Abstract
INTRODUCTION
Splenic artery aneurysms are rare but clinically important entities because of their potential for life threatening rupture. They seldom exceed 3 cms in size and only a few cases of giant splenic artery aneurysms (more than 10 cm size) have been reported until now.
PRESENTATION OF CASE
A 58 yr old female presented with painless pulsatile progressively enlarging lump in left upper abdomen. Contrast enhanced computed tomography revealed a 10.6 × 10.38 cm aneurysm arising from distal splenic artery along with a normal pancreas. Surgical treatment in form of complete excision of the aneurysm along with spleen and distal pancreas was performed. Gross examination showed an unruptured 12.7 × 11.8 cm true aneurysm of distal splenic artery. Postoperative course was uneventful.
DISCUSSION
Splenic artery aneurysms are discovered incidentally and the life time risk of rupture is 28% for giant aneurysms. Even with availability of less invasive procedures such as laproscopy or endovascular treatment, open surgery is mostly preferred.
CONCLUSION
Giant splenic artery aneurysms, although rare, should be considered in patients presenting with left upper abdomen pulsatile masses. Clinical suspicion followed by emergent management is necessary to prevent potentially life threatening complications.
Keywords: Splenic artery, Giant aneurysm, True aneurysm, Surgical management
1. Introduction
An aneurysm is a localized abnormal dilation of a blood vessel.1 Any artery can be affected by a true or a pseudoaneurysm. In true aneurysm, the aneurysmal wall is composed of all the 3 layers, that is, the intima, media and adventitia. Whereas in a pseudoaneurysm there is a breach in vessel wall along with an extra vascular hematoma bounded by surrounding tissue. The most common site of intra abdominal aneurysm is the abdominal aorta followed by iliac arteries and then splenic artery.2 Aneurysms in visceral arteries are rare and splenic artery is the commonest site, being affected in 60% of cases.3 True aneurysms of splenic artery seldom exceed 3 cm in size4,5 and giant splenic artery aneurysms (more than 10 cm in size) are extremely rare.4 These aneurysms may be complicated by rupture in 2–10% of cases7,8 but risk of rupture in giant aneurysms is as high as 28%7 with mortality approaching 40%.9 Early definitive surgical intervention is cornerstone in management.
2. Presentation of case
A 58 year old female presented with chief complaints of painless gradually enlarging lump in left upper abdomen for 6 months. She was normotensive, non diabetic, non smoker and non alcoholic. There was no history suggestive of pancreatitis, peptic ulcer disease, abdominal trauma, hepatobiliary disease, previous surgery or any other significant illness. On examination she was comfortable with blood pressure 136/90 and pulse 90 per min−1 and pallor was absent. A well defined non tender pulsatile intra abdominal lump was palpable in left hypochondrium, left lumbar and epigastric region which was oval in shape, 10 cm × 9 cm in size, moving well with respiration and its upper margin was extending beneath the left costal margin.
Hematological and coagulation profile was within normal limits. A Doppler ultrasonography showed a well defined mass in region of lesser sac with turbulent blood flow suggestive of an aneurysm. Contrast enhanced computed tomography showed a 10.6 cm × 10.38 cm mass in region of lesser sac with contrast enhancement and few calcification specs in its wall (Fig. 1). It was medial to spleen, anterior to and compressing body and tail of pancreas, anterior to left kidney and compressing left renal vein. There were no features suggestive of pancreatitis. Overall picture was suggestive of an aneurysm arising from distal splenic artery. Transcatheter angiography via femoral artery failed to delineate the lesion.
Fig. 1.
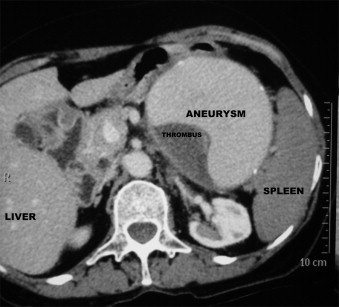
CECT abdomen showing the aneurysm.
