Abstract
Introduction
Acute lung injury (ALI) is a devastating condition that places a heavy burden on public health resources. Although the need for effective ALI prevention strategies is increasingly recognised, no effective preventative strategies exist. The Lung Injury Prevention Study with Aspirin (LIPS-A) aims to test whether aspirin (ASA) could prevent and/or mitigate the development of ALI.
Methods and analysis
LIPS-A is a multicentre, double-blind, randomised clinical trial testing the hypothesis that the early administration of ASA will result in a reduced incidence of ALI in adult patients at high risk. This investigation will enrol 400 study participants from 14 hospitals across the USA. Conditional logistic regression will be used to test the primary hypothesis that early ASA administration will decrease the incidence of ALI.
Ethics and dissemination
Safety oversight will be under the direction of an independent Data and Safety Monitoring Board (DSMB). Approval of the protocol was obtained from the DSMB prior to enrolling the first study participant. Approval of both the protocol and informed consent documents were also obtained from the institutional review board of each participating institution prior to enrolling study participants at the respective site. In addition to providing important clinical and mechanistic information, this investigation will inform the scientific merit and feasibility of a phase III trial on ASA as an ALI prevention agent. The findings of this investigation, as well as associated ancillary studies, will be disseminated in the form of oral and abstract presentations at major national and international medical specialty meetings. The primary objective and other significant findings will also be presented in manuscript form. All final, published manuscripts resulting from this protocol will be submitted to Pub Med Central in accordance with the National Institute of Health Public Access Policy.
Keywords: acute lung injury, acute respiratory ditress syndrome, aspirin, critical illness, prevention, clinical trial
Article summary.
Article focus
The primary objective of this manuscript is to provide the background information and methodology for a randomised clinical trial aiming to test the safety and efficacy of aspirin (ASA) in the prevention of acute lung injury (ALI) in patients determined to be at high risk.
A secondary aim of this trial is to determine if early administration of ASA modulates plasma mediators shown to be important in the development of ALI and its outcomes.
Third, this study will evaluate novel mechanisms by which an antiplatelet agent ASA may modulate the development and progression of lung injury in patients at risk.
Key messages
This paper describes the background information, methodology and statistical analysis plan for the first multicentre clinical trial aiming to test a promising ALI prevention strategy.
The results of this investigation will inform the scientific merit of a future phase III clinical trial on ASA administration as an ALI prevention strategy in at-risk patients.
This protocol will facilitate the development of an essential infrastructure for future clinical trials aiming to test ALI prevention strategies.
Strengths and limitations of this study
A major strength of this investigation is its multicentre, randomised clinical trial study design. A second strength of this investigation is the use of a lung injury prediction score for the timely identification of patients at high risk for ALI. A third strength of this investigation is the use of a checklist for lung injury prevention which will standardise important co-interventions in patients at high risk for ALI thereby minimising confounding of the primary association of interest (ASA and ALI).
Limitations of this study protocol include the recognition that many patients may have ‘injured lungs’ at the time of study initiation despite not meeting the formal criteria for ALI. In addition, it is recognised that a modest proportion of the study population may be resistant to the actions of ASA. Finally, the time-sensitive nature of the study protocol and the high prevalence of ASA use at the time of hospital admission may impact the feasibility of this work.
Introduction
Acute lung injury (ALI) and the acute respiratory distress syndrome (ARDS) are life-threatening syndromes that continue to consume substantial healthcare resources and profoundly impact on patient-important outcomes.1 Although recent epidemiological studies suggest the incidence of lung injury may be on the decline,2 even conservative estimates suggest the associated mortality continues to exceed 25%.3 Beyond mortality, an episode of ALI/ARDS also substantially influences the patient's long-term outcomes with functional deficits persisting up to 5 years after the episode of respiratory failure.4
Importantly, the clinical syndrome of ALI generally occurs as a complication of an initial predisposing acute injury such as pneumonia, aspiration, sepsis, trauma, shock or massive transfusion.5 However, only a fraction of patients (10–30%) with these initial injuries develop ALI/ARDS.6 7 Moreover, only 30% of ALI patients fulfil criteria for ALI within 6 h of presentation to the emergency department (ED).8 The majority of patients develop ALI a median of two days after hospital presentation (IQR 1–4 days). This period of time between hospital presentation and development of ALI presents a window of opportunity for interventions to prevent the development of ALI.
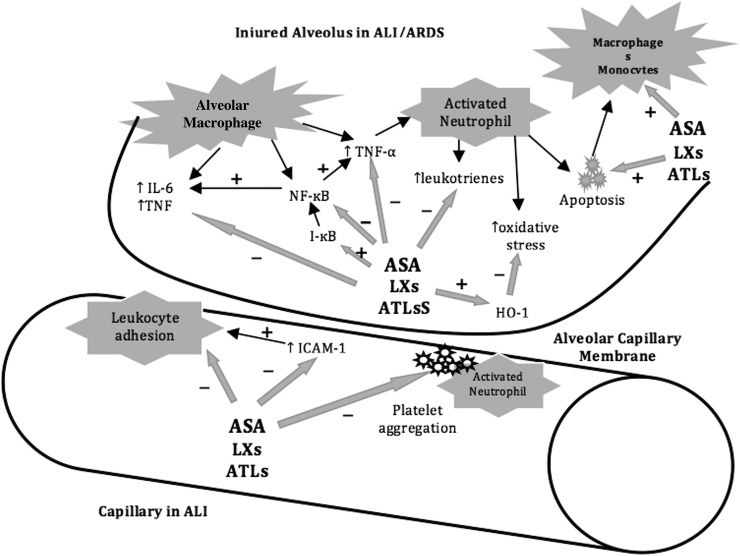
Recently, accumulating evidence suggests an important role for platelets in ALI pathogenesis9–11 and resolution.12–14 Notably, preclinical data suggest that aspirin (ASA) can modulate many of the platelet-mediated processes involved in ALI development11 15 16 and resolution.17 18 Proposed mechanisms for these protective effects include reduced thromboxane A2,9 P-selectin19 and platelet-derived chemokine (eg, CCL5 and CXCL4)20 production, prevention of the formation of platelet-neutrophil aggregates9 and neutrophil extracellular traps,21 22 and enhanced formation of anti-inflammatory lipid mediators such as 15-epi-lipoxin A4 (figure 1).17 Importantly, recent observational studies have also suggested a potential preventive role for antiplatelet therapy in patients at high risk of ALI.23 24 However, the evidence remains inconclusive and equipoise remains.
Figure 1.
Illustration of the potential role of aspirin, lipoxins and aspirin-triggered lipoxins on the mediators of ALI development and progression. Black arrows indicate events in ALI. Grey arrows indicate action of ASA, LXs, or ATLs. ALI, acute lung injury; ARDS, acute respiratory distress syndrome; ASA, aspirin; ATLs, aspirin-triggered lipoxins; HO, haeme oxygenase; I-κB, nuclear factor kappa-light-chain-enhancer of activated B-cell inhibitor; ICAM, intercellular adhesion molecule; IL-6, interleukin-6; LX, lipoxins; NF-κB, nuclear factor kappa-light-chain-enhancer of activated B-cells; TNF, tumour necrosis factor.
To further enhance our understanding of ASA's role in the prevention and/or mitigation of ALI, the Lung Injury Prevention Study (LIPS) group with the support of the US Critical Illness and Injury Trials Group (USCIITG) as well as the National Heart, Lung and Blood Institute (NHLBI) have designed the LIPS with Aspirin (LIPS-A), a randomised clinical trial that aims to test the safety and efficacy of ASA in the prevention of ALI in patients determined to be at high risk. This paper describes the study procedures and planned analyses for this clinical trial.
