Abstract
Background
The kidney plays an important role in glucose metabolism, and has been considered a target for therapeutic intervention. The sodium-glucose cotransporter type 2 (SGLT2) mediates most of the glucose reabsorption from the proximal renal tubule. Inhibition of SGLT2 leads to glucosuria and provides a unique mechanism to lower elevated blood glucose levels in diabetes. The purpose of this review is to explore the physiology of SGLT2 and discuss several SGLT2 inhibitors which have clinical data in patients with type 2 diabetes.
Methods
We performed a PubMed search using the terms “SGLT2” and “SGLT2 inhibitor” through April 10, 2012. Published articles, press releases, and abstracts presented at national and international meetings were considered.
Results
SGLT2 inhibitors correct a novel pathophysiological defect, have an insulin-independent action, are efficacious with glycosylated hemoglobin reduction ranging from 0.5% to 1.5%, promote weight loss, have a low incidence of hypoglycemia, complement the action of other antidiabetic agents, and can be used at any stage of diabetes. They are generally well tolerated. However, due to side effects, such as repeated urinary tract and genital infections, increased hematocrit, and decreased blood pressure, appropriate patient selection for drug initiation and close monitoring after initiation will be important. Results of ongoing clinical studies of the effect of SGLT2 inhibitors on diabetic complications and cardiovascular safety are crucial to determine the risk-benefit ratio. A recent decision by the Committee for Medicinal Products for Human Use of the European Medicines Agency has recommended approval of dapagliflozin for the treatment of type 2 diabetes as an adjunct to diet and exercise, in combination with other glucose-lowering medicinal products, including insulin, and as a monotherapy for metformin-intolerant patients. Clinical research also remains to be carried out on the long-term effects of glucosuria and other potential effects of SGLT2 inhibitors, especially in view of the observed increase in the incidence of bladder and breast cancer. SGLT2 inhibitors represent a promising approach for the treatment of diabetes, and could potentially be an addition to existing therapies.
Keywords: sodium-glucose cotransporter type 2, SGLT2, inhibitors, kidney, glucosuria, oral diabetes agent, weight loss
Introduction
The prevalence of diabetes in the US is estimated to be around 25.8 million, which is equivalent to 8.3% of the US population.1 Oral hypoglycemic agents and insulin are standard therapeutic approaches in the management of type 2 diabetes. The efficacy of sulfonylureas is dependent on the residual β-cell mass, and these agents are associated with hypoglycemia and weight gain. Thiazolidinediones can lead to fluid retention and exacerbate congestive heart failure, and rosiglitazone may be associated with an increased risk of myocardial infarction.2 Newer agents, like glucagon-like peptide analogs, which target the incretin pathway, have been shown to cause weight loss, while oral dipeptidyl peptidase inhibitors are associated with weight maintenance. The glucagon-like peptide analogs have to be injected, and are associated with nausea and vomiting in some patients. However, various other options which play a major role in glucose homeostasis, like the kidneys, are still unexplored.
Physicians taking care of patients with type 2 diabetes have to individualize management with consideration of a number of patient factors. These include the degree of glycosylated hemoglobin (HbA1c) reduction needed, risk of hypoglycemia, the side effects of medication, concomitant medical conditions, and the patient’s ability to adhere to the medication regimen and their preferences. Once-daily oral medications with an insulin-independent mechanism of action, less hypoglycemia, and weight loss benefits may simplify therapy and patient adherence, especially in this era of increasing obesity. There is a need for agents with a newer and complementary mechanism of action which can be used throughout the life of a patient with type 2 diabetes. This review explores the physiology of sodium glucose cotransporters (SGLTs) and discusses several SGLT2 inhibitors with early clinical data for patients with type 2 diabetes.
Role of SGLT in glucose homeostasis
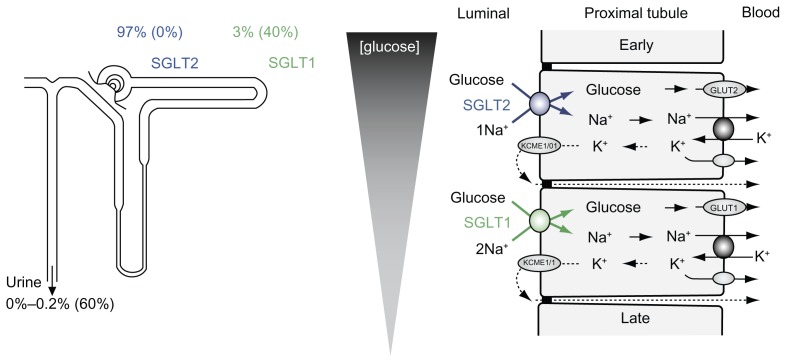
The kidney plays an important role in glucose homeostasis, not only in gluconeogenesis but also in reabsorbing all filtered glucose via transporters called SGLTs. Approximately 180 g of glucose is filtered daily in a healthy adult and most of this is reabsorbed by SGLTs, with <1% being excreted in the urine. The SGLTs are a family of membrane proteins that are responsible for the transport of glucose across the brushborder membrane of the proximal renal tubule and across the intestinal epithelium.3,4 Although there are several different types of SGLTs, the two most studied are SGLT1 and SGLT2. Specifically in the kidney, SGLT2 is predominantly expressed in the earlier segments of the proximal tubule and is responsible for reabsorption of over 90% of the glucose filtered,3,4 while SGLT1, located in the distal segments, absorbs the remainder (Figures 1 and 2).4,5
Figure 1.
