Abstract
Intratumoral hypoxia, a frequent finding in metastatic cancer, results in the activation of the hypoxia-inducible factors (HIFs). HIFs are implicated in many steps of breast cancer metastasis, including metastatic niche formation through induction of lysyl oxidase (LOX) and lysyl oxidase-like (LOXL) proteins, enzymes that remodel collagen at the metastatic site and recruit bone marrow-derived cells (BMDCs) to the metastatic niche. We investigated the effect of two chemically and mechanistically distinct HIF inhibitors, digoxin and acriflavine, on breast cancer metastatic niche formation. Both drugs blocked the expression of LOX and LOXL proteins, collagen cross-linking, CD11b+ BMDC recruitment, and lung metastasis in an orthotopic breast cancer model. Patients with HIF-1α-overexpressing breast cancers are at increased risk of metastasis and mortality and our results suggest that such patients may benefit from aggressive therapy that includes a HIF inhibitor.
Keywords: Hypoxia-inducible factor 1, Lysyl oxidase, Bone marrow derived cells, Breast cancer metastasis, Metastatic niche, HIF inhibitor
Introduction
Breast cancer is the most common type of cancer in women and is the second leading cause of cancer deaths in women. Metastasis is the major cause of mortality in breast cancer patients. More than 10% of breast cancer patients develop distant metastases within 3 years after first diagnosis and the median survival of these patients is less than 2 years [1]. There are no clinical tests that can unequivocally identify, at the time of diagnosis, women who will develop metastases. Effective targeted therapies are available for women with breast cancers that express the estrogen and progesterone receptors (ER/PR) or have amplification of the HER2 gene. In contrast, triple-negative breast cancers, which lack high-level ER/PR and HER2 expression, are frequently metastatic, and have a high relapse rate after chemotherapy [2].
Breast cancer is a heterogeneous disease due to different genetic and epigenetic alterations that occur during the development of malignancy. Breast cancers also develop in heterogeneous microenvironments. The mean PO2 in breast cancer is 10 mm Hg (~1.5% O2), as compared to 65 mm Hg in normal breast tissue [3]. Intratumoral PO2 values of less than 10 mm Hg are associated with increased risk of metastasis and mortality, independent of tumor size, stage, grade, or lymph node status [3]. A fundamental mechanism by which cancer cells adapt to the hypoxic microenvironment is through the activation of hypoxia-inducible factors (HIFs), which are composed of an O2-regulated HIF-1α or HIF-2α subunit and a constitutively expressed HIF-1β subunit [4]. Overexpression of HIF-1α or HIF-2α in the diagnostic biopsy is associated with increased metastasis and decreased survival in breast cancer patients, including those without lymph node involvement at the time of diagnosis [4]. Activation of HIFs results in the transcription of many genes that are critical for invasion [5–7], metastasis [5, 7–10], and resistance to therapy [11].
HIF-1α has been reported to play a key role in metastatic niche formation [7, 8], one of the earliest steps of metastasis, in which primary tumors produce factors that prepare the potential metastatic site as a receptive soil for cancer cell seeding [12]. Hypoxic breast cancer cells activate HIFs, which in turn induce the expression of a family of secretory proteins that includes lysyl oxidase (LOX), lysyl oxidase-like 2 (LOXL2), and LOXL4 [5, 7, 8]. LOX and LOXL proteins post-translationally modify collagen molecules in the extracellular matrix (ECM) by oxidizing lysine residues to -aminoadipic -semialdehydes, which then undergo condensation to form cross-linked collagen fibers [13]. LOX, LOXL2, and LOXL4 secreted from hypoxic breast cancer cells in the primary tumor cross-link collagens in the lungs, which facilitates the invasion of CD11b+ bone marrow derived cells (BMDCs). The recruitment of BMDCs at the potential metastatic site promotes metastasis in several ways. First, BMDC recruitment is associated with increased expression of chemokines (e.g. SDF-1), which may attract tumor cells that bear the cognate cytokine receptor (e.g. CXCR4) [12]. Second, CD11b+ BMDCs may promote the formation of blood vessels in the incipient metastatic lesion, thereby supporting cancer cell survival and proliferation [14–16]. Third, CD11b+ BMDCs may suppress natural killer cell-dependent immune responses in tumor-bearing animals [17]. Thus, the BMDCs that are recruited to the metastatic niche are a heterogeneous collection of myeloid cells, collectively identified by their expression of CD11b, which create a favorable microenvironment for subsequent lung colonization by metastatic cancer cells [7, 8].
We recently demonstrated that genetic knockdown of HIF-1α in human breast cancer cells inhibits primary tumor growth and lung metastasis [10] and blocks metastatic niche formation in the lungs of mice bearing primary breast tumors [7]. However, the clinical relevance of these studies is limited because inhibition of HIF-1 activity occurred prior to primary tumor formation, whereas cancer patients are treated with chemotherapy only after establishment of a primary tumor. Digoxin [18] and acriflavine [19] are HIF-1 inhibitors that were identified in cell-based screens of drugs that are FDA-approved or have a history of clinical use. Digoxin inhibits the synthesis of HIF-1α and HIF-2α, whereas acriflavine inhibits the dimerization of HIF-1α or HIF-2α with HIF-1β. Both drugs inhibited the growth of human prostate cancer and hepatocellular carcinoma xenografts [18, 19]. In this study, we specifically investigated whether these drugs inhibit metastatic niche formation in SCID mice following mammary fat pad (MFP) injection of human triple-negative breast cancer cells.
Materials and methods
Cell culture
Human MDA-MB-231 (MDA-231) and MDA-MB-435 (MDA-435) cells were cultured in Dulbecco’s modified essential medium (DMEM) supplemented with 10% fetal bovine serum (FBS) and 1% penicillin-streptomycin in a 5% CO2/95% air incubator at 37°C. Cells exposed to hypoxia were maintained at 1% O2/5% CO2/balance N2 at 37°C in a modulator incubator chamber (Billups-Rothenberg).
Real-time PCR and immunoblots
RNA extracted by Trizol (Invitrogen) served as template for reverse transcription using a cDNA synthesis kit (BD Biosciences). qPCR was performed with SYBR Green qPCR Master Mix (Fermentas) and primers as previously described [7]. Proteins extracted from cells by RIPA buffer were resolved by 10% SDS/PAGE. HIF-1α (BD Transduction Laboratory), β-actin (Santa Cruz), LOX (Santa Cruz), LOXL2 (Novus Biologicals), and LOXL4 (Novus Biologicals) antibodies were used for immunoblot assays.
Luciferase reporter assay
Cells were seeded onto 24-well plates and transfected with the HIF-dependent reporter p2.1 [20] and control reporter pSV-Renilla. Cells were exposed to 20% or 1% O2 for 24 h. Luciferase activites were determined by Dual-Luciferase Assay Kit (Promega).
Orthotopic implantation and metastasis assays
All animal experiments were performed according to protocols approved by the Johns Hopkins University Animal Care and Use Committee in accordance with the NIH Guide for the Care and Use of Laboratory Animals. Orthotopic implantation of breast cancer cells into the MFP of SCID mice was performed as previously described [7]. After palpable tumors were formed, mice were administered 2 mg/kg/day of digoxin (obtained from the Johns Hopkins Hospital Pharmacy), 4 mg/kg/day of acriflavine (Sigma), or saline via intraperitoneal injection. Following euthanization, the lungs were perfused with PBS. The left lung was inflated with low melting point agarose for formalin fixation and paraffin embedding for hematoxylin and eosin (H&E) staining and immunohistochemical analysis of tissue sections. The right lung was used for flow cytometry and genomic DNA extraction. Lung tissue preparation for flow cytometry analysis was performed as previously described using PerCP-conjugated CD45 antibody (BD Pharmingen) and APC-conjugated CD11b antibody (eBiosciences). Forward and side scatter, unstained control, CD45 single-stained, and CD11b single-stained cells were included in experiments for gating. Genomic DNA was used for qPCR to quantify human HK2 DNA and mouse 18S rDNA sequences as previously described [7].
Bone marrow cell (BMC) invasion assay
BMCs were isolated from the femurs and tibias of mice by flushing with sterile phosphate buffered saline (PBS) and sedimentation through Histopaque (Sigma). Transwell inserts (Corning) were coated with 10 µL of Matrigel (BD Biosciences). CM from breast cancer cells cultured under 20% or 1% O2 for 48 h was incubated with the Matrigel-coated insert overnight. Digoxin, acriflavine, or vehicle (DMSO) control was added to the cells before exposure to 20% or 1% O2. After CM was removed from the Matrigel-coated inserts, 1×106 freshly isolated BMCs resuspended in serum-free DMEM (CellGro) were seeded in the upper chamber and 10% FBS-supplemented DMEM was placed in the lower chamber as chemoattractant. After 20 hours, the BMCs that invaded through the membrane were counted using a hemocytometer or Countess automated cell counter (Invitrogen).
