Abstract
BACKGROUND
Anxiety and depressive disorders may pose a long-term, deleterious impact on youth, prompting a need for early and effective prevention of such concerns. A growing body of research has examined universal prevention programs targeting these emotional disorders in childhood. While most universal prevention programs are offered within the school setting, there is also a rationale for developing and investigating prevention programs within novel settings, including a recreational context.
OBJECTIVE
This initial investigation utilized the Emotion Detectives Prevention Program (EDPP), a universal prevention protocol focusing on anxiety and depression symptoms within a recreational summer camp. The aims of this pilot study were to assess the EDPP’s feasibility and participant satisfaction following its initial administration in a camp setting.
METHOD
Forty children (ages 7–10 years, 70.7% male) were recruited from an existent recreational sports camp and participated in a non-randomized, open trial of the EDPP. The EDPP, a 15-session program, presents cognitive-behavioral strategies in a manner that emphasizes strategy applicability across a range of emotional experiences.
RESULTS
Participating children reported a significant decrease in anxiety symptoms at post–prevention. No significant change in depression symptoms or other emotion regulation indices were reported. Moderate to high participant satisfaction was indicated.
CONCLUSIONS
The EDPP appears to be a feasible program for the prevention of child-reported anxiety symptoms in a camp setting. Given the novelty of the prevention context, issues inherent in the conduct of research in a recreational camp setting and future directions for research in this setting are discussed.
Keywords: Open Trial, Camp, Prevention, Anxiety, Depression, Children, Cognitive-Behavioral
Universal Prevention of Anxiety and Depression in a Recreational Camp Setting: An Initial Open Trial
Emotional disorders, such as anxiety and depression, are among the most prevalent mental disorders in childhood (Kessler, Chiu, Demler, & Walters, 2005). Evidence suggests that as many as 10 to 22% of youth experience clinical levels of anxiety (Dadds, Spence, Holland, Barrett, & Laurens 1997; Muris, Merckelbach, Mayer & Prins, 2000). Similarly, as many as two percent of children and 10% of adolescents suffer from mood disorders (Jellinek & Snyder, 1998; Wittchen, Nelson & Lachner, 1998). Depression and anxiety frequently present concurrently during youth, with an increasing frequency of such comorbidity in adolescence (Kessler et al., 1997). Current estimates indicate that as many as 90% of individuals experiencing clinical levels of depression also experience anxiety symptoms (Kessler et al., 1997; Pini, et al., 1997). In addition to being highly prevalent and comorbid, emotional disorders are functionally impairing, often chronic in course, and costly to treat over the long term (Kessler & Greenberg, 2002).
Children who experience clinically significant emotional disorders are unlikely to receive any treatment for these conditions (Wittchen, Stein, & Kessler, 1999). In fact, over three-quarters of youth experiencing mental health concerns never receive treatment (New Freedom Commission on Mental Health, 2003). Anxiety and depressive symptoms in youth may be particularly overlooked versus those with externalizing difficulties, the latter of whom appear more likely receive greater clinical attention at school and at home (Albano, Chorpita, & Barlow, 2003). The incidence of emotional disorders rises dramatically in adolescence. As these adolescents are unlikely to receive mental health treatment for these emotional disorders, the number of youth at risk for a protracted course of illness substantially rises during this time (Kessler, Ruscio, Shear, & Wittchen, 2010). Importantly, a window of opportunity for prevention of emotional disorders may be available in late childhood, prior to this marked increase in anxiety and depression rates during adolescence. To that end, the current investigation focuses on the development and initial open trial evaluation of the Emotion Detectives Prevention Program (EDPP), a universal prevention program for anxiety and depression directed at school age children and delivered in a novel camp environment.
Prevention Programs for Youth Anxiety and Depression
Programs devoted to the prevention of mental health disorders are often classified by the type of population for whom they are developed. Based on the presence or absence of relevant symptoms, programs may be classified as directing preventative skills in an indicated, targeted or universal manner (Gordon, 1987). Indicated prevention programs target individuals who are already experiencing symptoms of a disorder or problem area, often at a sub-clinical level. Targeted programs are applied to individuals evidencing risk factors for the development of a specific problem or disorder. Universal programs are applied to whole populations, without explicit regard to their risk status or current level of symptomatology.
While there is a strong rationale for developing and researching the efficacy of prevention programs across these three strategies, universal programs offer a number of unique advantages when considering the prevention of anxiety and depression. There is evidence that screening measures used to identify individuals for indicated prevention programs may not be sufficiently sensitive, and may fail to flag some individuals who are at risk (Dadds et al., 1997). Universal prevention programs are offered to all individuals regardless of risk status and therefore do not require highly sensitive screening measures. Initial research has also begun to examine the differential stigma associated with universal and indicated prevention programs. The difference in stigma perceived between such programs has been found to be small, but significant, with initial findings suggesting that universal programs are associated with less social stigma than other types of prevention programming (Rapee, 2009). When considering anxiety and depressive disorders more specifically, it is relevant to consider the high lifetime prevalence rates for these disorders and their sub-clinical manifestations (Craske, 1997; Kessler, Zhao, Blazer & Swartz, 1997a). Universal prevention programs developed to help children cope with anxiety and depression symptoms can teach relevant strategies to all individuals, including those who may be currently at risk or those that may experience such risks in the future. Durlak and Wells’ (1997) meta-analysis of universal prevention programs revealed small to medium effect sizes associated with improvements in internalizing concerns (Cohen’s d = 0.32). However, only 25% of the programs included within the meta-analysis included follow-up data, making the longevity of these effects difficult to examine. These results suggest that primary prevention programs are associated with modest but significant improvements in internalizing symptoms, although limited follow-up data may hasten enthusiasm about the durability of such effects.
Recent evidence indicates that cognitive behavioral principles and other strategies successful in the treatment of anxiety and depressive disorders may be particularly useful in the prevention of these disorders (Whittal, 2008). One natural avenue for the implementation of universal prevention programs that utilize such cognitive behavioral skills is the school setting. A recent meta-analysis of school-based prevention programs found 16 randomized, controlled trials that examined the efficacy of nine different programs for the universal prevention of anxiety (Neil & Christensen, 2009). Of these 16 trials, 11 (69%) demonstrated a significant difference between the control and prevention conditions, indicating the potential efficacy of school-based universal programs in the prevention of anxiety symptoms. In this meta-analysis, the FRIENDS program targeting anxiety symptoms (Barrett & Turner, 2001) had the greatest number of investigations, and demonstrated the largest effect size at follow-up of all child-directed programs (Neil & Christensen, 2009). Since its original conception, FRIENDS has been extended to include preventative skills for depression as well as anxiety (Farrell & Barrett; 2007), using a typical cognitive behavioral format incorporating physiological, cognitive and behaviorally-focused coping skills.
Studies evaluating the efficacy and effectiveness of FRIENDS indicate that this program is associated with reduced levels of child-reported anxiety symptoms at post-prevention, as compared to children attending schools assigned to a waitlist control condition (Lowry-Webster, Barrett, & Dadds, 2001). There is evidence that the FRIENDS program may also reduce depression symptoms; however, this result may not manifest until longer-term follow-up assessments (See Lowry-Webster et al., 2001; Lock & Barrett, 2003). Overall, evaluations of FRIENDS indicate that it is a generally effective prevention program for anxiety and potentially depression in the school context (for a comprehensive review of the literature evaluating FRIENDS, see Barrett, Farrell, Ollendick & Dadds, 2006).
Similar to the FRIENDS program, other studies of universal prevention programs have typically taken place in the school setting. Indeed, 73% of the universal prevention studies included in Durlak and Wells’ (1997) meta-analysis took place within a school setting. In many ways, the school setting lends itself very well to the study and implementation of universal prevention. Because primary education is obligatory and standardized in most countries, schools offer convenient and predictable access to large populations of children, including those individuals who experience heightened levels of emotional disorders, but have not received treatment. In terms of effective implementation, the school environment is a familiar setting to the students attending, and offers a naturalistic environment to practice and perfect skills (Barrett & Pahl, 2006). Additionally, school is a learning environment; so educational prevention programs may integrate well into the school day, or into an after-school program (Rambaldo, Wilding, Goldman, McClure, & Friedberg, 2001).
However, prevention programs also face inherent barriers when offered in a school context. Public schools are highly regulated, and often have very limited funding and resources. Teachers, schools, administrators and parents may have legitimate concerns about allocating the resources required for the effective training and delivery of prevention programs rather than to traditional education needs, which may be short-changed already (Owens & Murphy, 2004). Programs offered after school may also suffer from low levels of participant interest or from irregular attendance (e.g. Dynarski et al., 2003). Therefore, it may be concluded that, while research on school-based prevention programs offer one efficacious avenue for the implementation of universal prevention programs, there is also a rationale to investigate such programs in alternative community settings.
