Abstract
Objective This study examined whether emotional processing (understanding emotions), self-control (regulation of thoughts, emotions, and behavior), and their interaction predicted HbA1c for adolescents with type 1 diabetes over and above diabetes-specific constructs. Methods Self-report measures of self-control, emotional processing, self-efficacy for diabetes management, diabetes-specific negative affect, and adherence, and HbA1c from medical records were obtained from 137 adolescents with type 1 diabetes (M age = 13.48 years). Results Emotional processing interacted with self-control to predict HbA1c, such that when adolescents had both low emotional processing and low self-control, HbA1c was poorest. Also, both high emotional processing and self-control buffered negative effects of low capacity in the other in relation to HbA1c. The interaction of emotional processing × self-control predicted HbA1c over diabetes-specific self-efficacy, negative affect, and adherence. Conclusions These findings suggest the importance of emotional processing and self-control for health outcomes in adolescents with diabetes.
Keywords: adolescence, diabetes management, emotional processing, self-control, self-regulation
For those with type 1 diabetes, adolescence, compared with middle childhood and adulthood, is marked by struggles to maintain sufficient metabolic control (Silverstein et al., 2005). Diabetes management requires self-control, defined as the regulation and modulation of thoughts, emotions, and behaviors (Finkenauer, Engels, & Baumeister, 2005). However, adolescents lack the self-control maturity of adults (Steinberg, 2010). Furthermore, emotion intensity and reactivity increases during adolescence; more effective processing of this emotion (i.e., acknowledging, understanding, and accepting emotion) is related to decreased impulsive behavior and distress, and improved social interaction (Cole, Martin, & Dennis, 2004; Stanton, Parsa, & Austenfeld, 2002; Steinberg, 2010). Diabetes management requires both effective self-control and emotional processing for completion of adherence behaviors (e.g., checking blood glucose even when feeling angry at your parents for reminding you to do so). Although the importance of self-control of emotions, thoughts, and behaviors is beginning to be studied in the pediatric literature (Tan & Holub, 2011), the relation of self-control and emotional processing to health outcomes in adolescents with type 1 diabetes has not been studied.
Self-control and emotional processing interact in predicting cognitive, emotional, and behavioral outcomes, such as effective coping strategies, mood, and impulsive behaviors (Dennis, 2010). Self-control and emotional processing are distinct constructs, with self-control involving regulation of emotion (e.g., reappraising anger in response to your parents reminding you to check blood glucose); while the latter involves understanding and acceptance of emotion (e.g., reappraising that you are angry after your parent gives the reminder). Skill in each is related to increased adaptation and positive psychosocial functioning (Cole et al., 2004; Tangney, Baumeister, & Boone, 2004).
Research indicates that the combined influence of emotional processing and self-control needs to be examined to understand cognitive, emotional, and behavioral outcomes in children and adolescents (Dennis, 2010; Gray, 2004). Appropriate emotional processing can facilitate self-control; just as ineffective emotional processing may exacerbate negative outcomes related to poor self-control (Austenfeld & Stanton, 2004; Lamm & Lewis, 2010). For example, in a sample of healthy adolescents, failure to process emotion due to disengagement and limited self-control capacity combined to predict increased depressive symptoms and problem behavior in adolescents (Silk, Steinberg, & Morris, 2003). Furthermore, neuropsychological studies in healthy children have found that increased brain activity related to emotional processing contexts was differentially associated with better psychosocial outcomes and this was enhanced by self-control capacity (Dennis & Hajcak, 2009). Due to the high self-control demands of diabetes management and increased emotion lability experienced during adolescence, we hypothesized that both self-control and emotional processing would be important for metabolic control. More specifically, we predicted that adolescents low in both would have the worst metabolic control and those high in either might be especially advantaged.
The interaction of emotional processing and self-control has yet to be examined in research in adolescents with type 1 diabetes. However, constructs related to self-control and emotional processing are linked to health behaviors and health outcomes (i.e., HbA1c) in adolescents with type 1 diabetes. Self-control and emotional processing are related to lower general externalizing and internalizing symptoms, academic performance, and autonomy (Duckworth & Seligman, 2005; Stanton et al., 2002; Tangney et al., 2004), which in turn have been associated with diabetes health outcomes (Berg et al., 2011; Horton, Berg, Butner, & Wiebe, 2009). Also, in children and adolescents with type 1 diabetes, emotion expression (e.g., alexithymia, affect, active coping) is related to adherence and metabolic control (Fortenberry et al., 2009; Housiaux, Luminet, Broeck, & Dorchy, 2010; Luyckx, Seiffge-Krenke, & Hampson, 2010). Research with other related health behaviors (e.g., regulating eating behaviors, exercising, alcohol consumption) indicates that multiple facets of self-control and emotional processing each contribute to impulse control (Hofmann, Friese, & Roefs, 2009; Kashdan, Ferssizidis, Collins, & Muraven, 2010). More specific to self-control and diabetes management, initial research indicates that self-control is related to both adherence and metabolic control (Hughes, Berg, & Wiebe, 2010), and that adolescents who show rapidly increasing HbA1c across adolescence evidence poorer self-control (King et al., in press). Thus, we expected that emotional processing and self-control would be important in understanding disease management in adolescents with type 1 diabetes.
