Abstract
Background
Lupoid cutaneous leishmaniasis (CL) is a rare form of CL having a striking resemblance to other granulomatous cutaneous conditions of infectious or inflammatory origin. The authors present a patient with a facial lupoid CL and discuss the diagnostic tools of this parasitological infection, the main differential diagnosis, and treatment.
Case report
A 54-year-old Tunisian woman, with no past medical history of lupus erythematosus or infectious disease, presented with a 3-month history of a slowly enlarging erythematous and infiltrated plaque, extending over the nose, the right cheek, and the internal aspect of the right lower eyelid. Microscopic examination of a parasitological smear showed numerous leishmania in their amastigote form, inside monocytes, confirming the diagnosis of CL. Clinical aspect was in favor of lupoid CL. The patient was cured by fluconazole 200 mg/day for 6 weeks after pancreatic intolerance with intramuscular meglumine antimoniate (60 mg/kg/day for 7 days), and no response to doxycycline (200 mg/day for 6 weeks).
Discussion
Lupoid CL is easily suspected in countries in which there is an endemic of leishmaniasis. In countries where there isn’t an endemic, although rarely observed, this diagnosis should also be kept in mind in front of an infiltrated facial lesion of a tuberculoid aspect on histology, especially when there is a positive travel history to an area in which there is an endemic.
Keywords: erythematous plaque, granulomatous cutaneous conditions, leishmania protozoa, lupoid cutaneous leishmaniasis
BACKGROUND
Cutaneous leishmaniasis (CL) is a widespread parasitic disease in Tunisia with numerous clinical presentations. The authors report a case of facial lupoid CL in a Tunisian patient. Lupoid leishmaniasis is the most common CL among patients with unusual presentations.1 The authors present its clinical feature, the diagnostic tools, differential diagnosis, course, and treatment of this uncommon long-lasting form of CL.
CASE REPORT
A 54-year-old Tunisian woman, with no past medical history, presented with a 3-month history of a slowly enlarging erythematous plaque of the central face. The patient had no other complaint. She was born and lived in a North-West city of Tunisia. The lesion started as a small, asymptomatic papule that slowly increased in size. Cutaneous examination showed a large solitary erythematous and infiltrated plaque, extending over the nose, a large part of the right cheek, and reaching the internal aspect of the right lower eyelid. Over the nose, the lesion appeared slightly squamous (Figure 1). Physical examination was otherwise normal; there was no fever or palpable lymph nodes. The patient did not respond to oral amoxicillin (4 g/day) for 10 days, prescribed by another physician before she was referred to our department. A parasitological smear after a skin scraping was performed. The resulting tissue was smeared on a slide and stained with May Grünwald Giemsa (Merck K GaA, 64271, Darmstadt, Germany). Microscopic examination showed numerous leishmania appearing in their amastigote form, outside monocytes (Figure 2), confirming the clinical suspicion of CL. Clinical aspect evoked the lupoid form of CL. The patient was treated with intramuscular injections of meglumine antimoniate (MA), 60 mg/kg/day. On the 7th day of treatment, she had elevated levels of serum amylase (two times the normal level) with high urine amylases. MA was stopped and replaced by doxycycline 200 mg/day for 6 weeks. The latter therapy was inefficient with extension of the plaque over the left cheek. She then underwent fluconazole 200 mg/day for 6 weeks, with a significant improvement of the lesion.
Figure 1.

Large erythematous and infiltrated plaque, extending over the nose, the right cheek and reaching the internal aspect of the right lower eyelid.
Figure 2.
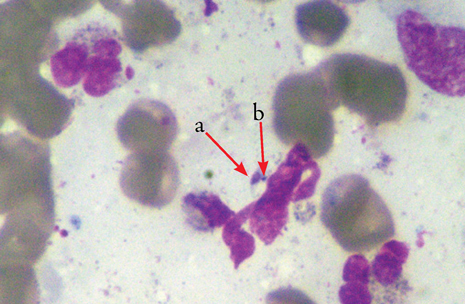
Extracellular amastigote form with the nucleus (a) and the kinetoplast (b).