Methods and analysis
Administrative structure
To facilitate the conduct of the present investigation, as well as future ALI prevention studies, three specialised centres were established. The data and statistical coordinating centre, responsible for data management, randomisation and pharmacy coordination, will reside at Mayo Clinic in Rochester, MN. The clinical coordinating centre (CCC), responsible for the study conduct and safety monitoring, will reside at Beth Israel Deaconess Medical Center in Boston, MA, USA. The biospecimen repository and Knowledge Translation Center, responsible for specimen management as well as the LIPS score and the checklist for lung injury prevention (CLIP) online screening tools, will reside at Montefiore Medical Center in Bronx, NY, USA. The principal investigators from these three centres form the LIPS-A Executive Committee. This committee will collaboratively oversee all aspects of the study design and the protocol implementation.
Study design
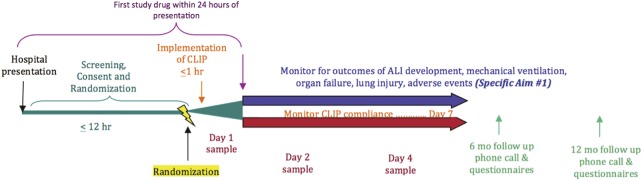
To test the hypothesis that ASA is associated with a reduced rate of incident ALI, the LIPS-A group has designed a multicentre, double-blind, placebo-controlled, parallel group, phase II randomised clinical trial. The ClinicalTrials.gov registration number is NCT01504867. An outline of the study design and study procedures appears in figure 2.
Figure 2.
Schematic of the planned study procedures.
Study population
Adult patients aged 18 years and older at high risk for ALI on admission to the hospital will be enrolled. To facilitate the identification of those at high risk for ALI, the LIPS-A will utilise the recently validated LIPS.8 Patients will be considered at high risk of development of ALI based on an LIPS score of 4 or greater. Patients who fulfil criteria for ALI on hospital presentation or at any point prior to randomisation will be excluded. A full list of exclusion criteria with the justification for each can be seen in table 1.
Table 1.
Study exclusion criteria
| Exclusion criteria | Justification |
|---|---|
| Antiplatelet therapy on admission or within 7 days prior to admission | Inability to ethically randomise |
| Presented to outside hospital emergency department >12 h before arrival at site's facility | Inability to enrol within time frame for possible benefit |
| Inability to obtain consent and randomise within 12 h of hospital presentation | Inability to enrol within time frame for possible benefit |
| Admitted for elective or emergency surgery | Aspirin not found to benefit this group in preliminary studies |
| ALI on hospital presentation or prior to randomisation | Inability to adequately assess outcome |
| Presentation believed to be due to pure heart failure and no other known risk factors for ALI | Inability to adequately assess outcome |
| Receiving mechanical ventilation through a tracheostomy tube prior to current hospital admission (patient who is ventilator dependent) | Inability to adequately assess outcome |
| Bilateral pulmonary infiltrates present on admission only if the patient has a history of interstitial lung disease that can reasonably explain the current degree of pulmonary infiltrates present | Inability to adequately assess outcome |
| Allergy to aspirin or NSAIDs | Intervention contraindicated |
| Bleeding disorder* | Intervention contraindicated |
| Suspected active bleeding or judged to be at high risk for bleeding complications | Intervention contraindicated |
| Presence of acute kidney injury† | Intervention contraindicated |
| Severe chronic liver disease (Child-Pugh class C) | Intervention contraindicated |
| Active peptic ulcer disease (within past 6 months) | Intervention contraindicated |
| Pregnancy or breast feeding | Intervention contraindicated |
| Inability to administer study drug | Unable to administer study drug |
| Expected hospital stay <48 h | Incomplete study procedures and outcome data |
| Admitted for comfort or hospice care | Incomplete study procedures and outcome data |
| Patient, surrogate or physician not committed to full support (exception: a patient will not be excluded if he/she would receive all supportive care except for attempts at resuscitation from cardiac arrest) | Unable to assess primary outcome |
| Not anticipated to survive >48 h | Incomplete study procedures and outcome data |
| Previously enrolled in this trial | Violates the statistical assumption of sample independence |
| Enrolment in concomitant intervention study | Potential confounding and co-enrolment interactions |
*Any disorder with known associated with increased risk of bleeding. Common disorders may include thrombocytopaenia, disseminated intravascular coagulation, haemophilia, von Willebrand disease, oral anticoagulant therapy or advanced liver disease with associated coagulation disorders. Platelet count <50000 or absence of platelet count in the previous 24 h to allow for assessment of platelet status.
†Acute kidney injury defined as ‘R’ or greater according to RIFLE criteria.
ALI, acute lung injury; NSAIDs, non-steroidal anti-inflammatory medications.
Patients will be recruited from 14 clinical sites in the USA with experience in the identification and management of ALI. A full list of the participating institutions as well as each site's primary investigator can be seen in table A1 and are indexed on ClinicalTrials.gov. The resulting study population is expected to be diverse and representative of the general population of patients at risk for ALI such that the study findings will be externally valid and generalisable to the broader academic community.
Table A1.
Lung Injury Prevention Study with Aspirin (LIPS-A) Coordinating Center Personnel and Site Investigators
| Coordinating centres | |
|---|---|
| Clinical Coordinating Center | Daniel S Talmor MD, MPH |
| Valerie M Banner-Goodspeed, ALB | |
| Data and Statistical Coordinating Center | Ognjen Gajic, MD, MSc, FCCP, FCCM |
| Daryl J Kor, MD | |
| Rickey E Carter, PhD | |
| Richard Hinds, BS, MS, RRT | |
| Biospecimen Repository and Knowledge Translation Center | Michelle N Gong MD, MS |
| Graciela Soto, MD | |
| Clinical sites | |
| Beth Israel Deaconess Medical Center | Daniel Talmor, MD, MPH |
| Michael Howell MD, MPH | |
| Bridgeport Hospital | David Kaufman, MD |
| Brigham and Womens Hospital | Peter Hou, MD |
| Bruce D Levy, MD | |
| Duke University Medical Center | Ian Welsby, BSc, MBBS |
| Heatherlee Bailey, MD, FAAEM, FCCM | |
| Harborview Medical Center | Timothy R Watkins, MD MSc |
| Massachusetts General Hospital | Ednan Bajwa, MD, MPH |
| Christopher Kabrhel, MD | |
| Mayo Clinic, Florida | Emir Festic, MD |
| Augustine Lee, MD | |
| Mayo Clinic, Rochester | Ognjen Gajic, MD |
| Daryl Kor, MD | |
| Rahul Kashyap, MBBS | |
| Leanne Clifford, MBBS | |
| Montefiore Medical Center | Michelle Gong, MD |
| Graciela Soto, MD | |
| University of Florida Medical Center | Marie-Carmelle Elie, MD |
| Hassan Alnuaimat, MD | |
| University of Illinois College of Medicine | Ruxana Sadikot, MD, MRCP, FCCP |
| University of Louisville Medical Center | Ozan Akca, MD, FCCM |
| Rodrigo Cavallazzi, MD | |
| Melissa Platt, MD | |
| University of Michigan | Pauline Park, MD |
| Jill Cherry-Bukowiec, MD, MS | |
| Lena Napolitano, MD | |
| Krishnan Raghavendran, MD | |
| John Younger, MD, MS | |
| Wake Forest University Medical Center | Jason Hoth, MD |
To facilitate patient enrolment, study coordinators at each participating institution will screen patients in the ED with a web-based LIPS calculator to determine each potential participant's risk for development of ALI. Eligible patients with an LIPS score ≥4 will be approached by study coordinators or study investigators for informed consent. Eligible patients will be enrolled and randomised within 12 h of hospital presentation. This will allow for maximal recruitment within the window of opportunity for interventions to prevent ALI development as our preliminary data show median time to ALI is 2 days after hospital admission.8
Interventions
Study drug: The first dose of study drug (ASA vs placebo) will be administered within the first 24 h after presentation to the hospital, either by mouth or by nasogastric or orogastric tube. For patients randomised to the intervention arm, a generic ASA 325 mg one-time loading dose on day 1 will be administered followed by generic ASA 81 mg by mouth once daily for study days 2–7 or until hospital discharge or death, whichever occurs first. The intervention duration of 7 days was chosen because >85% of ALI/ARDS cases were noted to have developed during this time frame in our preliminary studies.8 In support of the dosing scheme chosen for this investigation, a randomised clinical trial noted low-dose ASA at 81 mg daily was effective in elevating plasma levels of anti-inflammatory lipoxins and inhibiting platelet thromboxane activity with only a slight increase in effect at higher doses of ASA.25 26 All study medication doses (active treatment with ASA and placebo) will be in powder form of identical colour, contained within capsules that can be opened and administered via a gastric tube.