As self-control and emotional processing have conceptual overlap with existing diabetes-specific constructs that also relate to metabolic control, we examined the utility of self-control, emotional processing, and their interaction above and beyond self-efficacy for diabetes management, diabetes-specific negative affect, and adherence. These diabetes-specific constructs were selected because each represents a component of self-control involving cognition, emotion, and behavior. Relevant to control of cognition, self-efficacy for diabetes management (i.e., belief in one's ability to manage diabetes) has consistently been related to better metabolic control (Berg et al., 2011; Iannotti et al., 2006). With respect to control of emotion, diabetes-specific negative affect (i.e., negative emotion experienced in relation to diabetes; Moss-Morris et al., 2002) is related to decreased adherence, daily blood glucose testing, and worse metabolic control (Fortenberry et al., 2009). Finally, adherence involves the ability to complete behaviors and tasks required for type 1 diabetes management (La Greca et al., 1995) and is consistently associated with better metabolic control (Hood, Peterson, Rohan, & Drotar, 2009). By comparing self-control, emotional processing, and their interaction with these well-established diabetes-specific constructs, we provide a conservative test of the utility of examining self-control and emotional processing.
The primary goal of the study was to examine whether emotional processing, self-control, and their interaction predicted metabolic control for adolescents with type 1 diabetes, and whether these constructs predicted metabolic control above and beyond diabetes-specific constructs. First, it was hypothesized that emotional processing would interact with self-control to predict metabolic control such that adolescents low in both would have the worst metabolic control and those high in either might be especially advantaged (i.e., each construct would compensate for low amounts of the other). We also hypothesized that self-control, emotional processing, and their interaction would predict metabolic control above and beyond self-efficacy for diabetes management, diabetes-specific negative affect, and adherence.
Methods
Participants
The University Institutional Review Board approved the larger project from which this study was conducted (n = 252). The larger longitudinal project followed adolescents with type 1 diabetes over a 3-year period to explore developmental changes in adolescent and parent relationships related to diabetes management (Berg et al., 2008). Parents gave written informed consent and adolescents gave written assent, both were compensated for participation in the study. Initial eligibility criteria included adolescent ages between 10 and 14 years, diabetes diagnosis for more than 1 year (M = 5.43 years), and parent and child ability to read and write either English or Spanish. Families were recruited from both a university/private partnership clinic (76%) and a community-based private practice (24%) that each followed similar treatment regimens and clinic procedures. Participants from each did not differ on metabolic control, age, sex, or ethnicity, but the university clinic had proportionately more participants using multiple daily injections (MDI; 54% vs. 24%; Wiebe et al., 2010). Approximately half (63%) of the adolescents were on an insulin pump, with the remainder prescribed MDI. Only adolescent report data are used in this study; however, mothers reported that physicians recommended an average of 3.98 insulin injections, for those adolescents on MDI (SD = 1.65, range = 1–8 injections), and 5.58 blood glucose checks per day (SD = 1.65, range = 1–11 checks). Families were largely Caucasian (95%) and middle class, with approximately half (53%) reporting household incomes averaging $50,000 or more annually. The sample in the present paper came from the third wave (1 year into the study) of this larger project where 194 of the original 252 individuals participated. Those participants at Time 3 were not different in child gender or age from those that did not participate at Time 3, but did have lower glycosolated hemoglobin percentages at Time 1 (HbA1c M = 8.30) than those not completing Time 3 (M = 10.26), t(247) = 3.73, p < .001.
Participants in this study, who completed all necessary measures at Time 3, included 137 adolescents (M age = 13.48 years, SD = 1.51, 54% females). At Time 3, the first 57 participants did not complete the emotional processing measure (as it was added after Time 3 data collection had begun), and the adolescents in this study did not differ from the other 57 participants at Time 3 in any key variables including, gender, age, or HbA1c (p’s > .05).
Procedure
Participants were recruited from diabetes clinics by research staff and individually completed three of the study measures (self-control, diabetes-specific negative affect, and self-efficacy for diabetes management) at home, just prior to the lab visit, while two of the study measures (emotional processing and adherence) were completed at the lab visit. For questionnaires completed at home, adolescents were instructed to complete these without their parents. A cover sheet reiterated the importance of completing questionnaires separately and asked that questions be directed to the investigators rather than family members.
Measures
Self-control
Adolescents completed a self-control scale that consisted of 11-items tapping aspects of the ability to regulate emotions, behaviors, and impulses (Finkenauer et al., 2005). The scale is a shortened version of a 36-item scale created by Tangney, Baumeister, and Boone (2004). Adolescents rated statements about self-control (e.g., “I wish I had more self-discipline”) on a 5-point scale (1 = Not at all like me to 5 = Very much like me). Finkenauer et al. (2005) reported adequate reliability (α = .67); in the present study reliability was α = .73.
Emotional Processing
The Emotional Processing subscale of the Emotional Approach Coping Scale (Stanton, Kirk, Cameron, & Danoff-Burg, 2000) measured the degree to which one actively attempts to understand, acknowledge, and accept one's emotions (i.e., “I explore my feelings to really understand them”). Four items were rated on a 5-point scale (1 = Never to 5 = Always). The measure has been used with adolescents (Diamond & Fagundes, 2008) and in the present study reliability was α = .70.