DISCUSSION
CL is an infection caused by various species of leishmania protozoa. The parasite is inoculated and transmitted by the bite of phlebotomine sandflies. Tunisia is a country where CL is frequent and there have been incidences in which there has been an endemic and an epidemic of Old World leishmaniasis.2 Thus, the diagnosis of CL was easily suspected in our patient, when presented with such a facial lesion having a chronic course with no signs of inflammation, pain, or pruritus. In Tunisia, there are three main epidemiological and clinical forms, depending on geographic origin and each due to a different species of leishmania: the sporadic CL, which is predominant in the North of Tunisia and caused by Leishmania infantum MON-24, the zoonotic form (Centre and South-West of Tunisia) caused by Leishmania major MON-25, and the chronic CL occurring in the Southern-East of Tunisia and caused by Leishmania killicki.3 The most frequent form is the zoonotic form, which is epidemic with a seasonal outbreak especially in autumn and summer (mean of 3000–5000 cases per year).3 In zoonotic CL, lesions have a rapid self-limiting evolution and in the absence of treatment, lesions heal in 6–8 months. In contrast, the chronic form is a long-lasting infection with a 2–6 year duration having an endemic pattern along the year (50–100 cases per year).3,4
Since the patient originates from and lives in the North of Tunisia, our patient probably had the sporadic form of CL (L. infantum). The sporadic form is also a relatively long-lasting infection with a 1–2 year duration. It occurs at an incidence of 30 cases per year.3
The typical clinical presentation is an erythematous infiltrated, ulcerated, and crusted papule or nodule (classical oriental sore) of any region of the body, with a frequent involvement of exposed areas, especially the face and limbs. This typical lesion heals slowly over a period of 3–12 months and constitutes the most frequent one.5 There are many other clinical forms of CL, among them the lupoid CL, observed in the present patient, which is a particularly uncommon form with characteristic spreading of the initial lesion leading to a solitary erythematous; infiltrated plaque with unlimited borders progressively confounding with adjacent normal skin. Sometimes, brown-red or brown-yellow papules appear and progressively coalesce and even lead to the formation of apple-jelly nodules, characteristic of the lupoid aspect of this form.6,7 The lesion may even be squamous with a psoriasiform aspect or produce crusts, and may closely resemble lupus vulgaris (LV). Although not as destructive as LV, lupoid CL may persist and spread for many years and aggravate gradually.7,8
Lupoid CL is most prevalent in the endemic areas of leishmaniasis, particularly in the Middle East and Afghanistan with a reported incidence of 0.5%–6.2% of all CL cases.9 In Tunisia, in a recent study including sporadic CL cases, lupoid CL represented 8.9% of cases in adults.10
It seems that in lupoid CL, the parasite is not killed, but it replicates inside the macrophage. These findings suggest that certain leishmanial strains, which induce chronic disease, may have the capacity to evade intracellular destruction by activated macrophages, or that there is a defect in the T-cell activation process.7,11
In lupoid CL, the amastigote forms are rare or absent on a parasitological smear.7,8 In this patient, there was fortunately a positive parasitological smear. This can be explained by the short course of the lesion (only 3 months) at the moment of diagnosis.
Histologically, the aspect is that of a tuberculoid granuloma with giant multinucleated cells but without classification. Intra-macrophagic amastigotes are also rare or usually absent.7,8
In this form of CL, promastigotes are also difficult to maintain on Novy-MacNeal-Nicolle (NNN) medium, especially in sporadic CL due to L. infantum. Although species-specific polymerase chain reaction (PCR) analysis is sensitive in cases of acute cutaneous leishmaniasis, Momeni et al. found lesser sensitivity of PCR in lupoid leishmaniasis (only 47%).6
In the literature, leishmania tropica is thought to be the most frequent causative agent of lupoid CL.7 In Tunisia, this form seems to be less rare with L. infantum and L. killicki.