Co-interventions: Important co-interventions will be standardised in all study patients. To this end, the investigative team has developed a web-based, computerised, interactive tool to standardise essential elements of care delivery such as mechanical ventilation, aspiration precautions, infection control, fluid management and transfusion in patients at risk. This tool is termed CLIP.2 A summary of the CLIP elements is listed in table 2. Having identified high-risk patients early in the course of the illness with the LIPS calculation and having standardised the important elements of care delivery with the CLIP, we expect to have optimised our ability to investigate whether ASA is a safe and effective agent in preventing ALI.
Table 2.
Elements of CLIP
| CLIP elements | Definition |
|---|---|
| Lung protective mechanical ventilation | Tidal volume between 6 and 8 ml/kg predicted body weight and plateau pressure <30 cm H2O; PEEP ≥5 cm H2O, minimise FiO2 (target oxygen saturation 88–92% after early shock) |
| Aspiration precautions | Rapid sequence intubation supervised by experienced providers, elevated head of the bed, oral care with chlorhexidine, gastric acid neutralisation in those not receiving tube feeds |
| Adequate empiric antimicrobial treatment and source control | According to suspected site of infection, healthcare exposure and immune suppression |
| Limiting fluid overload | Modified ARDSNet FACTT protocol after early shock (first 12 h) |
| Restrictive transfusion | Haemoglobin target >7 g/dl in the absence of acute bleeding and/or ischaemia |
| Appropriate handoff of patients at risk | Providers taking care of patients at risk who require ICU admission will complete a structured handoff to the ICU team to continue with CLIP protocol for the duration of ICU stay |
ARDSNet, Acute Respiratory Distress Syndrome Network; CLIP, checklist for lung injury prevention; FACTT, fluid and catheter treatment trial; FiO2, fraction of inspired oxygen concentration; ICU, intensive care unit; PEEP, positive end-expiratory pressure.
Related conditions and variables of interest: Additional conditions and variables of interest including pertinent baseline demographics and clinical characteristics such as age, sex, race, comorbidities and all LIPS elements will also be recorded. Additional variables of note will include vital signs and laboratory values that are obtained during the course of routine care, APACHE IV scores, coadministration of statins, ACE inhibitors and angiotensin-receptor blocking agents, insulin, amiodarone or steroids; blood product administration, daily fluid status and vasopressor requirements. A full description of the schedule of events for this study protocol can be seen in table 3.
Table 3.
Schedule of events
| Event | Time of presentation until first dose (screen/baseline) | First dose until end of that calendar day (Day 1) | Day 2 | Day 3 | Day 4 | Day 5 | Day 6 | Day 7 | 7 days after last dose | Hospital discharge or study Day 28, whichever comes first | 6 months | 12 months |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Informed consent | X | |||||||||||
| Inclusion/exclusion criteria | X | |||||||||||
| Pregnancy test in women of childbearing potential | X | |||||||||||
| Demographics | X | |||||||||||
| Medical history | X | |||||||||||
| LIPS score | X | |||||||||||
| Randomisation | X | |||||||||||
| Study drug administration | X | X | X | X | X | X | X | |||||
| Clinical outcome assessment | X | X | X | X | X | X | X | X | ||||
| Safety labs: Cr and Hb | X | X | X | X | X | X | X | |||||
| Clinical data as available: labs, ABG | X | X | X | X | X | X | X | X | ||||
| CXR/ABG* | X | X | X | X | X | X | X | |||||
| CLIP | X | X | X | X | X | X | X | X | ||||
| AE/SAE monitoring | X | X | X | X | X | X | X | X | X | |||
| Survival | X | X | ||||||||||
| Plasma biomarkers of ALI | X | X | X | |||||||||
| SF-12 | X | X | X | |||||||||
| Barthel Index | X | X | X | |||||||||
| Vulnerable Elders Survey | X | X | X | |||||||||
| Brussels/SOFA composite | X |
-
▪▪ Previous P/F ratio≥300, with current P/F ratio<300 and no CXR within 24 h.
-
▪▪ Prior P/F ratio<300 and the P/F ratio has fallen more than 10% AND no CXR within 24 h.
-
▪▪ In cases where an ABG is not available, the research team should obtain an ABG only if the S/F ratio falls below 315 consistently. The P/F ratio obtained from that ABG will be used to determine whether a CXR needs to be obtained (as per criteria outlined above).
-
▪▪ If change in P/F ratio triggers the need for a CXR or ABG as above, sites have 24 h to conduct the necessary procedure. An ABG or CXR obtained by the clinical team during that time period is also acceptable and obviates the need to obtain said procedure for the research study.
ABG, arterial blood gas; AE, adverse events; ALI, acute lung injury; ARDS, acute respiratory distress syndrome; CLIP, checklist for lung injury prevention; Cr, creatinine; Hb, haemoglobin; LIPS, Lung Injury Prevention Study; LIS, lung injury severity score; SAE, serious adverse events; SF-12, 12-Item Short-Form Health Survey; SOFA, sequential organ failure assessment.
Outcomes
Clinical Outcomes: The primary outcome is the development of ALI within 7 days of hospital admission. ALI will be defined as requirement for invasive mechanical ventilation and fulfilment of the American-European consensus definition for ALI/ARDS.27 Patients will be screened daily for respiratory failure and the partial pressure of arterial oxygen (PaO2) to fraction of inspired oxygen (FiO2) ratio will be calculated daily for those on mechanical ventilation. Patients ventilated with non-invasive ventilation will not be considered ALI/ARDS as our preliminary data showed that the majority (90%) of ALI patients are eventually intubated.8 Investigators at each site will review structured online training for assessment of ALI as was used and described in the LIPS.8 In addition, de-identified chest x-rays of the first five patients enrolled at each site will be sent to CCC for validation by the primary investigators. Any site with significant deviation will be retrained. Each participating centre's principal investigator will adjudicate the diagnosis of ALI/ARDS using standardised definitions. Patients receiving invasive mechanical ventilation who, within a given 24-h period, fulfil criteria for PaO2/FiO2<300 mm Hg, bilateral infiltrates consistent with ALI and not completely explained by heart failure, will be determined to have developed ALI. Given prior data suggesting poor agreement in the radiological interpretation of bilateral infiltrates on chest radiographs consistent with ALI,28 a secondary review of all ALI cases and a random sample of non-ALI cases will be performed by an independent expert investigator who is blinded to the initial ALI/ARDS adjudication. Study participants who die or are discharged from the hospital prior to day 7, and had not met criteria for ALI at the time of death or discharge, will be adjudicated as not having developed ALI.