Self-Efficacy for Diabetes Management
The Self-Efficacy for Diabetes Management Scale (Iannotti et al., 2006) assessed adolescents’ perceptions of their competence and resourcefulness in being able to manage diabetes across 10 problematic situations (e.g., “How sure are you that you can manage your diabetes even when you feel overwhelmed?”). Adolescents rated items on a 10-point scale (1 = Not at all sure to 10 = Completely sure). Iannotti et al. (2006) reported high reliability (α = .90); in the present study α = .90.
Diabetes-Specific Negative effect
Negative affect linked to diabetes was measured with the Negative Consequences and Emotional Representation scale from the Revised Illness Perceptions Questionnaire (Moss-Morris et al., 2002). This six-item scale measured adolescents’ worries and negative emotions about diabetes (e.g., “When I think about my diabetes I get upset”). Adolescents rated items on a 5-point scale (1 = Strongly disagree to 5 = Strongly agree. Moss-Morris et al. (2002) reported good reliability (α > .84); in the present study α = .89.
Adherence
A 16-item Self Care Inventory (La Greca et al., 1995) was used to assess adherence to the diabetes regimen over the preceding month (1 = never to 5 = always did this as recommended without fail). Items reflected current standards of diabetes care around blood glucose testing, insulin management, diet, and exercise. Reliability in this study was α = .83.
Metabolic Control
Metabolic control using glycosolated hemoglobin percentages (HbA1c) was obtained from medical records. HbA1c provides information on average blood glucose levels over the preceding 3 or 4 months. Lower HbA1c levels reflect better metabolic control. At all clinic sites, HbA1c was obtained using the Bayer DCA2000 by clinic staff. Participant authorization provided access to adolescents’ medical records to obtain HbA1c and other illness information (e.g., duration of diabetes, pump vs. non-pump treatment).
Preliminary Analyses
All study variables were examined graphically and statistically for outliers and normality. No outliers were found and each variable, except for metabolic control (skewness = 1.53), had a sufficiently normal distribution. Metabolic control was not transformed to correct skew and kurtosis, as HbA1c percentages are not expected to produce a completely normal distribution in a sample of adolescents with type 1 diabetes. For participants missing less than 20% of the items, missing data were replaced with the mean of the sample. Overall, less than 5% of the participants were missing data in this study's sample, so no further action was taken.
Analyses were also conducted to determine needed covariates in the main analyses; potential covariates considered included those that were commonly associated with key study variables (e.g., income, age, insulin pump use, time since diagnosis). Household income was not correlated with key study variables and was not controlled for in further analyses. Pump status (i.e., dichotomously coded as uses a pump or not) was correlated with metabolic control and controlled for in analyses. Length of diagnosis was also controlled for as management and metabolic control decline with longer illness duration (Wiebe et al., 2005). The effects of age and gender were analyzed through regression in separate three-way interactions with self-control and emotional processing, and two-way interactions with diabetes management self-competence, diabetes-specific negative affect, and adherence predicting metabolic control. For both age and gender, neither the three-way interactions nor the two-way interactions including age and gender were significant for any of the variables.
Our analysis plan included conducting Pearson correlations to examine relations among study variables. Next, we conducted multiple hierarchical linear regressions to examine the relation of the interaction of self-control and emotional processing with metabolic control and to assess the utility of the interaction above and beyond the diabetes-specific constructs.
Results
Correlations among study variables revealed that higher self-control, emotional processing, self-efficacy for diabetes management, and adherence and lower diabetes-specific negative affect were each significantly correlated with lower HbA1c as expected (Table I). Higher self-control was associated with higher self-efficacy, lower negative affect, and higher adherence. Supporting our conceptualization of emotional processing as distinct from self-control, emotional processing was not correlated with self-control.
Table I.
Means, Standard Deviations, and Correlations of Key Study Variables
| M (SD) | 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|---|
| 1. HbA1c | 8.60 (1.75) | ||||||
| 2. Self-control | 3.51 (0.60) | −.22** | |||||
| 3. Emotional processing | 11.81 (3.02) | −.17* | .01 | ||||
| 4. Self-efficacy for diabetes management | 6.90 (1.78) | −.28** | .41** | .29** | |||
| 5. Diabetes-specific negative affect | 2.47 (0.92) | .21** | −.37** | −.10 | −.36** | ||
| 6. Adherence | 3.91 (0.57) | −.25** | .38** | .23** | .56** | −.24** |
*p < .05. **p < .01.
Emotional Processing and Self-Control Predicting Metabolic Control
Hierarchical regression was used to examine the interaction of self-control and emotional processing on metabolic control. Covariates (see above) were entered on Step 1, self-control and emotional processing, centered around their mean (Aiken & West, 1991), were entered on Step 2, and the interaction of self-control and emotional processing was entered on Step 3.
