Abstract
Objectives:
Spontaneous bacterial peritonitis (SBP) is associated with a high mortality rate. After antibiotic therapy, improvement in fluid polymorphonuclear (PMN) cell count is expected within 2 days. However, our institution recognized cases unresponsive to standard treatment.
Methods:
To study these recalcitrant cases, we completed a retrospective chart review of patients admitted for SBP to the University of Chicago from 2002 to 2007. SBP was defined by an ascitic PMN cell count ≥250/ml.
Results:
Of 55 patients with SBP, 15 did not show improvement in fluid PMN cell count to below 250/ml with standard treatment, leading to a prevalence of 27%. The patients with persistent SBP were younger than those with nonpersistent SBP [mean (SD) 51.80 (9.84) compared with 58.13 (8.79); p = 0.0253]. Persistent SBP had a higher serum ascites albumin gradient (SAAG) [median (Q1, Q3) 1.85 (1.50, 2.41) compared with 1.10 (0.60, 1.60)] and a higher score in the model for end-stage liver disease (MELD) [mean (SD) 27.98 (8.09) compared with 22.22 (8.10)] than nonpersistent SBP patients; p = 0.027 and p = 0.023, respectively. In addition, persistent SBP patients were more likely to have a positive ascitic fluid culture than nonpersistent SBP patients [odds ratio (OR) (95% CI) 4.33 (1.21, 15.47); p = 0.024]. Importantly, in-hospital mortality in the persistent SBP group was 40%, compared with 22.5% in the nonpersistent SBP group [OR = 2.30 (0.64, 8.19); p = 0.20].
Conclusions:
The risk of persistent SBP is nearly 40% in patients with MELD score >25, SAAG >1.5 or positive ascitic fluid culture. Furthermore, patients who develop persistent SBP tend to experience a higher mortality rate. This study underscores the importance of further examination of this vulnerable population.
Keywords: ascites, cirrhosis, model for end-stage liver disease (MELD) score, portal hypertension, spontaneous bacterial peritonitis
Background and aims
The most frequent infectious complication in patients with cirrhosis of the liver is spontaneous bacterial peritonitis (SBP), occurring with a prevalence of 10–35%, followed by urinary tract infection, pneumonia and bacteremia [Borzio et al. 2001]. SBP, first described in 1970, is defined as the presence of an infection of ascitic fluid in the absence of a visceral perforation and intra-abdominal focus of inflammation.
Although it is a common complication of cirrhosis, SBP is also serious. It is now associated with in-hospital mortality rates ranging from 20% to 40% [Thuluvath et al. 2001]. Furthermore, mortality rates 1 and 2 years after an episode of SBP are reported to be 50–70% and 70–75%, respectively [Rimola et al. 2000]. However, mortality after SBP has been improving, largely owing to early diagnosis and prompt treatment with empiric antibiotics.
The diagnosis of SBP is established by ascitic fluid analysis. The most common marker of infection is an ascites fluid polymorphonuclear (PMN) cell count of 250/ml or more [Runyon, 2009]. In a recent meta-analysis, the negative likelihood ratio for SBP if the PMN cell count was greater than 250/ml was 0.2 [Wong et al. 2008]. Although ascitic fluid culturing is an important diagnostic test, the use of culture results to diagnose SBP would delay therapy, and ascitic fluid culture is negative in as many as 60% of patients [Runyon, 2009]. In addition, culture-negative neutrocytic ascites is generally treated identically to typical SBP, as the natural progression mirrors that for culture-positive neutrocytic ascites [Kim et al. 2010; Lata et al. 2009; Runyon, 2009].
Several studies document an exponential decline in PMN cell count after initiation of antibiotic therapy [Angeloni et al. 2008; Ljubicic et al. 2000; Fong et al. 1989]. Currently, the AASLD guidelines do not recommend repeat paracentesis to confirm improvement in fluid PMN cell count and fluid sterility unless clinically warranted [Runyon, 2009]. Although a response to therapy can be evaluated by clinical criteria, an important parameter remains a dramatic decrease in the ascitic fluid PMN cell count after 2 days of therapy [Caruntu and Benea, 2006; Rimola et al. 2000; Runyon, 1986]. Many clinicians and current guidelines recommend using clinical signs of improvement or a 25–50% decrease in ascitic fluid PMN cell count after 2 days of antibiotic treatment to document response to therapy [EASL, 2010; Runyon, 2009; Tandon and Garcia-Tsao, 2008]. However, small studies reveal that the failure of the PMN cell count to drop below 250/ml results in higher mortality and higher recurrence rates of SBP [Castellote et al. 2010; Angeloni et al. 2008; Cereto et al. 2008; Cho et al. 2007; Ljubicic et al. 2000; Fong et al. 1989].