In case of negative parasitological examination and in the absence of intra-amastigotes on histology, diagnosis is made based on suggestive clinical aspect, facial localization, chronic evolution, and sometimes patients may recall the initial sandfly bite. All these criteria in a region where there is an endemic or epidemic of leishmaniasis, like Tunisia, or even in case of positive travel history to an endemic area, can aid in correct diagnosis. Despite all the above-mentioned arguments for the diagnosis of CL, when presented with such a facial lesion, the authors can evoke other diagnoses such as LV (cutaneous tuberculosis),12 lupus erythematosus (LE), or lupus pernio, which is a form of cutaneous sarcoidosis and facial erysipelas.12,13
In the absence of randomized controlled trials, there is not enough data about the correct and selective therapeutic protocol for the treatment of lupoid CL. Pentavalent antimony compounds are, at present, the first choice of treatment. This is also the case in Tunisia, where most clinicians use either intralesional MA or intramuscular injection of MA 60 mg/kg/day for 15–20 days in cases of resistance to local injections, multiple lesions (>5), proximity to the cartilage, joint, and periorificial lesions.10 This dose is considered as the standard dose of systemic MA in the treatment of CL.14 Oral fluconazole has been shown to be safe and effective for CL with advantages particularly important in pediatrics;15,16 for some authors it may be a second line treatment.17 The patient responded adequately to fluconazole after MA intolerance. Many other treatments have been reported to be used as monotherapy in treating CL such as cryotherapy, paramomycin ointment, intradermal injections of sodium stibogluconate, oral itraconazole, pentamidine, and miltefosine for the last few years. Lupoid CL is usually resistant to conventional therapies for CL and it may persist and spread slowly for many years.18,19 Due to possible resistance of lupoid CL to the previous modalities, combined therapies were tried. Momeni et al. reported a successful result with a combination of MA and allopurinol.20 Nilfrousihzadeh also showed that 17%, 57%, and 65% of complete cure of the lesions at the end of the 4th, 8th, and 10th week, respectively, were observed with combined cryotherapy, paramomycin, and intralesional MA in treating lupoid and chronic leishmaniasis,21 however, another study showed that carbon dioxide laser seems to be highly effective since it led to 90% efficacy in treating 24 patients with lupoid CL,18 and another study reported 16 cases who responded very well to MA without chronic infection or relapse, which suggests that lupoid CL should be revisited and redefined.7
CONCLUSION
In conclusion, while lupoid CL is an easily-suspected diagnosis in endemic countries for leishmaniasis, outside endemic areas it can be mistaken for other disorders due to a clinical similarity. Thus, this diagnosis should be considered in patients who present an infiltrated facial plaque with a tuberculoid granuloma on histology.
Acknowledgments
Dr. Goucha declares that there is no funding or sponsorship received in relation to this paper. Dr. Goucha is the guarantor for this article, and takes responsibility for the integrity of the work as a whole. There is no other person who contributed to the manuscript, other than the authors named. All authors declare they have no conflict of interest.
Open Access. This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Footnotes
To view enhanced content go to www.dermtherapy-open.com
This article is published with open access at Springerlink.com
References
- 1.Bari A.U., Rahman S.B. Many faces of cutaneous leishmaniasis. Indian J Dermatol Venereol Leprol. 2008;74:23–27. doi: 10.4103/0378-6323.38402. [DOI] [PubMed] [Google Scholar]
- 2.Masmoudi A., Ayadi N., Boudaya S., et al. Clinical polymorphism of cutaneous leishmaniasis in Centre and South of Tunisia. Bull Soc Pathol Exot. 2007;100:36–40. [PubMed] [Google Scholar]
- 3.Aoun K., Amri F., Chouihi E., et al. Epidemiology of Leishmania (L.) infantum, L. major and L. Killicki in Tunisia: results and analysis of the identification of 226 human and canine isolates. Bull Soc Pathol Exot. 2008;101:323–328. doi: 10.3185/pathexo3201. [DOI] [PubMed] [Google Scholar]
