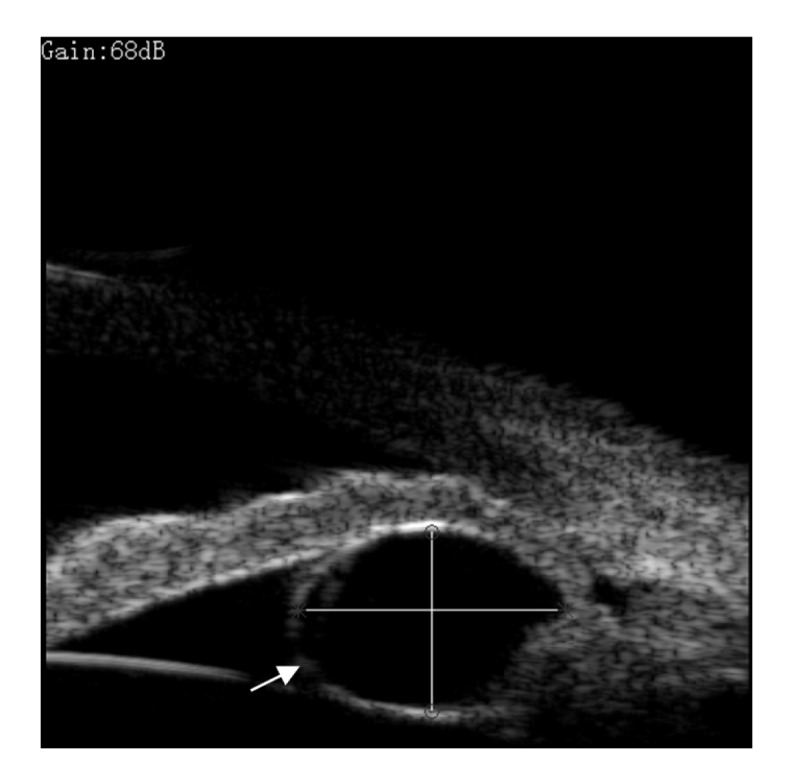
A cyst (arrow) characterized as round or ovoid, solitary or multiple, with a thin and hyperechogenic wall and a sonolucent interior
The local angle of the cyst showed plateau iris configuration
Cysts are categorized according to their mean size (average of the horizontal and vertical diameters in radial position in UBM). Small cysts are defined as cyst ≤0.4 mm, middle cysts are defined as ≤0.8 mm but >0.4 mm, large cysts are defined as >0.8 mm but ≤1.3 mm, and extra large cysts are defined as >1.3 mm. According to the distribution of quadrant of cysts detected in the iris or ciliary body, a single quadrant cyst was defined as a distribution of the cysts equal to or less than one quadrant, multi-quadrant cysts were defined as cysts in more than one quadrant. According to the number of cysts found in iris or ciliary body, a single cyst was defined as only one cyst found within the iris or/and ciliary, double cysts were defined as 2 cysts, and multiple cysts were defined as ≥3 cysts.
2.5. Statistical analysis
All data were entered into a computerized database. Parametric and nonparametric tests were used to compare continuous variables, according to data distribution. For parametric data, differences in mean values of ocular biometric parametric data between study groups were examined using a paired Student’s t-test. For nonparametric data, differences were examined using a Wilcoxon Signed Ranks test. The chi-square test was used to compare categorical data. A P value of less than 0.05 was considered statistically significant.
3. Results
All cysts observed by using UBM were categorized as round or ovoid, solitary or multiple, with a thin and hyperechogenic wall and a sonolucent interior (Fig. 4). The diagnosis of primary iris or ciliary body cysts was made according to the patients’ history and clinical manifestation, after excluding other possible etiological factors that can cause secondary cysts.
Among the 727 subjects with shallow anterior chamber, primary iris and ciliary body cysts were detected in 250 (34.4%) patients (164 eyes in 109 males, 197 eyes in 141 females) by UBM in this study. Plateau iris configuration was found in 140 of 361 (38.8%) eyes with cysts.