Importantly, we have not been able to identify any studies that further examined these persistent cases. At our institution, despite adherence to established diagnostic and therapeutic guidelines, anecdotal experience points to emerging cases of SBP that do not respond to initial treatment. It was our goal to study these resistant cases of SBP. We hypothesized that the patients who experience persistent SBP possess predisposing characteristics that increase their likelihood of developing a recalcitrant infection that is more likely to result in death than typical SBP. Identification of these characteristics would prompt more vigilance on the part of the clinician and may lead to a better clinical outcome for the patient.
Methods
Study population and design
The study was performed with the approval of the Institutional Review Board. All patients, 18 years or older, with ascites from chronic liver disease, who were admitted to the University of Chicago Medical Center between 1 January 2002 and 31 July 2007 were identified from a billing database, utilizing the ICD-9 diagnosis codes for peritonitis or for the procedure code for paracentesis. Those who were suspected to have secondary peritonitis were excluded from the study. SBP was defined by an ascitic PMN cell count >250/ml, with or without a positive fluid culture. In the subset of patients with SBP, persistent cases were defined by continued PMN cell count >250/ml on repeat paracentesis after 2 days of antibiotic therapy. Demographics and clinical features were recorded, including peritoneal fluid characteristics; hepatic and renal function at time of diagnosis; time interval from initial paracentesis to receiving antibiotics, albumin and undergoing repeat paracentesis; antibiotic choices; concomitant variceal hemorrhage; use of prophylactic antibiotics; HIV infection or immunocompromised status; model for end-stage liver disease (MELD) score; and survival to the end of the hospitalization.
Statistical methods
We analyzed data from the first episode of SBP in the study population. With SAS System software (version 9.2, Cary, NC, USA), two-sample t-tests, Wilcoxon rank-sum tests, and logistic regression models were used to determine whether persistent SBP patients differed from nonpersistent SBP patients with respect to clinically relevant measures and outcomes. All hypothesis tests were two-sided and performed at the customary α = 0.05 level.
Results
Of 841 patients initially screened we identified 58 episodes of SBP among 55 patients, and data from the first episode for each patient were included in the study. A total of 37 patients had a repeat paracentesis a mean (SD) of 70.35 (21.47) hours from the initial paracentesis. At the time of repeat paracentesis, 15 patients continued to have a fluid PMN cell count >250/ml. In these 15 patients, secondary peritonitis was excluded by imaging studies in all patients with abdominal computed tomography scans. A total of 22 patients had fluid PMN cell counts <250/ml, and the remaining 18 patients did not undergo repeat paracentesis because of clinical improvement and were considered nonpersistent. Therefore, the prevalence of persistent SBP was measured to be at least 27% in our study population.
Demographic and clinical data for the study population are summarized in Table 1. The average age of the study group was 56 years, with patients being predominantly male. Most patients were either African American or White. The most common cause of ascites was hepatitis C cirrhosis with and without concomitant alcoholic liver disease. Peritoneal fluid culture was positive in 40% of all cases, with a higher prevalence of Gram-negative than Gram-positive infections. The most common Gram-negative isolate was Escherichia coli, and the most common Gram-positive isolates were streptococcal and enterococcal species. The median fluid PMN cell count on initial paracentesis was 773/ml, and on repeat paracentesis was 127.6/ml. Of the 55 patients, three were on immunosuppressive medications (combinations of tacrolimus, mycophenolate mofetil and/or prednisone post-liver transplant), three had AIDS (CD4 cell counts of 9, 28, 101/ml), eight patients experienced gastrointestinal hemorrhage, and five were already on antibiotics at the time of diagnosis of SBP (Table 1). Importantly, 14 of the 15 patients with persistent SBP had no prior documentation of SBP in their medical history, making their first episode of SBP a persistent case.
Table 1.
Summary of baseline characteristics of all patients included as part of the study population.