The Camp Environment as a Context for Prevention Programming
Recently, there have been successful attempts to investigate the feasibility of treatment programs for emotional disorders and other mental health concerns in camp-like settings, suggesting that a similar paradigm may be feasible for prevention programs. For instance, Santucci, Ehrenreich, Tropser, Bennett and Pincus (2009) developed a one-week intensive program for the treatment of separation anxiety disorder (SAD) in young girls (ages 7–12). This program teaches exposure-focused, cognitive behavioral treatment skills within a developmentally sensitive and creative, camp-like environment. The treatment plan for this program integrates enjoyable activities such as jewelry making, pottery painting and sleepovers into the treatment format to both extend the usage of certain skills to naturalistic social situations and to increase the overall interest and motivation of young participants (Santucci et al., 2009). The Summer Treatment Program (STP) for children with ADHD takes advantage of a summer camp environment to implement and generalize skills across a range of settings including the classroom, the playground and field sports (Pelham & Hoza, 1996). Additionally, Walker, Barry & Bader (2010) examined the benefits of offering a social skills intervention for children with autism spectrum disorders (ASD) as part of a summer treatment camp. They highlight the importance of taking advantage of the summer months to provide extended treatment options that might not be possible during the busy school year.
Camps providing prevention programming for at-risk youth or those experiencing life stressors have also been examined. Wu and colleagues (2010) evaluated a summer camp for children with cancer and their siblings. In line with the camp’s mission, participants reported that camp was a place where they could experience respite, as well as receive peer support in a unique environment tailored to their needs (Wu, Prout, Roberts, Parikshak & Amylon, 2010). Another camp for at risk youth, the AileyCamp, teaches dance and psychosocial competence skills to inner-city youth (Kirschman, Roberts, Shadlow & Pelley, 2010). Results from a five-year investigation indicated that the AileyCamp was associated with improved “hopeful thinking” and other positive outcomes. Together, these studies demonstrate that summer camps may be a convenient mechanism for incorporating psychosocial treatments, and that they also can provide opportunities for creatively teaching and generalizing treatment principles.
While there is a small treatment literature demonstrating the feasibility and efficacy of treatment-focused camps for mental health concerns and prevention-focused camps for those with other life stressors, there is no relevant research regarding prevention programs for mental health in a pre-existing recreational camp environment. The Emotion Detectives Prevention Program (EDPP; Ehrenreich-May & Bilek, 2009) was developed as a universal prevention for emotional disorders that may be implemented in an existent camp environment. The EDPP was developed initially as a downward extension of and a prevention framework for the Unified Protocols for the Treatment of Emotional Disorders for adults and youth (Barlow et al., 2010; Ehrenreich et al., 2008), both of which are transdiagnostic, cognitive-behavioral treatment approaches that use an emotion-focused framework to impart skills across a range of potential emotional disorders.
The aims of the current investigation were to examine initial outcomes as well as acceptability and feasibility issues associated with the implementation of a universal prevention program, the EDPP, within an existent summer camp environment. With regard to outcomes, we hypothesized that participants in the EDPP would evidence improvements in parent- and child-reported symptoms of anxiety and depression, in addition to gains in emotion-focused coping skills and other emotion regulation skills. Given the existent literature on camp-like treatment programs for emotional and behavioral problems, we hypothesized that the EDPP would achieve high acceptability among EDPP participants and their families. We further anticipated that the implementation of the EDPP would be feasible in a camp setting.
Method
Participants
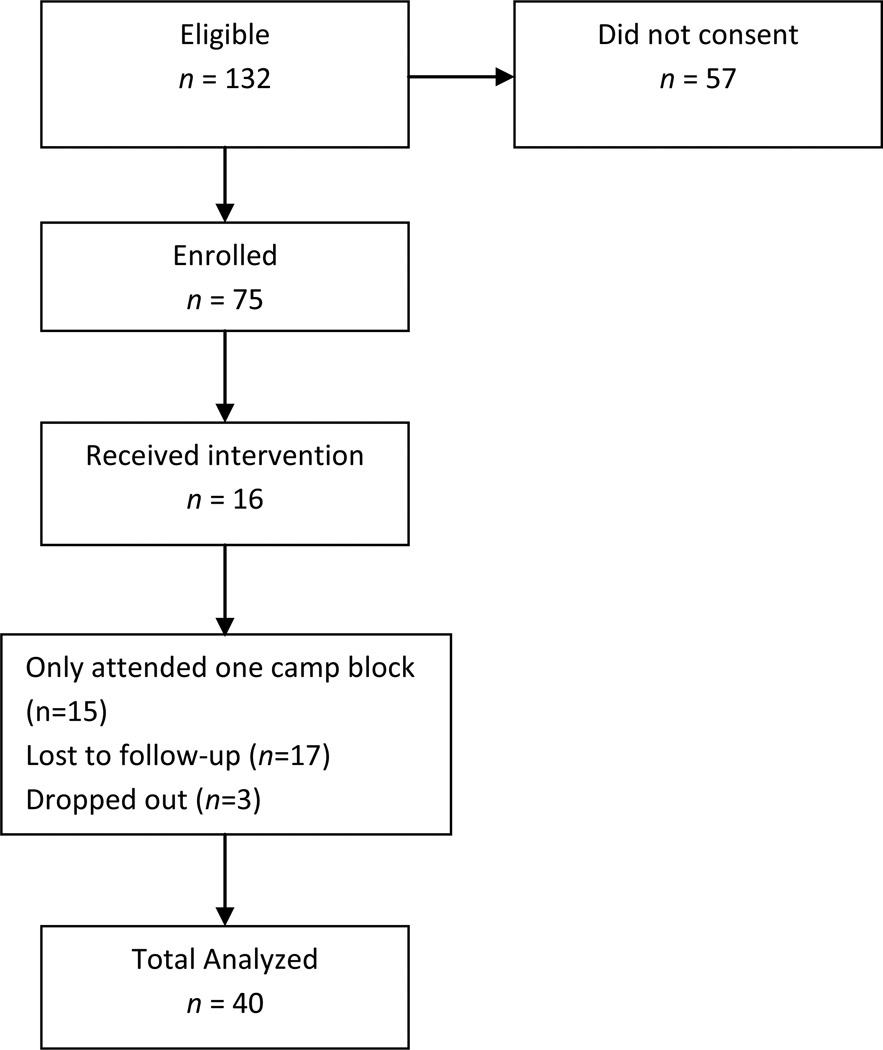
Participants in the EDPP were children between the ages of 7 to 10 years (inclusive) enrolled in a for-profit, recreational sports camp. Seventy-five male and female children (70.7% male; mean age=8.39 years) were recruited from a larger cohort of 150 eligible children to participate in EDPP twice per week during regular camp hours. The camp itself was implemented in four two-week blocks (with three to four sessions of the EDPP available to participants per block) during the summer of 2009. Forty boys and girls (70.0% male; mean age=8.45 years) completed more than one block of the EDPP and provided post-prevention data (see Figure 1 for a flow chart including recruitment and attrition information). Participating children were recruited from the camp regardless of pre-program scores on any measure. A total of 16 parents participated in optional EDPP parent sessions.
Figure 1.
Participant Enrollment Flow Diagram
Note: This flowchart is an adaptation of the flowchart offered by the Consolidated Standard of Reporting Studies Group (CONSORT; Altman et al., 2001; Moher, Schulz, & Altman, 2001).
Measures
Child-Report Measures
In order to assess for child symptomatology and emotion regulation strategies, children completed questionnaires in person at their first (T1) and last (T2) EDPP session. At each time point (with the exception of End of Program Questionnaire, only completed at T2), children completed the following measures. Younger children that expressed difficulty reading or understanding items were assisted by a group leader.
Screen for Child Anxiety Related Emotional Disorders, Child Report (SCARED; Birmaher, et al., 1999)
This 41-item questionnaire assesses a child’s perceptions of fear and anxiety symptoms. Children are instructed to respond to questions in terms of how they react to different situations. They are asked to indicate the degree and frequency of each item for themselves on a three point, Likert-type scale, ranging from “Not True or Hardly Ever True” to “Very True or Often True”. The questionnaire provides five subscale scores including: Panic, Generalized Anxiety, Separation Anxiety, Social Anxiety and School Avoidance. The questionnaire also provides an overall score (0–82) with a score of 26 or greater indicating elevated anxiety symptoms (Birmaher et al., 1999). The SCARED has demonstrated good test-retest reliability (intraclass correlation coefficients =.70 to .90) and validity (Birmaher et al., 1999). In the current study, the SCARED demonstrated excellent internal consistency at pre- and post-program (α=.91; .94 respectively).