Immunohistochemistry
Lung sections were stained with Picrosirius Red (Sigma Aldrich) and analyzed by phase contrast microscopy under polarized light to identify cross-linked collagen fibers. Immunohistochemistry was performed using CD11b antibody (Novus Biologicals) and LSAB+System HRP kit (DAKO) for the detection of CD11b+ myeloid cells. The number of CD11b+ cell clusters was counted in at least 5 random fields. Lung sections were stained with H&E and metastases were quantified by determining the area of lung occupied by metastases divided by the total area of lung section that was analyzed. Results were normalized to the saline control.
Statistical Analysis
Continuous parametric data were analyzed with Student’s t-test when two groups of data were involved. Multiple groups of data were analyzed with one-way ANOVA with Bonferroni correction using GraphPad Prism 5 software.
Results
Increased LOXL2 and LOXL4 expression in invasive breast cancers
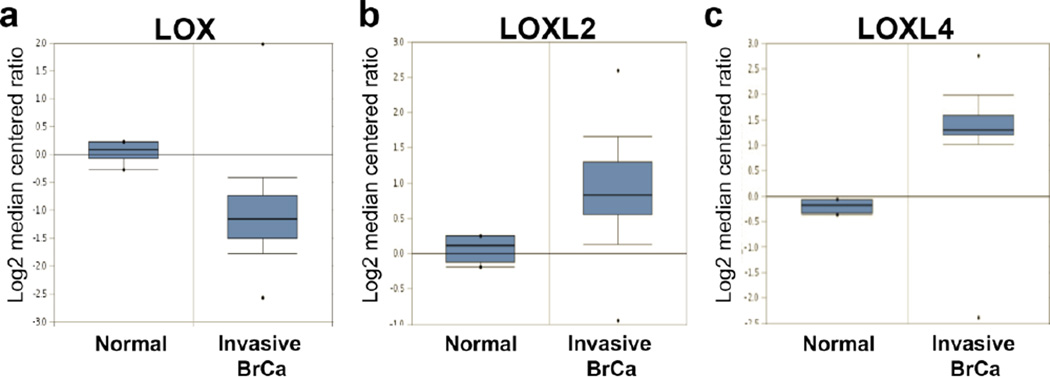
Previously, we demonstrated that different combinations of LOX, LOXL2, and LOXL4 mRNA were overexpressed in 11 human breast cancers relative to surrounding normal breast tissue [7]. Increasing evidence reveals that stromal cells such as fibroblasts, mesenchymal stem cells, vascular cells, and inflammatory cells, which are recruited into the primary tumor, facilitate cancer progression and metastasis [21]. We utilized microarray data available in the Oncomine database to analyze LOX/LOXL mRNA expression in human clinical samples of 6 normal breast stromal tissues and stromal tissue isolated from 53 invasive breast cancers [22]. LOX mRNA expression was not significantly increased in cancer, compared to normal, breast stroma (P = 1.0), but LOXL2 (2.3 fold; P = 4.6 × 10−8) and LOXL4 (3.0 fold; P = 1.64 × 10−20) mRNAs were significantly overexpressed in the invasive breast cancer stroma (Fig. 1). Whereas previous studies have focused on the role of LOX, LOXL2, and LOXL4 in breast cancer cells [5, 7, 8], these clinical data suggest that intratumoral hypoxia may also induce expression of LOXL2 and LOXL4 in stromal cells of invasive breast cancers, whereas LOX overexpression [5] may be restricted to cancer cells.
Fig. 1.
Increased LOXL2 and LOXL4 expression in stromal tissue from invasive breast cancer. Box and whiskers plots of Oncomine data on LOX, LOXL2, and LOXL4 mRNA levels (expressed as the log2 median-centered ratio [17]) in stromal tissues isolated from normal breast (n = 6) and breast cancer (BrCa; n = 53).
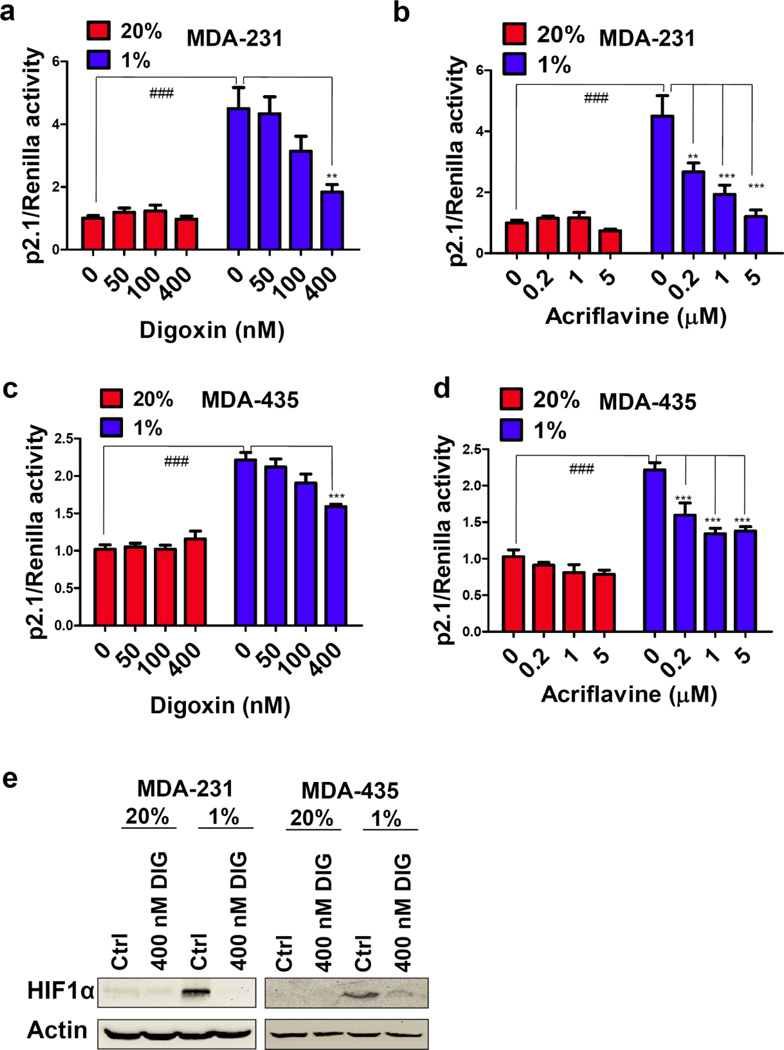
Digoxin and acriflavine inhibit HIF activity in breast cancer cells
We analyzed two triple-negative, metastatic human breast cancer cell lines: MDA-MB-231 (MDA-231), which was established from metastatic cells collected from pleural fluid [23]; and MDA-MB-435 (MDA-435), the derivation of which was questioned [24] but recent evidence has confirmed its identity as a breast cancer cell line [25]. The cells were transfected with HIF-dependent reporter plasmid p2.1, in which firefly luciferase expression was driven by a hypoxia response element located upstream of a basal SV40 promoter, and control reporter pSV-Renilla, in which Renilla luciferase expression was driven by the SV40 promoter alone. The ratio of p2.1:pSV-Renilla activity, which is a measure of HIF transcriptional activity, was increased approximately 5-fold in MDA-231 cells cultured under hypoxic (1% O2) as compared to non-hypoxic (20% O2) conditions and approximately 2.5-fold in hypoxic MDA-435 cells (Fig. 2a–d), in the absence of drug treatment. Treatment with digoxin or acriflavine abolished the induction of HIF transcriptional activity in hypoxic MDA-231 and MDA-435 cells (Fig. 2a–d). Digoxin blocked the induction of HIF-1α protein expression in hypoxic MDA-231 and MDA-435 cells (Fig. 2e). Acriflavine does not affect HIF-1α protein levels, but instead blocks HIF-1α:HIF-1β dimerization [19], which is reflected in the inhibition of HIF-1 transcriptional activity (Fig. 2b, d).
Fig. 2.
Digoxin and acriflavine inhibit HIF transcriptional activity in breast cancer cells. a–d MDA-231 and MDA-435 cells were co-transfected with HIF-dependent firefly luciferase (p2.1) and control Renilla luciferase (pSV-Renilla) reporter plasmids and cultured for 24 h in the presence of the indicated digoxin or acriflavine concentration at either 20% (red bar) or 1% (blue bar) O2. The ratio of p2.1/pSV-Renilla activity was determined by dual luciferase assays. For the indicated comparisons: ###P < 0.001, **P < 0.01, and ***P < 0.001; one-way ANOVA with Bonferroni correction (mean ± SEM; n = 3). e Immunoblot assays were performed to analyze HIF-1〈 and β-actin protein levels in whole cell lysates prepared from control and digoxin-treated MDA-231 and MDA-435 cells were analyzed by immunoblot assays.
