Abstract
Sexual assault (SA) is common, but the epidemiology of acute pain after SA has not previously been reported. We evaluated the severity and distribution of pain symptoms in the early aftermath of SA among women receiving sexual assault nurse examiner (SANE) care, and the treatment of pain by SANE nurses. Severe pain (≥7 on a 0–10 numeric rating scale) was reported by 53/83 women sexual assault survivors (64% [95% CI, 53%–74%]) at the time of SANE evaluation and 43/83 women (52% [95% CI, 41%–63%]) one week later. Pain in four or more body regions was reported by 44/83 women (53% [95% CI, 42%–64%]) at the time of initial evaluation and 49/83 women (59% [95% CI, 48%–70%]) at one week follow-up. Among survivors with severe pain at the time of initial post-assault evaluation, only 7/53 (13% [95% CI, 6%–26%]) received any pain medication at the time of initial SANE treatment. These findings suggest that pain is common in SA survivors in the early post-assault period, but rarely treated.
Perspective
Acute pain is common after sexual assault. Practice guidelines for SANE nurses and others who provide care to sexual assault survivors in the early aftermath of assault should include specific recommendations for pain evaluation and treatment. Prospective longitudinal studies of pain outcomes among sexual assault survivors are needed.
Keywords: Sexual assault, musculoskeletal pain, stress, pain, treatment
A recent national survey found that 1 in 5 US women experience sexual assault during their lifetime2. Severe acute pain is known to frequently occur after other common trauma exposures, such as motor vehicle collision and burn injury,4, 19 but the epidemiology of acute pain after sexual assault has not been reported. One factor that may contribute to this relative lack of study is that, while sexual assault is a fundamental violation of physical integrity and a profound stress, even minor injury is documented in only one third of sexual assault cases.10
However, even in sexual assault cases in which physical trauma is limited, other factors such as stress-induced hyperalgesia may contribute to post-assault pain. A substantial body of evidence from animal models demonstrates that non-noxious stress exposures may induce hyperalgesia.9 Non-noxious stress exposures in these animal models include unpredictable sound,6 cold environment,16 a vibrating floor plate,22 and restraint.5 Similarly, recent clinical studies indicate that stress system function may have a greater influence on acute pain severity than trauma characteristics (e.g. amount of motor vehicle damage,13 size of burn injury14). These results provide a rationale for the evaluation of acute pain in a sample of women experiencing sexual assault.
In the US, women presenting for care after sexual assault are commonly treated by Sexual Assault Nurse Examiners (SANEs), nurses who have completed training in the delivery of care to sexual assault survivors including standardized forensic evidence collection. SANE programs are most often based in emergency departments, but may also be located in other areas of the hospital or in free standing clinics or community centers. SANE evaluation includes obtaining a detailed medical and forensic history, performing a detailed physical examination to document evidence of trauma or body areas of tenderness, performing comprehensive evidence collection (e.g. combing pubic hair and swabbing oral, vaginal, and/or anal areas), administering medication prophylaxis for sexually transmitted disease and pregnancy, notifying mandated agencies (e.g. law enforcement), and providing follow up medical and community resources. If the SANE program is hospital-based, then an MD will generally also perform an evaluation focused on prescribing medication and excluding additional medical conditions requiring treatment. If the SANE program is located in a free-standing clinic, then MD evaluation is generally only performed on patients referred for additional evaluation by the SANE.