Center for Epidemiologic Studies-Depression Scale (CES-D; Radloff, 1977)
This 20-item questionnaire assesses the child’s depressive symptoms during the past week. Children are instructed to respond to how frequently they have felt or experienced these symptoms on a four point, Likert-type scale, ranging from rarely or none of the time to most or all of the time. The questionnaire provides an overall score (0–60) with a score of 16 or greater indicating elevated depressive symptoms (Weissman, Sholomskas, Pottemger, Prusoff & Locke, 1977). The CES-D has demonstrated adequate test-retest reliability in an adolescent sample (intraclass correlation coefficients [ICC] =.49 to .60; Roberts, Andrews, Lewinsohn & Hops, 1990). In the current study, the CES-D demonstrated acceptable to good internal consistency pre- and post-program (α=.71; .83 respectively).
Emotion Regulation Questionnaire – Child and Adolescent (ERQ-CA; MacDermott, Betts, Gullone, & Allen, submitted for publication)
The ERQ-CA is a 10-item questionnaire assessing the child’s ability to regulate emotions. Children are instructed to respond to questions about how they feel inside and how they manage their emotions. They are asked to indicate how much they agree with each of 10 statements on a four point, Likert-type scale. The scale provides scores for two subscales: reappraisal and suppression. An initial psychometric investigation of the scale with 1745 children ages 9–16, demonstrated good internal consistency, especially for the Reappraisal scale. It has also demonstrated fair test-retest reliability for both scales (r = .54 Reappraisal, .59 Suppression; MacDermott et al., submitted for publication). In the current study, the ERQ-CA demonstrated only fair internal consistency pre-program and acceptable post-program (α=.56; .62 respectively), in comparison to previously reported internal consistency findings.
End of Program Questionnaire
Children also completed a short End of Program Questionnaire at T2. This Program Evaluation questionnaire was developed for this investigation and included 10 items with a nine point, Likert-type scale inquiring to what degree the child believes he/she benefited from the program (responses range from 0= Not at All, to 8=Very Much). Sample items include: How much do you think this program has helped you deal with difficult emotions? How much would you recommend this program to a friend who was having a tough time dealing with his emotions? In the current study, the End of Program Questionnaire demonstrated excellent internal consistency (α=.88).
Parent-Report Measures
In order to assess child symptomatology and emotion regulation strategies, parents were administered questionnaires via an online survey program created for this investigation and administered through a secure server. Parents were sent a unique participant identification number and password that gave access to their own questionnaires online. They were prompted to complete these questionnaires through email and phone call reminders at two different time points: upon starting the EDPP (T1), and upon completing the program (T2). At T1 and T2 parents completed parent-report versions of the CES-D (with the parent sample, the CES-D demonstrated acceptable internal consistency pre- and post-program (α=.77; .68 respectively) and the SCARED (with the parent sample, the SCARED demonstrated a higher level of internal consistency, pre- and post-program (α=.89; .87 respectively). Parents also completed the following measures at T1 and T2.
Children’s Emotion Management Scales (CEMS; Zeman, Shipman & Penza-Clyve, 2001)
This 36-item questionnaire assesses parent report of a child’s ability to manage the emotions of fear (10 items), anger (11 items) and sadness (12 items). The scale provides scores for three subscales including inhibition, coping and dysregulation, which are calculated for each emotion. Total inhibition, coping and dysregulation scores are also calculated. The CEMS has demonstrated good internal consistency and test-retest reliability for each scale (Zeman et al., 2001). The scale was normed with children ages 9–12, but has been successfully used with children as young as 6 and 7 (Penza-Clyve, Zeman, & Sim, 1999; Suveg, Sood, Comer & Kendall, 2009). In the current study, the CEMS demonstrated acceptable pre- and post-program internal consistency (α=.63; .63 respectively).
End of Program Questionnaire
Parents also completed a parallel form of the End of Program questionnaire at T2. The End of Program Questionnaire demonstrated good internal consistency in this investigation (α=.93).
Procedure
Recruitment
In the spring of 2009, a letter including an IRB-approved consent form and brochure was sent to all parents of children between the ages of 7 and 10 enrolled in a recreational sports camp. The letter explained that the summer camp had decided to offer an experimental prevention program as educational programming for the summer. Parents were informed that the program would focus on teaching children how to understand and manage their emotions more confidently and teach children how to take actions to help support healthy management of their feelings over the longer term. Interested parents signed the consent and completed initial questionnaires online. Parents who were not interested in having their child participate in the EDPP were told that they would engage in non-sports-related recreational activities with other campers and camp staff (e.g., board games or similar) during the time set aside for the EDPP. During the first meeting of the EDPP, participating children were informed of the plan and goals of the program, and of their alternatives to participation. They were asked to sign assent forms and complete initial questionnaires.
Design
The EDPP was implemented in an open trial format. Specifically, all children whose parents signed consent for the program received the EDPP as described below. Although a randomized design using a control or comparison condition was desired by the investigatory team, this was not enacted in the resultant investigation due to resistance from camp administrators that indicated a strong desire for a consistent psychoeducational programming choice for all eligible campers and the administration’s belief that parents of campers would prefer a non-randomized design.
Prevention Program
The EDPP is a 15-session program that was developed as a downward extension of the UP and UP-Y. The program includes instruction and experiential activities related to adaptive coping skills applicable across a range of emotional experiences (e.g., fear, sadness, anger, happiness, surprise, etc.); as such, the prevention strategies are purposely presented to participants in an explicitly transdiagnostic manner that easily allows for discussion of varying levels of symptom intensity (see Ehrenreich-May & Bilek, in press for a discussion of the transdiagnostic features of Emotion Detectives). Participants were grouped by age level in EDPP sessions, at the encouragement of the camp’s leadership, to best accommodate the structure of the day camp; each age-based group met separately, for a total of four EDPP groups (age 7, 8, 9, and 10). Overall, EDPP participants met with group leaders for forty-five minutes per session, with sessions occurring twice weekly. Each age group had one designated leader that facilitated initial skill learning and maintained overall behavior management of the group. Several co-leaders, including both predoctoral students in clinical psychology and undergraduate volunteers assisted the primary leaders. As groups ranged in size from 18–21, an approximate 1:5 group facilitator to camper ratio was achieved. The inclusion of a single group leader as well as co-leaders facilitated both efficient uptake of overall concepts as well as personalized instruction during experiential activities.
The EDPP was initially developed as a downward extension of Unified Protocol for the Treatment of Emotional Disorders in Youth (UP-Y; Ehrenreich et al., 2008). The UP-Y is a modular treatment approach to anxiety and depression in adolescence, based on three theoretical principles that are believed to be critical change processes in treating a range of emotional disorders: 1) altering antecedent cognitive reappraisal, 2) the prevention of emotional avoidance and 3) modifying behavioral action tendencies (Allen, Ehrenreich & Barlow, 2005). These principles provide the framework for selection of a variety of cognitive behavioral and emotion regulation skills taught as part of the UP-Y (Trosper, Buzzella, Bennett, & Ehrenreich, 2009). Initial investigations of the UP-Y indicate that this approach, which also formats its treatment strategies in the context of emotions more generally, rather than any one disorder more specifically, demonstrates initial promise for the treatment of a wide array of anxiety and depressive disorders (Ehrenreich-May & Remmes, 2010; Trosper et al., 2009). In order to optimally implement the UP-Y’s core principles in a prevention context, the key components of the UP-Y were adapted and modified during the development of the EDPP in several important ways.
Antecedent cognitive reappraisal
Antecedent cognitive reappraisal refers to the process of anticipating cognitive distortions that one might engage in during an emotionally evocative situation and engaging in reappraisal of these distortions in the antecedent condition (Allen et al., 2005). Although practicing antecedent cognitive reappraisal can help prevent maladaptive responses to uncomfortable emotions, it may be especially difficult for children in a prevention program to comprehend and practice this skill. Given a lack of overt distress, children in a universal prevention program were anticipated to have difficulties generating personal examples of distressing emotional situations, which could be broken down into their component parts and analyzed for cognitive distortions. Thus, rather than rely on personal clinical examples of cognitive distortions, EDPP teaches what are referred to as “flexible thinking skills” by utilizing stimuli, whereby participants are taught and encouraged to see situations from multiple perspectives. Participants also learn restructuring skills and practice solving common problems facing young children in a systematic manner (e.g. how to disengage a bully). In this way, antecedent reappraisal is implemented in a highly relevant and applicable context for a prevention population, while still taught with enough specificity to be implemented in the context of more symptomatic presentations, should the need arise.