| Characteristic | n (%) unless otherwise indicated |
|---|---|
| Age | 56.40 (9.43)* |
| Male sex | 43 (78.18) |
| Race | |
| African American | 21 (38.18) |
| White | 26 (47.27) |
| Other$ | 8 (14.55) |
| Cause of cirrhosis | |
| Hepatitis C | 16 (29.09) |
| Alcohol | 14 (25.45) |
| Hepatitis C and alcohol | 10 (18.18) |
| Hepatitis B | 3 (5.45) |
| Nonalcoholic steatohepatitis | 3 (5.45) |
| Cryptogenic cirrhosis | 3 (5.45) |
| Other# | 6 (10.90) |
| MELD score | 23.80 (8.43)* |
| Serum creatinine | 1.70 (1.20, 2.60)‡ |
| Serum bilirubin | 5.40 (2.10, 11.60)‡ |
| Serum INR | 1.60 (1.40, 2.10)‡ |
| Serum sodium | 133.09 (7.43)* |
| Immunocompromised status | 6 (10.91) |
| Variceal hemorrhage | 8 (14.55) |
| On antibiotics at time of diagnosis¶ | 5 (9.09) |
| Gram-stain positive | 6 (13.95)§ |
| Initial peritoneal fluid PMN cell count | 773.10 (517.50, 2188.80)‡ |
| Repeat peritoneal fluid PMN cell count | 127.60 (56.60, 607.60)‡ |
| Peritoneal fluid culture positive** | 22 (40.00) |
| Gram positive | 8 (14.54) |
| Gram negative | 11 (20.00) |
INR, international normalized ratio; MELD, model for end-stage liver disease; PMN, polymorphonyclear.
Mean (SD).
Other races: Hispanic (6), Middle Eastern (1), Eygptian (1).
Other causes of ascites: cirrhosis from alpha-1-antitrypsin deficiency (2), autoimmune hepatitis (2), giant-cell hepatitis (1), biliary obstruction (1).
Median (Q1, Q3).
Antibiotic regimens: ciprofloxacin weekly for prophylaxis of spontaneous bacterial peritonitis (SBP) (1), ciprofloxacin weekly for SBP prophylaxis and metronidazole for extraperitoneal infection (1), trimethoprim and sulfamethoxazole prophylaxis for patient with HIV (1). Other antibiotic regimens for extraperitoneal infections included dapsone/trimethoprim and sulfamethoxazole/ampicillin (1), vancomycin/cefepime (1).
Gram stain not performed on 12 (21.81) patients.
Peritoneal fluid culture was negative in 31 (56.36%) patients and not performed on 2 (3.63%) patients. Fluid culture was multi-organismal in 3 (5.45%) patients.
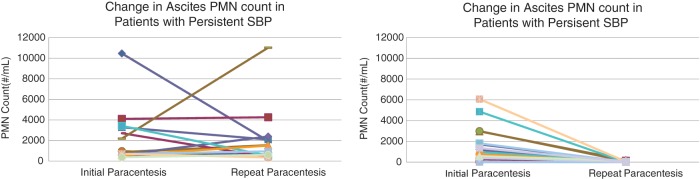
Of the continuous variables analyzed (Table 2), patients with persistent SBP were younger, and had lower mean ascites albumin and higher median serum ascites albumin gradient (SAAG) than patients with typical SBP. Furthermore, patients with persistent SBP had a higher mean MELD score than those with typical SBP. The mean PMN cell count at initial paracentesis was not statistically different between the two groups. At the time of repeat paracentesis, however, of the 15 patients with persistent SBP, six experienced a greater than 25% decrease in ascitic fluid PMN cell count after 2 days of antibiotic treatment and eight actually experienced a rise in their fluid PMN cell count on repeat paracentesis. All patients in the nonpersistent group showed a decrease in the PMN cell count on repeat paracentesis (Table 2, Figure 1). Other variables such as age, ascitic fluid glucose and lactate dehydrogenase (LDH), serum sodium, creatinine, and international normalized ratio (INR) were not statistically different between the two groups. However, some of these values were not assessed by the clinician for all patients (n = 24 for ascites glucose and n = 32 for ascites LDH), and a significant difference may have been missed owing to inadequate statistical power.
Table 2.
Utility of continuous variables for risk assessment of developing persistent spontaneous bacterial peritonitis (SBP).