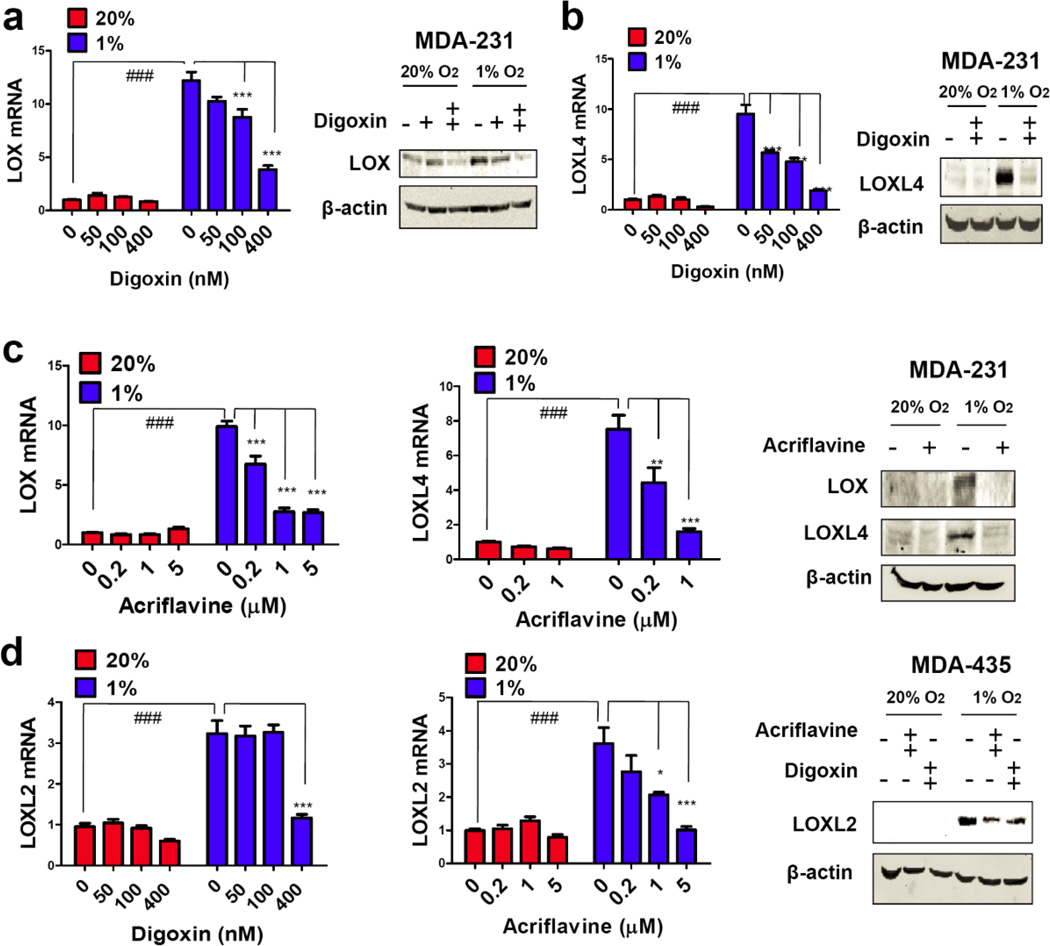
Digoxin and acriflavine block hypoxia-induced LOX/LOXL expression in breast cancer cells
Previously, we demonstrated that distinct subsets of LOX family members were overexpressed in biopsies from different primary human breast cancers and that multiple LOX family members were induced by hypoxia and regulated by HIF-1 in different breast cancer cell lines [7]. Specifically, hypoxia induced the expression of LOX and LOXL4 in MDA-231 cells, whereas LOXL2 expression was induced in MDA-435 cells [7]. Both digoxin and acriflavine abrogated hypoxia-induced LOX and LOXL4 mRNA and protein expression in MDA-231 cells (Fig. 3a–c) and inhibited hypoxia-induced LOXL2 mRNA and protein expression in MDA-435 cells (Fig. 3d). Thus, digoxin and acriflavine each effectively inhibited the hypoxia-induced expression of all LOX family members.
Fig. 3.
HIF inhibitors block hypoxia-induced expression of LOX, LOXL2, and LOXL4. Human breast cancer cells were treated with digoxin or acriflavine and exposed to 20% or 1% O2 for 24 or 48 h prior to mRNA or protein analysis, respectively. a Left: LOX mRNA expression was analyzed in MDA-231 cells treated with the indicated concentration of digoxin by reverse transcription quantitative real-time PCR (RT-qPCR) relative to 18S rRNA and normalized to the result from cells exposed to 20% O2 in the absence of digoxin. Right: LOX and β-actin protein levels were analyzed in MDA-231 cells treated with 100 nM digoxin (+), 400 nM digoxin (++), or vehicle (0.02% DMSO) control (−). b Left: LOXL4 mRNA expression was analyzed in MDA-231 cells treated with the indicated concentration of digoxin. Right: LOXL4 protein levels were analyzed in MDA-231 cells treated with 400 nM digoxin (++) or vehicle control (−). c LOX (left) and LOXL4 (middle) mRNA levels were analyzed in MDA-231 cells treated with the indicated concentration of acriflavine. Right: LOX and LOXL4 protein levels were analyzed in MDA-231 cells treated with 5 µM acriflavine (++) or vehicle control (−). d LOXL2 mRNA expression was analyzed in MDA-435 cells treated with the indicated concentration of digoxin (left) or acriflavine (middle). Right: LOXL2 protein levels were analyzed in MDA-435 cells treated with 5 µM acriflavine (++), 400 nM digoxin (++), or vehicle control (−). ###P < 0.001 vs 20% O2 control; *P < 0.05, **P < 0.01, and ***P < 0.001 vs 1% O2 control, one-way ANOVA with Bonferroni correction (mean ± SEM; n = 3).
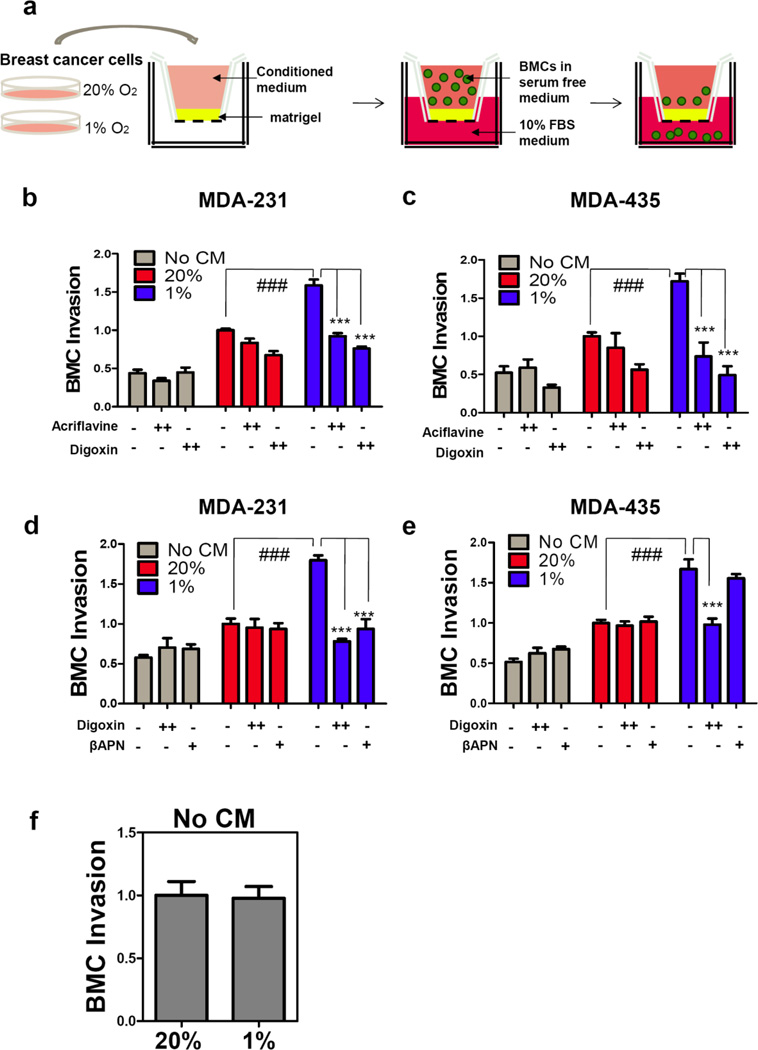
Digoxin and acriflavine inhibit breast cancer-mediated bone marrow cell invasion
Hypoxic breast cancer cells produce LOX/LOXL proteins, which remodel collagen in the lungs, leading to the invasion of BMDCs, which is required for metastatic niche formation. As an ex vivo model, MDA-231 or MDA-435 cells were exposed to 20% or 1% O2 in the presence of digoxin, acriflavine, or vehicle and the conditioned medium (CM) from these breast cancer cells was incubated with matrigel (tumor-derived ECM), which coated Transwell filters in modified Boyden chambers. Then, freshly isolated mouse bone marrow cells (BMCs) were seeded into the chamber above the matrigel-coated filter (Fig. 4a). BMCs showed a significant increase in invasive capability when seeded onto matrigel that was treated with CM from hypoxic cells, but this effect was lost when the breast cancer cells that generated the CM were treated with digoxin or acriflavine (Fig. 4b, c).
Fig. 4.