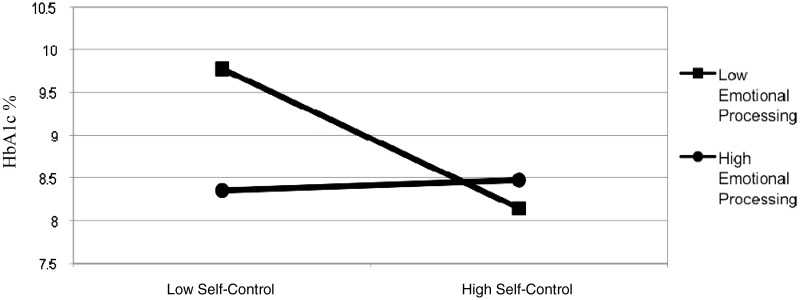
At Step 1, pump status was associated with lower HbA1c. At Step 2, higher self-control significantly predicted lower metabolic control, whereas emotional processing did not predict metabolic control (see top of Table II). Step 2 accounted for a significant change in variance (ΔR2 = .07). Finally at Step 3, the interaction of self-control and emotional processing significantly predicted metabolic control, accounting for a significant increase in variance (ΔR2 = .06). The full model accounted for 22% of the variance in HbA1c (Table II). We plotted the interaction for emotional processing at 1 SD above the mean and at 1 SD below the mean (Figure 1). Through simple slopes testing (Preacher, Curran, & Bauer, 2006), it was determined that the slope was significant for adolescents with low emotional processing, slope = −1.35, t = −4.08, p < .001, but not for adolescents with high emotional processing, slope = .098, t = 0.27, p = .79. Thus, high levels of emotional processing compensated for the detrimental effects of low self-control on metabolic control, with the poorest metabolic control occurring when emotional processing and self-control were both low.
Table II.
Hierarchical Regressions of the Interaction of Self-Control and Emotional Processing and Diabetes-Specific Resources Predicting HbA1c
| Model | Step | Variable(s) | R2 | ΔR2 | F | B(SE) | β | t | 95% CI |
|---|---|---|---|---|---|---|---|---|---|
| Emotional processing and self-control | 1 | .09 | 6.10** | ||||||
| Pump status | –0.84* (0.38) | –.20 | 2.00 | (−0.001 to 0.21) | |||||
| Length since diagnosis | 0.10 (0.06) | .16 | –2.58 | (−1.48 to −0.19) | |||||
| 2 | .16 | .07** | 6.13** | ||||||
| Self-control (SC) | –0.63* (0.26) | –.19 | –2.42 | (−1.14 to −0.11) | |||||
| Emotional processing (EP) | –0.091 (0.05) | –.14 | –1.73 | (−0.20 to 0.01) | |||||
| 3 | .22 | .06** | 7.07** | ||||||
| SC × EP | 0.24** (0.08) | .24 | 3.04 | (0.08 to 0.40) | |||||
| SC × EP utility versus self-efficacy for diabetes management | 1 | .09 | 6.10** | ||||||
| Pump status | −0.81* (0.32) | −.20 | 2.16 | (0.01 to 0.21) | |||||
| Length since diagnosis | 0.11* (0.05) | .17 | −2.50 | (−1.45 to −0.17) | |||||
| 2 | .16 | .08** | 8.29*** | ||||||
| Self-efficacy for diabetes management | −0.18 (0.10) | −.16 | −1.80 | (−0.39 to 0.02) | |||||
| 3 | .24 | .08** | 6.54** | ||||||
| SC | −0.41 (0.28) | −.13 | −1.46 | (−0.97 to 0.15) | |||||
| EP | −0.06 (0.06) | −.09 | −1.09 | (−0.17 to 0.05) | |||||
| SC × EP | 0.23** (0.08) | .23 | 2.92 | (0.07 to .38) | |||||
| SC × EP utility versus diabetes-specific negative affect | 1 | .09 | 6.10** | ||||||
| Pump status | −0.79* (0.33) | −.19 | 2.07 | (0.005 to 0.21) | |||||
| Length since diagnosis | 0.11* (0.05) | .17 | −2.43 | (−1.44 to −0.15) | |||||
| 2 | .14 | .05** | 6.80** | ||||||
| Diabetes-specific Negative Affect | 0.29 (0.19) | .13 | 1.51 | (−0.09 to 0.67) | |||||
| 3 | .24 | .10** | 6.33** | ||||||
| SC | −0.44 (0.29) | −.14 | −1.52 | (−1.00 to 0.13) | |||||
| EP | −0.09 (0.05) | −.13 | −1.60 | (−0.20 to 0.02) | |||||
| SC × EP | 0.24** (0.08) | .24 | 3.00 | (0.08 to 0.40) | |||||
| SC × EP utility versus adherence | 1 | .09 | 6.10** | ||||||
| Pump status | −0.75 (0.33) | −.18 | 1.93 | (−0.003 to 0.20) | |||||
| Length since diagnosis | 0.10 (0.05) | .15 | −2.30 | (−1.40 to −0.10) | |||||
| 2 | .13 | .05** | 6.51** | ||||||
| Adherence | −0.36 (0.29) | −.11 | −1.25 | (−0.92 to 0.21) | |||||
| 3 | .23 | .10** | 6.28** | ||||||
| SC | −0.55* (0.27) | −.17 | −2.02 | (−1.08 to −.01) | |||||
| EP | −0.07 (0.06) | −.11 | −1.35 | (−0.18 to 0.04) | |||||
| SC × EP | 0.24** (0.08) | .24 | 3.00 | (0.08 to 0.39) |
Note. All B(SE), β, t, and CI are from Block 3 of each regression. Significant effects are bold.
*p < .05, **p < .01.
Figure 1.
Simple slopes of the interaction of self-control and emotional processing predicting HbA1c at 1 SD below the mean and at 1 SD above the mean of emotional processing.
Consistent with our hypothesis, these results indicate that the interaction of self-control and emotional processing was a significant predictor of metabolic control, and that low emotional processing combined with low self-control was especially detrimental for adolescents.