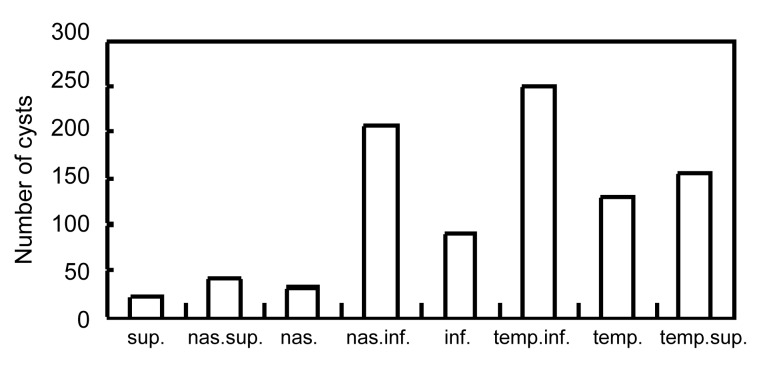
Among all the patients with cysts, there were 96 (38.4%) patients with unilateral single cyst, 21 (8.4%) patients with unilateral double cysts, 42 (16.8%) patients with unilateral multiple and multi-quadrants cysts. A total of 922 cysts (average 2.6 cysts per eye, range 1 to 18 cysts) were observed in all patients, 47.4% of the cysts located at the iridociliary sulcus; 52.5% at pars plicata, and 0.1% at midzonal iris. There was a characteristic distribution pattern, with cysts found predominantly in the inferior and temporal quadrants (Fig. 5).
Fig. 5.
Locations of 922 cysts in 361 eyes with shallow anterior chamber
The number of cysts exceeds the number of eyes because many eyes had multiple cysts in various sectors. nas.: nasal; sup.: superior; inf.: inferior; temp.: temporal
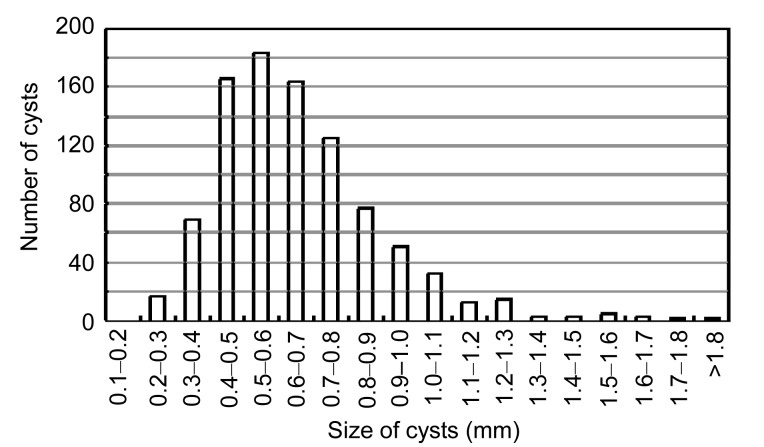
The mean size of cysts was (0.6547±0.2319) mm (range 0.2402 to 2.1609 mm) (Fig. 6). There were 85 eyes with small cysts (9.22%), 716 eyes with middle cysts (77.66%), 109 eyes with large cysts (11.82%), and 12 eyes with the extra large cyst (1.30%). There were 172 eyes with single cyst (47.7%), 85 eyes with double cysts (23.5%), and 104 eyes with multiple cysts (28.8%). There were 224 eyes with single quadrant cyst (62.0%), and 137 eyes with multi-quadrants cysts (38.0%). Fig. 7 showed a 31-year-old patient in her left eye with multiple and multi-quadrant cysts.
Fig. 6.
Number distribution of the size of cysts
The mean size of cysts is (0.6547±0.2319) mm
Fig. 7.
Ultrasound biomicroscopy (UBM) images of the left eye 1 (a), 2 (b), 3 (c), 5 (d), 7 (e), and 9 (f) o’clock radial positions in a 31-year-old patient with multiple and multi-quadrant cysts (arrows)
In evaluation of the effects of the cyst size and location on narrowing the corresponding angle, the proportion of the cysts causing corresponding angle narrowing or closure among the cysts larger than 0.8 mm (113/121, 93.4%) was significantly higher than that in the cysts smaller than 0.8 mm (373/801, 46.6%; P=0.000), and a significantly higher proportion was also found in the cysts located at iridociliary sulcus (354/437, 81.0%) than in that at the pars plicata (131/484, 27.1%, P=0.000). Significant differences were found among the proportion of the cysts caused narrowing or closure of the corresponding angles to their position in the small, middle, large and extra large cysts (χ 2=111.0, P=0.000; Table 1). It means that the cysts larger than 0.8 mm or locating at iridociliary sulcus are inclined to cause narrowing or closure of the corresponding angles.