Secondary clinical outcome assessments will include changes in the lung injury score and sequential organ failure assessment score, as well as the number of ventilator-free days at hospital day 28 and intensive care unit (ICU) and hospital lengths of stay. Mortality will be assessed at discharge from the ICU, from the hospital, and at 28 days. In addition, hospital survivors will undergo a brief follow-up phone survey to assess functional status (Barthel Index), health-related quality of life (QOL (SF-12)) and frailty (VES-13) at 6-months and 12-months after enrolment.
Mechanistic Outcomes: Secondary analyses will include evaluations of the mechanisms by which antiplatelet agents (eg, ASA) may modulate the development and progression of lung injury as well as a determination of the value of plasma biomarkers of lung injury in the prediction of ALI development in patients at risk (beyond clinical variables). The study will examine biomarkers previously found to be associated with the development of ALI/ARDS in at-risk individuals (table 4). In addition, to better understand the mechanisms by which ASA may affect the development and progression of ALI, the study will also examine the effect of ASA on ASA-triggered lipoxins, plasma thromboxane and platelet–neutrophil aggregates. As it is likely that other important biomarkers in ALI may be identified in the future, plasma from consenting patients will be banked at the biorepository for future studies. Blood samples will be obtained at baseline (after randomisation and before initiation of study intervention), on day 2 of study (approximately 24 h after the first dose of study drug) and on day 4 of study (any time during day 4). For patients who provide consent relating to future genetic analyses, appropriate samples will be obtained.
Table 4.
Plasma biomarkers in ALI/ARDS
| Plasma biomarker | Importance in ALI/ARDS development | Associated outcomes other than ALI/ARDS |
|---|---|---|
| Surfactant protein-D44–46 | Reflect injury and ↑ permeability of alveolar epithelium | VFD, organ failure |
| Receptor for advanced glycation end products47–49 | Reflects endothelial activation and injury | VFD,49 organ failure,49 ARDS after lung transplant47 |
| Intercellular adhesion molecule-144 50–53 | Reflects endothelial activation and injury | VFD,51 organ failure51 |
| Interleukin-644 54–56 | Inflammation | VFD,55 organ failure55 |
| Interleukin-844 48 50 54–56 | Inflammation | VFD,55organ failure55 |
| Plasminogen activator inhibitor-144 50 57–61 | Activation of coagulation and inhibition of fibrinolysis | VFD,61 organ failure61 |
| von Willebrand factor44 48 60 62 63 | Reflects endothelial activation and injury | Organ failure |
| Protein C44 50 59 61–64 | Activation of coagulation and inhibition of fibrinolysis | ARDS after lung transplant,47 VFD,61 organ failure61 |
ALI, acute lung injury; ARDS, acute respiratory distress syndrome; VFD, ventilator-free days.
Sample size estimation
The primary hypothesis for this investigation is that ASA (when compared to placebo) will result in a lower rate of incident ALI at day 7 following randomisation. To adequately address this hypothesis, the sample size is estimated to be 200 participants per group (400 total). The assumptions involved in this calculation include the following: (1) the hypothesised placebo response rate will be 18%,8 (2) the minimum clinically relevant effect is 10 percentage points, and (3) the type I error rate (α)=0.10 (two-sided; final α=0.0889 after interim analysis at 50% information fraction using O'Brien-Fleming-like αspending function). To be conservative during sample size estimation, the null proportion was shifted upwards to 25% (ie, towards the region of maximum binomial variance) so that the initial sample size estimates are based on 25% vs 15%. A χ2 test of proportions at the α=0.10 level of significance will have 80% power to detect the 10 percentage point difference with 197 participants per group. Overall recruitment is rounded to 200 participants per group (400 total) to allow for minor attrition, although attrition is not expected to affect the ascertainment of primary outcome. At the hypothesised level of 18% vs 8% and with the α adjusted for multiple interim looks, power with 200 participants per group is 90%. Thus, for the primary analysis 400 total participants randomised 1:1 to placebo or ASA is anticipated to yield sufficient power to detect a clinically relevant difference in the incidence of ALI.
The Data and Statistical Coordinating Center will prepare weekly reports on the accrual process for the trial. The reports, which will be reviewed on the weekly executive committee calls, will include summarisation of screening and randomisation metrics. Detailed descriptions of exclusion criteria for disqualified study candidates will be provided and reviewed as well. Each clinical centre has a target enrolment of two randomised participants per month. The reports will include a comparison of observed versus expected accrual, by clinical centre and overall for the trial. The randomisation performance of each clinical centre will be disseminated monthly to all study personnel through a study newsletter. If site-specific enrolment concerns are identified, methods for addressing these issues will be evaluated by the executive committee working with the site of interest. If a more pervasive and sustained gap between expected and observed participant accrual is identified, potential modifications to the inclusion and exclusion criteria of the protocol will be discussed. Any amendments to the inclusion and/or exclusion criteria deemed necessary by the executive committee will require approval by the Data and Safety Monitoring Board (DSMB) as well as the institutional review board (IRB) of each participating institution before implementation. If enrolment remains below plan, the inclusion of additional clinical sites will be considered as well.
Randomisation and blinding
LIPS-A will utilise centralised randomisation software hosted by the Data and Statistical Coordinating Center. Randomisation through the electronic data management system will be enabled upon electronic verification of inclusion and exclusion criteria and enrolment of the study participant by the clinical site investigators. Enrolled participants will be randomised in a 1:1 ratio to the ASA or placebo treatment arm using dynamic minimisation29 with a second guess probability of 0.2. Randomisation will be stratified by centre. To maintain the double blind for the study, only the research pharmacist at each centre will have electronic access to the unblinded treatment code for study medication preparation and dispensing. The rest of the site investigators and coordinating centres will be blinded to the actual treatment assignment. Emergency unblinding is available electronically and through dispensing records at each pharmacy.
In the event the electronic randomisation system is not functioning, the research pharmacist at each centre has a sealed emergency randomisation kit to enable offline randomisation. A manual of operation governs the use of the emergency randomisation process. Briefly, prior to use of the emergency process, approval of the coordinating centres is required. All attempts will be made to recover the system prior to the use of the offline procedure. Should the offline procedure be used, the electronic data management system will be updated to reflect the treatment assignment using the identification number contained within the randomisation kit.
Statistical methods
Conditional logistic regression will be used to test the primary hypothesis that early ASA administration will decrease the rate of ALI development. Clinical site will be treated as the stratification variable and conditioned out of the estimating equations. This approach is optimal in a clinical trial setting as it provides a test of null hypothesis that the ALI incidence is equal in the two treatment group and estimates the association in the event the null hypothesis is rejected (through the conditional OR estimate). SAS PROC LOGISTIC (Cary, North Carolina, USA) will be used for estimation of the primary model.
This analysis will be supplemented by the Cochran-Mantel-Haenszel stratified analysis with ORs computed for each site. The Breslow-Day test will be used to examine the data for potential effect modification (ie, a ‘site effect’). In the event there is significant site-to-site variability in the estimated effect, stratified results will be reported for this phase II study. Evidence of heterogeneity of response at this phase of study will yield invaluable preliminary data for the planning of future changes.
Planned interim analyses will be conducted at 50% of study participants enrolled. With the O'Brien-Fleming-like stopping boundaries, a final adjusted α of 0.08885 is anticipated; however, the final value may be changed depending on unplanned interim analyses (conducted at the request of the DSMB) or slight deviations from the anticipated information milestones (0.5 and 1). Stopping boundaries will be estimated using the LD Bounds package for the R system.