Renal glucose transport.
Note: Both SGLT1 and SGLT2 reabsorb the filtered glucose, although the majority of glucose is reabsorbed by SGLT2.
Reproduced with permission: Vallon V. Am J of Physiol Cell Physiol. 2011;300(1):C6–C8.
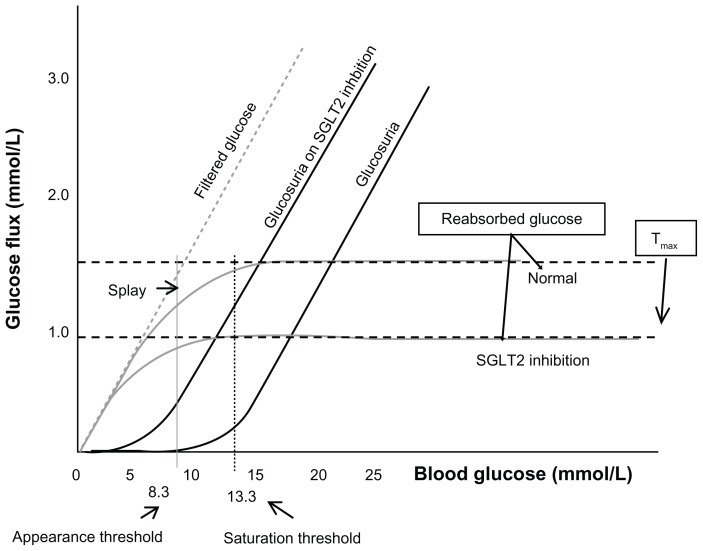
Figure 2.
At plasma glucose concentration around 8.3 mmol/liter, glucose appears in the urine.
Notes: After the saturation threshold of 13.3 mmol/liter, glucosuria increases linearly along with plasma glucose. SGLT2 inhibition promotes glucosuria at an earlier saturation threshold, permitting less reabsorption of glucose.
©2010 The Endocrine Society. Reproduced with permission from Nair S, Wilding JP. Sodium glucose co transporter 2 inhibitors as a new treatment for diabetes mellitus. J Clin Endocrinol Metab. 2010;95(1):34–42.44 http://jcem.endojournals.org/.
SGLT2 has become the focus of a great deal of interest in the field of type 2 diabetes.5 SGLT2 inhibitors block the reabsorption of filtered glucose, leading to glucosuria and improvements in glycemic control. They are also associated with caloric loss, providing the potential for weight loss.
A rare genetic condition which serves as a model for SGLT2 inhibition is familial renal glucosuria. In this disorder, there is impaired functioning of SGLT26,7 secondary to mutation of the SLCA2 gene, leading to daily urinary excretion of up to 100 g of glucose.7,8 Most patients are asymptomatic, and this condition is not associated with any changes in blood glucose concentration, intravascular volume, or renal or bladder function. They do not show an increased incidence of kidney disease, diabetes, or urinary tract infections.7,8 However, in patients with severe forms of familial renal glucosuria, there is indirect evidence of moderate volume contraction, as assessed by activation of the renin-angiotensin-aldosterone system.6–8
SGLTs also play a significant role in the diabetic kidney. In animal models of type 2 diabetes, there is increased expression of SGLT1 and SGLT2 mRNA, with increases in renal glucose transporter expression and activity.9 It has been suggested that reabsorption of glucose from the proximal tubule, that has evolved over generations as an adaptive response, becomes maladaptive in diabetes.10 When proximal tubular cells isolated from patients with both normal glucose tolerance and type 2 diabetes were exposed to a hyperglycemic environment, cells from the patients with type 2 diabetes expressed significantly more SGLT2 and GLUT2 proteins, resulting in a glucose uptake that was three times greater than that in controls.10