In this study, we evaluated the distribution and severity of pain symptoms at the time of SANE exam and at one week following SANE examination in a sample of women sexual assault survivors presenting for care within 48 hours of sexual assault. In addition, among women reporting pain, we assessed the frequency of pain medication treatment and the types of pain medication provided. Interim results of this study were presented in part at the 2010 and 2011 American Pain Society Annual Scientific Meeting.18, 23
Methods
Participant eligibility criteria and study sites
Women sexual assault survivors 18 years of age or older who presented for medical care (Sexual Assault Nurse Examiner (SANE) evaluation) within 48 hours of sexual assault were recruited for the study. Women unable to give informed consent (e.g. due to intoxication) were excluded, as were women who lived with their assailant, were hospitalized, were prisoners, pregnant, did not have a telephone, and/or did not live within driving distance for the one week follow-up interview. Ten SANE programs (Mercy Medical Center, Baltimore, MD; University of North Carolina, Chapel Hill, NC; Cone Health System, Greensboro, NC; Inova Fairfax Hospital, Falls Church, VA; Sentara Norfolk Hospital, Norfolk, VA; Carolinas Medical Center, Charlotte, NC; Palmetto Health Alliance, Columbia, SC; Wake Forest Baptist Medical Center, Winston-Salem, NC; Forsyth Medical Center, Winston-Salem, NC; Mission Health System, Asheville, NC) participated in the study. These programs care for women sexual assault survivors from diverse environments, from inner-city Baltimore to rural Appalachia. Institutional review board approval was obtained at all study sites.
Study procedures
When a potentially eligible sexual assault survivor presented for care, the SANE nurse provider notified the on call research nurse via a 24 hour study cell phone. The research nurse then came to the study site, introduced themselves to the sexual assault survivor, and asked for consent to (1) telephone the survivor in several days to assess their willingness to perform a one week follow-up interview; (2) perform a brief questionnaire evaluation assessing current pain intensity in each of eight body regions (head & face, neck, breast, arms, abdomen, back, genital and pelvic, and legs). Pain intensity was assessed using a verbal 0–10 numeric rating scale, as this scale has been validated against the visual analogue scale for acute pain measurement and has advantages in acute care settings.1 In recognition of the fact that this consent was obtained at the time of SANE care, a time of great duress and vulnerability, and that safety data regarding this type of research protocol is not available, women were informed that pain questionnaire data would only be retained/used if they also consented to take part in one week interview evaluation.
Sexual assault survivors contacted by telephone and consenting to a one week in person follow-up interview received a re-assessment of current pain symptoms (using the methods described above) and an evaluation of acute stress disorder (ASD) symptoms (ASD Interview3). Detailed sexual assault history and patient physical exam information, demographic information, and information regarding medication prescribed at the time of initial SANE evaluation were obtained from SANE/medical records. Women were compensated $50 for completing the one week interview.
Statistical Analyses
Pain intensity numeric rating scale cut-off scores were defined based on previous research and clinical practice (none (0), mild (1–3), moderate (4–6), severe (7–10)).11 Patient characteristics were evaluated using standard descriptive statistics. Changes in pain characteristics during the week after sexual assault were compared using paired t-tests. The correlation between pain and acute stress disorder symptoms was evaluated using Spearman’s rank correlation analysis. Statistical analyses were performed using SPSS software (SPSS Inc. v19, Chicago, IL).
Results
Participant Characteristics
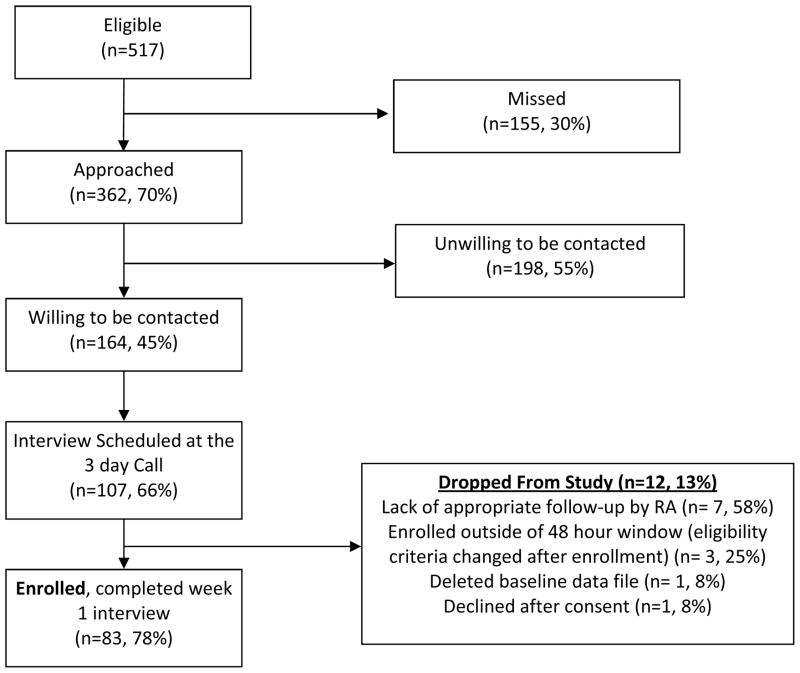
A flow diagram of participant screening and recruitment is shown in Figure 1. Most women were European American (53/83), less than 30 years of age (59/83), had some post high school training or college (71/83), and did not have children (47/83). Median annual family income of study participants was $24,000 – $39,999. Ninety percent (75/83) of women presented within 24 hour of sexual assault, all women presented within 2 days of assault. Most women (69/83, 83%) were evaluated by an emergency physician in addition to the SANE nurse.