Prevention of emotional avoidance
Emotional avoidance refers to the effortful evasion of uncomfortable emotions and may be achieved through a variety of means including physical avoidance, untimely distraction or suppression. While avoidance results in immediate relief from the uncomfortable emotion, it may lead to increased distress and fear of the emotionally laden situation in the long run (Levitt, Brown, Orsillo & Barlow, 2004). The goal, therefore, of this segment of the program is to reverse the avoidance process by asking individuals to fully experience their uncomfortable emotions. The implementation of this technique has been associated with improvement in treatment for emotional disorders (e.g. Ellard, Fairholme, Boisseau, Farchione & Barlow, 2010). However, in a universal prevention context, children may lack experience with interfering levels of emotional avoidance. Thus, rather than having the children identify situations that they frequently avoid and altering that response, the prevention program focuses on learning how an emotion can be experienced or avoided. Special attention is paid to learning about distraction and suppression and when these strategies can become maladaptive. For example, the children are taught to engage in and to experience emotions rather than to avoid them. To practice emotional engagement, the children complete generalized emotion exposures, such as watching emotionally evocative film clips (e.g. a sad scene from an animated movie), and practice experiencing their emotional response as fully as possible. They are instructed to notice any emotions they might be experiencing, and not to judge them, but to experience them fully without distraction or suppression. In this way, the participants can experience the full range of uncomfortable emotions, regardless of clinical status.
Managing behavioral action tendencies
Modifying behavior action tendencies refers to increasing behavioral activation and experiencing emotional situations without engaging in avoidance, subtle or overt. Given that most participants in a universal prevention program do not have clinical levels of anxiety or depression, it is difficult to develop individualized hierarchies and exposure plans; thus, the UP-Y treatment principle that has the most potential for difficulty in adaptation to a prevention context is this behavioral component. As the EDPP was developed to be administered in a larger group setting, the feasibility of individualized exposure sessions was questionable. However, this third principle is regarded as a mechanism of change in treatment protocols for such symptoms, and may be essential in the prevention of emotional disorders as well (e.g. Barlow, 2002). As such, behavioral components were adapted and included in EDPP as much as possible. Adaptations included practicing graduated exposure with non-feared stimuli (such as plastic spiders). Participants also engaged in group exposures (e.g. telling jokes in front of small groups) as well as imaginal exposures (e.g. imagining being lost in an airport). The participants also practiced behavioral activation techniques, such as tracking their mood and activity levels, and engaging in brainstorming a list of pleasant activities. In this way, the EDPP offers a breadth of assignments that reflect common fears and group activities that reinforce approaching fear in a productive way across relevant stimuli.
To enhance understanding and retention of material, the goals of these core principles were broken down and organized into five progressive parts, referred to collectively as the CLUES skills. The CLUES skills are: Consider how I feel (introduces the prevention of emotional avoidance), Look at my thoughts (introduces antecedent cognitive reappraisal), Use detective questions (reinforces antecedent cognitive reappraisal), Experience my fears and feelings (introduces managing behavior action tendencies and reinforces prevention of emotional avoidance), Stay healthy and happy (in which all core strategies are reviewed and future coping plans are reviewed). For more information about the CLUES skills, see Table 1 and Ehrenreich-May & Bilek (in press).
Table 1.
Emotion Detectives Prevention Program Content
| Sessions | Associated Skill | Content |
|---|---|---|
| 1–5 | Consider How I Feel | Psychoeducation/Prevention of Emotional Avoidance |
| 6 | Look at my Thoughts | Antecedent Cognitive Reappraisal |
| 7–9 | Use Detective Questions | Antecedent Cognitive Reappraisal |
| 10–14 | Experience Fears and Feelings | Emotion Exposure/Behavior Activation |
| 15 | Staying Healthy and Happy | Relapse Prevention |
Developmental approach
The EDPP was developed as a downward adaptation of the UP-Y. As such, the skills taught in the EDTP were originally developed for an older audience (Ehrenreich et al., 2008). To ensure maximum uptake and retention of material, adaptations and developmentally appropriate explanations of relevant program skills were included. As the EDPP was offered as part of a recreational day camp, it was important that the children not only understand the material delivered, but also that they view it as a natural and enjoyable addition to their camp activities. Thus, the EDPP protocol was developed to be as accessible and engaging to a school age audience as possible. Often this required that complex treatment principles were taught through interactive activities and then reinforced though iterative practice. For example, children were encouraged to use creative reappraisal skills in a developmentally sensitive manner by viewing common optical illusions and discussing as a group what they see upon their first glance, and then upon a more critical second viewing. Additional discussions of ambiguous situations and critical thinking were then encouraged to extend the application to negative thoughts.
A developmentally sensitive approach was also taken to teaching children the rationale and function of behavior activation. Before the concept of behavior activation is introduced, each participant rated his mood on a zero to eight scale, where zero is equated with being very grouchy or “down in the dumps” and eight being “the happiest you have ever been”. Participants then listened to an upbeat song and are asked to move or dance for the duration. When the song ended, the participants rated their mood again. This “experiment” allowed the participants to engage in a camp-like activity, while simultaneously gaining firsthand experience with how behavior activation can work to bolster mood. In a similar manner, enjoyable, engaging and illustrative activities were incorporated throughout the EDPP and served to keep school-age participants as entertained as possible, while simultaneously allowing them to learn sophisticated cognitive behavioral skills at an age-appropriate level.
Parent participation
Optional parent sessions were offered twice during the course of the summer program. Flyers were sent home to parents to inform them of these informational sessions. Sessions included a description of the prevention program, a brief review of EDPP skills and a discussion of how these skills could best be reinforced outside of the camp environment. Parents were also given an opportunity to ask questions of the group leaders and raise any concerns that they might have.
Results
Initial Sample Statistics
Participant income and ethnicity were not collected or reported at the request of the recreational camp. However, participants were primarily residents of Coral Gables, Florida. In 2010, residents of the city of Coral Gables had a median yearly income of $83,530 (Nielsen Claritas, 2010). The ethnic composition of the city of Coral Gables in 2010 was 50.8% Hispanic, 40.83% White, Non-Hispanic, 3.2% African-American, 1.87 % Asian and 3.37% Other or Not Specified (Nielson Claritas, 2010). All participants in the current trial spoke English; degree of acculturation was not assessed. At pre-prevention, 22 members of the completer sample (total of 40 children) demonstrated elevated anxiety symptoms (55%) by child- or parent-report on scales of the SCARED. Fifteen children in this completer sample demonstrated elevated depressive symptoms (37%) by child- or parent-report on the CES-D.
Preliminary Analyses and Data Analytic Approach
Given the nature of summer camp attendance (e.g., due to planned vacations and variable schedules, some children attend for only a portion of the summer, while others attend for the entire summer), several participants attended the EDPP for only part of the time it was offered. Participant attendance ranged from attending one camp block (3–4 sessions) to all four camp blocks (15 sessions). Paired sample t-tests revealed that there were no significant differences between participants who only attended the first camp block (sessions 1 – 3) and those who attended more than one camp block (up to eight weeks) regarding pre-prevention parent or child report on the CES-D (parent: t(49) = .47, NS; child: t(54)= .07, NS), on the SCARED (parent: t(49)=.22, NS; child: t(66)=−.92, NS), or on emotion regulation questionnaires (CEMS: t(48)= −.93, NS), by either parent or child report. To ensure that at least a minimal dose of the EDPP was administered, individuals who completed fewer than one camp block were dropped from future analyses. Moreover, parent participation in optional EDPP sessions did not significantly predict any treatment outcomes. To assess changes from pre- to post-prevention, paired-samples t-tests were primarily utilized for symptom-based and emotion regulation measures from pre- to post-prevention. Descriptive analyses of satisfaction measures were also utilized for this investigation.
Symptom Measures
Results from the current study demonstrated moderate support for the hypothesis that the EDPP would be associated with reductions of emotional symptoms. Paired samples t-tests were conducted to compare parent and child report of symptoms prior to completing the EDPP to their report of symptoms after the child received the program. At pre-prevention, children reported high levels of total anxiety symptoms, averaging just above the cut-off (26) for elevated symptoms (M=26.7). Consistent with our hypothesis, by post-prevention, children reported significantly fewer symptoms of anxiety on the SCARED total scale (M=22.7, t(38)=2.11, p<.05, d=.26. However, parents reported no significant change in symptoms of anxiety on the SCARED (t(26)=1.58, NS). Additionally, there was no significant change in child or parent-reported depressive symptoms on the CES-D (t(28)= −.85, NS; t(26)= −1.25, NS). No differential outcomes on parent or child reported measures of depression or anxiety were found for individuals who met clinical cut-off criteria at T1.