HIF inhibitors suppress breast cancer-mediated bone marrow cell (BMC) invasion. a Transwell chambers were coated with matrigel. Conditioned medium (CM) from breast cancer cells was incubated with matrigel for 16 h at 37°C. BMCs in serum-free medium were seeded in the top chamber. Fresh medium containing 10% FBS was placed in the bottom chamber. The number of BMCs that invaded through the pretreated matrigel to the bottom chamber was counted. The results were normalized to those obtained using CM from cells exposed to 20% O2 in the absence of HIF inhibitor (acriflavine or digoxin). b–c Analysis of CM from MDA-231 cells or MDA-435 cells, which were treated with 5 µM acriflavine (++), 400 nM (++) digoxin, or vehicle (−) and cultured in 20% (red bar) or 1% (blue bar) O2 for 48 h. d–e Analysis of CM from MDA-231 or MDA-435 cells, which were treated with 200 µM βAPN, 400 nM digoxin, or vehicle and cultured in 20% or 1% O2 for 48 h. Blank (fresh) medium and drug-containing blank medium were included as controls (gray bars). f Blank medium incubated at 20% O2 or 1% O2 was incubated with matrigel prior to BMC invasion assay. For the indicated comparisons: ###P < 0.001 and ***P <l 0.001, one-way ANOVA with Bonferroni correction (mean ± SEM; n = 3).
Clinical and cell line data suggested that LOXL2 may be the dominant LOX family member expressed in certain breast cancers [7]. β-aminopropionitrile (βAPN) is a small molecule inhibitor of LOX catalytic activity that is reported to be less effective against LOXL2, although this remains controversial [26, 27]. We hypothesized that HIF inhibitors might more effectively suppress BMC invasion because of their inhibitory effect on the expression of all LOX family proteins. We therefore compared the effect of digoxin and βAPN treatment of MDA-435 and MDA-231 cells exposed to 20% or 1% O2. APN exerted a suppressive effect on hypoxic MDA-231, but not hypoxic MDA-435 cells, in BMC invasion assays (Fig. 4d, e). This result is consistent with the reported failure of βAPN to inhibit LOXL2 activity [27], because LOXL2 is the only family member induced by hypoxia in MDA-435 cells. Digoxin, in contrast, exhibited an inhibitory effect on CM from both cell lines (Fig. 4d, e). To eliminate the possibility that residual inhibitors in the CM might affect the invasion of BMCs directly, fresh medium with or without inhibitors was included as negative controls. The presence of digoxin, acriflavine, or βAPN had no effect on BMC invasion under these conditions (gray bars in Fig. 4b–e). Media incubated in the absence of cells at 20% O2 and 1% O2 were used to treat the matrigel that is coated on the chamber and showed no different effect on BMC invasion (Fig. 4f), indicating that hypoxia does not alter components in the blank media.
HIF inhibitors suppress metastatic niche formation
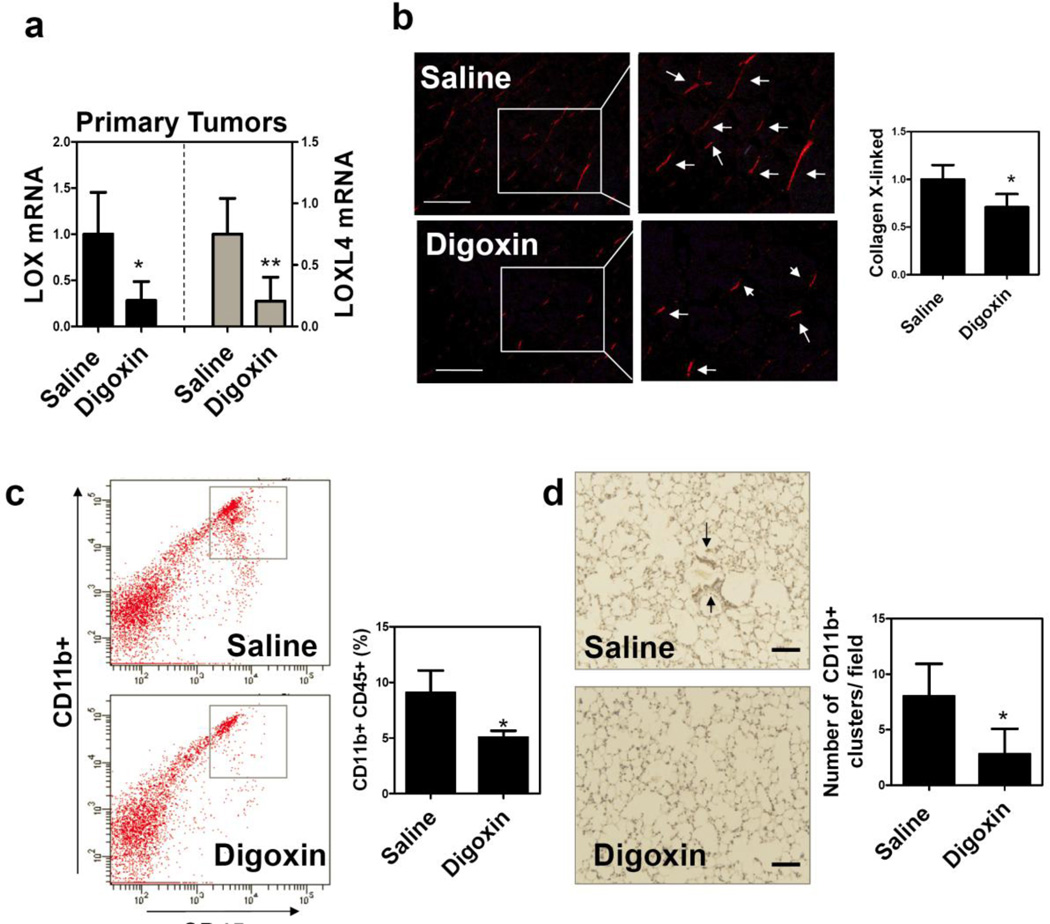
To test the pharmacologic effect of HIF inhibition on metastatic niche formation in vivo, we treated mice bearing MDA-231 tumors in the MFP with 2 mg/kg/day of digoxin by intraperitoneal (IP) injection after palpable tumors had formed. Digoxin inhibited LOX and LOXL4 mRNA expression in the primary tumors (Fig. 5a). We also analyzed the lungs of tumor-bearing mice with Picrosirius Red, which selectively stains cross-linked collagen fibrils when tissue sections are viewed under polarized light. Digoxin-treated mice demonstrated significantly decreased collagen cross-linking (Fig. 5b). Next, we analyzed BMDC recruitment to the lungs by flow cytometry (using antibodies against CD11b and CD45) or by CD11b immunohistochemistry. Digoxin significantly suppressed recruitment of CD11b+ BMDCs to the lungs of tumor-bearing mice (Fig. 5c, d).
Fig. 5.
Treatment with digoxin blocks metastatic niche formation in the lungs of MDA-231 tumor-bearing mice. SCID mice received mammary fat pad (MFP) injections of MDA-231 cells followed by intraperitoneal (IP) injection of saline or digoxin (2 mg/kg/day) starting 14 days after MFP injection. Primary tumors and lungs were harvested 47 days after orthotopic implantation. a LOX (black bar) and LOXL4 (gray bar) mRNA levels in the primary tumors were determined by RT-qPCR. Values were normalized to saline control. b Lung sections (scale bar = 100 µm) were treated with Picrosirius Red, which selectively stains cross-linked (fibrillar) collagen when viewed under circularly polarized light (arrow). The number of collagen fibers per field was counted in 5 fields per section and normalized to the result obtained from the saline treated mice. c Single cell suspensions from lung were analyzed by flow cytometry to quantify CD11b+CD45+ cells (percentage of total cell population analyzed). d Lung sections (scale bar = 100 µm) were analyzed by immunohistochemistry using an antibody against CD11b. CD11b+ cell clusters was counted in at least 5 random fields per section and the mean ± SD value for cell clusters per field was determined. *P < 0.05 and **P < 0.01 vs saline, Student’s t-test (n = 5 mice).