Figure 1.
Flow diagram of participant screening and enrollment.
Assault Characteristics
Thirty two women (39%) were not conscious during the assault. Among women who recalled at least some of the assault, 45/50 (90%) experienced penile-vaginal penetration, and 26/50 (52%) experienced multiple forms of assault (e.g. penile-anal, penile-oral, oral-vaginal). Thirteen (26%) experienced repeated assaults over time during the incident, four (8%) experienced assault by multiple assailants. Most women (59/83, 71%) were assaulted by an individual who was not a stranger. Forty five women (54%) had no identifiable physical injury at the time of SANE exam.
Pain Severity and Distribution During the Week after Sexual Assault
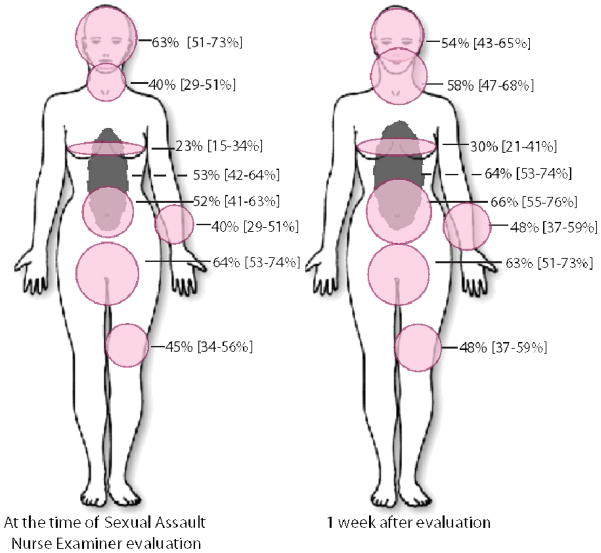
Severe pain in one or more body regions was reported by 53/83 women (64% [95% CI, 53%–74%]) at the time of SANE evaluation and 43/83 women (52% [95% CI, 41%–63%]) one week later. No pain or mild pain was experienced by only 12/83 women (14% [95% CI, 8%–24%]) at the time of SANE evaluation and by 19/83 women (23% [95% CI, 15%–34%])) one week later. The most common locations of pain at the time of initial evaluation were the genital region, head, back, and abdomen (Figure 1). At one week, the most common regions of pain were the abdomen, back, genital and head/neck regions (Figure 1).
Pain in multiple body regions was common (Table 1). Pain in four or more body regions was reported by 44/83 women (53% [95% CI, 42%–64%]) at the time of initial evaluation and 49/83 women (59% [95% CI, 48%–70%]) at one week follow-up (Table 1). Pain in six or more body regions was reported by 19/83 women (23% [95% CI, 15%–34%]) at the time of initial evaluation and 24/83 women (29% [95% CI, 20%–40%]) at one week follow-up. Compared to pain symptoms at the time of initial evaluation, at one week follow-up pain symptoms had decreased in severity (from 6.9 to 6.0, p=.009) and increased in distribution (3.8 to 4.3 body regions with pain, p = .035).
Table 1.