- 4.Bousslimi N., Aoun K., Ben-Abda I., Ben-Alaya-Bouafif N., Raouane M., Bouratbine A. Epidemiologic and clinical features of cutaneous leishmaniasis in southeastern Tunisia. Am J Trop Med Hyg. 2010;83:1034–1039. doi: 10.4269/ajtmh.2010.10-0234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kubba R., Al-Gindan Y., El-Hassan A.M., Omer A.H. Clinical diagnosis of cutaneous leishmaniasis (oriental sore) J Am Acad Dermatol. 1987;16:1183–1189. doi: 10.1016/S0190-9622(87)70155-8. [DOI] [PubMed] [Google Scholar]
- 6.Momeni A.Z., Yotsumoto S., Mehregan D.R., et al. Chronic lupoid leishmaniasis. Evaluation by polymerase chain reaction. Arch Dermatol. 1996;132:198–202. doi: 10.1001/archderm.1996.03890260100015. [DOI] [PubMed] [Google Scholar]
- 7.Ul Bari A., Raza N. Lupoid cutaneous leishmaniasis: a report of 16 cases. Indian J Dermatol Venereol Leprol. 2010;76:85. doi: 10.4103/0378-6323.58698. [DOI] [PubMed] [Google Scholar]
- 8.Masmoudi A., Boudaya S., Ayadi N., et al. Clinical and histological study of lupoid cutaneous leishmaniasis (16 cases) Presse Med. 2007;36:1738–1742. doi: 10.1016/j.lpm.2007.07.004. [DOI] [PubMed] [Google Scholar]
- 9.Gurel M.S., Ulukanligil M., Ozbilge H. Cutaneous leishmaniasis in Sanlurfia epidemiologic and clinical features of the last four years (1997–2000) Int J Dermatol. 2002;41:32–37. doi: 10.1046/j.0011-9059.2001.01396.x. [DOI] [PubMed] [Google Scholar]
- 10.Zaraa I., Ishak F., Kort R., et al. Childhood and adult cutaneous leishmaniasis in Tunisia. Int J Dermatol. 2010;49:790–793. doi: 10.1111/j.1365-4632.2010.04467.x. [DOI] [PubMed] [Google Scholar]
- 11.Farah F.S., Samra S.A., Nuwayri-Salti N. The role of the macrophage in cutaneous leishmaniasis. Immunology. 1975;29:755–764. [PMC free article] [PubMed] [Google Scholar]
- 12.Landau M., Srebrnik A., Brenner S. Leishmaniasis recidivans mimicking lupus vulgaris. Int J Dermatol. 1996;35:572–573. doi: 10.1111/j.1365-4362.1996.tb03658.x. [DOI] [PubMed] [Google Scholar]
- 13.Zahaf A., Turki H., Masmoudi A. Tubercular lupus. Ann Dermatol Venereol. 2004;131:503–507. doi: 10.1016/S0151-9638(04)93652-6. [DOI] [PubMed] [Google Scholar]
- 14.Nilforoushzadeh M.A., Jaffary F., Ansari N., Siadat A.H., Nilforoushan Z., Firouz A. A comparative study between the efficacy of systemic meglumine antimoniate therapy with standard or low dose plus oral omeprazole in the treatment of cutaneous leishmaniasis. J Vector Borne Dis. 2008;45:287–291. [PubMed] [Google Scholar]
- 15.Sklavos A.V., Walls T., Webber M.T., Watson A.B. Cutaneous leishmaniasis in a child treated with oral fluconazole. Australas J Dermatol. 2010;5:195–197. doi: 10.1111/j.1440-0960.2010.00642.x. [DOI] [PubMed] [Google Scholar]
- 16.Emad M., Hayati F., Fallahzadeh M.K., Namazi M.R. Superior efficacy of oral fluconazole 400 mg daily versus oral fluconazole 200 mg daily in the treatment of cutaneous leishmania major infection: a randomized clinical trial. J Am Acad Dermatol. 2011;64:606–608. doi: 10.1016/j.jaad.2010.04.014. [DOI] [PubMed] [Google Scholar]
- 17.Minodier P., Jurquet A.L., Noël G., Uters M., Laporte R., Garnier J.M. Leishmaniasis treatment. Arch Pediatr. 2010;17:838–839. doi: 10.1016/S0929-693X(10)70137-8. [DOI] [PubMed] [Google Scholar]
- 18.Asilian A., Iraji F., Hedaiti H.R., Siadat A.H., Enshaieh S. Carbon dioxide laser for the treatment of lupoid cutaneous leishmaniasis (LCL): a case series of 24 patients. Dermatol Online J. 2006;12:3. [PubMed] [Google Scholar]
- 19.Benmously Mlika R., Hammami H., Sioud A., Mokhtar I. Fenniche. Lupoid leishmaniasis of the nose responding well to cryotherapy. Dermatol Ther. 2011;24:378–379. doi: 10.1111/j.1529-8019.2011.01424.x. [DOI] [PubMed] [Google Scholar]
- 20.Momeni A.Z., Aminjavaheri M. Successful treatment of non-healing cases of cutaneous leishmaniasis, using a combination of meglumine antimoniate plus allopurinol. Eur J Dermatol. 2003;13:40–43. [PubMed] [Google Scholar]
- 21.Nilfrousihzadeh M.A., Jaffray F., Reiszadeh M.R., Ansari N. The therapeutic effect of combined cryotherapy, paramomycin, and intralesional meglumine antimoniate in treating lupoid leishmaniasis and chronic leishmaniasis. Int J Dermatol. 2006;45:989–991. doi: 10.1111/j.1365-4632.2006.02748.x. [DOI] [PubMed] [Google Scholar]