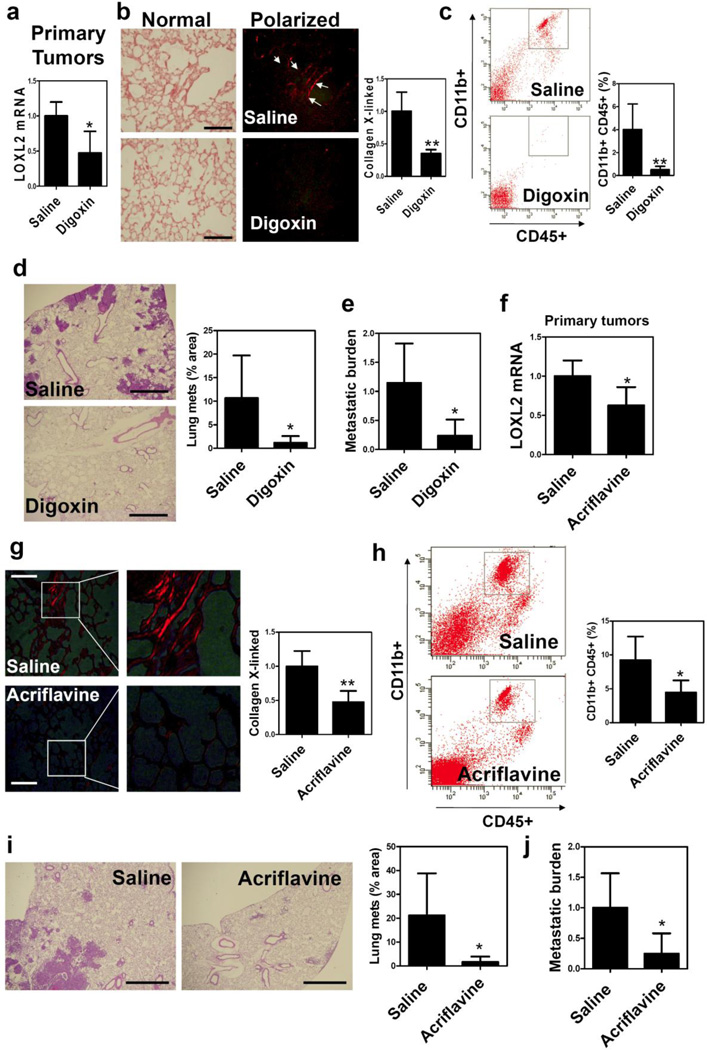
Mice bearing MDA-435 tumors in the MFP were also treated with digoxin. Digoxin inhibited LOXL2 mRNA expression in the primary tumors (Fig. 6a) and significantly reduced collagen cross-linking and the percentage of CD11b+ BMDCs in the lungs of the tumor-bearing mice (Fig. 6b, c). Most importantly, digoxin reduced the metastasis of breast cancer cells to the lungs (Fig. 6d, e). We also treated MDA-435 tumor-bearing mice with 4 mg/kg/day of acriflavine by IP injection. Acriflavine reduced LOXL2 mRNA expression in the primary tumors (Fig. 6f). Similar to digoxin, acriflavine significantly reduced collagen cross-linking (Fig. 6g), CD11b+ BMDC recruitment (Fig. 6h), and metastasis formation (Fig. 6i, j) in the lungs.
Fig. 6.
Treatment with digoxin or acriflavine blocks metastatic niche formation and breast cancer metastasis in the lungs in MDA-435 tumor-bearing mice. a–e SCID mice received MFP injection of MDA-435 cells followed by IP injection of saline or digoxin (2 mg/kg/day), starting 8 days after implantation. 42 days after MFP injection, lungs and primary tumors were harvested. a LOXL2 mRNA levels in the primary tumors were determined by RT-qPCR. Values were normalized to saline control (mean ± SD; n = 5). b Picrosirius Red staining under polarized light (scale bar = 100 µm), c flow cytometry analysis of CD11b+CD45+ cells (% of total cell population analyzed), and d lung metastases (% of total lung area, H&E staining, scale bar = 1 mm) are shown. e Metastatic burden was determined by isolation of lung DNA and qPCR using human-specific HK2 gene primers and mouse 18S rDNA primers; the ratio was normalized to the result obtained from saline control (mean ± SD; n = 5). f–j NOD-SCID mice received MFP injection of MDA-435 cells followed by IP injection of saline or acriflavine (4 mg/kg/day) starting 8 days after orthotopic implantation. Lungs and tumors were harvested 45 days after implantation. f LOXL2 mRNA expression in primary tumors was determined by RT-qPCR and normalized to saline control. Cross-linking of collagen was visualized with Picrosirius Red staining under polarized light (g; scale bar = 100 µm). Flow cytometry analysis of CD11b+CD45+ BMDCs in lungs (h), H&E staining (scale bar = 1 mm) of lung metastases (i; % of total lung area), and qPCR analysis of metastatic burden in lungs (j) from saline and acriflavine treated mice are shown. *P < 0.05 and **P < 0.01 vs saline, Student’s t-test (mean ± SD; n = 3–5).
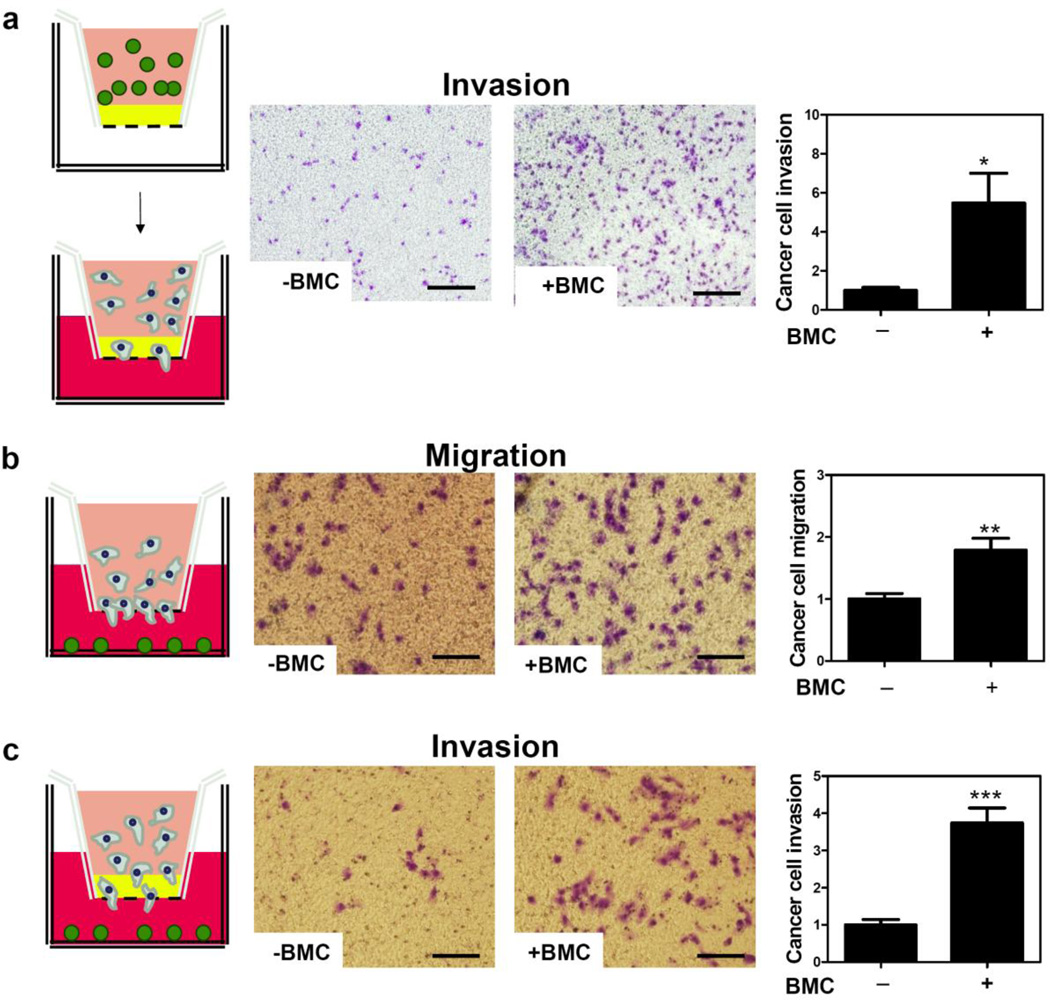
BMCs stimulate breast cancer cell migration and invasion
In order to study the mechanisms by which BMDCs facilitate breast cancer metastasis, we investigated whether they remodel the metastatic environment to make it more susceptible to cancer cell invasion. We coated the membrane of a transwell insert with matrigel, which was incubated with BMCs or medium only in the upper chamber for 16 h. Then, the BMCs were removed and naïve MDA-231 cells were seeded into the upper chamber. Increased breast cancer cell invasion through BMC-treated matrigel was observed (Fig. 7a). We next investigated whether the migration and invasion of MDA-231 cells could be stimulated by diffusible factors secreted by BMCs located in the lower chamber. BMCs significantly increased breast cancer cell migration through an uncoated transwell membrane (Fig. 7b) and also increased cell invasion through a matrigel-coated membrane (Fig. 7c). These results suggest that BMCs may facilitate cancer cell invasion of the metastatic niche by remodeling ECM and by acting as a source of chemoattractants, but additional studies are required to test these hypotheses in greater detail.”
Fig. 7.
BMCs facilitate migration and invasion of breast cancer cells. a Medium with (+) or without (+) BMCs (green in schematic at left) was added to the top chamber and incubated with matrigel-coated filter inserts at 37°C for 16 h. The BMCs were removed and MDA-231 cells (blue in schematic) were seeded in the top chamber with medium containing 10% FBS in the bottom chamber. Representative photomicrographs of invaded cells stained with crystal violet are shown (middle panels; scale bar = 250 µm) and mean + SEM data are shown (bar graph at right). b–c Medium with (+) or without (−) BMCs was seeded in the bottom chamber. MDA-231 cells in serum-free medium were seeded in the top chamber containing a non-coated filter (Migration assay; b) or matrigel-coated filter (Invasion assay; c). Representative photomicrographs of crystal violet-stained cells are shown (scale bar = 100 µm). The number of migrated or invaded cells was counted in a blinded fashion in at least 3 random fields, the data were normalized to the results obtained from medium without BMCs, and mean + SEM (n = 3) are shown (bar graph at right). *P < 0.05, **P < 0.01, and ***P < 0.001 vs medium without BMCs, Student’s t-test.