Number of discrete body regions in which sexual assault survivors reported pain (n=83)
| Body regions with pain | At presentation
|
1 week after presentation
|
||
|---|---|---|---|---|
| N (%)* | Cumulative N (%) | N (%)* | Cumulative N (%) | |
| 8 | 4 (5) | 4 (5) | 11 (13) | 11 (13) |
| 7 | 8 (10) | 12 (14) | 7 (8) | 18 (22) |
| 6 | 7 (8) | 19 (23) | 6 (7) | 24 (29) |
| 5 | 7 (8) | 26 (31) | 14 (17) | 38 (46) |
| 4 | 18 (22) | 44 (53) | 11 (13) | 49 (59) |
| 3 | 17 (21) | 61 (73) | 19 (23) | 68 (82) |
| 2 | 9 (11) | 70 (84) | 4 (5) | 72 (87) |
| 1 | 8 (10) | 78 (94) | 5 (6) | 77 (93) |
| 0 | 5 (6) | 83 (100) | 6 (7) | 83 (100) |
Percents may not sum to 100 due to rounding.
Association between location of pain and locations of trauma
Fifty women reported complete recall of the assault. As shown in Table 2, only 62/176 body regions with pain at the time of initial SANE evaluation (36% [95% CI, 28%–43%]) and 54/186 body regions with pain one week after evaluation (29% [95% CI, 23%–36%]) were in body areas in which trauma was documented during detailed SANE history or physical exam (genital region excluded.) Two case examples demonstrate the appearance of extra-genital pain symptoms among women who did not appear to experience extra-genital physical trauma during the assault. One woman stopped at a gas station for gasoline when a man approached her with a gun. At gunpoint he instructed her to drive to a dead end street and to perform oral sex and to have vaginal intercourse with him. She reported begging him not to kill her for the sake of her one year old child, and stated that she offered no resistance. She denied any physical trauma and had no evidence of trauma on exam. At the time of SANE exam, she reported pain in one extra-genital area (head and face), with maximal pain intensity score in extra-genital areas of six. One week after SANE exam, she reported pain in six extra-genital regions, with maximal pain intensity score in extra-genital areas of eight. Another woman was vaginally raped with her six week old baby in her arms. She reported no physical trauma, and she stated that she offered no resistance due to concerns for her child’s safety. At the time of initial SANE evaluation, she reported pain in seven extra-genital body regions, and her maximal pain intensity score in extra-genital areas as ten. One week after presentation, she reported pain in three extra-genital body areas and rated her maximal pain intensity score in extra-genital areas as ten. Among all women sexual assault survivors in our sample, body regions with the highest proportion of pain symptoms one week after assault in the absence of identified trauma were the breast, abdominal, and back regions.
Table 2.
Number of sexual assault survivors reporting pain in each body region at the time of initial presentation for SANE* evaluation and 1 week after presentation, and the number of sexual assault survivors reporting trauma to each body region, by history or physical examination, at the time of SANE evaluation. Only survivors reporting consciousness throughout sexual assault are included (n=50). Genital region excluded.
| Body Region | At presentation
|
1 week after presentation
|
||
|---|---|---|---|---|
| Total with pain in region | Trauma to region | Total with pain in region | Trauma to region | |
| N | N (%) | N | N (%) | |
| Head/Face | 30 | 11 (37) | 29 | 11 (38) |
| Neck | 22 | 11 (50) | 31 | 13 (42) |
| Breast | 14 | 3 (21) | 15 | 1 (7) |
| Arms | 24 | 10 (42) | 23 | 9 (39) |
| Abdomen | 32 | 9 (28) | 32 | 7 (22) |
| Back | 30 | 6 (20) | 34 | 5 (15) |
| Legs | 24 | 12 (50) | 22 | 8 (36) |
| Total Regions | 176 | 62 (35) | 186 | 54 (29) |
SANE = Sexual Assault Nurse Examiner
Association between Pain Severity and Acute Stress Disorder Symptom Severity
All women met diagnostic criteria for acute stress disorder one week after assault (mean ASD score 74.7(11.9). ASD symptom severity was moderately associated with both the intensity of pain symptoms (r = .486, p <.0001) and the number of body regions with pain (r = .331, p = .004). Specific ASD symptoms most strongly associated with pain severity were bad dreams, trouble sleeping, irritability, and feeling jumpy (p < .0001 for all associations).