Among those participants who attended more than one camp block, 12.5% attended two blocks, 14.5% attended three blocks, and 70% attended all four blocks. There was a trend toward a significant interaction between child report of anxiety symptoms and number of camp blocks attended (F(2,36)=3.15, p=.06). Specifically, children who attended four camp blocks reported significantly greater improvements in anxiety symptoms than those who completed only three camp blocks (t(36)=2.36, p=<.05, d=.92). No other significant dose effects were found by child or parent report.
Emotion Regulation
Results from the current study did not provide support for our hypothesis that the EDPP would be associated with improvements in child and parent reported emotion-focused coping and regulation skills. Parents reported no significant change in child coping, dysregulation or inhibition on the CEMS from pre- to post-prevention. Children reported no significant change in use of emotion regulation strategies from pre- to post-prevention (Reappraisal: t(39)=1.61, NS; Suppression: t(39)=.71, NS). Table 2 presents the means and standard deviations for symptom and emotion regulation measures at pre- and post-prevention.
Table 2.
Mean Scores on Symptom Measures
| Measure | Pre-Prevention | Post-Prevention |
|---|---|---|
| M (SD) | M (SD) | |
| CES-D-Parent | 8.41 (5.33) | 9.52 (5.18) |
| CES-D-Child | 14.10 (8.82) | 15.66 (11.01) |
| SCARED-Parent | 10.11 (7.39) | 8.93 (8.08) |
| SCARED-Child | 26.69 (14.92) | 22.74 (15.94) |
| CEMS dysregulation-Parent | 14.14 (4.36) | 13.86 (4.07) |
| CEMS coping-Parent | 23.00 (6.03) | 21.71 (5.44) |
| CEMS inhibition-Parent | 15.00 (4.59) | 14.40 (2.79) |
| ERQ-CA reappraisal-Child | 14.88 (3.19) | 13.93 (3.91) |
| ERQ-CA suppression-Child | 7.60 (3.13) | 7.23 (2.69) |
Note. SCARED= Screen for Child Anxiety Related Emotional Disorders. CES-D = Center for Epidemiological Studies – Depression Scale. CEMS = Children’s Emotion Management Scale. ERQ-CA = Emotion Regulation Questionnaire – Child and Adolescent.
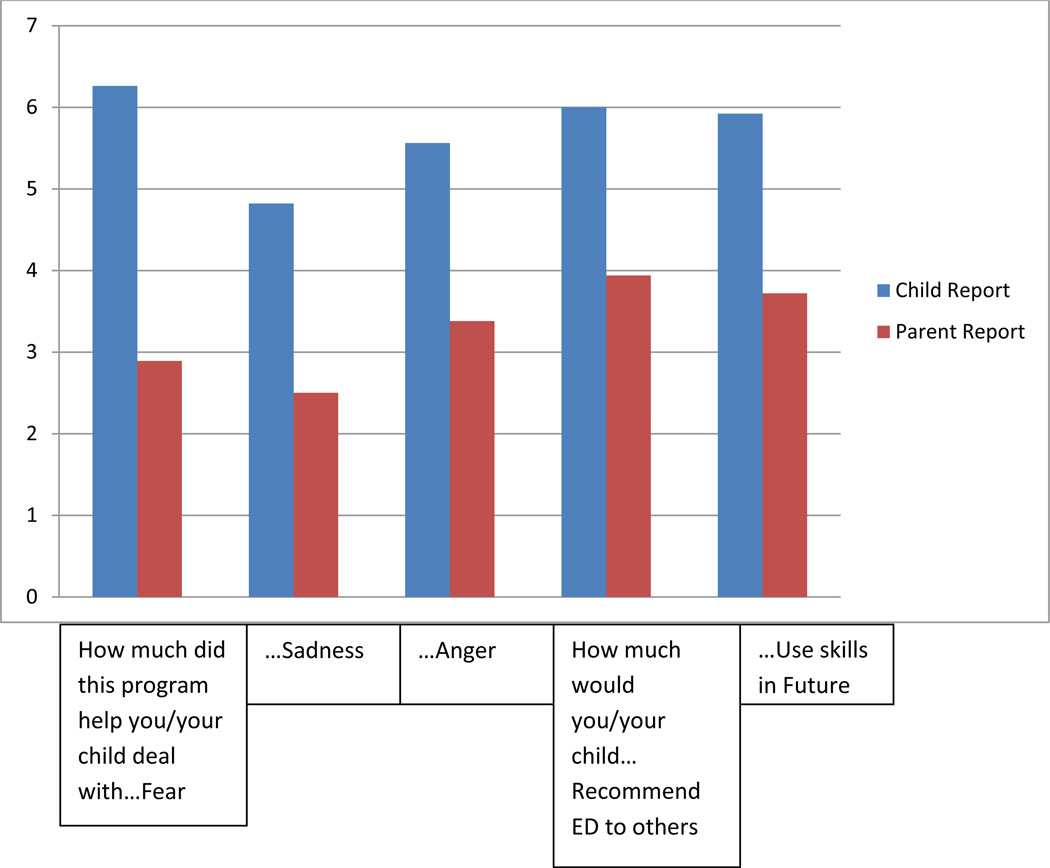
Satisfaction
Participant satisfaction data provided support for the hypothesis that the EDPP would achieve high acceptability with participants and their families. Children reported high levels of satisfaction with various aspects of the EDPP, including how much the participants believed the program helped the children deal with fear (Child Report M=6.3; Parent Report M= 2.9), anger (Child Report M=5.6; Parent Report M= 3.4), and sadness (Child Report M= 4.8; Parent Report M= 2.5). Parents reported being somewhat likely to recommend the program to a friend (M=3.94). Mean parent and child EDPP satisfaction scores are reported in Figure 2.
Figure 2.
Parent and Child repot of Treatment Satisfaction
Discussion
This initial open trial demonstrated promising results indicating the initial feasibility, acceptability and outcomes of the Emotion Detectives Prevention Program, as offered in a novel recreational camp setting. Children reported significant decreases in anxiety symptoms following the EDPP, although few other changes in coping, emotion regulation or depression symptoms were reported at the post-program evaluation point. Discrepancies between child and parent report, regarding the scope of such improvements, were notable. Additionally, participants reported moderate to high levels of treatment satisfaction and program acceptability.
As noted, children reported significant decreases in anxiety symptoms, from pre- to post-prevention. In the current trial, the effect size associated with this change was small. For comparison purposes, reported effect sizes for reductions in self-reported anxiety symptoms over the 12 weeks of the FRIENDS program generally range from .15 (Lock & Barrett, 2003) to .57 (Barrett & Turner, 2001). Although effect sizes for reduction in self-reported anxiety in the current trial were at the lower end of this spectrum, they were still within this range. While the FRIENDS trials do not provide an ideal comparison to the current prevention program, which assessed change in anxiety symptoms over a briefer course of 4–8 weeks using a different outcome measure, such data is suggestive that the reduction in anxiety symptoms in the current study is generally consistent with those results found by prevention in the FRIENDS trials (Lock & Barrett, 2003).
Although parents and children in the current trial of EDPP did not report any change in depressive symptoms from pre- to post-prevention time points, there is mixed body of research suggesting that a reduction in depressive symptoms associated with the FRIENDS prevention program may not emerge until later, often up to 12 months post-prevention (Lowry-Webster et al., 2001; Lock and Barrett, 2003). Unfortunately, such follow-up data was not available for the current investigation. Therefore, longer term effects of the EDPP on the prevention of both anxiety and depression symptoms remain in need of further study at this time. Furthermore, although the CES-D evidenced good reliability with this population, this measure is most often used with adults and adolescents and it is possible that it was not the most sensitive measure of depressive symptoms for this younger age range.
While the initial results of this trial are in some ways similar to results of the FRIENDS prevention program, results of the current investigation must be considered with some caution. First, the FRIENDS results have demonstrated that symptom reduction at post-prevention points is greater for individuals who participate in the FRIENDS program, as compared to control groups (Lowry-Webster et al., 2001). The current trial of EDPP did not offer a control comparison condition; consequently, any significant difference in symptoms found at post-prevention in the current EDPP trial may simply be due to the passage of time or a placebo effect arising from interaction with clinicians. As noted, a randomized trial was not acceptable to the camp’s administration for this initial trial. The successful conduct of an initial trial such as this with the camp may enable more flexibility in the future regarding this important design element, increasing the potential for understanding the efficacy of the prevention program more comprehensively.