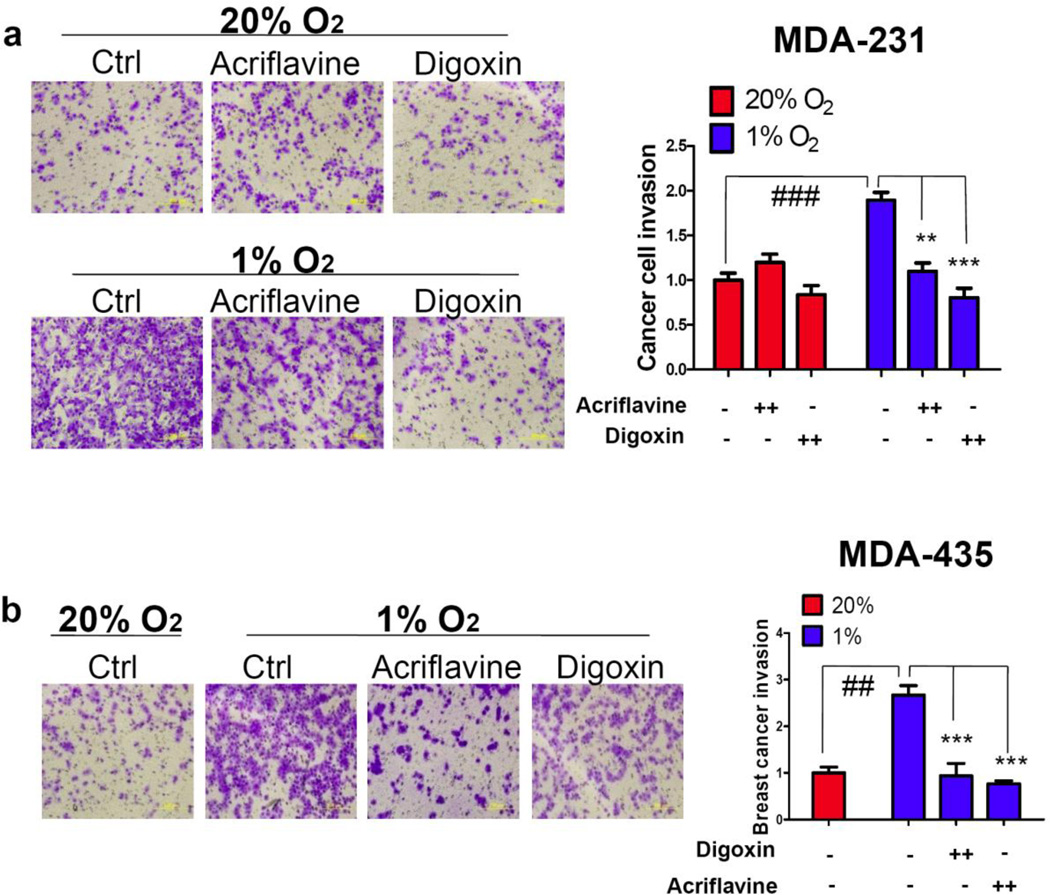
Fig. 8.
Analysis of conditioned media from breast cancer cells treated with digoxin or acriflavine. Matrigel-coated inserts were incubated with CM from MDA-231 (a) or MDA-435 cells (b) that were treated with vehicle (−), 400 nM digoxin (++), or 5 µM acriflavine (++) and exposed to 20% or 1% O2. Naïve MDA-231 cells were seeded in the top chamber. Cells that invaded through the pretreated matrigel were fixed, stained with crystal violet, and counted. Representative photomicrographs of invaded cells are shown (panels at left; scale bar = 200 µm). The number of invaded cells was counted, normalized to the control (Ctrl; 20% O2, no drug), and mean ± SEM (n = 3) values (bar graph at right) are shown. For the indicated comparisons: ###P < 0.001, **P < 0.01, and ***P < 0.001; one-way ANOVA with Bonferroni correction.
HIF inhibitors suppress breast cancer cell invasion of ECM
Treatment of tumor-bearing mice with digoxin or acriflavine resulted in a significant reduction in BMDC recruitment, but lung metastasis was even more drastically reduced. These observations suggested that HIF plays other roles in addition to stimulating metastatic niche formation in the lungs. We hypothesized that HIF-induced expression of LOX/LOXL (as well as other collagen-modifying enzymes) also leads to remodeling of the primary tumor microenvironment, which facilitates invasion of breast cancer cells through ECM to the vascular endothelium. To test this hypothesis, we treated matrigel with CM that was generated by MDA-231 cells cultured in 20% or 1% O2. Next, we seeded naïve MDA-231 cells into the upper transwell chamber and allowed them to invade. We observed significantly increased breast cancer cell invasion through matrigel that was treated with CM from hypoxic cells as compared to non-hypoxic cells (Fig. 8a). This effect of hypoxia was abolished when the MDA-231 cells that were the source of the CM were treated with digoxin or acriflavine (Fig. 8a). Similar results were obtained when these experiments were performed with MDA-435 cells (Fig. 8b). These results suggest that digoxin and acriflavine may inhibit breast cancer cell invasion through ECM of the primary tumor as well as inhibiting metastatic niche formation in the lungs.
Discussion
HIFs confer metastatic capabilities on hypoxic cancer cells. The critical role of HIF-1 in breast cancer metastasis to the lungs has been demonstrated by genetic knockout or knockdown of HIF-1 in autochthonous [9] and orthotopic [10] mouse models, respectively. Previously, we demonstrated by genetic approaches that the HIF-1 → LOX/LOXL pathway is crucial for breast cancer metastatic niche formation [7]. Knockdown of LOX or LOXL4 in MDA-231 cells and knockdown of LOXL2 in MDA-435 cells suppressed collagen cross-linking, BMDC recruitment, and breast cancer metastasis [7]. Here, we show that two pharmacologic HIF-1 inhibitors, digoxin and acriflavine, are capable of blocking this early step of breast cancer metastasis. Although metastasis is commonly considered a late stage in cancer progression, recent data from our lab and others has demonstrated that the HIF-dependent process of metastatic niche formation is initiated within days after MFP injection of human breast cancer cells [7, 8]. These results may explain why HIF-1α expression correlates with patient mortality even in early-stage, lymph node-negative breast cancers [28] and are consistent with immunohistochemical data indicating that increased HIF-1α levels in the diagnostic breast cancer biopsy may identify women at increased risk of metastasis [29]. Our data also suggest that patients with HIF-1α-overexpressing breast cancers may benefit from inclusion of a HIF inhibitor in their therapeutic regimen. A clinical trial utilizing topotecan to inhibit HIF-1α expression was recently reported [30].
Although the present study has focused on the role of HIFs in metastatic niche formation, the involvement of HIFs in other steps of metastasis has been demonstrated in previous studies. First, HIF activity enhances epithelial-mesenchymal transition (EMT), a step in which adherens junctions between cancer cells are lost due to decreased E-cadherin expression [31]. HIFs promote EMT via induction of repressors of E-cadherin gene transcription including TCF3 [32], ZEB1/2 [32], SNAIL [33], and TWIST1 [34]. Second, HIFs enhance cancer cell migration and invasion through activation of c-Met expression [35]. Third, HIFs enhance basement membrane disruption through induction of matrix metalloproteinase 2 (MMP2) [36], membrane type-1 MMP [37], and the urokinase-type plasminogen activator receptor [36], which facilitate local invasion of cancer cells. Fourth, HIF-dependent expression of L1CAM promotes binding of circulating tumor cells to vascular endothelial cells, thereby promoting extravasation [10]. Fifth, HIFs induce expression of MMP1 [38], MMP2 [38], vascular endothelial growth factor (VEGF) [39], and angiopoietin-like 4 [10], which enhance vessel permeability, thereby facilitating intravasation or extravasation. Sixth, HIFs promote metastatic growth through VEGF-dependent angiogenesis [40]. Finally, data from this study and others [5, 26, 41–43] indicate that LOX/LOXL expression promotes cancer cell invasion in the primary tumor. Thus, digoxin and acriflavine are likely to target multiple steps in breast cancer invasion and metastasis, which is consistent with the dramatic inhibitory effect of these drugs on lung metastasis.
The human cell lines utilized in this study, MDA-231 and MDA-435, are derived from triple-negative breast cancers, which are highly aggressive with frequent metastasis and have a high recurrence rate after neoadjuvant chemotherapy [2]. The effect of HIF inhibitors as single agents was examined in this study and potential combinatorial effects with other anti-cancer drugs require further investigation. Anthracyclines such as doxorubicin are administered as adjuvant therapy and first-line therapy for metastatic breast cancer [44]. Preliminary studies have indicated that combining low dose digoxin (1 mg/kg/day) with low-dose doxorubicin (2 mg/kg/week) resulted in significantly increased inhibition of MDA-231 tumor xenograft growth compared to either drug alone [10].
Digoxin has been used as treatment for congestive heart failure and atrial fibrillation for decades [45] and, prior to the development of antibiotics, acriflavine was administered as an anti-bacterial agent for periods of up to 5 months [46]. Thus, both digoxin and acriflavine are suitable candidates for clinical trials for breast cancer, especially in those patients whose primary tumors express high levels of HIF-1α.
Acknowledgements
We thank Karen Padgett (Novus Biologicals) for providing antibodies against LOXL2, LOXL4, and CD11b; and Rashmi Bankoti and Sergio Rey for advice. This work was supported by grants from the Emerald Foundation and National Cancer Institute (U54-CA143868) and funds from the Johns Hopkins Institute for Cell Engineering.