For the remaining continuous and dichotomous secondary endpoints, treatment group comparisons will be performed with respect to clinical outcomes as well as important prognostic factors at screening, baseline and individual follow-up time points during the study duration. For continuous variables (eg, age, weight and laboratory assays), linear model techniques including t-tests, analysis of variance and analysis of covariance will be applied. Non-parametric procedures (eg, the Wilcoxon rank sum test), will be used if data are not normally distributed and transformations of the data are not considered useful. Standard techniques for categorical data will be applied, including Fisher's exact test, Pearson χ2 procedures, weighted least squares and logistic regression analysis.
Longitudinal (or serially measured) endpoints will be evaluated by generalised linear models and linear mixed. Repeated measure analyses of binary endpoints will be analysed using generalised estimating equations methods which do not require imputation of missing values, provided the data are ignorable missing.30 Continuous-dependent variables will utilise the mixed model approach with emphasis on evaluating the trajectories of values over time. However, early improvement in these parameters may suggest a supportive, stabilising role for ASA as a treatment option in patients at high risk of ALI. For the primary analysis, the clinical centre will be treated as a ‘nuisance’ parameter and conditioned out of the estimation routine. For secondary analyses, the clinical centre will be used as a fixed covariate to account for differences across sites.
The safety endpoints (see below Adverse outcomes section) will be examined for all participants in the safety evaluable analysis set. Safety endpoints will include expected clinical events, including death, for this patient population and summarised by the treatment group. Also, all serious and unexpected adverse events will be summarised by the treatment group. Fisher's exact test will be used to estimate treatment differences in the incidence of each specified adverse event. No adjustments will be made for multiple hypothesis evaluations of safety endpoints. Adverse events will be summarised with groupings by body system. Other safety data (eg, labs and assay data) will be listed, and when appropriate, summarised in tabular or graphical format.
Data quality and management
This investigation will utilise the Medidata Rave system for data management and storage as well as to assist with the randomisation procedures. This product has been designed to facilitate multicentre clinical trials conducted under 21 Code of Federal Regulations (CFRs) Part 11 requirements. This secure, web-based system provides robust data validation routines, custom reporting and straightforward integration with statistical software packages such as SAS (utilised for this investigation). The system is coupled with an integrated randomisation module that uses a multidimensional dynamic allocation algorithm to minimise imbalances across multiple dimensions including overall study, sites, factors and cross-factor strata. Specific details regarding the randomisation process are given above.
Ethics and dissemination
Adverse outcomes
Safety data including adverse events such as gastrointestinal ulcers, bleeding from any site, gastrointestinal discomfort, wheezing, rash, hives, angioedema, tinnitus and mortality will be recorded. Adverse events will be defined as ‘unexpected,’ ‘expected,’ and ‘serious.’ As our patient population is by definition ‘critically ill,’ it is expected that they will have a number of unrelated adverse health events during the course of their hospital stay. Therefore, we will limit the scope of our adverse event monitoring and recording to the following:
- Serious adverse events (SAEs) will be defined as
-
▸Death, believed to be related to the study medication or procedures, or a death that is unexpected considering the acuity of a patient.
-
▸A life-threatening experience believed to be related to the study medication or procedures.
-
▸Persistent or significant disability or incapacity that is of greater frequency or severity than what would be normally expected in the course of critical illness.
-
▸An event that jeopardises the human subject and may require medical or surgical treatment to prevent one of the preceding outcomes and is not expected in the course of critical illness.
-
▸
- Adverse events possibly related to ASA administration will be defined as
-
▸Anaphylaxis/allergic reaction.
-
▸Gastrointestinal bleed/bleeding complications.
-
▸Transfusion requirements for suspected bleeding.
-
▸Acute kidney injury, defined as RIFLE stage ‘I’ or greater.
-
▸Tinnitus.
-
▸Reye's syndrome.
-
▸
Role of the data safety and monitoring board
Reporting of SAEs will be conducted through the CCC. All centres will report SAEs within 24 h of discovering the presence of the SAE. The CCC will report all potentially related SAEs to the DSMB and to NHLBI within 7 days of discovery. A summary report of the events will be provided to the DSMB prior to each DSMB meeting, at least every 6 months. Safety oversight will be under the direction of a DSMB whose members will be independent from the study operations. The safety endpoints will be examined for all eligible patients who sign informed consent and are enrolled in the study on an intent-to-treat basis. Safety endpoints will include expected clinical events, including death, for this patient population and summarised by the treatment group. All serious and unexpected adverse events will be summarised by the treatment group as well.
Ethics approval
Approval of the protocol was obtained from the data safety and monitoring board as well as from NHLBI prior to enrolling the first study participant. In addition, approval of both the protocol and informed consent documents was required and obtained from the institutional review board of each participating institution prior to enrolling study participants at the respective study site. To ensure that each participating institution's informed consent documentation complied with NHLBI requirements and the CFRs Title 21 Part 50 Section 50.25, all informed consent forms were reviewed and approved by the CCC. Official documentation of all IRB approvals and all finalised informed consent forms have been collected and stored by the CCC.
Considerations for continuation to a phase III clinical trial
The decision to proceed with a phase III trial is formally outlined as follows:
Initiate Phase III Study: Demonstrated efficacy signal in addition to adequate safety profile. Criteria: Early termination for benefit at interim analysis or p<0.08885 at final analysis (α=0.10 for study). Serious adverse event profile of ASA not statistically worse than placebo (95% CI for the relative risk of any SAE covers the null value of RR=1.0).
Further Development Potentially Required: Weak efficacy signal. Criteria: Primary endpoint did not achieve a priori level of significance but there were at least a general consistency of secondary endpoints indicating propensity for efficacy with a larger sample size and/or more specific primary endpoint.
Abandon Treatment Platform: Harm (in efficacy or safety endpoints). Criteria: Study terminated early per recommendation by DSMB for safety and/or risk/benefit ratio concerns (ie, stop for futility, harm, unacceptable risk profile, etc).
Ancillary studies
The LIPS-A group will encourage investigator-initiated ancillary study proposals that extend or complement the specific aims of the primary LIPS-A trial. As policy, all proposals will be reviewed by a separate Ancillary Studies and Publications Committee, both to ensure consistency with the goals and conduct of the main study and evaluate scientific merit and validity. Proposed studies may utilise data and/or samples already accrued during the LIPS-A trial or, when feasible, request additional data collection from participating sites. The investigative and statistical plan will be reviewed a priori, with committee approval required before analysis begins. Where equivocal, review decisions will be referred to the LIPS-A Executive Committee. All reports, manuscripts or presentations derived from data obtained through the ancillary study process will require review and approval by the Ancillary Studies and Publications Committee prior to submission.
Protocol funding and role of the funding sources
This study is supported by the National Institutes of Health-National Heart Lung and Blood Institute (Grant Number U01-HL108712-01), the Mayo Clinic Center for Translational Science Activities (Grant Number KL2 RR024151) and the Mayo Clinic Critical Care Research Committee. Specifically, funding has been provided by each of these entities to support study personnel time and effort, protocol and data management development (Medidata Rave), sample acquisition, processing and storage and statistical support. These funding sources have had no specific influence on the scientific content of the study protocol. Similarly, the funding sources will have no direct role in the study conduct, nor data collection, analyses or interpretation. The funding sources will also have no role in the writing or presentation of study results, nor decisions to submit for publication. The ultimate authority over each of these activities will be the executive committee of the LIPS-A study.