With regard to emotion regulation, parents reported no significant changes in child coping, dysregulation or inhibition from pre- to post-prevention. Additionally, there were no significant changes reported regarding child use of reappraisal or suppression strategies. These results were generally contrary to our prediction that children would experience an improvement in emotion regulation strategies. However, the start of the EDPP (T1) also coincided with the beginning of summer vacation, while the end of the program (T2) coincided with the end of camp and with the beginning of a new school year. It is possible that the children in our sample may have reported better regulation abilities at the beginning of the summer term, simply because they were no longer experiencing some of the emotional stressors that characterize the school year (i.e. homework, exams, more rigid schedules, etc.). In contrast, the end of the summer may be a difficult time for students who are experiencing sadness about the end of camp and apprehension about the new school year, which may tax their coping abilities. Thus, children may display more negative coping when the emotional climate is more difficult and uncomfortable, regardless of their overall emotion regulation abilities (Compas, Connor-Smith, Saltzman, Thomsen & Wadsworth, 2001). This potential bias toward experiencing positive emotions at the beginning of the program and more negative emotions toward the end of the program might have masked true improvements in emotion regulation and/or depressive symptoms. Further research would need to evaluate the effect of the prevention program independent from naturally occurring environmental stressors, although this effort would likely prove difficult as implemented in a summer camp setting.
In addition to the potential confound of situational stressors, the lack of significant findings regarding emotion regulation may suggest that the coping skills taught in the EDPP could have been delivered with more specificity. There is a dearth of literature illuminating normative and adaptive emotion regulation skills and their fluctuations across child development (Cole, Martin & Dennis, 2004). Thus, many of the techniques taught in this program necessarily focus on general adaptive coping strategies, such as problem solving and reappraisal, rather than tailoring the instruction to deficits relevant to this specific age group. Emerging research from neurobiological and neuropsychological domains is beginning to examine these issues, and future revisions of the EDPP may include more directed instruction on how to best implement adaptive emotion regulation strategies in a developmentally sensitive manner (Izard et al., 2011).
Acceptability and Feasibility
Above and beyond the assessment of symptom and emotion regulation outcomes, one of the primary purposes of this open trial was to examine whether the delivery of a universal prevention program in a camp environment would be acceptable to participants. Initial results demonstrate that the child participants believed that the program was effective, fun and engaging. Children indicated that the program helped the participants deal with difficult emotions and that they had significantly higher levels of life satisfaction at the conclusion of EDPP as compared to before the program. As on all other questionnaires, parents were more conservative in their report of changes and impressions than were their children, a pattern that is frequently observed in non-clinical services research (e.g., Cantwell, Lewinsohn, Rohde & Seeley, 1997). However, despite their relatively lesser evaluations of the program, parents reported that they were somewhat likely to recommend the program to other families.
In addition to assessing EDPP acceptability, the current trial examined the feasibility of offering a prevention program in a novel context: a summer camp environment. Because there is no literature examining prevention programs offered in a camp context, it was unclear at the outset what, if any, barriers we would encounter during the implementation of the EDPP in this setting. In many ways this study was therefore exploratory in nature and driven by the goal of examining the feasibility of offering a universal prevention in this context, and documenting the advantages and barriers to research and to the EDPP as they were encountered.
Advantages
Offering the prevention program within a summer camp setting allowed for a large range of creativity that may have been more difficult to obtain in a typical school or after-school setting. Rather than arriving at our program after a long day at school, the child participants in this investigation attended our program as part of a fun and exciting day at camp. The EDPP activities were developed to take advantage of the spirit of camp, and participants reported enjoying the creative nature of the activities (e.g. tracing their bodies, having a dance party, etc.). The camp atmosphere also allowed for flexibility that might have not been afforded in an after-school setting. The summer camp took place on a large university campus, which provided access to a diverse community as well as to facilities that more closely mimic real-world settings versus a traditional classroom setting. Participants were able to practice exposures in a local coffee shop as easily as they could on athletic fields, providing maximum opportunity for generalizability of the skills that were presented. Thus, the creativity and flexibility of the EDPP was in large part facilitated by the implementation of the program within this particular recreational camp setting, and likely contributed to the high degree of satisfaction reported by the child participants.
Barriers
Although the recreational camp setting provided a number of advantages, there were also several barriers associated with the implementation of the EDPP within this context. Primarily, the program suffered from poor communication with parent participants. Unlike a school environment that typically fosters an ongoing relationship between parents and school personnel, camp is a voluntary activity lasting at most, three months, and does not usually include a strong parent component. This communication challenge was evident even before the trial began, as only 57% of the parents of eligible participants signed consent for their child. This figure is consistent with other camp-based trials that report participation rates as low as 18% (e.g., Wu et al., 2010). Such low participation rates may be a product of the recruitment method. Although parents in the current trial were mailed materials describing the EDPP, it is possible that many of them did not receive or read this information. Group leaders endeavored to recruit parents who may have missed this information as they dropped off their children on the first day of camp; however, several children were dropped off in carpools or by caretakers other than their legal guardians. Thus, our ability to recruit all of the eligible participants was limited. The difficulties communicating with and engaging parents continued throughout the trial. While the children had ongoing interactions with the group leaders, only a small number of their parents met Emotion Detectives personnel during the course of the investigation (on the first day of the program and during the optional parent sessions). Accordingly, parents had limited knowledge about the program’s goals, skills and assignments. This gap in communication between the program and the parents may have contributed to the more conservative reports of program impact and satisfaction indicated by the parents of the participants.
Insufficient parent contact may have also contributed the high rates of parent attrition that we experienced in the current trial (see Table 1). While it may be relevant and meaningful for program staff or school personnel to contact parents to complete post- and follow-up assessments, even months after a program has been completed, this same process may have less inherent relevancy when associated with a time-limited summer camp. Thus, future research should include a more significant parent component and more consistent information transfer between the camp and parents, in order to maximize parent involvement and potentially increase parent interest and participation in follow-up assessments.
In addition to struggling with parent communication and participation, we also experienced difficulty with some aspects of data collection within the camp setting. For example, as mentioned, we were not able to evaluate the EDPP using a comparison condition, which limited our ability to draw conclusions about the efficacy of the program. This, as well as the difficulties associated with collecting post-prevention and follow-up data, may be in part due to the novelty of providing the program within this camp setting. Since research in existing recreational settings is scarce, it is probable that parents and camp staff were not familiar with procedures of data collection or fearful of its implications, which may be better established within a school setting.
Future Directions
Upon initial investigation, a camp environment appears to offer an effective and acceptable context for disseminating prevention materials, at least to child participants. However, possibly because it is an environment where little research has been conducted, there may be barriers to communicating with parents and to evaluating a program in a setting such as this, which may lack a year-round infrastructure. Despite the barriers that may arise in such a setting, conducting such interventions within a camp environment allow for unique levels of creativity and flexibility. Thus, in order to capitalize upon these advantages of the EDPP, future research should investigate how best to prioritize the program among parents and within the camp setting.
In the current study the lack of parent involvement may have been as much related to parent’s knowledge about the program as it was related parent’s interest in engaging in the program. To improve program awareness, future research should engage in more systematic means of contacting parents prior to program onset, potentially through multiple mailings associated with the camp. To increase interest in the program, successful parent recruitment may also depend upon direct contact, either via phone or email, which can establish the importance of the program and assess as well as assuage any barriers to family participation (McKay et al., 2004). Other researchers have recommended offering monetary incentives to improve parent participation in research (Ingoldsby, 2010). While this could certainly improve research compliance in funded trials, this approach might be less feasible for camp administrators seeking to implement programs, if they are not taking part in funded research. Additionally, to maximize parent investment in the program, it may be critical to offer parent informational sessions on several occasional prior to the commencement of camp. To accommodate the parents’ busy schedules, it would be important to offer these sessions frequently and to keep them brief.
Furthermore, it may be critical for interested investigators to establish a relationship with the camp administration far in advance of the proposed trial to successfully accomplish a potentially more burdensome research design, including a randomized, controlled design. To enhance camp investment, it might also be vital to assess the camp’s goals and interests. Specifically, it is important to assess what, if anything, the proposed intervention can do to further not only the researchers’ goals, but also those of the camp. Although the camp administrators were excited to offer the EDPP as an educational opportunity within their larger camp, the EDPP was considered a stand-alone specialty without a high degree of integration with the camp at large. By furthering the goals not only of the investigation but also the camp, and by including camp personnel in the administration of the prevention (either during the intervention sessions, or through extra generalization activities throughout the day), we may be able to strengthen the camp’s investment in our program and thus strengthen our research design. This high level of integration may also provide an avenue for maximizing the generalizability of EDPP skills and potentially strengthen the outcomes associated with the program.