Treatment of Pain in the Acute Aftermath of Sexual Assault
Among sexual assault survivors with severe pain at the time of initial post-assault evaluation, only 7/53 (13% [95% CI, 6%–26%]) received any pain medication at the time of initial SANE treatment. Upon discharge, two patients received a non-opioid pain medication, one received an opioid, and three received non-medication pain treatment instructions (local heat application). One week after assault, only 12/43 (28% [95% CI, 16%–44%]) with severe pain had received any pain medication.
Discussion
To our knowledge, this is the first prospective study of pain symptoms in the early aftermath of sexual assault. The results of this study, which sampled women sexual assault survivors presenting for care to ten SANE Programs in four states, indicate that the majority of sexual assault survivors experience moderate or severe pain during the early aftermath of assault. In more than half of women sexual assault survivors, pain was present in 4 or more body regions and was rated as severe. Less than one third of women with severe pain received any pain medication.
Among women conscious throughout assault, the majority of areas of pain were not in body areas in which women reported direct trauma. These data, together with case history data such as the two described above, suggest that pain in the aftermath of sexual assault may not simply be an ancillary experience resulting from co-occurring physical trauma or struggle, but (like psychological symptoms) may also be a neurobiological sequela of the stress experience itself. Further research is needed to understand the epidemiology, etiology, and longitudinal course of pain symptoms developing in the aftermath of sexual assault.
Regardless of cause, acute pain is important to identify and treat when present, not only to reduce immediate suffering but also because preliminary evidence suggests that the treatment of acute pain may also improve psychological outcomes8. The education of SANE nurses and others who provide care to sexual assault survivors in the early aftermath of assault should emphasize that moderate or severe pain is common after sexual assault, and should provide specific recommendations for pain evaluation and treatment. This education should include recommendations that both an NSAID and an opioid pain medication be offered to patients with severe pain.12
Several limitations should be considered when interpreting our study results. Most importantly, consistent with other studies enrolling trauma survivors 7, 15, 17, and the challenges of performing ethical studies of severely traumatized individuals in the acute aftermath of trauma, this study enrolled only a minority of potentially eligible women, creating the potential for selection bias. Data from two sources suggest that women sexual assault survivors consenting to the study may have had increased pain symptoms compared to women who did not consent. First, while unweighted group sizes are too small to generate confidence intervals, 2009 data from the National Hospital Ambulatory Care Survey(NHAMCS)20 found that among an estimated 328,272 sexual assault survivors presenting to the ED in 2009 for care in the acute aftermath of sexual assault, 63% reported moderate or severe pain (data not shown), vs. 86% of women in our study. (2009 NHAMCS data is most accurate for comparison, because this was the first year of the NHAMCS in which complete numeric rating scale pain data was collected, resulting in a marked reduction in missing pain rating responses.) Second, during the course of the pilot study, after respondent follow-up data collected by the study team demonstrated that women did not feel coerced to provide data at the SANE time point (data not shown), the consent form was revised to allow use of participant responses at the time of SANE exam. Moderate or severe pain was present in 8/13 (62%) women who completed ED evaluation alone, vs. 86% of women who consented to both ED and one week evaluation. Importantly, while these estimates suggest that women recruited into the study may have had increased pain symptoms, they confirm that moderate or severe pain is present in the majority of sexual assault survivors. An additional study limitation is that women sexual assault survivors in this study were drawn from the Southeastern United States. However, these women came from a wide variety of community settings, from intercity Baltimore to rural settings in Western North Carolina. Finally, available evidence suggests that the majority of sexual assault survivors never present for care or treatment after assault.21 Therefore the pain experiences of these women are not known. Longitudinal studies are needed which assess the epidemiology and etiology of pain after sexual assault, and the potential impact of improved pain treatment on both long term pain and psychological sequelae.
Figure 2.