These observations led to development of the SGLT2 inhibitors. Inhibition of glucose uptake by the kidneys appears to be a new, unique, and promising insulin-independent approach to the treatment of type 2 diabetes. The parent compound from which the SGLT2 inhibitors are derived is phlorizin, a glucoside isolated from the bark of apple trees that causes inhibition of both SGLT1 and SGLT2.11,12 Because phlorizin had low oral bioavailability and is not selective for SGLT2, other SGLT2 inhibitors were developed, including AVE-2268, remogliflozin, sergliflozin, and WAY-123783. In all of these products, the glucoside moiety was linked via an O-linkage to a distal phenolic ring. However, this O-linkage was subject to β-glucosidases in vivo, which reduced their utility and prompted development of more metabolically stable C-linkage SGLT2 inhibitors. These include dapagliflozin, canagliflozin, empagliflozin, ipragliflozin, BI 44847, and LX 4211.13,14
Dapagliflozin
Dapagliflozin is the selective, orally active, once-daily SGLT2 inhibitor for which there is the most clinical data published in the literature. It has shown linear pharmacokinetics over the dose range of 2.5–500 mg/day and is primarily eliminated via the kidneys.15 Pharmacokinetic and pharmacodynamic studies of dapagliflozin in various populations all over the world have shown predictable dose-proportional parameters in both healthy subjects and those with type 2 diabetes.16 Glucosuria is dose-dependent and ranges from 18 g to 62 g, the effects of which are sustained.15 Dapagliflozin can be administered without regard to meals and has a half-life of approximately 17 hours.15,17 The urinary excretion of dapagliflozin as a parent compound ranges between 0.8% and 4%,15,16 while urinary excretion of its metabolite is 0.1%–0.2%.15
Effects on glycemic parameters and weight
In a 14-day study of patients with type 2 diabetes randomized to three different doses of dapagliflozin, there was a dose-dependent increase in glucosuria ranging from 36.6 g/day to 70.1 g/day versus no change in controls.18 In another study, 389 new-onset, drug-naïve patients with type 2 diabetes were randomized to five different doses of dapagliflozin (2.5, 5, 10, 20, and 50 mg), metformin extended-release, or placebo for 12 weeks.19 The HbA1c reduction ranged from 0.55% to 0.90% for dapagliflozin, was 0.73% for metformin, and was 0.18% in the placebo group. Reduction in fasting plasma glucose was 0.88–1.70 mmol/L (15.8–30.6 mg/dL) in the dapagliflozin groups, and 0.99 mmol/L (17.8 mg/dL) and 0.33 mmol/L (5.9 mg/dL) in the metformin and placebo groups, respectively. There was a similar reduction in post-prandial blood glucose levels in all groups. An HbA1c goal of <7% were reached in 40%–59% in the various dapagliflozin groups versus 54% and 32% in the metformin and placebo groups, respectively, at the end of the study. Moderate glucosuria (mean urinary glucose 52–85 g/day) was found in the dapagliflozin groups versus 6 g/day in the placebo group. Weight reduction was higher in the dapagliflozin groups compared with that on metformin and placebo (2.5–3.4 kg versus 1.7 kg and 1.2 kg, respectively).19