Table 1.
Percentage distributions of the small, middle, large, and extra large cysts which caused or did not cause the corresponding angle narrowing or closure
| Angle narrowing or closure | Number of cysts |
|||
| Small cysts* | Middle cysts* | Large cysts* | Extra large cysts | |
| Positive | 16 (18.8%) | 357 (49.9%) | 101 (92.7%) | 12 (100%) |
| Negative | 69 (81.2%) | 359 (50.1%) | 8 (7.3%) | 0 (0%) |
| Total | 85 | 716 | 109 | 12 |
Positive: cause the corresponding angle narrowing or closure; Negative: not cause the corresponding angle narrowing or closure
χ 2=111.0, P=0.000
In evaluation of the mechanism of the cyst on narrowing the local angle, 242 angles showed plateau iris configuration in the 486 narrowed or closed angles with the cysts (49.8%), which was significantly higher than that in the non-narrowed or closed angles with cysts (20/436, 4.6%; P=0.000).
In evaluating the effect of the cyst on the entire anterior chamber angle, the eyes with multiple and multi-quadrants cysts manifested significant narrowing of the entire anterior chamber angle as compared with the eyes without cysts, based on the data analysis in comparison of TIA, AOD500, and gonioscopic grading evaluation (Table 2; P=0.001, P=0.002, P=0.000, respectively). The unilateral single or double cysts in the eyes had no significant effect of narrowing of anterior chamber angle as compared with eyes without cysts (P>0.05). The iris and/or ciliary body cysts did not seem to affect the axial length, ACD, lens thickness, RLP, and LAF (Table 3; P>0.05).
Table 2.
Comparing the TIA, AOD500, gonioscopic grading within bilateral eyes of patients with unilateral single or double cysts or with unilateral multiple and multi-quadrants cysts
| Group | Eyes and P-value | TIA (°) | AOD500 (mm) | Gonioscopic grading* |
| I | Eyes with cysts | 15.68±7.03 | 0.18±0.07 | 1.34±0.76 |
| Fellow eyes | 16.52±6.69 | 0.19±0.07 | 1.28±0.74 | |
| P-value# | 0.08 | 0.06 | 0.38 | |
| II | Eyes with cysts | 15.63±5.72 | 0.18±0.07 | 1.33±0.88 |
| Fellow eyes | 17.29±7.29 | 0.19±0.07 | 1.19±0.85 | |
| P-value# | 0.13 | 0.09 | 0.06 | |
| III | Eyes with more cysts | 15.30±6.62 | 0.19±0.07 | 1.26±0.81 |
| Fellow eyes | 18.08±6.96 | 0.22±0.08 | 1.02±0.70 | |
| P-value# | 0.001 | 0.002 | 0.000 |
Values are presented as mean±standard deviation. I: the patients with unilateral single cyst (n=96); II: the patients with unilateral double cysts (n=21); III: the patients with unilateral multiple and multi-quadrants cysts (n=42). TIA: trabecular-iris angle; AOD500 (mm): angle opening distance at 500 μm
Using the Scheie grading system
Wilcoxon Signed Ranks test, P-value (bilateral)
Table 3.
