Abstract
INTRODUCTION
Gastric outlet obstruction (GOO) is a clinical syndrome characterized by abdominal pain and postprandial vomiting. Causes of GOO include both benign and malignant disease. Bezoars, concretions of undigested or partially digested material in the gastrointestinal tract, are a rare entity and GOO due to duodenal bezoar is an uncommon presentation.
PRESENTATION OF CASE
We report the case of a 56-year-old woman who presented to the emergency department acutely with a 3-day history of epigastric pain, weakness and postprandial nonbilious vomiting. Initially, an upper gastrointestinal endoscopy (UGE) was performed to evaluate the cause of the GOO. A solid impacted bezoar was detected in the first portion of the duodenum with complete obstruction of the pyloric canal. In spite of multiple attempts for fragmentation using different devices, the extraction attempts failed. We administered acetylcysteine and cola per os. Abdominal computerized tomography was obtained and showed a solid mass in the duodenum. UGE was performed once more however, the mass was not suitable for fragmentation and removal. Thus, surgical treatment was decided. The bezoar was extracted via gastrotomy. The postoperative period was uneventful.
DISCUSSION
Even if a duodenal bezoar is small, because of its location it may cause GOO with abruptly clinical features. The diagnostic approach is similar to the other causes of the GOO. However, therapeutic options differ for each patient.
CONCLUSION
We should remember all the therapeutic and diagnostic options for a patient with upper gastrointestinal bezoars who present at the hospital whether or not there is a predisposing risk factor.
Keywords: Bezoar, Duodenal bezoar, Endoscopy, Gastric outlet obstruction, Gastrotomy
1. Introduction
Gastric outlet obstruction (GOO) is not a single entity, it is a clinical syndrome characterized by abdominal pain and postprandial vomiting due to mechanical obstruction of the outlet of the stomach. The causes of GOO include both benign disease as well as malignant conditions. Formerly, peptic ulcer disease was the most common cause of this entity. However, in recent decades, benign causes have become less common and 50–80% of cases have been attributed to malignancy.1 Besides peptic ulcer disease, gastric polyps, ingestion of caustics, congenital duodenal webs, and pancreatic pseudocysts are the other benign causes of GOO.2 Bezoars, concretions of undigested or partially digested material in the gastrointestinal tract, are a rare entity and GOO due to duodenal bezoar is an uncommon presentation.
Patients with an intestinal bezoar usually remain asymptomatic for many years and develop symptoms insidiously. However, if a bezoar occurs in the postpyloric region, it may be referred as an emergency. Herein, we report a case who was admitted to the emergency room with GOO secondary to a bezoar and present our experience while reviewing the literature.
2. Presentation of the case
A 56-year-old Turkish woman presented to the emergency department acutely with a 3-day history of epigastric pain, weakness and postprandial nonbilious vomiting. She had been tolerating only liquids for a month and had complaints of nausea and vomiting, particularly after solid food intake. She lost 6 kg in weight during this period. She did not have a history of any comorbidity or any previous surgery. On physical examination, she appeared ill and weak. Her abdomen was soft but showed tenderness over the epigastric area. The rest of her examination was unremarkable.
Laboratory test results did not show any notable abnormality. Supine abdominal X-ray film and abdominal ultrasonography were also unremarkable. After sufficient fluid resuscitation and nasogastric tube insertion for gastric decompression, an upper gastrointestinal endoscopy (UGE) was performed to evaluate the cause of GOO using a forward-viewing endoscope. A greenish solid impacted bezoar was detected in the first portion of the duodenum with complete obstruction of the pyloric canal (Fig. 1). As the patient was lying in the left lateral decubitis position, the bezoar was occluding the pyloric canal more. Therefore, because of its hardness and the obstruction of the pyloric canal, the endoscope could not be passed to the post-pyloric region. In spite of multiple attempts for fragmentation using a polypectomy snare, biopsy forceps and a Dormia basket, because the bezoar was fixed and hard, the extraction attempts failed. After the procedure, we administered acetylcysteine and cola three times daily for two days per os. In this time, abdominal computerized tomography was obtained to evaluate the size of the bezoar. It showed a dilated stomach and a solid mass with pockets of air in the second portion of the duodenum (5 cm × 6 cm in size), compatible with the features of bezoars (Fig. 2). On the third day of the treatment, UGE was performed once more; however the mass was still hard and not suitable for fragmentation and removal. Thus, surgical treatment was decided and a laparotomy through an upper midline incision was performed. At operation, intraduodenal mass was determined. The bezoar was pulled in to the stomach. After a longitudinal 5-cm gastrotomy, the bezoar was extracted and the gastrotomy was closed in two layers. Oral feeding was initiated on the second postoperative day and the patient was discharged on the postoperative fourth day with full recovery.