In patients with type 2 diabetes given dapagliflozin monotherapy at three different doses (2.5, 5, and 10 mg) there was a statistically significant improvement in glycemic parameters in the 5 mg and 10 mg groups compared with controls.20 Mean reductions in HbA1c and fasting plasma glucose were 0.58%–0.89% and from 0.84–1.59 mmol/L (15.1–28.6 mg/dL), respectively, in the various dapagliflozin groups compared with 0.23% and 0.22 mmol/L (3.9 mg/dL) for the placebo group. The mean HbA1c reduction was higher in patients with a baseline HbA1c > 9%, ranging from 1.23% to 1.98% compared with 0.16% in the placebo group. An HbA1c goal of <7% were reached in 41%–51% of the various dapagliflozin groups versus 32% in the placebo group at the end of the 24-week study. Mean weight reduction was 2.8–3.3 kg in the dapagliflozin groups compared with 2.2 kg in the control group.20
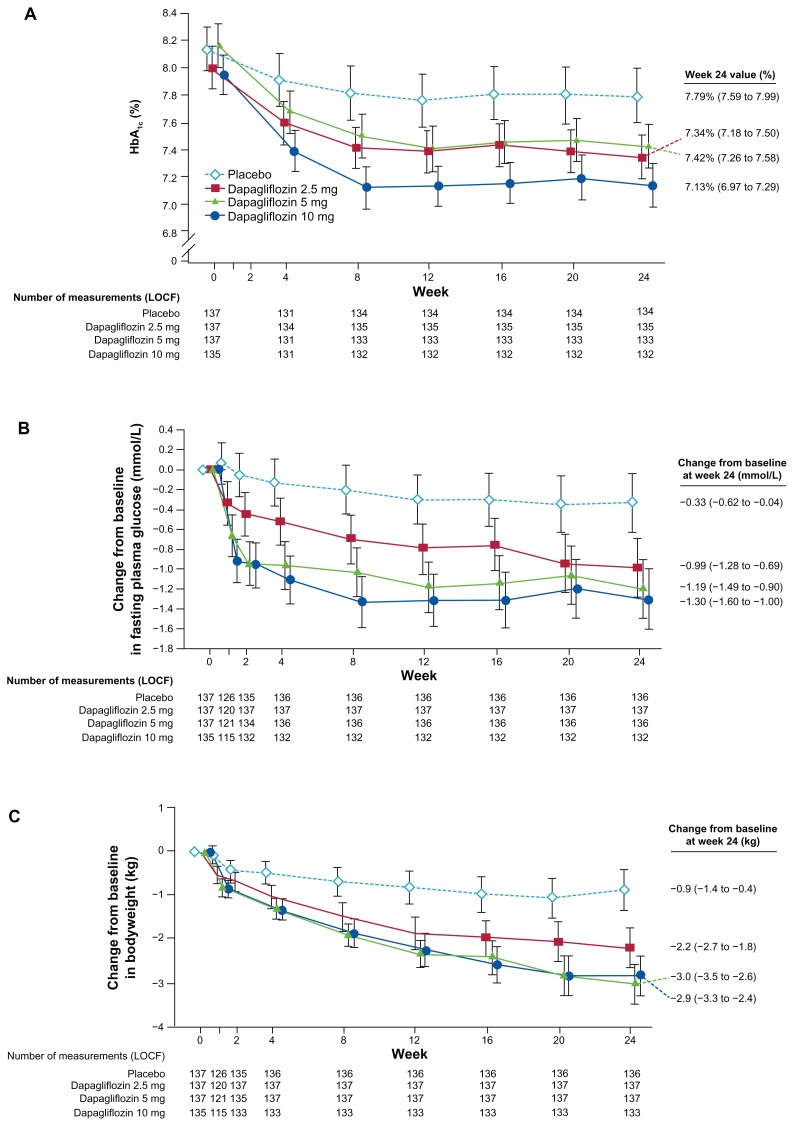
When dapagliflozin was added to metformin monotherapy at various doses (2.5, 5, and 10 mg) in patients with inadequate glycemic control, both HbA1c and fasting plasma glucose showed improvement compared with the control group.21 The mean reduction in HbA1c was 0.67%–0.84% versus 0.30% in the control group. Mean fasting plasma glucose decreased from 0.99 mmol/L to 1.3 mmol/L (17.8 mg/dL to 23.4 mg/dL) from baseline compared with 0.33 mmol/L (5.9 mg/dL) in the control group (Figure 3).21 By the end of the 24-week study, 33% of patients on dapagliflozin 5 mg and 40.6% of those on dapagliflozin 10 mg achieved an HbA1c goal of <7% versus 25.9% of those on placebo. Weight loss ≥ 5% was found in 18.1%–22.1% of patients on dapagliflozin, with an average weight reduction of 2.2–2.9 kg, whereas patients on placebo achieved only a 0.9 kg decrease over 24 weeks (Figure 3).21 Similarly, a reduction in waist circumference of 1.7–2.5 cm occurred in the various dapagliflozin groups compared with 1.3 cm in the placebo group.21
Figure 3.
Change from baseline in A1c, percentage fasting plasma glucose concentration, and total body weight in dapagliflozin 2.5, 5 and 10 mg and placebo groups up to week 24. Reproduced with permission: Bailey et al. Lancet. 2010;375:2223–2233.
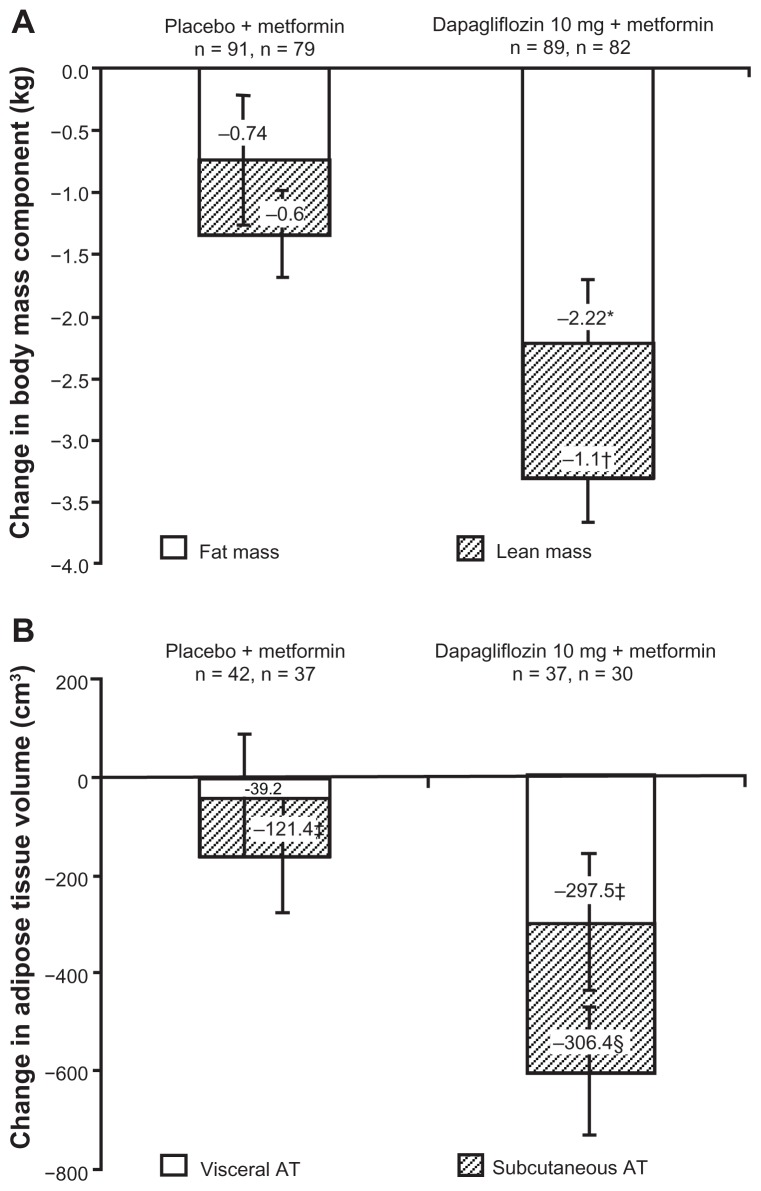