| Variable | Median (Q1, Q3) by type of SBP unless otherwise indicated |
p-value | |
|---|---|---|---|
| Nonpersistent | Persistent | ||
| Age (years) | 58.13 (8.79)* | 51.80 (9.84)* | 0.0253$ |
| Initial ascitic fluid PMN cell count (/ml) | 660.80 (384.30, 1708.00) | 878.40 (615.40, 3283.20) | 0.1530‡ |
| Change in ascitic fluid PMN cell count (/ml) | 652.00 (331.28, 1651.00) | −69.79 (−671.60, 1189.20) | 0.0270$ |
| Ascites albumin (g/dl) | 1.00 (1.00, 1.20) | 0.61 (0.24, 1.00) | 0.0141‡ |
| SAAG | 1.10 (0.60, 1.60) | 1.85 (1.50, 2.41) | 0.0270‡ |
| Ascites glucose (mg/dl) | 107.50 (98.50, 131.50) | 100.00 (51.50, 125.00) | 0.6710‡ |
| Ascites LDH (IU/l) | 120.50 (86.00, 250.00) | 143.00 (92.00, 278.50) | 0.9577‡ |
| Serum creatinine (mg/dl) | 1.60 (1.00, 2.30) | 1.70 (1.40, 4.40) | 0.0997‡ |
| Serum bilirubin (mg/dl) | 4.95 (2.10, 9.10) | 6.20 (2.30, 15.10) | 0.1890‡ |
| Serum INR | 1.60 (1.35, 2.15) | 1.80 (1.58, 2.10) | 0.5574‡ |
| Serum sodium (mEq/l) | 132.78 (6.93)* | 133.93 (8.84)* | 0.6111$ |
| Serum albumin (g/dl) | 2.10 (1.90, 2.90) | 2.60 (2.10, 2.90) | 0.5489‡ |
| MELD score | 22.22 (8.10)* | 27.98 (8.09)* | 0.0225$ |
INR, international normalized ratio; LDH, lactate dehydrogenase; MELD, model for end-stage liver disease; PMN, polymorphonuclear; SAAG, serum ascites albumin gradient.
Of the continuous variables tested, change in ascitic fluid PMN cell count, ascites albumin, SAAG, and higher MELD score were the only statistically significant variables to predict an increased risk for the development of persistent SBP.
Mean (SD).
Wilcoxon rank-sum test.
Two-sample t-test.
Figure 1.
Change in asctic fluid polymorphonuclear (PMN) cell count from initial to repeat paracentesis. Of the 23 patients with nonpersistent spontaneous bacterial peritonitis (SBP) who underwent repeat paracentesis, all had a significant decline in ascitic fluid PMN cell count. Of the 15 patients with persistent SBP, only seven had a decline in ascites PMN cell count and eight patients experienced a rise in the PMN cell count at the time of repeat paracentesis.
In the set of categorical variables (Table 3), persistent SBP patients were more likely to have a positive culture result from the initial paracentesis sample than nonpersistent SBP patients. Other variables, including cause of ascites, antibiotics at time of diagnosis, immunocompromised status, incidence of gastrointestinal hemorrhage, Gram-stain positivity, treatment with a third-generation cephalosporin or a fluoroquinolone, and albumin infusion after diagnosis were not significantly different between the two groups. Comparing the resistance pattern of organisms cultured between the two groups, there was no significant difference in rates of infection with a resistant organism between the persistent and nonpersistent groups. Furthermore, it is unlikely that patients with persistent SBP did not clear their peritonitis owing to failure of initial therapy, as patients in both groups received appropriate empiric antibiotics. All patients with persistent SBP had changes in their antibiotic regimen after repeat paracentesis, most commonly broadening of antibacterial coverage (i.e. change of initial antibiotic to imipenem or piperacillin/tazobactam, addition of linezolid or metronidazole) and/or addition of an antifungal agent.
Table 3.
Utility of categorical variables for risk assessment of developing persistent spontaneous bacterial peritonitis (SBP).
| Categorical variable | Nonpersistent n/total n (%) |
Persistent n/total n (%) |
Odds ratio (95% CI) (persistent versusnonpersistent) |
p-value* |
|---|---|---|---|---|
| Male sex | 31/40 (77.50) | 12/15 (80.00) | 1.16 (0.27, 5.03) | 0.8416 |
| African American race** | 21/37 (56.76) | 5/10 (50.00) | 1.31 (0.32, 5.32) | 0.7034 |
| On antibiotics at time of diagnosis | 4/40 (10.00) | 1/15 (6.67) | 0.64 (0.07, 6.26) | 0.7037 |
| Immunocompromised state | 5/40 (12.50) | 1/15 (6.67) | 0.50 (0.05, 4.67) | 0.5432 |
| Variceal hemorrhage | 4/40 (10.00) | 4/15 (26.67) | 3.27 (0.70, 15.29) | 0.1317 |
| Gram-stain positive | 4/31 (12.90) | 2/12 (16.67) | 1.35 (0.21, 8.55) | 0.7499 |
| Culture positive | 12/38 (31.58) | 10/15 (66.67) | 4.33 (1.21, 15.47) | 0.0240 |
| Resistant organism$ | 4/11 (36.36) | 1/9 (11.11) | 0.22 (0.02, 2.45) | 0.2174 |
| Appropriate antibiotic administration‡ | 26/39 (66.67) | 13/15 (86.67) | 3.25 (0.64, 16.60) | 0.1566 |
| Ineffective antibiotic administration# | 1/10 (10.00) | 1/7 (14.29) | 1.50 (0.08,28.89) | 0.7881 |
| Albumin administration | 27/40 (67.50) | 11/14 (78.57) | 1.77 (0.42, 7.436) | 0.4385 |
| In-hospital mortality§ | 9/40 (22.50) | 6/15 (40.00) | 2.30 (0.64, 8.19) | 0.2002 |
Of the categorical variables tested, positive fluid culture from initial paracentesis was statistically significant for its ability to predict an increased risk for the development of persistent SBP. Patients with persistent SBP were also less likely to experience a >50% fall in their ascitic fluid PMN cell count from initial to repeat paracentesis.