The patient underwent exploratory laprotomy by midline incision. A 12.7 cm × 11.8 cm pulsatile swelling was present in left upper abdomen between stomach and transverse colon medial to the hilum of spleen. Lesser omentum was first opened and access was gained to lesser sac. Celiac trunk was exposed and splenic artery was identified and traced up to the lesion and was seen entering it. Splenic artery control was taken at the origin with a vascular clamp (Fig. 2). This made the lump non pulsatile, confirming its origin from the splenic artery. Spleen was mobilized by dividing peritoneal attachments and gastrosplenic ligament but communication with lesion was maintained. Gastrocolic omentum was opened and the lesion was mobilized along with spleen. Pancreas was mobilized off the posterior wall of lesion and small part of tail was excised as it was densely adhered to it (Fig. 3). Splenic artery at the point of entry into aneurysm was transfixed and transected (Fig. 4). Thus aneurysectomy with splenectomy with distal pancreatectomy was performed and the lesion removed in toto.
Fig. 2.
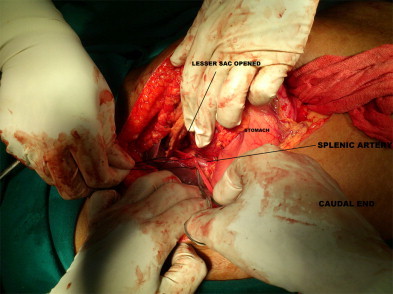
Splenic artery control.
Fig. 3.
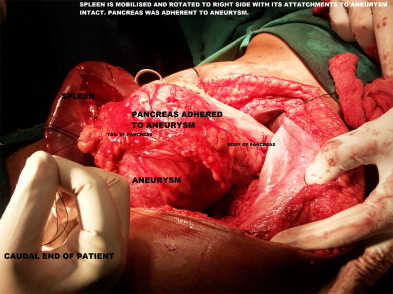
Pancreas adherent to aneurysm.
Fig. 4.
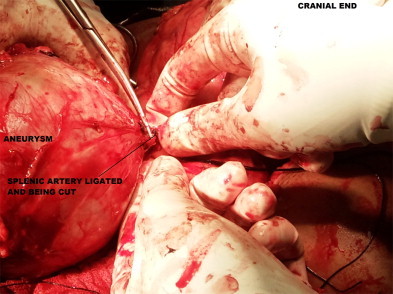
Feeding vessel of aneurysm being cut after ligation.
Gross specimen showed a 12.7 cm × 11.8 cm aneurysm filled with clotted blood along with spleen measuring 14 cm in largest diameter and 1 cm of tail of pancreas (Fig. 5). Histopathology showed aneurysm with all the three layers of vessel wall suggestive of a true aneurysm.
Fig. 5.
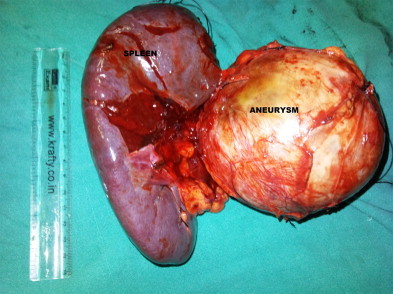
Gross specimen showing the aneurysm and the spleen.
Postoperative recovery was good and patient was discharged on 5th postoperative day.
3. Discussion
True splenic artery aneurysms are rare but potentially life threatening entities. There is an estimated prevalence of 0.02–0.1% in general autopsies but their true incidence is difficult to determine as these are mostly asymptomatic.8 The disease is four times more common in females and affects population in their fifth to sixth decade of life.10 Mostly, these aneurysms are saccular in shape and are located in middle to distal part of the splenic artery.8,11 Pseudoaneurysms of the splenic artery are rare and fewer than 200 cases are reported in English literature till now. Giant pseudoaneurysms (more than 5 cm in size) of splenic artery are also extremely rare and about 20 cases have been reported, largest being 19 cm as reported by Goldberg et al. in 2010.6 In present case the patient was female in sixth decade of her life and had 12.7 cm sized saccular true aneurysm in the distal part of splenic artery.