Emotional Processing, Self-Control and Diabetes-Specific Resources in Predicting Metabolic Control
To assess whether the interaction of self-control and emotional processing predicted HbA1c over and above diabetes-specific constructs, we examined the interaction and the diabetes-specific constructs each in separate regressions predicting metabolic control. Three analogous hierarchical regressions were run, with covariates entered on Step 1, and a diabetes-specific construct, self-efficacy for diabetes management, diabetes-specific negative affect, or adherence on Step 2, and self-control and emotional processing, centered around their mean (Aiken & West, 1991), and the interaction of self-control and emotional processing on Step 3.
In each regression, the interaction of self-control and emotional processing predicted unique variance in metabolic control above each diabetes-specific construct, and each full model predicted a significant amount of variance in metabolic control (Table II). At Step 1, pump status was associated with lower HbA1c. At Step 2, each diabetes-specific construct significantly predicted metabolic control. Step 2 accounted for a significant change in variance (regression with self-efficacy for diabetes management ΔR2 = .08; negative affect ΔR2 = .05; adherence ΔR2 = .05). Finally, at Step 3, the interaction of self-control and emotional processing significantly predicted metabolic control, while the diabetes-specific variables did not, accounting for a significant change in variance (regression with self-efficacy for diabetes managements ΔR2 = .08; negative affect ΔR2 = .10; adherence ΔR2 = .10). The full model with self-efficacy for diabetes management accounted for 24% of the variance in HbA1c, model with negative affect 24% of the variance in HbA1c, and model with adherence 23% of the variance in HbA1c (Table II). Standardized β values and R2 change values from these regressions indicated that the interaction of self-control and emotional processing was a unique predictor of metabolic control. In fact, diabetes-specific constructs did not predict HbA1c when self-control and emotional processing were included in the analyses, despite their zero correlations with HbA1c.
In sum, these results indicate that, consistent with our hypotheses, the interaction of emotional processing and self-control was unique and particularly useful, above and beyond diabetes-specific constructs, in predicting metabolic control in adolescents with type 1 diabetes.
Discussion
These results highlight how low emotional processing and self-control may be particularly detrimental, while high capacity in either may compensate for deficits in the other related to HbA1c. Our data suggest that an adolescent with low emotional processing combined with low self-control will likely struggle to manage metabolic control and be at risk for poor diabetes outcomes. In contrast, adolescents with low self-control but high emotional processing might use their greater understanding of emotions to offset low self-control (e.g., acknowledging anger at parents after being reminded to check may reduce anger through its acknowledgment, offsetting the need for limited self-control resources). Conversely, adolescents with high self-control seem able to offset their poorer emotional understanding, perhaps through greater regulation of thoughts, cognition, or behavior (e.g., having the self-discipline to check blood sugar, which avoids parents reminding and the subsequent anger this could produce). These findings elucidate the importance of both emotional processing and self-control for adolescents with type 1 diabetes.
Our finding that emotional processing combined with self-control uniquely predicted HbA1c over and above diabetes-specific constructs argues for the importance of examining general abilities, like self-control and emotional processing in adolescents with type 1 diabetes. The fact that a measure of the interaction of emotional processing and self-control predicted over and above conceptually overlapping diabetes-specific measures (i.e., self-efficacy for diabetes management, diabetes-specific negative affect, and adherence) is a quite stringent test of the interaction's predictive utility. These results suggest that emotional processing, self-control, and their combination tap an important adolescent regulation skill for HbA1c that is not currently tapped by commonly used measures of diabetes regulation.
Future research should continue to explore how understanding emotional processing and self-control can help explain diabetes-specific behaviors and health outcomes. Emotional processing and self-control develop both as separate and as integrated capacities influencing health across the lifetime (Moffitt et al., 2011). During adolescence there are increased social and emotional influences (e.g., greater and more labile activation of emotion, differential dopamine signaling to social rewards) on maturing emotion and self-control capacities, which are still developing biological inter-connectivity (Steinberg, 2008; Yurgelun-Todd, 2007). Thus, self-control and emotional processing and their interaction are likely important in explaining adolescent judgment and decision making, risk-taking behavior, mood, and coping skills, all related to health behavior (Cole et al., 2004; Farrell, Hains, Davies, Smith, & Parton, 2004; Steinberg, 2008). Importantly, the integration or lack thereof, of emotional processing and self-control may be involved in how adolescents manage social and emotional events that indirectly and directly influence diabetes care. Our findings indicated that among young adolescents with type 1 diabetes, when a deficit exists in either self-control or emotional processing, these two maturing capabilities might compensate for each other. However, adolescents who were low in both showed high risk for poor metabolic control, perhaps signaling adolescents experiencing broader or more serious deficits in regulation capabilities.
Future research is needed to more fully understand what comprises self-control and emotional processing. Many different constructs are studied in self-control and emotion research (e.g., cognitive control, effortful control, emotional regulation, and coping; Austenfeld & Stanton, 2004; Gray, 2004; Posner & Rothbart, 2000), and understanding which of these is most important in understanding metabolic control will be a fruitful area for research. Furthermore, research on the importance of disease specific measures (Nansel, Weisberg-Benchell, Wysocki, Laffel, & Anderson, 2008) suggests that future research will also benefit from measuring diabetes-specific emotional processing (e.g., the adolescent's awareness, understanding, and acceptance of emotions around diabetes), self-control (e.g., regulating and modulating diabetes-related thoughts, emotions, and behaviors), and their interaction.