p-value from Wald test of a logistic regression parameter estimate of effect of persistent SBP.
Compared with White race only.
An organism was considered resistant based on culture data showing resistance to fluoroquinolones and/or third-generation cephalosporins. Data not available for all patients with positive cultures as our microbiology laboratory does not routinely perform antibiotic sensitivity assays for coagulase-negative staphylococci, the causative agent in one patient in each group.
Appropriate antibiotic administration was defined as treatment with a third-generation cephalosporin or fluoroquinolone.
An antibiotic regimen was considered ineffective if the organism ultimately cultured was resistant to any part of the initial antibiotic regimen.
In-hospital mortality was defined as death from any cause during the hospitalization.
Importantly, all-cause in-hospital mortality in patients with persistent SBP was 40%, compared with 22.5% in those with nonpersistent SBP [OR = 2.30 (0.64, 8.19), p = 0.20]. Although we are limited by our small study numbers, and this difference was not statistically significant, this trend is an ominous finding for patients with persistent SBP. Cause of death in patients from both groups was most commonly septic shock with multiorgan failure or hepatic failure and its complications. Septic shock with multiorgan failure was the most common cause of death in the persistent SBP group, while hepatic failure and cardiac arrest of primary cardiac etiology were the most common cause of death in the nonpersistent group.
Discussion
Our study of patients with SBP has identified a set of vulnerable patients who experience recalcitrant infection. These persistent cases have not been previously investigated in the literature.
Although there has been a dramatic improvement in the clinical outcome of patients with SBP over the past 20 years, with a drastic decrease in SBP-associated mortality, recent studies still document high in-hospital mortality rates for this common complication [Lata et al. 2009; Tandon and Garcia-Tsao, 2008]. Previous studies have documented that not all patients show improvement in their fluid PMN count at 2 days, and have linked this lack of improvement to higher mortality and recurrence rates. Ljubicic and colleagues showed that a higher recurrence rate was associated with an ascitic fluid PMN cell count greater than 250/ml at 2 days in 62.5% of his study population [Ljubicic et al. 2000]. Fong and colleagues completed a prospective study to document serial ascitic fluid PMN cell count and showed a 92% mean reduction in survivors and a 66% mean reduction in nonsurvivors (p ≤ 0.01) within 2 days [Fong et al. 1989]. Cho and coworkers documented that 12.2% of patients (23/189 patients) with SBP did not become culture negative after 48–72 h of appropriate antibiotic therapy. They also found on further analysis that lack of microbiological response was an independent risk factor for higher SBP-related mortality [Cho et al. 2007]. In our study population, 38% of patients continued to have an ascitic PMN cell count greater than 250/ml after 2 days of therapy.
We chose to define persistent SBP cases using a repeat ascitic fluid PMN cell count >250/ml after 2 days of antibiotic therapy rather than determining a percentage reduction in PMN cell count to less than 25% or 50%, as previous studies showed a very high mortality rate associated with the failure of the PMN cell count to drop below 250/ml [Castellote et al. 2010; Angeloni et al. 2008; Ljubicic et al. 2000; Fong et al. 1989]. This clinical distinction is also supported by our data. In our patient population, of the 15 patients who died, the same number of patients had more than a 50% drop in the PMN cell count (n = 4) as those who had a drop of less than 50% or a rise in PMN cell count (n = 4). Therefore, it is unsafe to assume resolution of SBP when PMN cell count only drops by 50% or less by the time of repeat assessment, as this is not sufficient to identify those patients at higher risk of death.
There is a large body of literature describing the many clinical characteristics that predict a poor prognosis for patients after developing SBP. These include, but are not limited to, advanced age [Nobre et al. 2008; Thuluvath et al. 2001], poor hepatic function as measured by a higher MELD score [Nobre et al. 2008; Obstein et al. 2007], concomitant gastrointestinal bleeding [Borzio et al. 2001; Deschenes and Villeneuve, 1999; Bleichner et al. 1986], low ascitic protein content [Runyon, 1986], low serum albumin concentration [Deschenes and Villeneuve, 1999], renal dysfunction [Sort et al. 1999; Follo et al. 1994; Llovet et al. 1993], hyponatremia [Angeli et al. 2006; Llovet et al. 1993], and HIV infection [Shaw et al. 2006].