Fig. 1.
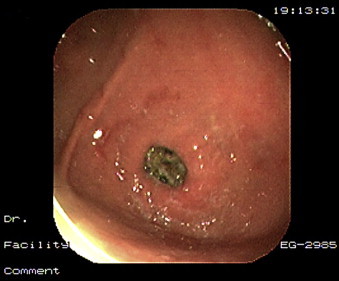
Upper gastrointestinal endoscopic view of the duodenal bezoar which caused the obstruction of the pyloric canal.
Fig. 2.
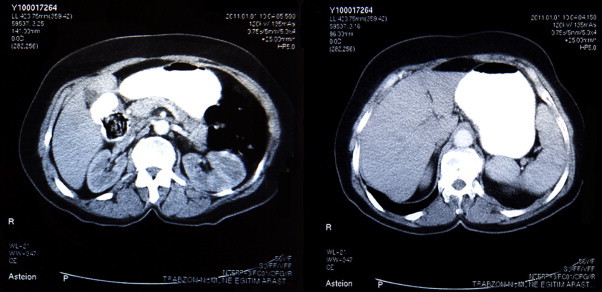
Computerized tomography shows a dilated stomach and a solid mass in the second portion of the duodenum.
3. Discussion
Any disease that mechanically impedes gastric emptying causes a clinical syndrome named GOO. The cause of the obstruction may be a benign or malignant disease. Before the 1980s, peptic ulcer disease was the most common cause of GOO, accounting for up to 90% of cases. Furthermore, 12% of patients with a peptic ulcer presented with gastric outlet obstruction as a direct consequence of a pyloric canal ulcer with associated pylorospasm. However, the incidence has declined with the discovery of the Helicobacter pylori and proton pump inhibitors. Currently, 50–80% of cases have been attributable to malignancy.3
Bezoars, one of the benign causes of the GOO, result from the accumulation of foreign indigested or partially digested material in the form of concretions. The true incidence of bezoars is unknown, however, reported incidence was found in less than 1% of patients undergoing UGE. The underlying cause of all types of the bezoars is ingestion of indigestible materials such as hair, cotton, paper or food rich in cellulose. Bezoars are classified according to these compositions. The major types are phytobezoars (fruit or vegetable matter), trichobezoars (hair), pharmacobezoars (medication such as tablets or semi-liquid drugs), and lactobezoars (concentrated milk formulas).4 For our presented case, there was neither previous surgery nor psychiatric disorder. A relatively small greenish mass that included indigestible food was detected after extraction of the bezoar during laparotomy. She had no contributing factors such as dehydration, malnutrition or diabetes mellitus.
The symptoms of GOO are similar regardless of the etiology. Nausea, vomiting, and epigastric pain are the most common clinical symptoms. However, onset of symptoms of GOO varies depending upon the etiology. It may be either abrupt or quiet. For bezoars, development of the symptoms may take a long time when it occurs in the stomach which can expand to a large volume, or for a few days if occurs in a small-volume region such as the duodenum. For our patient, she had a 3-day history of vomiting and epigastric pain, and some restrictions on food intake for a month. As the endoscopic view and computerized tomography film showed, a small volume of bezoar had fully obstructed the duodenal lumen and had caused gastric dilatation (Figs. 1 and 2).
The diagnosis may be suspected based upon clinical features and physical examination. It is confirmed by radiologic evaluation and UGE. Computerized tomography scans show a well-circumscribed intraluminal lesion, composed of concentric whorls of different densities with pockets of air enmeshed within it appearing in the intestinal lumen. UGE is the most sensitive method to establish the diagnosis and also helps to confirm and treat the underlying pathology.5 For our patient, abdominal X-ray and ultrasonography were unremarkable; however computerized tomography and UGE were helpful to define the location of the obstruction and to try treatment.