Discussion
We have presented the study protocol and data analysis plans for the first phase II, multicentre randomised clinical trial that will test the efficacy and safety of a promising ALI prevention agent. Specifically, we have hypothesised that early administration of ASA to hospitalised patients who are at high risk of ALI, will be safe and will reduce the likelihood of progression to the full ALI phenotype. Secondarily, this investigation will glean important mechanistic data on ASA's impact on the pathways believed important in ALI pathogenesis as well as the potential value of relevant biomarkers in the prediction of subsequent development of ALI. Finally, the results of this study will provide essential information on both the scientific merit and feasibility of a larger, phase III trial testing the role of ASA in the prevention of lung injury.
The persistent difficulty in translating promising preclinical therapies into the clinical setting has fostered interest in the potential development of effective ALI prevention strategies. Indeed, prevention of ALI has been identified as a key strategic priority for invested parties such as the NHLBI.31 However, implementation of protocols aiming to test potential ALI prevention strategies have been historically hindered by an inability to accurately predict who is at risk for ALI. Moreover, the typically short interval between risk exposure and development of ALI as well as the small proportion of patients who progress to the full ALI phenotype following an ALI-related exposure has limited the feasibility of ALI prevention studies. In addition, the historic lack of standardisation for numerous important co-interventions that confound the associations of interest (eg, ventilator management, transfusion and resuscitation practices) has also limited our ability to test preventative strategies.
To this end, the recently validated LIPS score is a key element of the herein described study protocol.8 Specifically, the LIPS score is expected to facilitate the identification of patients at greatest risk of progressing to ALI (an LIPS score ≥4 is expected to identify a subgroup of patients who have a risk of progressing to ALI that is greater than 18%). In addition, it is notable that this ALI risk assessment tool was validated using data collected within the first 6 h after the initial evaluation in the ED. In an ALI prevention protocol such as described herein, where the time to randomisation is limited to 12 h from presentation to the ED, the ability to accurately determine risk for ALI in such a time-efficient manner is critical.
A second notable strength of the current protocol is expected to be the implementation of the CLIP for standardising important co-interventions that may otherwise confound our association of interest (ASA and ALI). During the period between hospital admission and the development of ALI, healthcare delivery factors (timely treatment of infection and shock, appropriate administration of fluid and transfusion therapies, prevention of aspiration, avoidance of large tidal volume ventilation), may be as important as individual biology in determining ALI development and outcome.32–39 Moreover, a recent survey noted wide variation in clinical practices such as the existence of a sepsis protocol, use of low tidal volume ventilation, positive end-expiratory pressure and restrictive transfusion practices, between hospitals and among the ED, ICU and operating room within hospitals.40 Thus, to effectively investigate preventive strategies in ALI, the standardisation of care delivery during the early phase of hospitalisation would appear critical. Indeed, the ARDSNet investigators have repeatedly shown the value of standardisation of clinical processes for ALI patients in clinical trials, allowing for determination of incremental benefit of new interventions.41 42 In the current investigation, standardisation of care with best practices will help to reduce variability in the rates of ALI and the intensity of lung injury (noise) due to inconsistencies in care delivery. The result is expected to be an increased chance of seeing a beneficial clinical or biological effect from ASA and a better assessment of the potential side effects of ASA in this population.
Although the multicentre randomised clinical trial design, availability of a time-efficient risk assessment tool (LIPS score) and the standardisation of important co-interventions with CLIP, as well as the robust study support and quality control offered through Metadata Rave, are clear strengths of the current study protocol, several important limitations with the planned investigation are worth being noted. Lung injury may be present at study entry even as clinical criteria for ALI are not fulfilled. Though a formal diagnosis of prevalent ALI is exclusionary, the molecular machinery will have been clearly set in motion in many of the study participants. Therefore, the study may be more accurately characterised as a prevention/early treatment trial rather than a pure prevention trial. Nonetheless, we have attempted to focus on the early period of ALI development by mandating a short interval from hospital presentation to randomisation (12 h) and a similarly short interval from hospital presentation to administration of the first study dose (24 h). In addition, the study will exclude patients who presented to an outside hospital ED more than 12 h before arrival at the enrolling site's facility. The study will also exclude those with ALI on hospital presentation or prior to randomisation as well as those who are receiving mechanical ventilation through a tracheostomy tube prior to the current hospital admission (patient who is ventilator dependent) or those with a history of interstitial lung disease with chronic pulmonary infiltrates that may mimic ALI.
A second limitation relates to the intervention of ASA administration. Specifically, it is now well documented that more than 10% of the population will have a variable response to ASA or at least some form of ASA resistance.17 These patients may not benefit from ASA, even if ASA can modulate the development of lung injury. However, as part of this study, we will measure plasma thromboxane, a sensitive indicator of ASA resistance, to determine the prevalence of ASA resistance in patients at high risk of ALI. As such, sensitivity analyses, stratifying study participants by ASA resistance (as determined by changes in thromboxane levels), may allow us to determine whether the effect of ASA on ALI development is isolated to those susceptible to the actions of ASA. A related concern is the potential influence of concomitant medications that may impact on ASA's ability to prevent or mitigate ALI (eg, statins and corticosteroids). To address this concern, we will be collecting detailed information on concomitant medications and, when necessary, appropriate statistical adjustments will be made.
A third potential limitation with this study relates to a previously recognised major barrier to ALI prevention studies, namely feasibility. First and foremost, a substantial proportion of the target population may be expected to be receiving ASA on presentation to the ED, an exclusion criteria for the current protocol. Notably, however, our preliminary work suggests that upwards of two-thirds of the target population was not on ASA prior to admission. We also note that over the 3 months of the initial LIPS,8 there were 800 patients who fulfilled study inclusion criteria of LIPS score ≥4 and did not fulfil the exclusion criteria of pre-existing ASA use, prevalent ALI and elective surgery. Therefore, we believe that with 14 proposed sites and 2 years of planned enrolment, we will successfully meet our enrolment goals of 400 total patients. Also relating to feasibility, it is possible that some sites will be challenged by the short time interval allowed for patient enrolment as well as the short time to study drug administration. Though a valid concern, we believe the use of the LIPS score and the robust support offered through Metadata Rave will greatly facilitate the enrolment and randomisation procedures such that sites will indeed be successful in meeting these time-sensitive challenges.
A fourth and final limitation which deserves mention relates to the potential toxicity of the intervention of interest. Generally, ASA is well tolerated even in acutely ill, hospitalised patients in whom ASA is often continued during the hospitalisation. As an example, in a study of ASA use up to the time of cardiac surgery, its continuation was not associated with an increased need for transfusion therapies.43 Nevertheless, there may be injury associated with the administration of ASA. To address this concern, patients at risk for major complications from ASA therapy have been excluded from the study. Multiple stopping criteria for patients who experience adverse events have also been incorporated into the protocol. In addition, the more complete understanding of the safety profile of an intervention of interest is an important goal of all phase II trials. In this regard, the information gleaned from this study, adverse events included, is necessary to help decide on the merits of proceeding to a phase III clinical trial.
Conclusion
This manuscript describes the study protocol and analysis plans for the first phase II randomised clinical trial of the promising ALI prevention agent ASA. In addition to providing important information on the safety and efficacy of ASA in patients at high risk for ALI, the results of this trial will also inform the scientific community regarding the merit and feasibility of a more definitive phase III clinical trial. Importantly, the significance of this effort lies not only in the specific results which will be obtained from the study protocol, but equally in the infrastructure that will be created to facilitate the conduct of this trial. Specifically, the development and utilisation of innovative methods to facilitate the early identification of high-risk patients with the LIPS and the standardisation of potential confounding co-interventions with CLIP will address key barriers to studying ALI prevention measures and is expected to lay a framework for the meaningful conduct of future ALI prevention studies as well.
Supplementary Material
Appendix
See table A1.