Percentage (95% CI) of women sexual assault survivors (n = 83) reporting pain in each of eight body regions (head & face, neck, breast, arms, abdomen, back, genital and pelvic, and legs) at the time of Sexual Assault Nurse Examiner evaluation and at one week follow-up evaluation. At each time point, women rated current pain intensity in each region using a 0–10 numeric rating scale (NRS) score. Size of each shaded area is proportional to the percentage of women reporting pain (NRS score > 0) in the region.
Acknowledgments
We would like to thank the participants for taking part in this study.
Footnotes
DISCLOSURES:
The project described was supported by Award Number UL1RR025747 from the National Center for Research Resources. Dr. Rauch’s contribution to this manuscript was partially supported by a Career Development Award (CDA-2) from the Department of Veteran Affairs, Veterans Health Administration, Office of Research and Development, Clinical Sciences Research and Development (PI: Rauch). No conflicts of interest exist for any of the authors.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Bijur PE, Latimer CT, Gallagher EJ. Validation of a verbally administered numerical rating scale of acute pain for use in the emergency department. Acad Emerg Med. 2003;10:390–2. doi: 10.1111/j.1553-2712.2003.tb01355.x. [DOI] [PubMed] [Google Scholar]
- 2.Black MC, Basile KC, Breiding MJ, Smith SG, Walters ML, Merrick MT, Chen J, Stevens MR. The National Intimate Partner and Sexual Violence Survey (NISVS): 2010 Summary Report. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention; 2011. [Google Scholar]
- 3.Brooks R, Silove D, Bryant R, O’Donnell M, Creamer M, McFarlane A. A confirmatory factor analysis of the acute stress disorder interview. J Trauma Stress. 2008;21:352–5. doi: 10.1002/jts.20333. [DOI] [PubMed] [Google Scholar]
- 4.Carroll LJ, Holm LW, Hogg-Johnson S, Cote P, Cassidy JD, Haldeman S, Nordin M, Hurwitz EL, Carragee EJ, van der Velde G, Peloso PM, Guzman J. Course and prognostic factors for neck pain in whiplash-associated disorders (WAD): results of the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders. Spine. 2008;33:S83–92. doi: 10.1097/BRS.0b013e3181643eb8. [DOI] [PubMed] [Google Scholar]
- 5.Gamaro GD, Xavier MH, Denardin JD, Pilger JA, Ely DR, Ferreira MB, Dalmaz C. The effects of acute and repeated restraint stress on the nociceptive response in rats. Physiol Behav. 1998;63:693–7. doi: 10.1016/s0031-9384(97)00520-9. [DOI] [PubMed] [Google Scholar]
- 6.Green PG, Alvarez P, Gear RW, Mendoza D, Levine JD. Further validation of a model of fibromyalgia syndrome in the rat. J Pain. 2011;12:811–8. doi: 10.1016/j.jpain.2011.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hoge E, Worthington J, Nagurney J, Chang Y, Kay E, Feterowski C, Katzman A, Goetz J, Rosasco M, Lasko N, Zusman R, Pollack M, Orr S, Pitman R. Effect of Acute Posttrauma Propranolol on PTSD Outcome an Physiological Responses During Script-Driven Imagery. CNS Neurosci Ther. 2011:1–7. doi: 10.1111/j.1755-5949.2010.00227.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Holbrook TL, Galarneau MR, Dye JL, Quinn K, Dougherty AL. Morphine use after combat injury in Iraq and post-traumatic stress disorder. N Engl J Med. 2010;362:110–7. doi: 10.1056/NEJMoa0903326. [DOI] [PubMed] [Google Scholar]
- 9.Imbe H, Iwai-Liao Y, Senba E. Stress-induced hyperalgesia: animal models and putative mechanisms. Front Biosci. 2006;11:2179–92. doi: 10.2741/1960. [DOI] [PubMed] [Google Scholar]
- 10.Kilpatrick D, Edmunds C, Seymour A. Rape in America: A Report to the Nation. National Victim Center; Arlington, VA: 1992. [Google Scholar]