Intervention research would also benefit from exploring if and how changes in these capacities mediate changes in diabetes-specific adherence behaviors and outcomes. Our findings suggest that assessing both adolescent self-control and emotional processing capacity will be important when developing and determining appropriate interventions. Addressing emotional processing is particularly important as research suggests that interventions targeted at increasing adolescent self-control often have limited effects due to the developmental and biological constraints on self-control during adolescence (Blair & Diamond, 2008). Adolescents low in self-control may benefit from interventions that serve to increase their skills in emotional processing, such as acceptance and commitment therapy (ACT), which has a strong focus on mindfulness and acceptance of emotion (Hayes, Luoma, Bond, Masuda, & Lillis, 2006). Interventions for adolescents with type 1 diabetes, such as Grey's (2000) coping skills training, Wysocki's (2008) behavioral family systems therapy, and Ellis’ (2005) multisystemic therapy, address social and emotional coping skills that likely support more effective emotional processing. Although ACT-based interventions have yet to be studied in adolescents with type 1 diabetes, findings from ACT interventions in other pediatric (e.g., chronic pain) and adolescent (e.g., depression, anxiety) populations suggest that ACT is related to increases in self-regulated emotion, thought, and behavior along with other positive psychosocial outcomes (Coyne, McHugh, & Martinez, 2011). During time-limited clinic visits, diabetes care providers might also support adolescents’ processing of emotion through modeling identification and discussion of emotions, as well as emotion, thought, and behavior relations in the context diabetes management. Clinical efforts at improving metabolic control in adolescents will benefit from consideration of emotional processing and self-control and their combined influence on health behaviors.
Our findings should be considered in the context of some limitations. This sample was comprised of primarily Caucasian participants; cultural differences seen in the development of self-regulatory capacity (Posner & Rothbart, 2000) should be considered in generalizing these findings. Additionally, this study used a cross-sectional design with brief, self-regulatory measures composed of only adolescent self-report, which had sufficient, but not strong internal consistency. The inclusion of parent and teacher report measures of adolescent self-regulation, as well as established behavioral measures such as neurocognitive tests that tap facets of self-regulation in adolescents with type 1 diabetes are needed. The results should be considered in the context of the truncated age range of participants (ages of 11–15 years) and a sample less likely to include adolescents with poorer metabolic control.
In summary, high emotional processing or self-control was related to positive health outcomes, while poor capacity in both was related to the worst health outcomes, over and above conceptually overlapping diabetes-specific constructs. These results suggest the inclusion of emotional processing and self-control will be essential to understanding the functioning of adolescents who are struggling to self-regulate and manage type 1 diabetes care.
Funding
This research was supported by Grant Number (R01 DK-063044) from the National Institute of Diabetes and Digestive and Kidney Diseases, awarded to Dr D.J.W. (PI) and Dr C.A.B. (co-PI).
Conflicts of interest: None declared.
Acknowledgments
We thank members of the ADAPT research group for their valuable input and assistance during the development and execution of this project. We also thank the physicians and staff at the Utah Diabetes Center and Mountain Vista Medicine, as well as the adolescents and their families who participated in this study.
References
- Aiken L S, West S G. Multiple regression: Testing and interpreting interactions. Thousand Oaks, CA: Sage; 1991. [Google Scholar]
- Austenfeld J, Stanton A. Coping through emotional approach: A new look at emotion, coping, and health related outcomes. Journal of Personality. 2004;72:1335–1364. doi: 10.1111/j.1467-6494.2004.00299.x. [DOI] [PubMed] [Google Scholar]
- Berg C, King P, Butler J, Pham P, Palmer D L, Wiebe D. Parental involvement and adolescents' diabetes management: The mediating role of self-efficacy and externalizing and internalizing behaviors. Journal of Pediatric Psychology. 2011;36:329–339. doi: 10.1093/jpepsy/jsq088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg C A, Butler J M, Osborn P, King G, Palmer D L, Butner J, Murray M, Lindsay R, Donaldson D, Foster C, Swinyard M, Wiebe D J. Role of parental monitoring in understanding the benefits of parental acceptance on adolescent adherence and metabolic control of type 1 diabetes. Diabetes Care. 2008;31:678–683. doi: 10.2337/dc07-1678. [DOI] [PubMed] [Google Scholar]
- Blair C, Diamond A. Biological processes in prevention and intervention: The promotion of self-regulation as a means of preventing school failure. Development and Psychopathology. 2008;20:899–911. doi: 10.1017/S0954579408000436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole P, Martin S, Dennis T. Emotion regulation as a scientific construct: Methodological challenges and directions for child development research. Child Development. 2004;75:317–333. doi: 10.1111/j.1467-8624.2004.00673.x. [DOI] [PubMed] [Google Scholar]