The primary outcomes of a 24-week trial in which patients with type 2 diabetes on metformin monotherapy were randomized to dapagliflozin 10 mg daily or placebo were changes in body weight and total and regional fat mass.22 Placebo-corrected mean reductions in various parameters for patients on dapagliflozin included a 2.08 kg reduction in body weight, a 1.52 cm reduction in waist circumference, and a 1.48 kg reduction in total body fat mass. Two thirds of the total weight loss was attributed to reduction in fat mass, as measured by dual-energy x-ray absorptiometry, and correlated with urinary glucose excretion (Figure 4).22 A weight reduction of at least 5% body weight was seen in 26.2% of patients on dapagliflozin. Men showed a greater decrease in mean body weight (2.76 kg) compared with women (1.22 kg); however, the men were 12 kg heavier at baseline. In a subset of patients who underwent magnetic resonance imaging, there was a reduction in volume of both visceral and subcutaneous adipose tissue (258.4 cm3 and 184.9 cm3, respectively) when controlled for gender and baseline visceral adipose tissue in the dapagliflozin group. There was also a slight reduction (0.82%) in hepatic lipid content.22
Figure 4.
(A and B) Change in body mass component as measured by dual-energy X-ray absorptiometer fat mass and lean mass and Visceral Adipose Tissue (VAT) and Subcutaneous Adipose Tissue (SAT) volume as measured by magnetic resonance substudy, in type 2 diabetes patients inadequately controlled on metformin, randomized to dapagliflozin versus placebo.
©2012 The Endocrine Society. Reproduced with permission from Bolinder J et al. Effects of dapagliflozin on body weight, total fat mass, and regional adipose tissue distribution in patients with type 2 diabetes mellitus with inadequate glycemic control on metformin. J Clin Endocrinol Metab 2012;97(3):20–31.47.22 http://jcem.endojournals.org/.
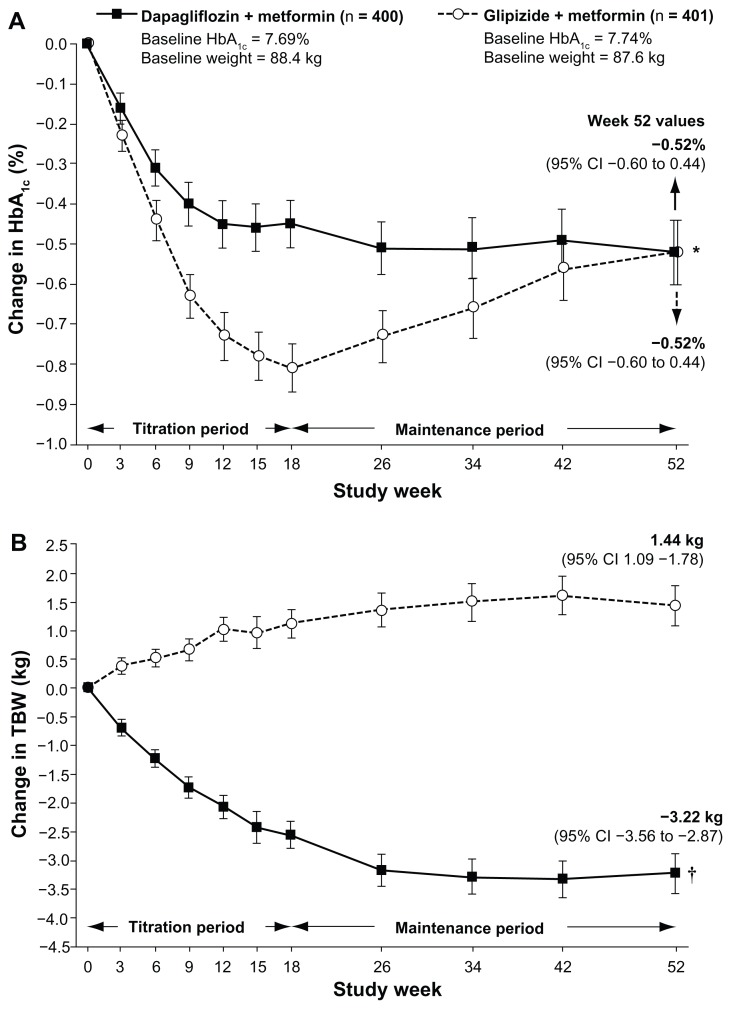
A noninferiority trial was performed in patients with type 2 diabetes (mean baseline HbA1c 7.7%) receiving metformin monotherapy who were randomized to receive either dapagliflozin or glipizide for 52 weeks.23 Doses of both dapagliflozin and glipizide were uptitrated to a maximum of 10 mg and 20 mg daily, respectively, or until the maximum tolerated dose was reached over the first 18 weeks. The mean HbA1c reduction at 18 weeks was greater for glipizide. However, at the end of the study, it was the same in both groups (0.52%), indicating that dapagliflozin was noninferior to glipizide. In addition, there was a mean difference in body weight of 4.65 kg between the two groups, ie, a 3.22 kg loss in the dapagliflozin group versus a 1.9 kg gain in the glipizide group (Figure 5). The percent of patients achieving a weight reduction ≥5% was higher in the dapagliflozin group than in the glipizide group (33.3% versus 2.5%). Glucosuria remained elevated and constant from week 12 to the end of the study.23
