Abstract
INTRODUCTION
Double appendix represents an extremely rare and commonly “missed” diagnosis, often with life threatening consequences.
PRESENTATION OF CASE
In this case report we present an interesting case of operative treatment of acute appendicitis in a doubled vermiform appendix stemming operative pitfalls. A 23-year-old female was admitted to the emergency room department complaining of diffuse abdominal pain, nausea, and vomiting over the past 36 h. As soon as the diagnosis of acute appendicitis was established a laparotomy via a McBurney incision was decided. Intraoperative findings included the presence of mild quantity of free fluid and surprisingly a thin non-inflamed appendiceal process. It was the preoperative ultrasound findings suggestive of acute appendicitis that dictated a more thorough investigation of the lower abdomen that led to the discovery of a second retrocecal inflamed appendix. Formal appendectomy was then performed for both processes. The patient had an uneventful recovery and was discharged on the fourth postoperative day.
DISCUSSION
Double appendix represents a challenging clinical scenario in cases of right lower quadrant pain.
CONCLUSION
Life threatening consequences with legal extensions can arise from the incomplete removal of both stumps.
Keywords: Double appendix, Acute appendicitis, Appendectomy, Ultrasonography, Abdominal pain
1. Introduction
Since originally observed and described by Picoli in 1892, double appendix emerged as a difficult to diagnose entity. With an incidence varying from 0.004% to 0.009%1,2 double appendix has become a neglected and commonly “missed” diagnosis, often with life threatening consequences. In adults, usually it constitutes an incidental finding during laparotomy for a different cause. On the other hand, double appendix in children, requires additional and more meticulous work-up as it is often represents a manifestation of more complex developmental intestinal, genitourinary or vertebral abnormalities.1,2
In the present paper we present an interesting case of operative treatment of acute appendicitis in a doubled vermiform appendix stemming operative pitfalls.
2. Case report
A 23-year-old female was admitted to the emergency room department complaining of diffuse abdominal pain, nausea, and vomiting over the past 36 h. The otherwise healthy patient with a free medical history reported aggravation of the symptom complex accompanied by low-grade fever (37.8 °C) and tachycardia upon admission. The physical examination confirmed the presence of the hallmarks of acute appendicitis, i.e. right lower quadrant pain (McBurney's sign) with signs of parietal peritoneum irritation (rebound tenderness). Digital per rectum examination revealed mild right-sided rectal wall tenderness. Leukocytosis (20 × 103/μL) with a left shift and increased C-reactive protein levels (15 mg/dL) were the results of the blood tests. The urine analysis test as well as the plain abdominal X-ray did not reveal any specific findings.
Using a GE Logic 9 scanner and a 10 MHz linear transducer a thorough ultrasonographic examination of the lower abdomen was then conducted which initially excluded occult pathology of the internal genitalia. Focusing on the point of maximum tenderness, in the right iliac fossa, and performing the graded compression technique a tubular, incompressible blind-ended loop, with a maximal cross-sectional diameter under compression of 11 mm consistent with the vermiform appendix was detected. There were no signs of perforation except a small quantity of free fluid surrounding its distal margin (Fig. 1). During Color Doppler study an increased vascularity of the appendiceal wall was also recorded.
Fig. 1.

The ultrasonographic exam performed with a GE Logic 9 scanner, using a 10 MHz linear transducer. Using the graded compression technique a tubular, incompressible blind ended loop, with a maximal cross-sectional diameter under compression of 11 mm approximately was revealed. The appendix resulted non-perforated, with a small quantity of free fluid surrounding its distal tip (margin).
As the diagnosis of acute appendicitis was non-questionable, a decision was made to perform an open appendectomy via a McBurney's incision. Intraoperative findings included mild quantity of free fluid and surprisingly a thin non-inflamed appendiceal process. A typical appendectomy was performed followed by a negative small bowel inspection for the presence of Meckel's diverticulum. It was the ultrasound findings that dictated a more meticulous investigation of the area around the cecum. A second appendix was detected with a definite mesoappendix and obvious signs of inflammation, retrocecally, 4 cm from the first one. A second formal appendectomy was then performed. Both appendiceal stumps were double tight with 2-0 absorbable sutures and were left in situ without further maneuver on the cecum wall (Fig. 2).
Fig. 2.
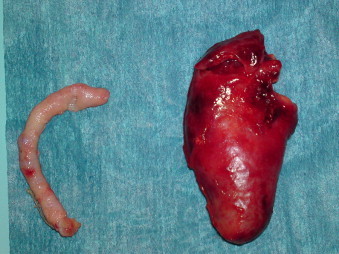
The two surgical specimens.
Histopathological examination of the surgical specimen confirmed the intraoperative findings of appendiceal duplication as well as findings of acute inflammation of the second appendix (Figs. 3 and 4). The patient had an uneventful recovery and she was discharged on the fourth postoperative day.
Fig. 3.