Comparing the ocular biometric parameters within bilateral eyes of patients with unilateral single or double cysts or with unilateral multiple and multi-quadrants cysts
| Group | Eyes and P-value | Axial length (mm) | ACD (mm) | Lens thickness (mm) | RLP | LAF |
| I | Eyes with cysts | 22.67±0.78 | 2.52±0.23 | 4.27±0.30 | 2.30±0.09 | 1.89±0.15 |
| Fellow eyes | 22.63±0.72 | 2.51±0.23 | 4.27±0.35 | 2.30±0.10 | 1.89±0.17 | |
| P-value# | 0.26 | 0.44 | 0.94 | 0.96 | 0.62 | |
| II | Eyes with cysts | 22.67±0.86 | 2.46±0.33 | 4.23±0.31 | 2.28±0.07 | 1.87±0.18 |
| Fellow eyes | 22.60±1.02 | 2.49±0.35 | 4.19±0.37 | 2.28±0.11 | 1.86±0.20 | |
| P-value# | 0.44 | 0.16 | 0.28 | 0.92 | 0.54 | |
| III | Eyes with more cysts | 23.07±0.95 | 2.56±0.28 | 4.16±0.26 | 2.24±0.13 | 1.81±0.13 |
| Fellow eyes | 23.01±0.98 | 2.56±0.27 | 4.15±0.29 | 2.26±0.12 | 1.82±0.15 | |
| P-value# | 0.25 | 0.67 | 0.73 | 0.23 | 0.91 |
Value are presented as mean±standard deviation. I: the patients with unilateral single cyst (n=96); II: the patients with unilateral double cysts (n=21); III: the patients with unilateral multiple and multi-quadrants cysts (n=42). ACD: anterior chamber depth in UBM; RLP: relative lens position; LAF: lens/axial length factor
Paired t-test
4. Discussion
Most of primary iris and ciliary body cysts are located at the iridociliary sulcus and pars plicata. They are seldom detected with slit-lamp biomicroscopy, gonioscopy (Lois et al., 1998). UBM is a useful noninvasive tool to examine the anterior segment with a high revolution, allowing us to visualize retro-iridian structures and ciliary processes (Conway et al., 2005; Gündüz et al., 2007; Ang et al., 2008). In this study, we used this technique to identify cystic lesions in the iris and ciliary body, and to analyze its association with the anterior chamber angle. Our study found that almost all cysts are located at the iridociliary sulcus or pars plicata and are predominantly distributed in the inferior and temporal quadrants. These results are well consistent with the finding of Kunimatsu et al. (1999). However, the prevalence of primary iris or ciliary body cysts in our subjects was 34.4%, lower than 54.3% found by Kunimatsu et al. (1999) (UBM procedure was similar with ours). This discrepancy may be explained by several reasons. Firstly, older patients in our study may be the main factor for the discrepancy; the mean age of our patients was (52.5±10.5) years with a percentage of 8.7% for age range as 25 to 40 years, but the mean age of the patients in Kunimatsu et al. (1999)’s study was (45.2±20.1) years, and patients aged 15 to 40 years accounted for 44.83%. Secondly, we included the patients with shallow anterior chamber in routine health examination in our department, whereas Kunimatsu et al. (1999) enrolled a normal population.
Our results demonstrate that single or double cysts have no significant narrowing effect on the entire anterior chamber angle in Chinese people with shallow anterior chamber, but multiple and multi-quadrant cysts may have a significant effect and further aggravate its narrowing. The reasons for this may be the special anatomic characteristics of iris and ciliary body around the angle. The iris is composed mainly of loose connective tissue and is thinnest at its root where it is attached loosely to the ciliary spur. Furthermore, iridociliary sulcus and pars plicata are against the iris root and the ciliary zones. As a result, the cysts in iridociliary sulcus or pars plicata are prone to push the weak root of the iris and ciliary zones. In some cases, the cysts can cause anterior rotation of the ciliary body and pseudoplateau configuration (Azuara-Blanco et al., 1996; Badlani et al., 2003; Ritch et al., 2003; Crowston et al., 2005; Shukla et al., 2008) by ‘self space occupying’ or ‘posterior-push’ mechanism. Accordingly, the corresponding peripheral anterior chamber angle is narrowed or closed. That is to say, the larger the cyst, the stronger the strength of ‘self space occupying’ or ‘posterior-push’, the easier the corresponding angle narrowing or closure occur. In our results, the mean diameter of the cysts was only (0.6547±0.2319) mm and the largest one was 2.1609 mm. Due to about 36 mm circumference of the total anterior chamber angle, the single cyst may contribute to the little effect of ‘self space occupying’ or ‘posterior-push’. However, large, multiple, or multi-quadrant cysts may narrow the peripheral anterior chamber angle.
It has been reported that the most important biometric feature predisposing to angle closure is the shallow anterior chamber (Marchini et al., 1998). The depth of the anterior chamber mainly depends on the thickness and position of the lens inside the eye. These parameters increase with aging. With aging, the lens increases in thickness and moves forward. Accordingly, the lens thickness to axial length factor increases (Lim et al., 2006; Yan et al., 2010). Furthermore, to our best knowledge, almost all patients with angle-closure glaucoma secondary to iris cysts in previous case reports showed shallow anterior chambers on UBM images. Whether angle-closure glaucoma is inclined to occur in older patients who have shallow anterior chamber coexisting with multiple and multi-quadrant cysts remains unknown. A population-based design including the patients with deep anterior chambers and long term follow-up will be necessary.