Figure 5.
(A and B) Change in A1c and body weight over a 52 week trial of type 2 diabetes patients uncontrolled on metformin randomized to glipizide versus dapagliflozin. Reproduced with permission: Nauck et al. Diabetes Care. 2011;34(9):2015–2022.
In a 24-week trial, 597 patients with uncontrolled type 2 diabetes (HbA1c 7%–10%) on glimepiride monotherapy were randomized to either dapagliflozin or placebo.24 The mean reduction in HbA1c from baseline for the placebo versus dapagliflozin 2.5, 5, and 10 mg groups was statistically significant (0.13% versus 0.58%, 0.63%, and 0.82%, respectively). This was associated with significant reductions in fasting plasma glucose, post-prandial blood glucose, and body weight in the dapagliflozin 5 mg and 10 mg groups compared with controls, ie, 1.18 mmol/L, and 1.58 mmol/L versus 0.11 mmol/L (21.2 mg/dL, and 28.4 mg/dL versus 1.98 mg/dL); 1.78 mmol/L, and 1.94 mmol/L versus 0.33 mmol/L (32.0 mg/dL, and 34.9 mg/dL versus 5.9 mg/dL); and 1.56 kg and 2.26 kg versus 0.72 kg, respectively. By the end of the study, 30.3% in the dapagliflozin 5 mg group and 31.7% in the dapagliflozin 10 mg group had achieved their HbA1c goal of <7% versus 13% in the placebo group.24
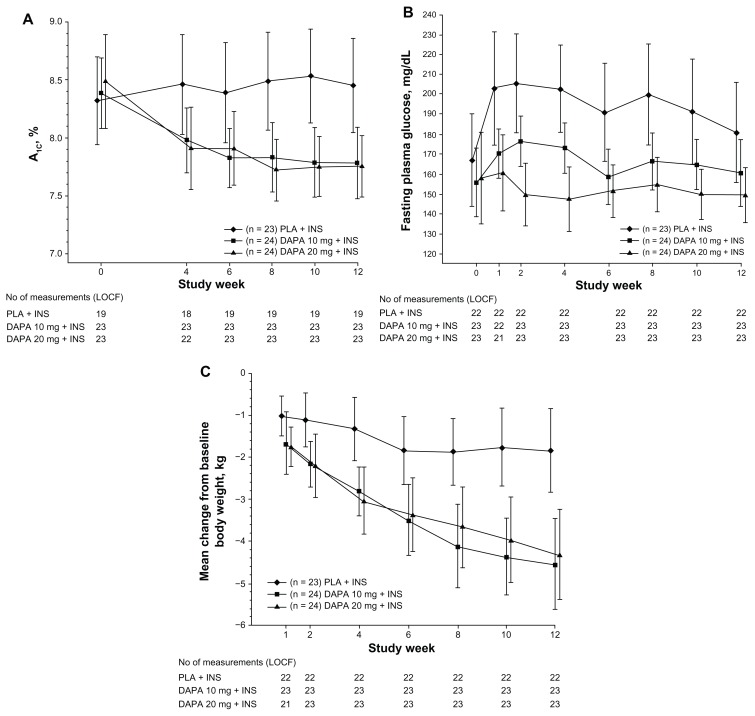
Patients with uncontrolled type 2 diabetes on high doses of insulin (≥50 U/day) and on oral sensitizers were randomized to dapagliflozin 10 mg or 20 mg daily or to placebo for 12 weeks.25 The baseline insulin dose was reduced by 50% in all three groups. The dapagliflozin 10 mg and 20 mg groups demonstrated an HbA1c reduction of 0.61% and 0.69%, compared with a rise of 0.09% in the placebo group. Mean fasting plasma glucose rose by 0.98 mmol/L (17.8 mg/dL) and 0.13 mmol/L (2.34 mg/dL) from baseline in the placebo group and dapagliflozin 10 mg group, respectively, but decreased by 0.53 mmol/L (9.54 mg/dL) in the dapagliflozin 20 mg group (Figure 6). Post-prandial blood glucose reductions with dapagliflozin were also dose-dependent, ie, 1.90 mmol/L (34.4 mg/dL) in the 10 mg group and 2.32 mmol/L (41.9 mg/dL) in the dapagliflozin 20 mg group compared with an increase of 1.03 mmol/L (18.7 mg/dL) in the placebo group. Urinary glucose excretion was 1.5 g/day in the placebo group compared with 83.5 g/day and 85.2 g/day in the 10 mg and 20 mg dapagliflozin groups, respectively. There was a greater reduction in total body weight in the dapagliflozin 10 mg and 20 mg groups compared with placebo, ie, 4.5 kg and 4.3 kg versus 1.9 kg, respectively.25
Figure 6.