The precise etiology of splenic artery aneurysms and pseudoaneurysms remains unknown. True splenic artery aneurysms are thought to be associated with hypertension, portal hypertension, cirrhosis, liver transplantation and pregnancy.12,13 80% of aneurysms show atherosclerotic changes and calcification5. Splenic artery pseudoaneurysms are thought to be caused by pancreatitis, abdominal trauma, postoperative cases of liver transplant and rarely peptic ulcer disease.14 The most common cause is considered to be chronic pancreatitis.14 Pancreatic enzymes are thought to cause necrotizing arteritis with destruction of vessel architecture and fragmentation of elastic tissue leading to pseudoaneurysm formation. In the present case however no significant history was elicited and pancreas was also normal.
Splenic artery aneurysms are mostly asymptomatic and are discovered incidentally. A case series from Mayo clinic showed that 97.5% patients with unruptured aneurysms were asymptomatic.12 Others can present with a palpable pulsatile lump or vague upper abdominal discomfort. In contrast, splenic artery pseudoaneurysms are usually symptomatic and only 2.5% of cases are incidental findings.14 The most common presenting complaint is of abdominal pain.14 Patients may also present with hematochezia or malena, hemosuccus pancreaticus or hematemesis. Our patient presented with painless progressive pulsatile lump in left upper abdomen consistent with that of a true aneurysm.
Splenic artery aneurysms are usually diagnosed incidentally. Diagnosis is usually made by contrast enhanced computed tomography scans and the lesions are imaged during the arterial phase. Doppler and magnetic resonance imaging are important adjunct in diagnosis. Digital subtraction angiography or transcatheter angiography via femoral artery is considered gold standard investigation2 because of its therapeutic potential. However in this present case angiography failed to visualize the aneurysm probably because of technical difficulty and clotting of blood in aneurysm.
Any aneurysm if left untreated will progress in size and will eventually rupture. The life time risk of rupture in 2–10% for small and 28% for giant aneurysms.7,8 The highest incidence of rupture is in young pregnant women with mortality being 75% and fetal mortality being 95%.15 Ruptured splenic artery aneurysm presents with abdominal pain and hemodynamic instability and may mimic ruptured ectopic pregnancy in young females. Double rupture phenomenon, that is, sudden hemodynamic instability followed by spontaneous stabilization and subsequent circulatory collapse, may be seen whereby initial bleeding tamponades into lesser sac followed by flooding into peritoneal cavity.16 Risk of rupture is higher in pseudoaneurysms as compared to true aneurysms and can be as high as 37% with mortality approaching 90% when untreated.4,17 Besides rupture, aneurysms can also be complicated by splenic infarction or compression of adjacent biliary tree causing pseudo-obstructive jaundice. Thus once the diagnosis is made immediate definite intervention is mandatory.
The literature suggests that treatment of symptomatic splenic artery aneurysms should be performed.12 As of now no definite guidelines for intervention are present but consensus recommends that all patients with symptomatic aneurysms, pregnant or women of child bearing age group, lesion larger than 2 cm, lesions gradually increasing in size or patients with portal hypertension should undergo treatment.18–21 Risk benefit ration must be evaluated for those with asymptomatic and <2 cm size lesions. Present case had gradually enlarging 12 cm size lesion thus a decision to operate was made.
Splenic artery aneurysms can be treated by endovascular or surgical procedure.18–20,22 Open surgical procedure depends on location of the lesion. Aneurysms of proximal splenic artery can be managed by ligation of splenic artery at both the ends of lesion and excision of aneurysm with splenic preservation. Aneurysms at middle or distal end of splenic artery, as in present case, are best treated by excision of lesion along with splenectomy and distal pancreatectomy. Aneurysms can also be managed laproscopically via an anterior or lateral approach with good exposure and lesser postoperative pain and swifter recovery.23 Endovascular techniques are also a good alternative to surgical approach with 80–92% success rate.24 Coil embolization, detachable balloon occlusion or stent graft may be used.25 Splenic abscess formation, splenic infarct, high rate of recurrence and inability to perform in larger lesions are drawbacks of endovascular techniques.24 However, even with availability of less invasive procedures such as laproscopy or endovascular treatment, open surgery is mostly preferred because of lower recurrence and complication rate.