In our group of patients with persistent SBP and nonpersistent SBP, many of these known markers of poor prognosis were not more likely to be present in those patients with persistent SBP. Specifically, patients with persistent SBP were younger than those with nonpersistent SBP. They also had similar causes for their liver disease and ascites. A majority of patients had not had a prior episode of SBP. Hyponatremia and renal dysfunction, as measured by serum creatinine, did not correlate with the development of persistent SBP in our study population. Patients with persistent SBP were also not more likely to have HIV infection and be immunocompromised. Finally, concomitant variceal bleeding did not predispose patients to persistent SBP.
There were only three clinically important characteristics available at the time of diagnosis of SBP that differed between patients with persistent SBP and typical SBP: lower ascites albumin level, higher SAAG, and higher MELD score indicating lower protein ascites and increased severity of liver disease in patients with persistent SBP than in those with nonpersistent SBP. In addition, although culture results are not available when SBP is initially diagnosed, they are typically available at the time when patients are being assessed for response to empiric antibiotic therapy. We document that patients with persistent SBP were twice as likely to have a positive ascitic fluid culture (32% in the nonpersistent group compared with 67% in the persistent group).
Based on our current understanding of the pathophysiology of SBP, many of these results are not surprising. It is well known that patients with cirrhosis are at risk of intestinal bacterial overgrowth and have increased intestinal permeability, leading to translocation of intestinal bacteria, bacterial DNA and endotoxins from the intestinal lumen to the peritoneal space [Caruntu and Benea, 2006]. In combination with an impaired immunologic response, these factors allow for bacterial translocation into the systemic circulation, leading to bacteremia and subsequent infection of the ascitic fluid [Ramachandran and Balasubramanian, 2001]. We would hypothesize that patients with persistent SBP, who are also likely to have increased severity of their liver disease as indicated by their higher MELD scores, are more likely to develop infection of their ascites and subsequently to have an inadequate immune response, leading to higher culture-positive rates with poor clearance of the infection. Furthermore, regardless of the severity of liver disease, those with lower ascitic fluid protein levels, as indicated by lower ascites albumin and higher SAAG, are also less likely to mount a satisfactory immune response.
As this was a retrospective study, there are several potential limitations. We relied on nursing and physician documentation for data such as timing of initial and follow-up paracentesis, time to administration of antibiotics and albumin, diagnosis of gastrointestinal bleeding, and use of prophylactic antibiotics and immunosuppressive medications. We are not able to control for confounders and cannot definitively comment on causes of the differences between the two groups of patients. Furthermore, our statistical analysis and results are limited by the small study population.
With these limitations, we show that patients with persistent SBP had an in-hospital mortality rate almost twice that of patients who had begun to clear their infection at the time of repeat paracentesis: 40% compared with 22.5%. Furthermore, there are only few clinical measures that would aid clinicians in predicting whether patients will have persistent SBP. In addition, this persistent peritonitis is often the first episode of SBP for the patient with ascites, and is not a phenomenon resulting from repeated infections.
In conclusion, based on our findings, the current standard-of-care measures, such as early diagnostic paracentesis with prompt fluid PMN cell count analysis, empiric antibiotics, and albumin infusion, are not sufficient to overcome the risk of mortality in this vulnerable patient population. From our results, about 40% of patients with a MELD score >25 or SAAG >1.3 or a positive fluid culture developed persistent SBP. These parameters can be used to identify those patients at risk for a recalcitrant episode of SBP. In these patients, further clinical vigilance and follow-up paracentesis at 2 days to verify clinical response is necessary. In addition, at the time of repeat paracentesis, if the ascitic PMN cell count has not dropped below 250/ml, a prompt and aggressive a change in clinical management is required, regardless of other clinical features of the case. Although earlier identification of this group with the above guidelines may improve clinical outcomes, a better understanding of the reasons why these patients develop a more recalcitrant infection is necessary to decrease the significantly higher mortality rate associated with this condition. Prospective studies are needed to confirm our findings, to further explore the factors that predict treatment failure, and to investigate potential therapeutic measures for patients with persistent SBP.
Acknowledgments
The authors would like to thank Jeffery Charbeneau, biostatistician in the Department of Health Studies at the University of Chicago, for his insights and work on the statistical analysis of the data presented in this manuscript.