(A–C) Mean A1c, Fasting Plasma Glucose (FPG) and change in body weight from baseline over 12 weeks in patients with type 2 diabetes receiving insulin plus insulin sensitizers, randomized to dapagliflozin versus placebo.
Reproduced with permission: Wilding JP et al. Diabetes Care. 2009;32(9):1656–1662.
To detect whether there was a difference in the efficacy and safety parameters for dapagliflozin 10 and 20 mg daily in patients with “early-stage” versus “late-stage” diabetes, data from two different studies performed in these populations were compared.20,25,26 Data from a total of 209 patients (151 early-stage patients and 58 late-stage patients) given dapagliflozin for 12 weeks were analyzed.26 Early-stage patients were treatment-naïve, while late-stage patients were already on insulin plus oral sensitizers, with an average diabetes duration of 0.9 years and 11.1 years, respectively. The baseline insulin dose was reduced by 50% in the “late-stage” patients. In addition, patients in the late-stage population had a higher HbA1c, body weight, fasting plasma glucose, and urinary glucose excretion at baseline when compared with the early-stage population. Both early-stage and latestage patients had similar HbA1c reductions on dapagliflozin therapy compared with placebo. Higher baseline HbA1c in both groups was associated with a greater reduction at the end of the study. Late-stage patients had a greater reduction in body weight, ie, 0.6 kg, 2.3 kg, and 2.5 kg more than early-stage patients in the placebo and dapagliflozin 10 mg and 20 mg groups, respectively. The higher baseline body mass index and reduction of insulin dose by 50% at the start of study may have contributed to the greater weight reductions. Even the late-stage placebo group showed a greater reduction in weight compared with the early-stage placebo group. There was no statistically significant difference in the amount of urinary glucose excretion between the early-stage and late- stage patients.26 Another study by Wilding et al reported on the efficacy and safety of adding various doses of dapagliflozin (2.5, 5, and 10 mg daily) for 48 weeks in 808 patients with inadequately controlled type 2 diabetes receiving at least 30 U of insulin daily, with or without up to two oral antidiabetic drugs. The mean HbA1c reduction at 24 weeks was 0.79%–0.96% on dapagliflozin compared with 0.39% on placebo. The daily insulin dose decreased by 0.63–1.95 U on dapagliflozin and increased by 5.65 U on placebo. Body weight decreased by 0.92–1.61 kg on dapagliflozin and increased by 0.43 kg on placebo. All these effects were maintained at 48 weeks. Patients in the dapagliflozin groups had a higher rate of hypoglycemic episodes (56.6% versus 51.8%), genital infections (9.0% versus 2.5%), and urinary tract infections (9.7% versus 5.1%) when compared with the placebo group.27 These studies indicate that dapagliflozin was efficacious regardless of diabetes duration.
Two recently published trials randomized treatment-naïve type 2 diabetic patients with a baseline HbA1c in the range of 7.5%–12% to one of three treatment arms, ie, a combination of metformin and dapagliflozin, metformin monotherapy, or dapagliflozin monotherapy for 24 weeks.28 Patients in study 1 received dapagliflozin 5 mg daily and achieved an HbA1c reduction of 1.98% compared with 1.35% and 1.19% in the metformin and dapagliflozin monotherapy groups, respectively. Patients in study 2 received dapagliflozin 10 mg daily, which was associated with an HbA1c reduction of 2.05% compared with 1.44% and 1.45% in the metformin and dapagliflozin monotherapy groups, respectively. The mean HbA1c reduction was better in the combination group in both studies and was similar in the groups receiving metformin 2 g/day and dapagliflozin 10 mg/day in study 2.28 Similarly, reductions in fasting plasma glucose and body weight were better in the combination group in both studies. The effects of dapagliflozin on glycemic parameters and weight are summarized in Table 1.