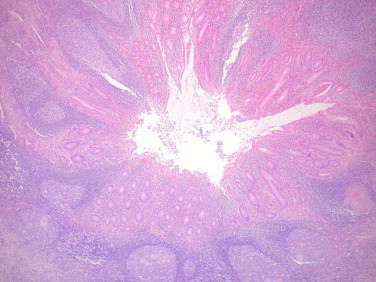
Low-power microscopic view of the vermiform appendix with acute appendicitis and lymphoid follicles with prominent germinal centers. H/E 100×.
Fig. 4.
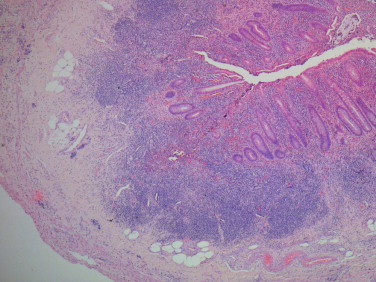
Low magnification of the second structure. The histologic composition is similar to the appendix. H/E 100×.
3. Discussion
Duplication of the appendix is considered a pretty rare entity with a reported incidence of 2 cases in 50,000 appendices.1 Literature references are usually exhausted in case reports reflecting the rarity of the condition. Approximately, 100 cases have been reported to date. From the anatomical and embryological viewpoint, a classification system for appendiceal duplications based on their anatomical location was elaborated by Cave in 1936. In 1963, Wallbridge devised this classification system by the reported until that date cases yielding the modified Cave–Wallbridge classification.3,4 This classification system, also “enriched” by Biermann in 1993, is shown at Table 1. More recently cases that cannot be included to the types shown in the table have been described as “the horseshoe appendix” in which one appendix has two openings into a common cecum5 and finally “the triple appendix”, an extremely rare condition with only a couple of cases reported.6
Table 1.
The modified Cave–Wallbridge classification.
| Type A | A single cecum with various degrees of partial duplication. |
| Type B1 | Also referred to as the “bird type” in which the 2 appendices are symmetrically placed on either side of the ileocecal valve. |
| Type B2 | Also referred to as the “taenia-coli type” in which one appendix arises from the cecum at the usual site and a second appendix branches from the cecum along the lines of the taenia at various distances from the first. |
| Type B3 | The second appendix arises from the hepatic flexure. |
| Type B4 | The second appendix arises from the splenic flexure. |
| Type C | A double cecum each with an appendix. |
Regarding the embryology of the normal appendix, briefly, during the 5th fetal week, a bud at the junction of the small and large bowel develops and undergoes rapid growth into a pouch. The proximal end of this pouch starts growing differentially to give rise to the cecum. The appendix first appears at the 8th week of gestation as an outpouching of the cecum. Then, it gradually rotates to a more medial location following the respective rotation of the gut which results in the fixation of the cecum in the right lower quadrant.7 However, although the normal embryogenesis of the appendix is generally known, data regarding the causes of its duplication are scarce. Unlike the other intestinal developmental disorders, malrotation does not seem to be implemented in the pathophysiology of the condition. In an attempt to explain the pathogenesis of duplication, Cave put forward two theories: (i) the persistence of a transient embryological structure and (ii) incidental appendiceal duplicity to a more general affection of the primitive midgut.3 However, despite the fact that Cave's theories may explain some types of duplication, they are inadequate to explain all types reported.
A double appendix may be either asymptomatic or it may present with symptoms deriving from obstruction or inflammation even long after an appendectomy performed for the excision of one of the two appendices. In children, however, concomitant malformations or duplications of the large intestine or the genitourinary system may be present, especially in types B1 and C probably due to their similar embryological origin and may serve as “alarm” signs. The critical point when treating this condition is the successful identification and removal of both appendices. Among the various types of duplication, Type B and especially subtypes where the second appendix lies retrocecally are of the highest risk to remain unnoticed. An unnoticed second appendix may result in serious clinical and medico-legal consequences due to the high risk of perforation, leading to generalized peritonitis.8 A history of appendectomy in a patient with a “missed” second appendix presenting with lower abdominal pain could reasonably shift differential diagnosis toward other medical conditions, i.e. diverticulum of the cecum, Meckel's diverticulum, colonic adenocarcinoma, gastroenteritis, acute mesenteric adenitis, intussusception, inflammatory bowel disease and genitourinary pathology thus, delaying diagnosis and appropriate treatment.9 In view of the management of such cases, laparotomy as well as laparoscopy has been successfully applied.10 However in cases where only one of the appendices shows signs of inflammation it is of paramount importance the total removal of both.7
Preoperative diagnosis of appendiceal duplication is usually difficult using routine imaging examinations. Abdominal ultrasound and computed tomography are the main available modalities. However, the reported sensitivity and specificity of both for the diagnosis and especially the detection of the appendix are of less importance because these modalities are usually not included in the routine workup of otherwise healthy patients with right lower quadrant pain. Theoretically, computed tomography has been reported to identify duplication of the appendix, especially in cases where both appendices are significantly inflamed.9
In our unit, we routinely submit all female patients with right quadrant pain to abdominal ultrasonography. The multiple pathologies arising from the female reproductive system and are included by definition in the differential diagnosis of a lower abdominal pain in the female patient is the main argument for this policy. Ultrasound detected the inflamed appendix but did not give any clues about the presence of duplication. Occasionally, the inflamed appendix may camouflage the presence of the second one, especially if it bears minimum or no signs of inflammation. The operator dependent nature of this diagnostic study logically exhausts the operator's attention when a firm pathology is detected, i.e. inflamed appendix and thus overlooks minor findings such as the presence of a second “normal” vermiform appendix. However, the additional information in the preoperative setting, extracted from the ultrasound examination, led in a more meticulous investigation after the recognition of the first non-macroscopically inflamed appendix.