Footnotes
Funding: This work was supported by the Liver Research Fund, University of Chicago Medical Center.
Conflict of interest statement: The authors declare that there are no conflicts of interest.
Author contributions: Archita Desai and Nancy Reau contributed to the acquisition of data; analysis and interpretation of data; drafting of the manuscript and statistical analysis. All authors contributed to the study concept and design; critical revision of the manuscript for important intellectual content; obtaining funding; administrative, technical, or material support; and study supervision.
Contributor Information
Archita P. Desai, Section of Gastroenterology, Department of Medicine, University of Chicago Medical Center, Chicago, IL, USA
Nancy Reau, Center for Liver Diseases, Department of Medicine, University of Chicago Medical Center, 5841 South Maryland Avenue, MC 7120, Chicago, IL 60637, USA.
K. Gautham Reddy, Section of Gastroenterology, Center for Liver Diseases, Department of Medicine, University of Chicago Medical Center, Chicago, IL, USA.
Helen S. Te, Section of Gastroenterology, Center for Liver Diseases, Department of Medicine, University of Chicago Medical Center, Chicago, IL, USA
Smruti Mohanty, Section of Gastroenterology, Center for Liver Diseases, Department of Medicine, University of Chicago Medical Center, Chicago, IL, USA.
Rohit Satoskar, Georgetown Transplant Institute, Georgetown University Medical Center, Washington, DC, USA.
Amanda DeVoss, Section of Gastroenterology, Center for Liver Diseases, Department of Medicine, University of Chicago Medical Center, Chicago, IL, USA.
Donald Jensen, Section of Gastroenterology, Center for Liver Diseases, Department of Medicine, University of Chicago Medical Center, Chicago, IL, USA.
References
- Angeli P., Wong F., Watson H., Gines P. (2006) Hyponatremia in cirrhosis: results of a patient population survey. Hepatology 44: 1535–1542 [DOI] [PubMed] [Google Scholar]
- Angeloni S., Leboffe C., Parente A., Venditti M., Giordano A., Merli M., et al. (2008) Efficacy of current guidelines for the treatment of spontaneous bacterial peritonitis in the clinical practice. World J Gastroenterol 14: 2757–2762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bleichner G., Boulanger R., Squara P., Sollet J.P., Parent A. (1986) Frequency of infections in cirrhotic patients presenting with acute gastrointestinal haemorrhage. Br J Surg 73: 724–726 [DOI] [PubMed] [Google Scholar]
- Borzio M., Salerno F., Piantoni L., Cazzaniga M., Angeli P., Bissoli F., et al. (2001) Bacterial infection in patients with advanced cirrhosis: a multicentre prospective study. Dig Liver Dis 33: 41–48 [DOI] [PubMed] [Google Scholar]
- Caruntu F.A., Benea L. (2006) Spontaneous bacterial peritonitis: pathogenesis, diagnosis, treatment. J Gastrointestin Liver Dis 15: 51–56 [PubMed] [Google Scholar]
- Castellote J., Girbau A., Ariza X., Salord S., Vazquez X., Lobaton T., et al. (2010) Usefulness of reagent strips for checking cure in spontaneous bacterial peritonitis after short-course treatment. Aliment Pharmacol Ther 31: 125–130 [DOI] [PubMed] [Google Scholar]
- Cereto F., Herranz X., Moreno E., Andreu A., Vergara M., Fontanals D., et al. (2008) Role of host and bacterial virulence factors in Escherichia coli spontaneous bacterial peritonitis. Eur J Gastroenterol Hepatol 20: 924–929 [DOI] [PubMed] [Google Scholar]
- Cho J.H., Park K.H., Kim S.H., Bang J.H., Park W.B., Kim H.B., et al. (2007) Bacteremia is a prognostic factor for poor outcome in spontaneous bacterial peritonitis. Scand J Infect Dis 39: 697–702 [DOI] [PubMed] [Google Scholar]
- Deschenes M., Villeneuve J.P. (1999) Risk factors for the development of bacterial infections in hospitalized patients with cirrhosis. Am J Gastroenterol 94: 2193–2197 [DOI] [PubMed] [Google Scholar]
- EASL (2010) EASL clinical practice guidelines on the management of ascites, spontaneous bacterial peritonitis, and hepatorenal syndrome in cirrhosis. J Hepatol 53: 397–417 [DOI] [PubMed] [Google Scholar]