Finally, the EDPP model, which was tested via a universal approach in the current trial, might also be applied to more specific or at-risk population in the future. Although the current trial did demonstrate a significant difference in child reported improvements based on symptom severity at intake, targeting the intervention may increase the EDPP’s appeal to parents and therefore its overall impact. And while the EDPP could be offered to a targeted group within a larger summer camp atmosphere, the EDPP might be especially relevant if offered within a summer camp that specifically caters to at risk populations with a high incidence rate of anxiety and/or depression, such as children with medical diseases, or those with high-functioning autism spectrum disorders.
Despite the barriers associated with implementing prevention programming and research within the camp environment, summer treatment camps that cater to at risk populations have been met with a good deal of success (e.g. Wu et al., 2010; Walker, Barry & Bader, 2010). In addition to providing a therapeutic camp experience for children, these specialized settings likely offer the infrastructure to maximize parent involvement and provide opportunities for the generalizability of the adaptive coping and emotion-focused skills taught in the EDPP.
Overall, the current study demonstrates the initial effectiveness of a cognitive-behavioral prevention program delivered within a recreational camp setting. The EDPP was associated with a reduction in child reported symptoms of anxiety and demonstrated that a camp setting can provide opportunities for the creative, generalizable and convenient implementation of effective treatment skills. Additionally, the trial illuminated several barriers to implementation within this camp context. Although limited in some respects, together these results provide a rationale for the further development of prevention research in camp settings.
Acknowledgments
The authors would like to acknowledge the contributions of Krystyna Ahlers, Jessica Alvarez, Rhonda DuBord, Ashley Falcon, Sara Klaben, Ryan Landoll, Elizabeth Penela, Alexander Queen, Nicole Schoenherr, Gregory Simpson, Thomas Soria, Carolyn Snell, Tanya Tran and Rita Zeiden regarding the conduct of this investigation and Lindsay Stewart for her comments on a previous draft of this manuscript.
Contributor Information
Jill Ehrenreich-May, Department of Psychology, University of Miami.
Emily L. Bilek, Department of Psychology, University of Miami
References
- Albano A, Chorpita BF, Barlow DH. Childhood anxiety disorders. In: Mash EJ, Barkley RA, Mash EJ, Barkley RA, editors. Child psychopathology. 2nd ed. New York, NY US: Guilford Press; 2003. pp. 279–329. [Google Scholar]
- Allen LB, Ehrenreich JT, Barlow DH. A unified treatment for emotional disorders: Applications with adults and adolescents. Japanese Journal of Behavior Therapy. 2005;31:3–31. [Google Scholar]
- Barlow DH. Anxiety and its disorders: The nature and treatment of anxiety and panic. 2nd ed. New York: The Guilford Press; 2002. [Google Scholar]
- Barlow DH, Ellard KK, Fairholme CP, Farchione TJ, Boisseau CL, Allen LB, Ehrenreich-May J. The unified protocol for transdiagnostic treatment of emotional disorders, therapist guide. New York: Oxford University Press; 2010. [Google Scholar]
- Barrett PM, Pahl KM. School-Based Intervention: Examining a Universal Approach to Anxiety Management. Australian Journal of Guidance & Counselling. 2006;16(1):55–75. [Google Scholar]
- Barrett PM, Farrell LJ, Ollendick TH, Dadds M. Long-Term Outcomes of an Australian Universal Prevention Trial of Anxiety and Depression Symptoms in Children and Youth: An Evaluation of the Friends Program. Journal of Clinical Child and Adolescent Psychology. 2006;35(3):403–411. doi: 10.1207/s15374424jccp3503_5. [DOI] [PubMed] [Google Scholar]
- Barrett P, Turner C. Prevention of anxiety symptoms in primary school children: Preliminary results from a universal school-based trial. British Journal of Clinical Psychology. 2001;40(4):399–410. doi: 10.1348/014466501163887. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, Baugher M. Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED): a replication study. Journal of American Academy Child Adolescent Psychiatry. 1999;38:1230–1236. doi: 10.1097/00004583-199910000-00011. [DOI] [PubMed] [Google Scholar]
- Cantwell DP, Lewinsohn PM, Rohde P, Seeley JR. Correspondence between adolescent report and parent report of psychiatric diagnostic data. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36(5):610–619. doi: 10.1097/00004583-199705000-00011. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences (rev. ed.) Hillsdale, NJ England: Lawrence Erlbaum Associates, Inc.; 1977. Retrieved from EBSCOhost. [Google Scholar]
- Cole PM, Martin SE, Dennis TA. Emotion Regulation as a Scientific Construct: Methodological Challenges and Directions for Child Development Research. Child Development. 2004;75(2):317–333. doi: 10.1111/j.1467-8624.2004.00673.x. [DOI] [PubMed] [Google Scholar]
- Compas BE, Connor-Smith JK, Saltzman H, Thomsen AH, Wadsworth ME. Coping with stress during childhood and adolescence: Problems, progress, and potential in theory and research. Psychological Bulletin. 2001;127(1):87–127. [PubMed] [Google Scholar]
- Craske MG. Fear and anxiety in children and adolescents. Bulletin of the Menninger Clinic. 1997;61:A4–A36. [PubMed] [Google Scholar]
- Dadds MR, Spence S, Holland DE, Barrett PM, Laurens KR. Prevention and early intervention for anxiety disorders: A controlled trial. Journal of Consulting and Clinical Psychology. 1997;65:627–635. doi: 10.1037//0022-006x.65.4.627. [DOI] [PubMed] [Google Scholar]
- Durlak JA, Wells AM. Primary prevention mental health programs for children and adolescents: A meta-analytic review. American Journal of Community Psychology. 1997;25(2):115–152. doi: 10.1023/a:1024654026646. [DOI] [PubMed] [Google Scholar]
- Dynarski M, Moore M, Mullens J, Gleason P, James-Burdumy S, Rosenberg L, Masnfield W, Heaviside S, Levy D, Pistorino C, Silva T, Deke J. When Schools Stay Open Late: The National Evaluation of the 21st-Century Community Learning Centers Program; First Year Findings; 2003. Retrieved from EBSCOhost. [Google Scholar]
- Ehrenreich-May J, Bilek EL. Emotion Detectives Prevention Program. University of Miami; 2009. Unpublished treatment manual. [Google Scholar]
- Ehrenreich-May J, Bilek EL. The Development of a Transdiagnostic, Cognitive Behavioral Group Intervention for Childhood Anxiety Disorders and Co-Occurring Depression Symptoms. Cognitive and Behavioral Practice. (in press) [Google Scholar]
- Ehrenreich-May J, Remmes C. The Unified Protocol for the Treatment of Emotional Disorders in Youth: Preliminary outcomes from a randomized, clinical trial. In: Suveg C, editor. Emotion and psychopathology: Conceptual foundations and clinical applications; Presented at the annual meeting of the Association for Behavioral and Cognitive Therapies; San Francisco, CA. 2010. Nov, (Chair) [Google Scholar]
- Ehrenreich JT, Buzzella BA, Trosper SE, Bennett SM, Wright LA, Barlow DH. Unified protocol for the treatment of emotional disorders in youth. University of Miami and Boston University; 2008. Unpublished treatment manual. [Google Scholar]
- Ellard KK, Fairholme CP, Boisseau CL, Farchione TJ, Barlow DH. Unified protocol for the transdiagnostic treatment of emotional disorders: Protocol development and initial outcome data. Cognitive and Behavioral Practice. 2010;17(1):88–101. doi: 10.1016/j.cbpra.2009.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farrell LJ, Barrett PM. Prevention of Childhood Emotional Disorders: Reducing the burden of suffering associated with anxiety and depression. Child and Adolescent Mental Health. 2007;12(2):58–65. doi: 10.1111/j.1475-3588.2006.00430.x. [DOI] [PubMed] [Google Scholar]
- Gordon R. An operational classification of disease prevention. In: Steinberg J, Silverman M, editors. Preventing mental disorders: A research perspective. Department of Health and Human Services: National Institute of Mental Health; 1987. pp. 20–26. [Google Scholar]