Footnotes
Contributors: DJK has contributed to all aspects of the study design and is the principal investigator at the Data and Statistical Coordinating Center. DT has contributed to all aspect of the study design and is the principal investigator at the Clinical Coordinating Center. VMB-G is the lead study coordinator at the Clinical Coordinating Center and has contributed to all aspects of the study protocol design as well as preparations for protocol implementation. REC is the lead statistician for this protocol. He has been involved in all aspects of the study design. He is the primary author of statistical descriptions in this manuscript and is the lead study coordinator at the Data and Statistical Coordinating Center. He has contributed to all aspects of the study protocol design and preparations for protocol implementation. PP has contributed in a consulting role to all aspects of the study design and is the primary author of the sections of this manuscript which detail the protocol's plans regarding ancillary studies. OG has contributed to all aspects of the study design and is the principal investigator for the grant mechanism that is the primary funding source for this protocol (Grant Number U01-HL108712-01). MNG has contributed to all aspects of the study design. She is the principal investigator for the Biorepository and Knowledge Translation Center. All named authors wrote or revised the manuscript and approved its final submitted version.
Funding: The funding was supported by National Institutes of Health. This study is supported by Grant Numbers U01-HL108712-01, KL2 RR024151, and the Mayo Clinic Critical Care Research Committee. This protocol is registered with ClinicalTrials.gov, registration number NCT01504867.
Competing interests: None.
Patient consent: Patients will sign institutional informed consent prior to enrolment in the study.
Ethics approval: Mayo Clinic Institutional Review Board.
Provenance and peer review: Not commissioned; internally peer reviewed.
References
- 1.Rubenfeld GD, Caldwell E, Peabody E, et al. Incidence and outcomes of acute lung injury. N Engl J Med 2005;353:1685–93 [DOI] [PubMed] [Google Scholar]
- 2.Li G, Malinchoc M, Cartin-Ceba R, et al. Eight-year trend of acute respiratory distress syndrome: a population-based study in Olmsted County, Minnesota. Am J Resp Crit Care Med 2011;183:59–66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Erickson SE, Martin GS, Davis JL, et al. Recent trends in acute lung injury mortality: 1996–2005. Crit Care Med 2009;37:1574–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Herridge MS, Tansey CM, Matté A, et al. Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med 2011;364:1293–304 [DOI] [PubMed] [Google Scholar]
- 5.Hudson LD, Milberg JA, Anardi D, et al. Clinical risks for development of the acute respiratory distress syndrome. Am J Respir Crit Care Med 1995;151:293–301 [DOI] [PubMed] [Google Scholar]
- 6.Fowler AA, Hamman RF, Good JT, et al. Adult respiratory distress syndrome: risk with common predispositions. Ann Intern Med 1983;98:593–7 [DOI] [PubMed] [Google Scholar]
- 7.Gong MN, Thompson BT, Williams P, et al. Clinical predictors of and mortality in acute respiratory distress syndrome: potential role of red cell transfusion. Crit Care Med 2005;33:1191–8 [DOI] [PubMed] [Google Scholar]
- 8.Gajic O, Dabbagh O, Park PK, et al. Early identification of patients at risk of acute lung injury: evaluation of lung injury prediction score in a multicenter cohort study. Am J Respir Crit Care Med 2010;183:462–70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zarbock A, Ley K. The role of platelets in acute lung injury (ALI). Front Biosci 2009;14:150–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zarbock A, Polanowska-Grabowska RK, Ley K. Platelet-neutrophil-interactions: linking hemostasis and inflammation. Blood Rev 2007;21:99–111 [DOI] [PubMed] [Google Scholar]
- 11.Looney MR, Nguyen JX, Hu Y, et al. Platelet depletion and aspirin treatment protect mice in a two-event model of transfusion-related acute lung injury. J Clin Invest 2009;119:3450–61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.El Kebir D, József L, Pan W, et al. 15-epi-lipoxin A4 inhibits myeloperoxidase signaling and enhances resolution of acute lung injury. Am J Respir Crit Care Med 2009;180:311–19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fukunaga K, Kohli P, Bonnans C, et al. Cyclooxygenase 2 plays a pivotal role in the resolution of acute lung injury. J Immunol 2005;174:5033–9 [DOI] [PubMed] [Google Scholar]
- 14.Maderna P, Godson C. Lipoxins: resolutionary road. Br J Pharmacol 2009;158:947–59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chelucci GL, Boncinelli S, Marsili M, et al. Aspirin effect on early and late changes in acute lung injury in sheep. Intensive Care Med 1993;19:13–21 [DOI] [PubMed] [Google Scholar]
- 16.Sigurdsson GH, Vallgren S, Christenson JT. Influence of aspirin and steroids on acute lung injury after i.v. injection of a sclerosing agent . Acta Chir Scand 1989;155:163–70 [PubMed] [Google Scholar]
- 17.Yasuda O, Takemura Y, Kawamoto H, et al. Aspirin: recent developments. Cell Mol Life Sci 2008;65:354–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jin SW, Zhang L, Lian QQ, et al. Posttreatment with aspirin-triggered lipoxin A4 analog attenuates lipopolysaccharide-induced acute lung injury in mice: the role of heme oxygenase-1. Anesth Analg 2007;104:369–77 [DOI] [PubMed] [Google Scholar]
- 19.Tabuchi A, Kuebler WM. Endothelium-platelet interactions in inflammatory lung disease. Vasc Pharmacol 2008;49:141–50 [DOI] [PubMed] [Google Scholar]
- 20.Grommes J, Alard J-E, Drechsler M, et al. Disruption of platelet-derived chemokine heteromers prevents neutrophil extravasation in acute lung injury. Am J Resp Crit Care Med 2012;185:628–36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Clark SR, Ma AC, Tavener SA, et al. Platelet TLR4 activates neutrophil extracellular traps to ensnare bacteria in septic blood. Nature Med 2007;13:463–9 [DOI] [PubMed] [Google Scholar]
- 22.Narasaraju T, Yang E, Samy RP, et al. Excessive neutrophils and neutrophil extracellular traps contribute to acute lung injury of influenza pneumonitis. Am J Pathol 2011;179:199–210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Erlich JM, Talmor DS, Cartin-Ceba R, et al. Prehospitalization antiplatelet therapy is associated with a reduced incidence of acute lung injury. A population-based cohort study. Chest 2011;139:289–95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kor DJ, Erlich J, Gong MN, et al. Association of prehospitalization aspirin therapy and acute lung injury: results of a multicenter international observational study of at-risk patients. Crit Care Med 2011;39:2393–400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Patrono C, Garcia Rodriguez LA, Landolfi R, et al. Low-dose aspirin for the prevention of atherothrombosis. N Engl J Med 2005;353:2373–83 [DOI] [PubMed] [Google Scholar]
- 26.Chiang N, Bermudez EA, Ridker PM, et al. Aspirin triggers antiinflammatory 15-epi-lipoxin A4 and inhibits thromboxane in a randomized human trial. Proc Natl Acad Sci USA 2004;101:15178–83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bernard GR, Artigas A, Brigham KL, et al. The American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med 1994;149:818–24 [DOI] [PubMed] [Google Scholar]
- 28.Rubenfeld GD. Interobserver variability in applying a radiographic definition for ARDS. Chest 1999;116:1347–53 [DOI] [PubMed] [Google Scholar]
- 29.Pocock SJ, Simon R. Sequential treatment assignment with balancing for prognostic factors in the controlled clinical trial. Biometrics 1975;31:103–15 [PubMed] [Google Scholar]