- Follo A., Llovet J.M., Navasa M., Planas R., Forns X., Francitorra A., et al. (1994) Renal impairment after spontaneous bacterial peritonitis in cirrhosis: incidence, clinical course, predictive factors and prognosis. Hepatology 20: 1495–1501 [DOI] [PubMed] [Google Scholar]
- Fong T.L., Akriviadis E.A., Runyon B.A., Reynolds T.B. (1989) Polymorphonuclear cell count response and duration of antibiotic therapy in spontaneous bacterial peritonitis. Hepatology 9: 423–426 [DOI] [PubMed] [Google Scholar]
- Kim S.U., Kim do Y., Lee C.K., Park J.Y., Kim S.H., Kim H.M., et al. (2010) Ascitic fluid infection in patients with hepatitis B virus-related liver cirrhosis: culture-negative neutrocytic ascites versus spontaneous bacterial peritonitis. J Gastroenterol Hepatol 25: 122–128 [DOI] [PubMed] [Google Scholar]
- Lata J., Stiburek O., Kopacova M. (2009) Spontaneous bacterial peritonitis: a severe complication of liver cirrhosis. World J Gastroenterol 15: 5505–5510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ljubicic N., Spajic D., Vrkljan M.M., Altabas V., Doko M., Zovak M., et al. (2000) The value of ascitic fluid polymorphonuclear cell count determination during therapy of spontaneous bacterial peritonitis in patients with liver cirrhosis. Hepatogastroenterology 47: 1360–1363 [PubMed] [Google Scholar]
- Llovet J.M., Planas R., Morillas R., Quer J.C., Cabre E., Boix J., et al. (1993) Short-term prognosis of cirrhotics with spontaneous bacterial peritonitis: multivariate study. Am J Gastroenterol 88: 388–392 [PubMed] [Google Scholar]
- Nobre S.R., Cabral J.E., Gomes J.J., Leitao M.C. (2008) In-hospital mortality in spontaneous bacterial peritonitis: a new predictive model. Eur J Gastroenterol Hepatol 20: 1176–1181 [DOI] [PubMed] [Google Scholar]
- Obstein K.L., Campbell M.S., Reddy K.R., Yang Y.X. (2007) Association between model for end-stage liver disease and spontaneous bacterial peritonitis. Am J Gastroenterol 102: 2732–2736 [DOI] [PubMed] [Google Scholar]
- Ramachandran A., Balasubramanian K.A. (2001) Intestinal dysfunction in liver cirrhosis: Its role in spontaneous bacterial peritonitis. J Gastroenterol Hepatol 16: 607–612 [DOI] [PubMed] [Google Scholar]
- Rimola A., Garcia-Tsao G., Navasa M., Piddock L.J., Planas R., Bernard B., et al. (2000) Diagnosis, treatment and prophylaxis of spontaneous bacterial peritonitis: a consensus document. International Ascites Club. J Hepatol 32: 142–153 [DOI] [PubMed] [Google Scholar]
- Runyon B.A. (1986) Low-protein-concentration ascitic fluid is predisposed to spontaneous bacterial peritonitis. Gastroenterology 91: 1343–1346 [DOI] [PubMed] [Google Scholar]
- Runyon B.A. (2009) Management of adult patients with ascites due to cirrhosis: an update. Hepatology 49: 2087–2107, http://www.aasld.org/practiceguidelines/Pages/default.aspx [DOI] [PubMed] [Google Scholar]
- Shaw E., Castellote J., Santin M., Xiol X., Euba G., Gudiol C., et al. (2006) Clinical features and outcome of spontaneous bacterial peritonitis in HIV-infected cirrhotic patients: a case-control study. Eur J Clin Microbiol Infect Dis 25: 291–298 [DOI] [PubMed] [Google Scholar]
- Sort P., Navasa M., Arroyo V., Aldeguer X., Planas R., Ruiz-del-Arbol L., et al. (1999) Effect of intravenous albumin on renal impairment and mortality in patients with cirrhosis and spontaneous bacterial peritonitis. N Engl J Med 341: 403–409 [DOI] [PubMed] [Google Scholar]
- Tandon P., Garcia-Tsao G. (2008) Bacterial infections, sepsis, and multiorgan failure in cirrhosis. Semin Liver Dis 28: 26–42 [DOI] [PubMed] [Google Scholar]
- Thuluvath P.J., Morss S., Thompson R. (2001) Spontaneous bacterial peritonitis–in-hospital mortality, predictors of survival, and health care costs from 1988 to 1998. Am J Gastroenterol 96: 1232–1236 [DOI] [PubMed] [Google Scholar]
- Wong C.L., Holroyd-Leduc J., Thorpe K.E., Straus S.E. (2008) Does this patient have bacterial peritonitis or portal hypertension? How do I perform a paracentesis and analyze the results?. JAMA 299: 1166–1178 [DOI] [PubMed] [Google Scholar]