- Ingoldsby EM. Review of interventions to improve family engagement and retention in parent and child mental health programs. Journal of Child and Family Studies. 2010;19(5):629–645. doi: 10.1007/s10826-009-9350-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Izard CE, Woodburn EM, Finlon KJ, Krauthamer-Ewing E, Grossman SR, Seidenfeld A. Emotion knowledge, emotion utilization, and emotion regulation. Emotion Review. 2011;3(1):44–52. [Google Scholar]
- Jellinek MS, Snyder JB. Depression and suicide in children and adolescents. Pediatric Review. 1998;19:255–264. doi: 10.1542/pir.19-8-255. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Greenberg . The Economic Burden of Anxiety and Stress Disorders. In: Davis KL, Charney D, Coyle JT, Nemeroff C, editors. Neuropsychopharmacology: The Fifth Generation of Progress. American College of Neuropsychopharmacology; 2002. [Google Scholar]
- Kessler RC, Anthony JC, Blazer DG, Bromet E, Eaton WW, Kendler K, Swartz M, Wittchen H-U, Zhao S. The US national comorbidity survey: Overview and future directions. Epidemiologia e Psichiatria Sociale. 1997;6(1):4–16. doi: 10.1017/s1121189x00008575. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of twelve-month DSM-IV disorders in the National Comorbidity Survey Replication (NCS-R) Archives of General Psychiatry. 2005;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Ruscio A, Shear K, Wittchen H. Epidemiology of anxiety disorders. In: Stein MB, Steckler T, Stein MB, Steckler T, editors. Behavioral neurobiology of anxiety and its treatment. New York, NY US: Springer Science + Business Media; 2010. pp. 21–35. Retrieved from EBSCOhost. [Google Scholar]
- Kessler RC, Zhao S, Blazer DG, Swartz M. Prevalence, correlates, and course of minor depression and major depression in the national comorbidity survey. Journal of Affective Disorders. 1997a;45(1–2):19–30. doi: 10.1016/s0165-0327(97)00056-6. [DOI] [PubMed] [Google Scholar]
- Kirschman K, Roberts MC, Shadlow JO, Pelley TJ. An evaluation of hope following a summer camp for inner-city youth. Child & Youth Care Forum. 2010;39(6):385–396. [Google Scholar]
- Levitt JT, Brown TA, Orsillo SM, Barlow DH. The effects of acceptance versus suppression of emotion on subjective and psychophysiological response to carbon dioxide challenge in patients with panic disorder. Behavior Therapy. 2004;35(4):747–766. [Google Scholar]
- Lock S, Barrett PM. A longitudinal study of developmental differences in universal preventive intervention for child anxiety. Behaviour Change. 2003;20:183–199. [Google Scholar]
- Lowry-Webster HM, Barrett PM, Dadds MR. A universal prevention trial of anxiety and depressive symptomatology in childhood: Preliminary data from an Australian study. Behaviour Change. 2001;18(1):36–50. [Google Scholar]
- MacDermott ST, Betts J, Gullone E, Allen SJ. Emotion regulation in childhood and adolescence: A revised version of the Emotion Regulation Questionnaire (ERQ-CA) (submitted for publication) [Google Scholar]
- McKay MM, Hibbert R, Hoagwood K, Rodriguez J, Murray L, Legerski J, Fernandez D. Integrating Evidence-Based Engagement Interventions Into 'Real World' Child Mental Health Settings. Brief Treatment and Crisis Intervention. 2004;4(2):177–186. [Google Scholar]
- Muris P, Merckelbach H, Mayer B, Prins E. How serious are common childhood fears? Behaviour Research and Therapy. 2000;38(3):217–228. doi: 10.1016/s0005-7967(98)00204-6. [DOI] [PubMed] [Google Scholar]
- Neil AL, Christensen H. Efficacy and effectiveness of school-based prevention and early intervention programs for anxiety. Clinical Psychology Review. 2009;29(3):208–215. doi: 10.1016/j.cpr.2009.01.002. [DOI] [PubMed] [Google Scholar]
- New Freedom Commission on Mental Health. Achieving the promise: Transforming mental health care in America. 2003 Retreived from www.mentalhealthcommission.gov.
- Owens J, Murphy CE. Effectiveness Research in the Context of School-Based Mental Health. Clinical Child and Family Psychology Review. 2004;7(4):195–209. doi: 10.1007/s10567-004-6085-x. [DOI] [PubMed] [Google Scholar]
- Pelham Wr, Hoza B. Intensive treatment: A summer treatment program for children with ADHD. In: Hibbs ED, Jensen PS, Hibbs ED, Jensen PS, editors. Psychosocial treatments for child and adolescent disorders: Empirically based strategies for clinical practice. Washington, DC US: American Psychological Association; 1996. pp. 311–340. [Google Scholar]
- Penza-Clyve S, Zeman J, Sim L. Mother and child report of asthmatic children’s emotional expressiveness. Presented at the annual meeting of the American Psychological Association; Boston, MA. 1999. [Google Scholar]
- Pini S, Cassano GB, Simonini E, Savino M, Russo A, Montgomery SA. Prevalence of anxiety disorders comorbidity in bipolar depression, unipolar depression and dysthymia. Journal of Affective Disorders. 1997;42:145–153. doi: 10.1016/s0165-0327(96)01405-x. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1(3):385–401. [Google Scholar]
- Rambaldo LR, Wilding LD, Goldman ML, McClure JM, Friedberg RD. School-based interventions for anxious and depressed children. In: VandeCreek L, Jackson TL, VandeCreek L, Jackson TL, editors. Innovations in clinical practice: A source book. Vol. 19. Sarasota, FL US: Professional Resource Press/Professional Resource Exchange; 2001. pp. 347–358. [Google Scholar]
- Rapee R. Perceived stigma and consumer satisfaction in school-based programs for anxiety and depression. Symposium presented at the annual meeting of the Anxiety Disorders of America Association; Baltimore, MD. 2009. [Google Scholar]
- Roberts RE, Andrews JA, Lewinsohn PM, Hops H. Assessment of depression in adolescents using the Center for Epidemiologic Studies Depression Scale. Psychological Assessment: A Journal of Consulting and Clinical Psychology. 1990;2(2):122–128. [Google Scholar]
- Santucci LC, Ehrenreich JT, Trosper SE, Bennett SM, Pincus DB. Development and preliminary evaluation of a one-week summer treatment program for separation anxiety disorder. Cognitive and Behavioral Practice. 2009;16:317–331. doi: 10.1016/j.cbpra.2008.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suveg C, Sood E, Comer J, Kendall PC. Changes in emotion regulation following cognitive-behavioral therapy for anxious youth. Journal of Clinical Child and Adolescent Psychology. 2009;38(3):390–401. doi: 10.1080/15374410902851721. [DOI] [PubMed] [Google Scholar]
- The City of Coral Gables, Demographic Data. Report of Nielsen Claritas, Inc. 2010 Retrieved from http://www.coralgables.com/CGWeb/documents/CG_DadeTbl_10_box.pdf. [Google Scholar]
- Trosper SE, Buzzella BA, Bennett SM, Ehrenreich JT. Emotion regulation in youth with emotional disorders: Implications for a unified treatment approach. Clinical Child and Family Psychology Review. 2009;12(3):234–254. doi: 10.1007/s10567-009-0043-6. [DOI] [PubMed] [Google Scholar]
- Walker A, Barry TD, Bader SH. Therapist and parent ratings of changes in adaptive social skills following a summer treatment camp for children with autism spectrum disorders: A preliminary study. Child & Youth Care Forum. 2010;39(5):305–322. [Google Scholar]
- Weissman MM, Sholomskas D, Potternger M, Prusoff BA, Locke BZ. Assessing depressive symptoms in five psychiatric populations: A validation study. American Journal of Epidemiology. 1977;106(3):203–214. doi: 10.1093/oxfordjournals.aje.a112455. [DOI] [PubMed] [Google Scholar]
- Whittal ML. Prevention of mental disorders. Cognitive and Behavioral Practice. 2008;15(1):1–2. [Google Scholar]
- Wittchen H, Nelson CB, Lachner GG. Prevalence of mental disorders and psychosocial impairments in adolescents and young adults. Psychological Medicine: A Journal of Research in Psychiatry and the Allied Sciences. 1998;28(1):109–126. doi: 10.1017/s0033291797005928. [DOI] [PubMed] [Google Scholar]
- Wittchen HU, Stein MB, Kessler RC. Social fears and social phobia in a community sample of adolescents and young adults: Prevalence, risk factors and comorbidity. Psychological Medicine. 1999;29:309–323. doi: 10.1017/s0033291798008174. [DOI] [PubMed] [Google Scholar]
- Wu Yelena P, Prout Kerry, Roberts Michael C, Parikshak Sangeeta, Amylon Michael D. "Assessing experiences of children who attended a camp for children with cancer and their siblings: A preliminary study.". [accessed June 10, 2011];Child & Youth Care Forum. 2011 40(no. 2):121–133. PsycINFO, EBSCOhost. [Google Scholar]
- Zeman J, Shipman K, Penza-Clyve S. Development and initial validation of the Children’s Sadness Management Scale. Journal of Nonverbal Behavior. 2001;25:187–205. [Google Scholar]