Footnotes
Disclosure statement G.L.S. is the C. Michael Armstrong Professor at Johns Hopkins University School of Medicine and an American Cancer Society Research Professor. C.C.W. is a Croucher Foundation Fellow. All authors confirm that there is no conflict of interest associated with this publication.
Contributor Information
Carmen Chak-Lui Wong, Vascular Program, Institute for Cell Engineering, Johns Hopkins University School of Medicine, Baltimore, MD 21205, USA; McKusick-Nathans Institute of Genetics, Johns Hopkins University School of Medicine, Baltimore, MD 21205, USA.
Huafeng Zhang, Vascular Program, Institute for Cell Engineering, Johns Hopkins University School of Medicine, Baltimore, MD 21205, USA; Department of Oncology, Johns Hopkins University School of Medicine, Baltimore, MD 21205, USA.
Daniele M. Gilkes, Vascular Program, Institute for Cell Engineering, Johns Hopkins University School of Medicine, Baltimore, MD 21205, USA McKusick-Nathans Institute of Genetics, Johns Hopkins University School of Medicine, Baltimore, MD 21205, USA.
Jasper Chen, Vascular Program, Institute for Cell Engineering, Johns Hopkins University School of Medicine, Baltimore, MD 21205, USA; McKusick-Nathans Institute of Genetics, Johns Hopkins University School of Medicine, Baltimore, MD 21205, USA.
Hong Wei, Vascular Program, Institute for Cell Engineering, Johns Hopkins University School of Medicine, Baltimore, MD 21205, USA; McKusick-Nathans Institute of Genetics, Johns Hopkins University School of Medicine, Baltimore, MD 21205, USA.
Pallavi Chaturvedi, Vascular Program, Institute for Cell Engineering, Johns Hopkins University School of Medicine, Baltimore, MD 21205, USA; McKusick-Nathans Institute of Genetics, Johns Hopkins University School of Medicine, Baltimore, MD 21205, USA.
Maimon E. Hubbi, Vascular Program, Institute for Cell Engineering, Johns Hopkins University School of Medicine, Baltimore, MD 21205, USA McKusick-Nathans Institute of Genetics, Johns Hopkins University School of Medicine, Baltimore, MD 21205, USA.
Gregg L. Semenza, Vascular Program, Institute for Cell Engineering, Johns Hopkins University School of Medicine, Baltimore, MD 21205, USA McKusick-Nathans Institute of Genetics, Johns Hopkins University School of Medicine, Baltimore, MD 21205, USA; Department of Oncology, Johns Hopkins University School of Medicine, Baltimore, MD 21205, USA; Departments of Pediatrics, Medicine, Radiation Oncology, and Biological Chemistry, Johns Hopkins University School of Medicine, Baltimore, MD 21205, USA.
References
- 1.Weigelt B, Peterse JL, van't Veer LJ. Breast cancer metastasis: markers and models. Nat Rev Cancer. 2005;5:591–602. doi: 10.1038/nrc1670. [DOI] [PubMed] [Google Scholar]
- 2.Pal SK, Childs BH, Pegram M. Triple negative breast cancer: unmet medical needs. Breast Cancer Res Treat. 2011;125:627–636. doi: 10.1007/s10549-010-1293-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vaupel P, Mayer A, Hockel M. Tumor hypoxia and malignant progression. Methods Enzymol. 2004;381:335–354. doi: 10.1016/S0076-6879(04)81023-1. [DOI] [PubMed] [Google Scholar]
- 4.Semenza GL. Defining the role of hypoxia-inducible factor 1 in cancer biology and therapeutics. Oncogene. 2010;29:625–634. doi: 10.1038/onc.2009.441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Erler JT, Bennewith KL, Nicolau M, Dornhofer N, Kong C, Le QT, Chi JT, Jeffrey SS, Giaccia AJ. Lysyl oxidase is essential for hypoxia-induced metastasis. Nature. 2006;440:1222–1226. doi: 10.1038/nature04695. [DOI] [PubMed] [Google Scholar]
- 6.Tafani M, Russo A, Di Vito M, Sale P, Pellegrini L, Schito L, Gentileschi S, Bracaglia R, Marandino F, Garaci E, et al. Up-regulation of pro-inflammatory genes as adaptation to hypoxia in MCF-7 cells and in human mammary invasive carcinoma microenvironment. Cancer Sci. 2010;101:1014–1023. doi: 10.1111/j.1349-7006.2010.01493.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wong CC, Gilkes DM, Zhang H, Chen J, Wei H, Chaturvedi P, Fraley SI, Wong CM, Khoo US, Ng IO, et al. Hypoxia-inducible factor 1 is a master regulator of breast cancer metastatic niche formation. Proc Natl Acad Sci USA. 2011;108:16369–16374. doi: 10.1073/pnas.1113483108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Erler JT, Bennewith KL, Cox TR, Lang G, Bird D, Koong A, Le QT, Giaccia AJ. Hypoxia-induced lysyl oxidase is a critical mediator of bone marrow cell recruitment to form the premetastatic niche. Cancer Cell. 2009;15:35–44. doi: 10.1016/j.ccr.2008.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liao D, Corle C, Seagroves TN, Johnson RS. Hypoxia-inducible factor-1α is a key regulator of metastasis in a transgenic model of cancer initiation and progression. Cancer Res. 2007;67:563–572. doi: 10.1158/0008-5472.CAN-06-2701. [DOI] [PubMed] [Google Scholar]
- 10.Zhang H, Wong CC, Wei H, Gilkes DM, Korangath P, Chaturvedi P, Schito L, Chen J, Krishnamachary B, Winnard PT, Jr, et al. HIF-1-dependent expression of angiopoietin-like 4 and L1CAM mediates vascular metastasis of hypoxic breast cancer cells to the lungs. Oncogene. 2011 doi: 10.1038/onc.2011.365. 2011 Aug 22. doi: 10.1038/onc.2011.365. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 11.Moeller BJ, Cao Y, Li CY, Dewhirst MW. Radiation activates HIF-1 to regulate vascular radiosensitivity in tumors: role of reoxygenation, free radicals, and stress granules. Cancer Cell. 2004;5:429–441. doi: 10.1016/s1535-6108(04)00115-1. [DOI] [PubMed] [Google Scholar]
- 12.Kaplan RN, Riba RD, Zacharoulis S, Bramley AH, Vincent L, Costa C, MacDonald DD, Jin DK, Shido K, Kerns SA, et al. VEGFR1-positive haematopoietic bone marrow progenitors initiate the pre-metastatic niche. Nature. 2005;438:820–827. doi: 10.1038/nature04186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Csiszar K. Lysyl oxidases: a novel multifunctional amine oxidase family. Prog Nucleic Acid Res Mol Biol. 2001;70:1–32. doi: 10.1016/s0079-6603(01)70012-8. [DOI] [PubMed] [Google Scholar]
- 14.Gao D, Nolan DJ, Mellick AS, Bambino K, McDonnell K, Mittal V. Endothelial progenitor cells control the angiogenic switch in mouse lung metastasis. Science. 2008;319:195–198. doi: 10.1126/science.1150224. [DOI] [PubMed] [Google Scholar]
- 15.Lyden D, Hattori K, Dias S, Costa C, Blaikie P, Butros L, Chadburn A, Heissig B, Marks W, Witte L, et al. Impaired recruitment of bone-marrow-derived endothelial and hematopoietic precursor cells blocks tumor angiogenesis and growth. Nat Med. 2001;7:1194–1201. doi: 10.1038/nm1101-1194. [DOI] [PubMed] [Google Scholar]
- 16.Yang L, DeBusk LM, Fukuda K, Fingleton B, Green-Jarvis B, Shyr Y, Matrisian LM, Carbone DP, Lin PC. Expansion of myeloid immune suppressor Gr+CD11b+ cells in tumor-bearing host directly promotes tumor angiogenesis. Cancer Cell. 2004;6:409–421. doi: 10.1016/j.ccr.2004.08.031. [DOI] [PubMed] [Google Scholar]
- 17.Liu C, Yu S, Kappes J, Wang J, Grizzle WE, Zinn KR, Zhang HG. Expansion of spleen myeloid suppressor cells represses NK cell cytotoxicity in tumor-bearing host. Blood. 2007;109:4336–4342. doi: 10.1182/blood-2006-09-046201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang H, Qian DZ, Tan YS, Lee K, Gao P, Ren YR, Rey S, Hammers H, Chang D, Pili R, et al. Digoxin and other cardiac glycosides inhibit HIF-1〈 synthesis and block tumor growth. Proc Natl Acad Sci U S A. 2008;105:19579–19586. doi: 10.1073/pnas.0809763105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee K, Zhang H, Qian DZ, Rey S, Liu JO, Semenza GL. Acriflavine inhibits HIF-1 dimerization, tumor growth, and vascularization. Proc Natl Acad Sci USA. 2009;106:17910–17915. doi: 10.1073/pnas.0909353106. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 20.Semenza GL, Jiang BH, Leung SW, Passantino R, Concordet JP, Maire P, Giallongo A. Hypoxia response elements in the aldolase A, enolase 1, and lactate dehydrogenase A gene promoters contain essential binding sites for hypoxia-inducible factor 1. J Biol Chem. 1996;271:32529–32537. doi: 10.1074/jbc.271.51.32529. [DOI] [PubMed] [Google Scholar]