In conclusion, the prevalence of primary iris and ciliary body cyst was 34.4% in the subjects of the eyes with shallow anterior chamber among the population receiving regular health check-up. The cysts larger than 0.8 mm, locating at iridociliary sulcus, or multiple and extensive cysts were inclined to cause the angle narrowing or closure.
Footnotes
Project (No. 2012KYA107) supported by the Health Bureau of Zhejiang Province, China
References
- 1.Ang GS, Bochmann F, Azuara-Blanco A. Argon laser peripheral iridoplasty for plateau iris associated with iridociliary cysts: a case report. Cases J. 2008;1(1):368. doi: 10.1186/1757-1626-1-368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Azuara-Blanco A, Spaeth GL, Araujo SV, Augsburger JJ, Terebuh AK. Plateau iris syndrome associated with multiple ciliary body cysts. Report of three cases. Arch Ophthalmol. 1996;114(6):666–668. doi: 10.1001/archopht.1996.01100130658004. [DOI] [PubMed] [Google Scholar]
- 3.Badlani VK, Quinones R, Wilensky JT, Hawkins A, Edward DP. Angle-closure glaucoma in teenagers. J Glaucoma. 2003;12(3):198–203. doi: 10.1097/00061198-200306000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Conway RM, Chew T, Golchet P, Desai K, Lin S, O′Brien J. Ultrasound biomicroscopy: role in diagnosis and for anterior segment tumours management in 130 consecutive patients evaluated. Br J Opthalmol. 2005;89(8):950–955. doi: 10.1136/bjo.2004.059535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Crowston JG, Medeiros FA, Mosaed S, Weinreb RN. Argon laser iridoplasty in the treatment of plateau-like iris configuration as result of numerous ciliary body cysts. Am J Ophthalmol. 2005;139(2):381–383. doi: 10.1016/j.ajo.2004.08.027. [DOI] [PubMed] [Google Scholar]
- 6.Dada T, Gadia R, Sharma A, Ichhpujani P, Bali SJ, Bhartiya S, Panda A. Ultrasound biomicroscopy in glaucoma. Surv Ophthalmol. 2011;56(5):433–450. doi: 10.1016/j.survophthal.2011.04.004. [DOI] [PubMed] [Google Scholar]
- 7.Dorairaj SK, Tello C, Liebmann JM, Ritch R. Narrow angles and angle closure: anatomic reasons for earlier closure of the superior portion of the iridocorneal angle. Arch Ophthalmol. 2007;125(6):734–739. doi: 10.1001/archopht.125.6.734. [DOI] [PubMed] [Google Scholar]
- 8.Gündüz K, Hoşal BM, Zilelioğlu G, Günalp I. The use of ultrasound biomicroscopy in the evaluation of anterior segment tumors and simulating conditions. Ophthalmologica. 2007;221(5):305–312. doi: 10.1159/000104760. [DOI] [PubMed] [Google Scholar]
- 9.He M, Foster PJ, Ge J, Huang W, Wang D, Friedman DS, Khaw PT. Gonioscopy in adult Chinese: the Liwan Eye Study. Invest Ophthalmol Vis Sci. 2006;47(11):4772–4779. doi: 10.1167/iovs.06-0309. [DOI] [PubMed] [Google Scholar]
- 10.Kuchenbecker J, Motschmann M, Klaus Schmitz K. Laser iridocystotomy for bilateral acute angle-closure glaucoma secondary to iris cysts. Am J Ophthalmol. 2000;129(3):391–393. doi: 10.1016/S0002-9394(99)00392-X. [DOI] [PubMed] [Google Scholar]
- 11.Kunimatsu S, Araie M, Ohara K, Behrens-Baumann W. Ultrasound biomicroscopy of ciliary body cysts. Am J Ophthalmol. 1999;127(1):48–55. doi: 10.1016/S0002-9394(98)00308-0. [DOI] [PubMed] [Google Scholar]