- 11.Krebs EE, Carey TS, Weinberger M. Accuracy of the pain numeric rating scale as a screening test in primary care. J Gen Intern Med. 2007;22:1453–8. doi: 10.1007/s11606-007-0321-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Macintyre PE, Schug SA, Scott DA, Visser EJ, Walker SM. APM:SE Working Group of the Australian and New Zealand College of Anaesthetists and Faculty of Pain Medicine: Acute Pain Management: Scientific Evidence. Melbourne, Australia: 2010. [Google Scholar]
- 13.McLean SA, Diatchenko L, Lee YM, Swor RA, Domeier RM, Jones JS, Jones CW, Reed C, Harris RE, Maixner W, Clauw DJ, Liberzon I. Catechol O-methyltransferase haplotype predicts immediate musculoskeletal neck pain and psychological symptoms after motor vehicle collision. J Pain. 2011;12:101–7. doi: 10.1016/j.jpain.2010.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Orrey DC, Bortsov AV, Hoskins JM, Shupp JW, Jones SW, Cicuto BJ, Hwang J, Jordan MH, Holmes JH, Haith LR, Roane BM, Diatchenko L, Cairns BA, McLean SA. Catechol-O-Methyltransferase Genotype Predicts Pain Severity in Hospitalized Burn Patients. J Burn Care Res. 2012 Jan 2; doi: 10.1097/BCR.0b013e31823746ed. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Roy-Byrne P, Russo J, Mcihelson E, Zatzick D, Pitman R, Berliner L. Risk Factors and Outcome in Ambulatory Assault Victims Presenting to the Acute Emergency Department Setting: Implications for Secondary Prevention Studies in PTSD. Depress Anxiety. 2004;19:77–84. doi: 10.1002/da.10132. [DOI] [PubMed] [Google Scholar]
- 16.Satoh M, Kuraishi Y, Kawamura M. Effects of intrathecal antibodies to substance P, calcitonin gene-related peptide and galanin on repeated cold stress-induced hyperalgesia: comparison with carrageenan-induced hyperalgesia. Pain. 1992;49:273–8. doi: 10.1016/0304-3959(92)90151-Z. [DOI] [PubMed] [Google Scholar]
- 17.Shalev AY, Freedman S, Peri T, Brandes D, Sahar T, Orr SP, Pitman RK. Prospective study of posttraumatic stress disorder and depression following trauma. American Journal of Psychiatry. 1998;155:630–7. doi: 10.1176/ajp.155.5.630. [DOI] [PubMed] [Google Scholar]
- 18.Soward A, Orrey D, Rotolo S, Rossi C, Roane B, Csontos E, Casto T, Wheeler B, Rauch S, Slade G, McLean SA. Incidence and Distribution of Pain Symptoms After Sexual Assault [abstract]. Presented at the Annual Scientific Meeting of the American Pain Society; Baltimore, MD. May 6–8, 2010. [Google Scholar]
- 19.Summer GJ, Puntillo KA, Miaskowski C, Green PG, Levine JD. Burn injury pain: the continuing challenge. J Pain. 2007;8:533–48. doi: 10.1016/j.jpain.2007.02.426. [DOI] [PubMed] [Google Scholar]
- 20.The National Hospital Ambulatory Medical Care Survey (NHAMCS) [Accessed November 2011]; http://www.cdc.gov/nchs/ahcd.htm.
- 21.Tjaden P, Thoennes N. Full Report of Prevalence, Incidence, and Consequences of Violence against Women: Findings from the National Violence Against Women Survey (NCJ 183781) Washington, DC: National Institute of Justice; 2000. [Google Scholar]
- 22.Vidal C, Jacob J. Hyperalgesia induced by non-noxious stress in the rat. Neurosci Lett. 1982;32:75–80. doi: 10.1016/0304-3940(82)90232-4. [DOI] [PubMed] [Google Scholar]
- 23.Westphal W, Soward AC, Rossi C, Rotolo S, Heafner T, Foley K, Batts J, Casto T, Collette R, Holbrook D, Goodman E, Harney K, Csontos E, Rauch S, Liberzon I, McLean SA. Severe pain is common but rarely treated in the immediate aftermath of sexual assault [abstract]. Presented at the Annual Scientific Meeting of the American Pain Society; Austin, TX. May 19–21, 2011. [Google Scholar]