- 21.Karnoub AE, Dash AB, Vo AP, Sullivan A, Brooks MW, Bell GW, Richardson AL, Polyak K, Tubo R, Weinberg RA. Mesenchymal stem cells within tumour stroma promote breast cancer metastasis. Nature. 2007;449:557–563. doi: 10.1038/nature06188. [DOI] [PubMed] [Google Scholar]
- 22.Finak G, Bertos N, Pepin F, Sadekova S, Souleimanova M, Zhao H, Chen H, Omeroglu G, Meterissian S, Omeroglu A, et al. Stromal gene expression predicts clinical outcome in breast cancer. Nat Med. 2008;14:518–527. doi: 10.1038/nm1764. [DOI] [PubMed] [Google Scholar]
- 23.Cailleau R, Young R, Olive M, Reeves WJ., Jr Breast tumor cell lines from pleural effusions. J Natl Cancer Inst. 1974;53:661–674. doi: 10.1093/jnci/53.3.661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rae JM, Creighton CJ, Meck JM, Haddad BR, Johnson MD. MDA-MB-435 cells are derived from M14 melanoma cells--a loss for breast cancer, but a boon for melanoma research. Breast Cancer Res Treat. 2007;104:13–19. doi: 10.1007/s10549-006-9392-8. [DOI] [PubMed] [Google Scholar]
- 25.Chambers AF. MDA-MB-435 and M14 cell lines: identical but not M14 melanoma? Cancer Res. 2009;69:5292–5293. doi: 10.1158/0008-5472.CAN-09-1528. [DOI] [PubMed] [Google Scholar]
- 26.Barry-Hamilton V, Spangler R, Marshall D, McCauley S, Rodriguez HM, Oyasu M, Mikels A, Vaysberg M, Ghermazien H, Wai C, et al. Allosteric inhibition of lysyl oxidase-like-2 impedes the development of a pathologic microenvironment. Nat Med. 2010;16:1009–1017. doi: 10.1038/nm.2208. [DOI] [PubMed] [Google Scholar]
- 27.Payne SL, Hendrix MJ, Kirschmann DA. Paradoxical roles for lysyl oxidases in cancer--a prospect. J Cell Biochem. 2007;101:1338–1354. doi: 10.1002/jcb.21371. [DOI] [PubMed] [Google Scholar]
- 28.Bos R, van der Groep P, Greijer AE, Shvarts A, Meijer S, Pinedo HM, Semenza GL, van Diest PJ, van der Wall E. Levels of hypoxia-inducible factor-1〈 independently predict prognosis in patients with lymph node negative breast carcinoma. Cancer. 2003;97:1573–1581. doi: 10.1002/cncr.11246. [DOI] [PubMed] [Google Scholar]
- 29.Dales JP, Garcia S, Meunier-Carpentier S, Andrac-Meyer L, Haddad O, Lavaut MN, Allasia C, Bonnier P, Charpin C. Overexpression of hypoxia-inducible factor HIF-1α predicts early relapse in breast cancer: retrospective study in a series of 745 patients. Int J Cancer. 2005;116:734–739. doi: 10.1002/ijc.20984. [DOI] [PubMed] [Google Scholar]
- 30.Kummar S, Raffeld M, Juwara L, Horneffer Y, Strassberger A, Allen D, Steinberg SM, Rapisarda A, Spencer SD, Figg WD, et al. Multihistology, target-driven pilot trial of oral topotecan as an inhibitor of hypoxia-inducible factor-1α in advanced solid tumors. Clin Cancer Res. 2011;17:5123–5131. doi: 10.1158/1078-0432.CCR-11-0682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yang J, Weinberg RA. Epithelial-mesenchymal transition: at the crossroads of development and tumor metastasis. Dev Cell. 2008;14:818–829. doi: 10.1016/j.devcel.2008.05.009. [DOI] [PubMed] [Google Scholar]
- 32.Krishnamachary B, Zagzag D, Nagasawa H, Rainey K, Okuyama H, Baek JH, Semenza GL. Hypoxia-inducible factor-1-dependent repression of E-cadherin in von Hippel-Lindau tumor suppressor-null renal cell carcinoma mediated by TCF3, ZFHX1A, and ZFHX1B. Cancer Res. 2006;66:2725–2731. doi: 10.1158/0008-5472.CAN-05-3719. [DOI] [PubMed] [Google Scholar]
- 33.Imai T, Horiuchi A, Wang C, Oka K, Ohira S, Nikaido T, Konishi I. Hypoxia attenuates the expression of E-cadherin via up-regulation of SNAIL in ovarian carcinoma cells. Am J Pathol. 2003;163:1437–1447. doi: 10.1016/S0002-9440(10)63501-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yang MH, Wu MZ, Chiou SH, Chen PM, Chang SY, Liu CJ, Teng SC, Wu KJ. Direct regulation of TWIST by HIF-1α promotes metastasis. Nat Cell Biol. 2008;10:295–305. doi: 10.1038/ncb1691. [DOI] [PubMed] [Google Scholar]
- 35.Pennacchietti S, Michieli P, Galluzzo M, Mazzone M, Giordano S, Comoglio PM. Hypoxia promotes invasive growth by transcriptional activation of the met protooncogene. Cancer Cell. 2003;3:347–361. doi: 10.1016/s1535-6108(03)00085-0. [DOI] [PubMed] [Google Scholar]
- 36.Krishnamachary B, Berg-Dixon S, Kelly B, Agani F, Feldser D, Ferreira G, Iyer N, LaRusch J, Pak B, Taghavi P, et al. Regulation of colon carcinoma cell invasion by hypoxia-inducible factor 1. Cancer Res. 2003;63:1138–1143. [PubMed] [Google Scholar]
- 37.Petrella BL, Lohi J, Brinckerhoff CE. Identification of membrane type-1 matrix metalloproteinase as a target of hypoxia-inducible factor-2〈 in von Hippel-Lindau renal cell carcinoma. Oncogene. 2005;24:1043–1052. doi: 10.1038/sj.onc.1208305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shyu KG, Hsu FL, Wang MJ, Wang BW, Lin S. Hypoxia-inducible factor 1α regulates lung adenocarcinoma cell invasion. Exp Cell Res. 2007;313:1181–1191. doi: 10.1016/j.yexcr.2007.01.013. [DOI] [PubMed] [Google Scholar]
- 39.Forsythe JA, Jiang BH, Iyer NV, Agani F, Leung SW, Koos RD, Semenza GL. Activation of vascular endothelial growth factor gene transcription by hypoxia-inducible factor 1. Mol Cell Biol. 1996;16:4604–4613. doi: 10.1128/mcb.16.9.4604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lu X, Yan CH, Yuan M, Wei Y, Hu G, Kang Y. In vivo dynamics and distinct functions of hypoxia in primary tumor growth and organotropic metastasis of breast cancer. Cancer Res. 2010;70:3905–3914. doi: 10.1158/0008-5472.CAN-09-3739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Levental KR, Yu H, Kass L, Lakins JN, Egeblad M, Erler JT, Fong SF, Csiszar K, Giaccia A, Weninger W, et al. Matrix crosslinking forces tumor progression by enhancing integrin signaling. Cell. 2009;139:891–906. doi: 10.1016/j.cell.2009.10.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Peinado H, Del Carmen Iglesias-de la Cruz M, Olmeda D, Csiszar K, Fong KS, Vega S, Nieto MA, Cano A, Portillo F. A molecular role for lysyl oxidase-like 2 enzyme in snail regulation and tumor progression. EMBO J. 2005;24:3446–3458. doi: 10.1038/sj.emboj.7600781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Schietke R, Warnecke C, Wacker I, Schodel J, Mole DR, Campean V, Amann K, Goppelt-Struebe M, Behrens J, Eckardt KU, et al. The lysyl oxidases LOX and LOXL2 are necessary and sufficient to repress E-cadherin in hypoxia: insights into cellular transformation processes mediated by HIF-1. J Biol Chem. 2010;285:6658–6669. doi: 10.1074/jbc.M109.042424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Palmieri C, Krell J, James CR, Harper-Wynne C, Misra V, Cleator S, Miles D. Rechallenging with anthracyclines and taxanes in metastatic breast cancer. Nat Rev Clin Oncol. 7:561–574. doi: 10.1038/nrclinonc.2010.122. [DOI] [PubMed] [Google Scholar]
- 45.Riganti C, Campia I, Kopecka J, Gazzano E, Doublier S, Aldieri E, Bosia A, Ghigo D. Pleiotropic effects of cardioactive glycosides. Curr Med Chem. 18:872–885. doi: 10.2174/092986711794927685. [DOI] [PubMed] [Google Scholar]
- 46.Wainwright M. Acridine - a neglected antibacterial chromophore. J Antimicrob Chemother. 2001;47:1–13. doi: 10.1093/jac/47.1.1. [DOI] [PubMed] [Google Scholar]