- 12.Lim MC, Lim LS, Gazzard G, Husain R, Chan YH, Seah SK, Aung T. Lens opacity, thickness, and position in subjects with acute primary angle closure. J Glaucoma. 2006;15(3):260–263. doi: 10.1097/01.ijg.0000212212.10395.76. [DOI] [PubMed] [Google Scholar]
- 13.Lois N, Shields CL, Shields JA, Mercado G. Primary cysts of the iris pigment epithelium. Clinical features and natural course in 234 patients. Ophthalmology. 1998;105(10):1879–1885. doi: 10.1016/S0161-6420(98)91034-X. [DOI] [PubMed] [Google Scholar]
- 14.Marchini G, Pagliarusco A, Toscano A, Tosi R, Brunelli C, Bonomi L. Ultrasound biomicroscopic and conventional ultrasonographic study of ocular dimensions in primary angle-closure glaucoma. Ophthalmology. 1998;105(11):2091–2098. doi: 10.1016/S0161-6420(98)91132-0. [DOI] [PubMed] [Google Scholar]
- 15.Marigo FA, Esaki K, Finger PT, Ishikawa H, Greenfield DS, Liebmann JM, Ritch R. Differential diagnosis of anterior segment cysts by ultrasound biomicroscopy. Ophthalmology. 1999;106(11):2131–2135. doi: 10.1016/S0161-6420(99)90495-5. [DOI] [PubMed] [Google Scholar]
- 16.McWhae JA, Rinke M, Crichton AC. Multiple bilateral iridociliary cysts: ultrasound biomicroscopy and clinical characteristics. Can J Ophthalmol. 2007;42(2):268–271. doi: 10.3129/canjophthalmol.i07-017. [DOI] [PubMed] [Google Scholar]
- 17.Minavi AZ, Holdeman NR. Peripheral pigmentary iris cyst: evaluation and differential diagnosis. Clin Exp Optom. 2007;90(1):49–52. doi: 10.1111/j.1444-0938.2006.00087.x. [DOI] [PubMed] [Google Scholar]
- 18.Ritch R, Chang BM, Liebmann JM. Angle closure in younger patients. Ophthalmology. 2003;110(10):1880–1889. doi: 10.1016/S0161-6420(03)00563-3. [DOI] [PubMed] [Google Scholar]
- 19.Shields JA, Kline MW, Augsburger JJ. Primary iris cysts: a review of the literature and report of 62 cases. Br J Ophthalmol. 1984;68(3):152–156. doi: 10.1136/bjo.68.3.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shukla S, Damji KF, Harasymowycz P, Chialant D, Kent JS, Chevrier R, Buhrmann R, Marshall D, Pan Y, Hodge W. Clinical features distinguishing angle closure from pseudoplateau versus plateau iris. Br J Ophthalmol. 2008;92(3):340–344. doi: 10.1136/bjo.2007.114876. [DOI] [PubMed] [Google Scholar]
- 21.Stieger R, Kniestedt C, Sutter F, Bachmann LM, Stuermer J. Prevalence of plateau iris syndrome in young patients with recurrent angle closure. Clin Exp Ophthalmol. 2007;35(5):409–413. doi: 10.1111/j.1442-9071.2007.01510.x. [DOI] [PubMed] [Google Scholar]
- 22.van Herick W, Shaffer RN, Schwartz A. Estimation of width of angle of anterior chamber. Incidence and significance of the narrow angle. Am J Ophthalmol. 1969;68(4):626–629. doi: 10.1016/0002-9394(69)91241-0. [DOI] [PubMed] [Google Scholar]
- 23.Xiao Y, Wang Y, Niu G, Li K. Transpupillary argon laser photocoagulation and Nd:YAG laser cystotomy for peripheral iris pigment epithelium cyst. Am J Ophthalmol. 2006;142(4):691–693. doi: 10.1016/j.ajo.2006.04.050. [DOI] [PubMed] [Google Scholar]
- 24.Yan PS, Lin HT, Wang QL, Zhang ZP. Anterior segment variations with age and accommodation demonstrated by slit-lamp-adapted optical coherence tomography. Ophthalmology. 2010;117(12):2301–2307. doi: 10.1016/j.ophtha.2010.03.027. [DOI] [PubMed] [Google Scholar]