The first treatment option of GOO is similar for all types of etiologies. Adequate fluid and electrolyte replacement, gastric decompression, and proton pump inhibitors is the first step of the treatment. Definitive treatment should be based upon the underlying etiology. Currently treatment options for bezoars include observation, chemical dissolution, and endoscopic fragmentation. Surgical treatment via laparotomy or laparoscopy is preferred after a failed conservative procedure. Dissolution should be considered for phytobezoars producing mild symptoms. Many agents have been successfully tried for this purpose. Cellulase, papain, acetylcysteine and in recent years cola have been used for the medical therapy of bezoars. Cellulase appears to be preferred over papain because of the side effects of papain. In a review, cellulase was more effective and papain showed some serious side effects such as gastric ulcers, esophageal perforation and hypernatremia.6 Recently, dissolution with cola has been described to be one of the effective treatment options. The largest series of this treatment showed a 23.5% success rate for complete dissolution, particularly for phytobezoars, excluding diospyrobezoars. They recommend the use of cola for pretreatment to facilitate endoscopic fragmentation.7
UGE is used for the fragmentation and removal of the bezoar. Endoscopic removal involves fragmenting the bezoar by water flushes, direct suction, large polypectomy snare, biopsy forceps, electrosurgical knife, mechanical or extracorporeal lithotripsy and Nd:YAG laser.6–8 Operative intervention may be needed if endoscopic therapy fails or if there is a complication related to the bezoar such as obstruction or bleeding. However, GOO due to bezoars requires early surgery as it rarely improves with conservative therapy. If surgical intervention is required, bezoar removal is commonly done by gastrotomy. For this, either a laparotomy or laparoscopy can be used. Different reports have been published for laparoscopic removal. This technique is usually preferred because of its less postoperative pain and better cosmetic results. However, the longer operating time, higher costs and retrieval problems are the disadvantages of laparoscopy.8 For the presented case, endoscopic fragmentation and removal attempts failed twice because of the bezoar's location and hardness. Dissolution trials with cola and acetylcysteine also failed. Thus, we performed a laparotomy and then gastrotomy for removal. In the same procedure we had the opportunity to observe the small bowels for additional bezoars.
4. Conclusion
Even if a duodenal bezoar is small, because of its location it may cause GOO with abruptly clinical features. The diagnostic approach is similar to the other causes of the GOO. Therapeutic options differ for each patient. However, we should remember all the therapeutic and diagnostic options for a patient with upper gastrointestinal bezoars who present at the hospital whether or not there is a predisposing risk factor.
Conflict of interest statement
None.
Funding
None.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contributions
All the authors contributed equally to this study.
Footnotes
This case was reported in the VIII Turkish National Trauma and Emergency Surgery Congress, September 2011, in Antalya/Turkey as a poster presentation. However it has not been published elsewhere.
References
- 1.Shone D.N., Nikoomanesh P., Smith-Meek M.M., Bender J.S. Malignancy is the most common cause of gastric outlet obstruction in era of H2 blockers. American Journal of Gastroenterology. 1995;90:1769–1770. [PubMed] [Google Scholar]
- 2.Leung E., Barnes R., Wong L. Bezoar in gastro-jejunostomy presenting with symptoms of gastric outlet obstruction: a case report and review of the literature. Journal of Medical Case Reports. 2008;2:323. doi: 10.1186/1752-1947-2-323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Samad A., Khanzada T.W., Shoukat I. Gastric outlet obstruction: change in etiology. Pakistan Journal of Surgery. 2007;23:29–32. [Google Scholar]
- 4.Phillips M.R., Zaheer S., Drugas G.T. Gastric trichobezoar: case report and literature review. Mayo Clinic Proceedings. 1998;73:653–656. doi: 10.1016/S0025-6196(11)64889-1. [DOI] [PubMed] [Google Scholar]
- 5.Lin C.S., Tung C.F., Peng Y.C., Chow W.K., Chang C.S., Hu W.H. Successful treatment with a combination of endoscopic injection and irrigation with coca cola for gastric bezoar-induced gastric outlet obstruction. Journal of the Chinese Medical Association. 2008;71:49–52. doi: 10.1016/S1726-4901(08)70073-X. [DOI] [PubMed] [Google Scholar]
- 6.Walker-Renard P. Update on the medicinal management of phytobezoars. American Journal of Gastroenterology. 1993;88:1663–1666. [PubMed] [Google Scholar]
- 7.Lee B.J., Park J.J., Chun H.J., Kim J.H., Yeon J.E., Jeen Y.T. How good is cola for dissolution of gastric phytobezoars? World Journal of Gastroenterology. 2009;15:2265–2269. doi: 10.3748/wjg.15.2265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sharma D., Srivastava M., Babu R., Anand R., Rohtagi A., Thomas S. Laparoscopic treatment of gastric bezoar. Journal of the Society of Laparoendoscopic Surgeons. 2010;14:263–267. doi: 10.4293/108680810X12785289144566. [DOI] [PMC free article] [PubMed] [Google Scholar]