- Coyne L, McHugh L, Martinez E. Acceptance and commitment therapy (ACT): Advances and applications with children, adolescents, and families. Child and Adolescent Psychiatric Clinics of North America. 2011;20:370–399. doi: 10.1016/j.chc.2011.01.010. [DOI] [PubMed] [Google Scholar]
- Dennis T, Hajcak G. Directed appraisals modulate the electrocortical response to arousing negative pictures in children. Journal of Child Psychology and Psychiatry. 2009;50:1373–1383. doi: 10.1111/j.1469-7610.2009.02168.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis T A. Neurophysiological markers for child emotion regulation from the perspective of emotion-cognition integration: Current directions and future challenges. Developmental Neuropsychology. 2010;35:212–230. doi: 10.1080/87565640903526579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diamond L, Fagundes C. Developmental perspectives on links between attachment and affect regulation over the lifespan. Advances in Child Development and Behavior. 2008;36:83–134. doi: 10.1016/s0065-2407(08)00003-7. [DOI] [PubMed] [Google Scholar]
- Duckworth A, Seligman M. Self-discipline outdoes IQ in predicting academic performance of adolescents. Psychological Science. 2005;16:939–944. doi: 10.1111/j.1467-9280.2005.01641.x. [DOI] [PubMed] [Google Scholar]
- Ellis D A, Frey M A, Naar-King S, Templin T. Use of multisystemic therapy to improve regimen adherence among adolescents with type 1 diabetes. Diabetes Care. 2005;28:1604–1610. doi: 10.2337/diacare.28.7.1604. [DOI] [PubMed] [Google Scholar]
- Farrell S P, Hains A A, Davies W H, Smith P, Parton E. The impact of cognitive distortions, stress, and adherence on metabolic control in youths with type 1 diabetes. The Journal of Adolescent Health. 2004;34:461–467. doi: 10.1016/S1054-139X(03)00215-5. [DOI] [PubMed] [Google Scholar]
- Finkenauer C, Engels R, Baumeister R. Parenting behavior and adolescent behavioural and emotional problems: The role of self-control. International Journal of Behavioral Development. 2005;29:58–69. [Google Scholar]
- Fortenberry K, Butler J, Butner J, Berg C, Upchurch R, Wiebe D. Perceived diabetes task competence mediates the relationship of both negative and positive affect with blood glucose in adolescents with type 1 diabetes. Annals of Behavioral Medicine. 2009;37:1–9. doi: 10.1007/s12160-009-9086-7. [DOI] [PubMed] [Google Scholar]
- Gray J R. Integration of emotion and cognitive control. Current Directions in Psychological Science. 2004;13:46–48. [Google Scholar]
- Grey M, Boland E A, Davidson M, Li J, Tamborlane W V. Coping skills training for youth with diabetes mellitus has long-lasting effects on metabolic control and quality of life. The Journal of Pediatrics. 2000;137:107–113. doi: 10.1067/mpd.2000.106568. [DOI] [PubMed] [Google Scholar]
- Hayes S, Luoma J B, Bond F W, Masuda A, Lillis J. Acceptance and commitment therapy: Model processes and outcomes. Behaviour Research and Therapy. 2006;44:1–25. doi: 10.1016/j.brat.2005.06.006. [DOI] [PubMed] [Google Scholar]
- Hofmann W, Friese M, Roefs A. Three ways to resist temptation: The independent contributions of executive attention, inhibitory control, and affect regulation to the impulse control of eating behavior. Journal of Experimental Social Psychology. 2009;45:431–435. [Google Scholar]
- Hood K, Peterson C, Rohan J, Drotar D. Association between adherence and glycemic control in pediatric type 1 diabetes: A meta-analysis. Pediatrics. 2009;124:e1171–e1179. doi: 10.1542/peds.2009-0207. [DOI] [PubMed] [Google Scholar]
- Horton D, Berg C, Butner J, Wiebe D. The role of parental monitoring in metabolic control: Effect on adherence and externalizing behaviors during adoelscence. Journal of Pediatric Psychology. 2009;34:1008–1018. doi: 10.1093/jpepsy/jsp022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Housiaux M, Luminet O, Broeck N, Dorchy H. Alexithymia is associated with glycaemic control of children with type 1 diabetes. Diabetes and Metabolism. 2010;36:455–462. doi: 10.1016/j.diabet.2010.06.004. [DOI] [PubMed] [Google Scholar]
- Hughes A, Berg C, Wiebe D. Poster presented at Annual Convention of the American Psychological Association. San Diego, CA: 2010. Adoelscent reactivity and self-control in understanding diabetes adherence. [Google Scholar]
- Iannotti R, Schneider S, Nansel T, Haynie D, Plotnick L, Clark L, Sobel D O, Simons-Morton B. Self-efficacy, outcome expectations, and diabetes self-management in adolescents with type 1 diabetes. Journal of Developmental and Behavioral Pediatrics. 2006;27:98–105. doi: 10.1097/00004703-200604000-00003. [DOI] [PubMed] [Google Scholar]
- Kashdan T, Ferssizidis P, Collins R, Muraven M. Emotion differentiation as resilience against excessive alcohol use: An ecological momentary assessment in underage social drinkers. Psychological Science. 2010;21:1341–1347. doi: 10.1177/0956797610379863. [DOI] [PubMed] [Google Scholar]