McBurney's incision although extremely practical for completing the vast majority of acute appendicitis cases allows minimal access to the intra-abdominal viscera. The laparoscopic approach could undoubtedly offer a more global visualization of the area around the cecum minimizing operative pitfalls. In support of the above, successful laparoscopic appendectomy in cases of appendiceal duplication has been reported in pediatric population confirming the aforementioned advantages of the approach.10,11 However, the laparoscopic approach for appendectomy is not the standard practice in our department, reserving it for difficult to diagnose cases. Missing the second appendix in the setting of duplication is a scenario that should be prevented with the necessary vigilance and the knowledge of the entity from the surgeon's viewpoint. Acute appendicitis should not be directly omitted from differential diagnosis in a patient with typical clinical presentation and a history of appendectomy. Regarding operative technique, although a routine complete abdominal exploration seems futile as the doubled appendix could arise from multiple sites across the colon, we suggest that at least a retrocecal exploration during open surgery would be justified.
In conclusion, duplication of appendix although infrequent represents, without doubt, a challenging clinical scenario in cases of right lower quadrant pain. Life threatening consequences with legal extensions can arise from the incomplete removal of both stumps.
Conflict of interest
All authors declare no conflicts of interest.
Funding
None.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contributions
Christodoulidis G and Symeonidis D contributed equally to this work; Christodoulidis G, Symeonidis D, Spyridakis M, Koukoulis G, Triantafylidis G, and Manolakis A designed research, acquired and analyzed the data; Christodoulidis G, Symeonidis D, Spyridakis M, and Koukoulis G diagnosed and operated the patient; Christodoulidis G, Symeonidis D and Tepetes K wrote the paper. All authors approved the final version to be published.
References
- 1.Collins D. A study of 50,000 specimens of the human vermiform appendix. Surgical Gynecological Obstetrics. 1955;101:437–446. [PubMed] [Google Scholar]
- 2.Kjossev K.T., Losanoff J.E. Duplicated vermiform appendix. British Journal of Surgery. 1996;83:1259. [PubMed] [Google Scholar]
- 3.Cave A.J.E. Appendix vermiformis duplex. Journal of Anatomy. 1936;70:283–292. [PMC free article] [PubMed] [Google Scholar]
- 4.Wallbridge P.H. Double appendix. British Journal of Surgery. 1963;50:346–347. doi: 10.1002/bjs.18005022124. [DOI] [PubMed] [Google Scholar]
- 5.Mesko T.W., Lugo R., Breitholtz T. Horseshoe anomaly of the appendix: a previously undescribed entity. Surgery. 1989;106(3):563–566. [PubMed] [Google Scholar]
- 6.Uriev L., Maslovsky I., Mnouskin Y., Ben-Dor D. Triple-barreled type of appendiceal triplication. Annals of Diagnostic Pathology. 2006;10(3):160–161. doi: 10.1016/j.anndiagpath.2005.09.016. [DOI] [PubMed] [Google Scholar]
- 7.Schumpelick V., Dreuw B., Ophoff K., Prescher A. Appendix and cecum. Embryology, anatomy, and surgical applications. Surgical Clinics of North America. 2000;80(1):295–318. doi: 10.1016/s0039-6109(05)70407-2. [DOI] [PubMed] [Google Scholar]
- 8.Yanar H., Ertekin C., Unal E.S., Taviloglu K., Guloglu R., Mete O. The case of acute appendicitis and appendiceal duplication. Acta Chirurgica Belgica. 2004;104(6):736–738. doi: 10.1080/00015458.2004.11679655. [DOI] [PubMed] [Google Scholar]
- 9.Chew D.K., Borromeo J.R., Gabriel Y.A., Holgersen L.O. Duplication of the vermiform appendix. Journal of Pediatric Surgery. 2000;35(4):617–618. doi: 10.1053/jpsu.2000.0350617. [DOI] [PubMed] [Google Scholar]
- 10.Petit T., Godart C., Ravasse P., Jeanne-Pasquier C., Delmas P. Laparoscopic excision of an unusual appendiceal duplication. Annales de Chirurgie. 2001;126(10):1023–1025. doi: 10.1016/s0003-3944(01)00643-5. [DOI] [PubMed] [Google Scholar]
- 11.Travis J.R., Weppner J.L., Paugh J.C., II Duplex vermiform appendix: case report of a ruptured second appendix. Journal of Pediatric Surgery. 2008;43(9):1726–1728. doi: 10.1016/j.jpedsurg.2008.04.023. [DOI] [PubMed] [Google Scholar]