- 30.Diggle P, Liang K, Zeger S. Analysis of longitudinal data. New York: Oxford University Press, Inc., 1994 [Google Scholar]
- 31.Spragg RG, Bernard GR, Checkley W, et al. Beyond mortality: future clinical research in acute lung injury. Am J Respir Crit Care Med 2010;181:1121–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gajic O, Dara SI, Mendez JL, et al. Ventilator-associated lung injury in patients without acute lung injury at the onset of mechanical ventilation. Crit Care Med 2004;32:1817–24 [DOI] [PubMed] [Google Scholar]
- 33.Rana R, Fernandez-Perez ER, Khan SA, et al. Transfusion-related acute lung injury and pulmonary edema in critically ill patients: a retrospective study. Transfusion 2006;46:1478–83 [DOI] [PubMed] [Google Scholar]
- 34.Gajic O, Rana R, Winters JL, et al. Transfusion-related acute lung injury in the critically ill: prospective nested case-control study. Am J Respir Crit Care Med 2007;176:886–91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gajic O, Rana R, Mendez JL, et al. Acute lung injury after blood transfusion in mechanically ventilated patients. Transfusion 2004;44:1468–74 [DOI] [PubMed] [Google Scholar]
- 36.Gajic O, Frutos-Vivar F, Esteban A, et al. Ventilator settings as a risk factor for acute respiratory distress syndrome in mechanically ventilated patients. Intensive Care Med 2005;31:922–6 [DOI] [PubMed] [Google Scholar]
- 37.Gajic O, Dzik WH, Toy P. Fresh frozen plasma and platelet transfusion for nonbleeding patients in the intensive care unit: benefit or harm? Crit Care Med 2006;34:S170–3 [DOI] [PubMed] [Google Scholar]
- 38.Fernandez-Perez ER, Keegan MT, Brown DR, et al. Intraoperative tidal volume as a risk factor for respiratory failure after pneumonectomy. Anesthesiology 2006;105:14–18 [DOI] [PubMed] [Google Scholar]
- 39.Khan H, Belsher J, Yilmaz M, et al. Fresh-frozen plasma and platelet transfusions are associated with development of acute lung injury in critically ill medical patients. Chest 2007;131:1308–14 [DOI] [PubMed] [Google Scholar]
- 40.Hou P, Cohen J, Elie-Turenne M, et al. A survey on behalf of USCIITG-LIPS investigators: toward standardization of a checklist for lung injury prevention (CLIP). Crit Care Med 2010;38:576 [Google Scholar]
- 41.Brower RG, Lanken PN, MacIntyre N, et al. Higher versus lower positive end-expiratory pressures in patients with the acute respiratory distress syndrome. N Engl J Med 2004;351:327–36 [DOI] [PubMed] [Google Scholar]
- 42.Wiedemann HP, Wheeler AP, Bernard GR, et al. Comparison of two fluid-management strategies in acute lung injury. N Engl J Med 2006;353:2564–75 [DOI] [PubMed] [Google Scholar]
- 43.Gerrah R, Elami A, Stamler A, et al. Preoperative aspirin administration improves oxygenation in patients undergoing coronary artery bypass grafting. Chest 2005;127:1622–6 [DOI] [PubMed] [Google Scholar]
- 44.Ware LB, Koyama T, Billheimer DD, et al. Prognostic and pathogenetic value of combining clinical and biochemical indices in patients with acute lung injury. Chest 2010;137:288–96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Eisner M, Parsons P, Matthay M, et al. Plasma surfactant protein levels and clinical outcomes in patients with acute lung injury. Thorax 2003;58:983–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Greene KE, Wright JR, Steinberg KP, et al. Serial changes in surfactant-associated proteins in lung and serum before and after onset of ARDS. Am J Respir Crit Care Med 1999;160:1843–50 [DOI] [PubMed] [Google Scholar]
- 47.Christie JD, Shah CV, Kawut SM, et al. Plasma levels of receptor for advanced glycation end products, blood transfusion, and risk of primary graft dysfunction. Am J Respir Crit Care Med 2009;180:1010–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Fremont RD, Koyama T, Calfee CS, et al. Acute lung injury in patients with traumatic injuries: utility of a panel of biomarkers for diagnosis and pathogenesis. J Trauma 2010;68:1121–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Calfee CS, Ware LB, Eisner MD, et al. Plasma receptor for advanced glycation end products and clinical outcomes in acute lung injury. Thorax 2008;63:1083–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.McClintock D, Zhuo H, Wickersham N, et al. Biomarkers of inflammation, coagulation and fibrinolysis predict mortality in acute lung injury. Crit Care 2008;12:R41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Calfee CS, Eisner MD, Parsons PE, et al. Soluble intercellular adhesion molecule-1 and clinical outcomes in patients with acute lung injury. Intensive Care Med 2009;35:248–57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Agouridakis P, Kyriakou D, Alexandrakis MG, et al. The predictive role of serum and bronchoalveolar lavage cytokines and adhesion molecules for acute respiratory distress syndrome development and outcome. Respir Res 2002;3:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Covarrubias M, Ware LB, Kawut SM, et al. Plasma intercellular adhesion molecule-1 and von Willebrand factor in primary graft dysfunction after lung transplantation. Am J Transplant 2007;7:2573–8 [DOI] [PubMed] [Google Scholar]
- 54.Bouros D, Alexandrakis MG, Antoniou KM, et al. The clinical significance of serum and bronchoalveolar lavage inflammatory cytokines in patients at risk for acute respiratory distress syndrome. BMC Pulm Med 2004;4:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Parsons PE, Eisner MD, Thompson BT, et al. Lower tidal volume ventilation and plasma cytokine markers of inflammation in patients with acute lung injury. Crit Care Med 2005;33:1–6 [DOI] [PubMed] [Google Scholar]
- 56.Meduri GU, Headley S, Kohler G, et al. Persistent elevation of inflammatory cytokines predicts a poor outcome in ARDS. Plasma IL-1 beta and IL-6 levels are consistent and efficient predictors of outcome over time. Chest 1995;107:1062–73 [DOI] [PubMed] [Google Scholar]
- 57.Prabhakaran P, Ware LB, White KE, et al. Elevated levels of plasminogen activator inhibitor-1 in pulmonary edema fluid are associated with mortality in acute lung injury. Am J Physiol Lung Cell Mol Physiol 2003;285:L20–8 [DOI] [PubMed] [Google Scholar]
- 58.Ware LB, Fang X, Matthay MA. Protein C and thrombomodulin in human acute lung injury. Am J Physiol Lung Cell Mol Physiol 2003;285:L514–21 [DOI] [PubMed] [Google Scholar]
- 59.Christie JD, Robinson N, Ware LB, et al. Association of protein C and type 1 plasminogen activator inhibitor with primary graft dysfunction. Am J Respir Crit Care Med 2007;175:69–74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ware LB, Conner ER, Matthay MA. von Willebrand factor antigen is an independent marker of poor outcome in patients with early acute lung injury. Crit Care Med 2001;29:2325–31 [DOI] [PubMed] [Google Scholar]
- 61.Ware LB, Matthay MA, Parsons PE, et al. Pathogenetic and prognostic significance of altered coagulation and fibrinolysis in acute lung injury/acute respiratory distress syndrome. Crit Care Med 2007;35:1821–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Rubin DB, Wiener-Kronish JP, Murray JF, et al. Elevated von Willebrand factor antigen is an early plasma predictor of acute lung injury in nonpulmonary sepsis syndrome. J Clin Invest 1990;86:474–80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ware LB, Eisner MD, Thompson BT, et al. Significance of von Willebrand factor in septic and nonseptic patients with acute lung injury. Am J Respir Crit Care Med 2004;170:766–72 [DOI] [PubMed] [Google Scholar]
- 64.Matthay MA, Ware LB. Plasma protein C levels in patients with acute lung injury: prognostic significance. Crit Care Med 2004;32:S229–32 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.