4. Conclusion
Splenic artery aneurysms are rare but are increasingly diagnosed as incidental findings. Giant aneurysm can present as pulsatile left upper quadrant masses. Expeditious diagnosis and treatment is the cornerstone in such cases so as to prevent catastrophic complications, as risk of rupture and subsequent mortality is significant.
Conflict of interest statement
The authors have no conflicts of interest.
Funding
None.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contributions
Siddharth Yadav prepared the manuscript and was assistant in surgery. Piyush Sharma helped in preparing the manuscript. Pintu Kumar Singh was assistant in surgery. Sudhanshu Punia and Pragnesh Desai helped in preparing the manuscript. Anjani Kumar was assistant in surgery. Sunil Jain was chief operating surgeon.
References
- 1.Kumar V., Abbas A.K., Fausto N. Robbins and Cortan pathologic basis of disease. Elsevier Saunders; India: 2004. Blood vessel. [Google Scholar]
- 2.Trastek V.F., Pairolero P.C., Joyce J.W., Hollier L.H., Bernatz P.E. Surgery. 1982;91(6):694–699. [PubMed] [Google Scholar]
- 3.Feo C.F., Scanu Am, Fancella A., Costantino S. Visceral aneurysm and vascular anomaly involving the splenic artery. Digestive Diseases and Sciences. 2004;49:1378–1380. doi: 10.1023/b:ddas.0000042233.14587.ef. [DOI] [PubMed] [Google Scholar]
- 4.Huang I.H., Zuckerman D.A., Mathews J.B. Occlusion of a giant splenic artery pseudoaneurysm with percutaneous thrombin-collagen injection. Journal of Vascular Surgery. 2004;40:574–577. doi: 10.1016/j.jvs.2004.06.020. [DOI] [PubMed] [Google Scholar]
- 5.Dave Sp, Reis E.D., Hossain A., Taub P.J., Kerstein M.D., Hollier L.H. Splenic artery aneurysm in 1990s. Annals of Vascular Surgery. 2000;14:223–229. doi: 10.1007/s100169910039. [DOI] [PubMed] [Google Scholar]
- 6.Goldberg R.F., Maley W., Kennedy E.P., Yeo C.J., Lavu H. Giant splenic artery pseudoaneurysm. Journal of Gastrointestinal Surgery. 2010:25. doi: 10.1007/s11605-010-1388-3. [PMID 21108018] [DOI] [PubMed] [Google Scholar]
- 7.Jamsheer N.S., Malik N. Ruptured splenic artery aneurysm. Annals of Saudi Medicine. 2001;21:215–219. doi: 10.5144/0256-4947.2001.340. [DOI] [PubMed] [Google Scholar]
- 8.Sibalis D., Papathanassiou Z.G., Karnabatidis D., Christeas N., Katsanosk K., Vagianos C. Splenic Arteriovenous fistula and sudden onset of portal hypertension as complication of ruptured splenic artery aneurysm: successfully treated with transcatheter arterial embolisation: a case study and review of literature. World Journal of Gastroenterology. 2006;12(26):4264–4266. doi: 10.3748/wjg.v12.i26.4264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Karaman K., Onat L., Sirvanci M., Olga R. Endovascular stent graft treatment in a patient with splenic artery aneurysm. Diagnostic and Interventional Radiology. 2005;11:119–121. [PubMed] [Google Scholar]
- 10.Kenningham R., Hershman M.J., McWilliam R.G., Cambell F. Incidental splenic artery aneurysm. Journal of the Royal Society of Medicine. 2002;95:460–461. doi: 10.1258/jrsm.95.9.460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kehagias D.T., Tzalonikos M.T., Moulopoulos L.A., Gouliamos A.D., Mourikis D.A., Valhos L.J. MRI of a giant splenic artery aneurysm. The British Journal of Radiology. 1998;71:444–446. doi: 10.1259/bjr.71.844.9659140. [DOI] [PubMed] [Google Scholar]