- King P, Berg C, Butner J, Drew L M, Foster C, Donaldson D, Swinyard M, Murray M, Wiebe D. Longitudinal trajectories of metabolic control across adolescence: Associations with parental involvement, adolescents’ psychosocial maturity, and health care utilization. Journal of Adoelscent Health. in press doi: 10.1016/j.jadohealth.2011.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- La Greca A M, Auslander W, Greco P, Spetter D, Fisher E B, Santiago J V. I get by with a little help from my family and friends: Adolescents' support for diabetes care. Journal of Pediatric Psychology. 1995;20:449–476. doi: 10.1093/jpepsy/20.4.449. [DOI] [PubMed] [Google Scholar]
- Lamm C, Lewis M D. Developmental change in the neurophysiological correlates of self-regulation in high- and low-emotion conditions. Developmental Neuropsychology. 2010;35:156–176. doi: 10.1080/87565640903526512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luyckx K, Seiffge-Krenke I, Hampson S E. Glycemic control, coping, and internalizing and externalizing symptoms in adolescents with type 1 diabetes. Diabetes Care. 2010;33:1424–1429. doi: 10.2337/dc09-2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moffitt T, Arseneault L, Belsky D, Dickson N, Hancox R, Harrington H, Houts R, Poulton R, Roberts B W, Ross S, Sears M R, Thomson W M, Caspi A. A gradient of childhood self-control predicts health, wealth, and public safety. Proceedings of the National Academy of Sciences of the United States of America. 2011;108:2693–2698. doi: 10.1073/pnas.1010076108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moss-Morris R, Weinman J, Petric K, Horne R, Cameron L, Buick D. The revised illness perception questionnaire. Psychology and Health. 2002;17:1–16. [Google Scholar]
- Nansel T, Weisberg-Benchell J, Wysocki T, Laffel L, Anderson B. Quality of life in children with type 1 diabetes: A comparison of general and diabetes-specific measures, and support for a unitary diabetes quality of life construct. Diabetic Medicine. 2008;25:1316–1323. doi: 10.1111/j.1464-5491.2008.02574.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Posner M, Rothbart M. Developing mechanisms of self-regulation. Development and Psychopathology. 2000;12:427–441. doi: 10.1017/s0954579400003096. [DOI] [PubMed] [Google Scholar]
- Preacher K, Curran P, Bauer D. Computational tools for probing interaction effects in multiple linear regression, multilevel modeling, and latent curve analysis. Educational and Behavioral Statistics. 2006;31:437–448. [Google Scholar]
- Silk J, Steinberg L, Morris A. Adolescents' emotion regulation in daily life: Links to depressive symptoms and problem behavior. Child Development. 2003;74:1869–1880. doi: 10.1046/j.1467-8624.2003.00643.x. [DOI] [PubMed] [Google Scholar]
- Silverstein J, Klingensmith G, Copeland K, Plotnick L, Kaufman F, Laffel L, Deeb L, Grey M, Anderson B, Holzmeister L,, American Diabetes Association (2005). Care of children and adolescents with type 1 diabetes: A statement of the American Diabetes Association. Diabetes Care, 28, 186–212. [DOI] [PubMed]
- Stanton A, Kirk S, Cameron C, Danoff-Burg S. Coping through emotional approach: Scale construction and validation. Journal of Personality and Social Psychology. 2000;78:1150–1169. doi: 10.1037//0022-3514.78.6.1150. [DOI] [PubMed] [Google Scholar]
- Stanton A, Parsa A, Austenfeld J. The adaptive potential of coping through emotional approach. Handbook of Positive Psychology. 2002:148–158. [Google Scholar]
- Steinberg L. A social neuroscience perspective on adolescent risk-taking. Developmental Review. 2008;28:78–106. doi: 10.1016/j.dr.2007.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg L. A dual systems model of adolescent risk-taking. Developmental Psychobiology. 2010;52:216–224. doi: 10.1002/dev.20445. [DOI] [PubMed] [Google Scholar]
- Tan C, Holub S. Children's self-regulation in eating: Associations with inhibitory control and parents' feeding behavior. Journal of Pediatric Psychology. 2011;36:340–345. doi: 10.1093/jpepsy/jsq089. [DOI] [PubMed] [Google Scholar]
- Tangney J, Baumeister R, Boone A. High self control predicts good adjustment, less pathology, better grades, and interpersonal success. Journal of Personality. 2004;72:271–324. doi: 10.1111/j.0022-3506.2004.00263.x. [DOI] [PubMed] [Google Scholar]
- Wiebe D, Berg C, Korbel C, Palmer D L, Beveridge R, Upchurch R, Lindsay R, Swinyard M T, Donaldson D L. Children's appraisals of maternal involvement in coping with diabetes: Enhancing our understanding of adherence, metabolic control, and quailty of life across adolescence. Journal of Pediatric Psychology. 2005;30:167–178. doi: 10.1093/jpepsy/jsi004. [DOI] [PubMed] [Google Scholar]
- Wiebe D, Croom A, Fortenberry K, Butner J, Butler J, Swinyard M T, Lindsay R, Donaldson D, Foster C, Murray M, Berg C A. Parental involvement buffers associations between pump duration and metabolic control among adolescents with type 1 diabetes. Journal of Pediatric Psychology. 2010;35:1152–1160. doi: 10.1093/jpepsy/jsq012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wysocki T, Harris M A, Buckloh L M, Mertlich D, Lochrie A S, Taylor A, Sadler M, White N H. Randomized, controlled trial of behavioral family systems therapy for diabetes: Maintenance and generalization of effects on parent-adolescent communication. Behavior therapy. 2008;39:33–46. doi: 10.1016/j.beth.2007.04.001. [DOI] [PubMed] [Google Scholar]
- Yurgelun-Todd D. Emotional and cognitive changes during adolescence. Current Opinion in Neurobiology. 2007;17:251–257. doi: 10.1016/j.conb.2007.03.009. [DOI] [PubMed] [Google Scholar]