- 12.Abbas M.A., Stone W.M., Fowl R.J., Karkaletsis A., Faros E., Dalamarinis K. Splenic artery aneurysm: two decade experience at Mayo Clinic. Annals of Vascular Surgery. 2002;16:442–449. doi: 10.1007/s10016-001-0207-4. [DOI] [PubMed] [Google Scholar]
- 13.Lee P.C., Rhee R.Y., Gordon R.Y., Fung J.J., Webster M.W. Management of splenic artery aneurysm: the significance of portal and essential hypertension. Journal of the American College of Surgeons. 1999;189:483–490. doi: 10.1016/s1072-7515(99)00168-4. [DOI] [PubMed] [Google Scholar]
- 14.Tessier D.J., Stone W.M., Fowl R.J., Karkaletsis A., Faros E., Dalamarinis K. Clinical features and management of splenic artery aneurysm: case series and cumulative review of literature. Journal of Vascular Surgery. 2003;38:969–974. doi: 10.1016/s0741-5214(03)00710-9. [DOI] [PubMed] [Google Scholar]
- 15.Sadat U., Dar O., Walsh S., Varty K. Splenic artery aneurysm in pregnancy – a systematic review. International Journal of Surgery. 2008;6:261–265. doi: 10.1016/j.ijsu.2007.08.002. [DOI] [PubMed] [Google Scholar]
- 16.Remy D., Linder J.L. Splenic artery aneurysm rupture: case report and review of literature. Acta Chirurgica Belgica. 1993;93:54–57. [PubMed] [Google Scholar]
- 17.LiPuma J.P., Sach P.B., Sands M.J., Stuhlmillee S., Herbener T.E. Angiography/interventional case of the day: splenic artery pseudoaneurysm associated with pancreatitis. American Journal of Roentgenology. 1997;169(259):262–263. doi: 10.2214/ajr.169.1.9207539. [DOI] [PubMed] [Google Scholar]
- 18.Fotopoulos N., Kyriakidis A., Dimopoulos K., Karkaletsis A., Faros E., Dalamarinis K. Splenic artery aneurysm rupture. Journal of Digestive Surgery. 2001;18:325–326. doi: 10.1159/000050162. [DOI] [PubMed] [Google Scholar]
- 19.Arepally A., Dagli M., Hofman L.V., Kim H.S., Cooper M., Klein A. Treatment of splenic artery aneurysm with use of a Stent-graft. Journal of Vascular and Interventional Radiology. 2002;13:631–633. doi: 10.1016/s1051-0443(07)61659-5. [DOI] [PubMed] [Google Scholar]
- 20.Babb R.R. Aneurysm of splenic artery. Archives of surgery. 1976;111(8):924–925. doi: 10.1001/archsurg.1976.01360260092027. [DOI] [PubMed] [Google Scholar]
- 21.Kitamura H., Nakayama K., Kitano, Ozaki N., Nagoka S. Removal of splenic artery with a large aneurysm adhered to pancreas without pancreatectomy: report of a case. Surgery Today. 2002;32(8):747–749. doi: 10.1007/s005950200141. [DOI] [PubMed] [Google Scholar]
- 22.Mattar S.G., Lumsden A.B. The management of splenic artery aneurysm: experience with 23 cases. American Journal of Surgery. 1995;169(6):580–584. doi: 10.1016/s0002-9610(99)80225-6. [DOI] [PubMed] [Google Scholar]
- 23.Lee S., Florica O. Laproscopic resection of splenic artery aneurysm with preservation of splenic function. Singapore Medical Journal. 2008;49:e303–e304. [PubMed] [Google Scholar]
- 24.Pescarus R., Montrenil B., Bendavid Y. Giant splenic artery aneurysm: case report and review of literature. Journal of Vascular Surgery. 2005;42:344–347. doi: 10.1016/j.jvs.2005.04.026. [DOI] [PubMed] [Google Scholar]
- 25.Herskowitz M.M., Safriel Y., Gillego V. Successful treatment of a giant splenic artery pseudoaneurysm solely by proximal coil embolisation. European Journal of Vascular and Endovascular Surgery Extra. 2002;3:52–53. [Google Scholar]