Table 1.
Efficacy of dapagliflozin in various studies
| Study | Dapagliflozin dose | Placebo-corrected decrease in HbA1c (%) | Placebo-corrected achievement of goal HbA1c < 7% (%) | Placebo-corrected decrease in FPG (mmol/L) | Placebo-corrected decrease in PPBG (mmol/L) | Placebo-corrected weight reduction (kg) |
|---|---|---|---|---|---|---|
| Bailey et al | 2.5, 5, 10 mg | 0.37–0.54 | 7.1–14.7 | 0.66–0.97 | N/A | 1.3–2.0 |
| Bolinder et al | 10 mg | 0.28 | N/A | 0.95 | N/A | 2.08 |
| Ferranini et al | 2.5, 5, 10 mg | 0.35–0.66 | 9–19 | 0.62–1.37 | N/A | 0.6–1.1 |
| List et al | 2.5, 5, 10, 20, 50 mg | 0.37–0.72 | 8–27 | 0.55–1.39 | 1.19–2.15 | 1.3–2.2 |
| Nauck et al* | 10 and 20 mg | 0 | 4.6 | 0.20 | N/A | 4.65 |
| Strojek et al | 2.5, 5, 10 mg | 0.45–0.69 | 17.3–18.7 | 1.07–1.47 | 1.45–1.61 | 0.46–1.54 |
| Wilding et al | 10 and 20 mg | 0.70–0.78 | N/A | 0.85–1.52 | 2.94–3.36 | 2.4–2.6 |
| Zhang et al+ | 10 and 20 mg | E, 0.3–0.5 | N/A | N/A | N/A | E, 1.05–1.55 |
| L, 0.6–0.8 | L, 2.75–3.5 |
Notes:
Dapagliflozin was compared with glipizide, not placebo, in a noninferiority trial;
patients with type 2 diabetes divided into early and late stages.
Abbreviations: E, early, L, late; N/A, not available; FPG, fasting plasma glucose.
Serum electrolytes, kidney function, and hematocrit
No clinically meaningful changes in serum electrolytes, serum creatinine, or estimated glomerular filtration rate have been noted.19–22,24 Two studies showed a mild decrease in calculated creatinine clearance without any associated renal impairment or failure, and no changes in estimated glomerular filtration rate.22,24,25 One study showed no change in blood urea nitrogen,20 while in most others there was a slight dose-dependent increase in blood urea nitrogen levels19,21–24 and hematocrit19–25 in the dapagliflozin groups compared with controls. A small increase in 24-hour urine volume was noted, ranging from 107 mL to 470 mL above baseline at the end of the study in the dapagliflozin group.19,25 Most studies showed a lowering of serum uric acid levels.19–25
The rise in hematocrit was small, in the range of 1.5%–2.9% from baseline, and was found in only a small number of patients. This elevation was not associated with thromboembolic events in most studies.19–22 A transient ischemic event that was not associated with a meaningful change in hematocrit was reported.22 Another study reported one stroke with pulmonary embolism, resulting in death, in the dapagliflozin 10 mg group. In this subject, the hematocrit increased from 38% at baseline to 42% 12 days prior to stroke, and was 45% one day after the stroke.24
Cardiovascular system
Dapagliflozin at supratherapeutic doses did not have a clinically significant effect on the QT interval29 or on seated heart rate in healthy men.22,23 There was a slight increase in serum high-density lipoprotein (from 1.8% to 4.4%) and a decrease in triglycerides (from 2.4% to 6.2%) from baseline on the various dapagliflozin doses compared with placebo (0.4% increase in high-density lipoprotein and 2.1% decrease in triglycerides).21 Similar slight increases in serum high-density lipoprotein levels were seen in some studies,20,23 while no change in serum lipids were seen in others.19
When dapagliflozin was used as monotherapy or added to metformin monotherapy, there was a decrease in mean systolic and diastolic blood pressure compared with the placebo group.19–21,23,24 A post hoc analysis in hypertensive patients not meeting their blood pressure goal of <130/80 mmHg at baseline showed that 29.5%–37.5% of such patients in the various dapagliflozin groups achieved their target blood pressure at 24 weeks compared with 8.8% of patients in the placebo group.21
When added to glimepiride, systolic blood pressure was reported to decrease in the dapagliflozin groups with no increase in orthostatic hypotension as compared with the control group (3% in placebo versus 3.6%–4.3% in the dapagliflozin groups).24 However, there was one reported episode of syncope in the dapagliflozin group, and it is noted that the use of other antihypertensive medications was not regulated during this trial.24 Similar results were seen when dapagliflozin was added in patients with type 2 diabetes on insulin and oral agents, with an average decrease in standing systolic and diastolic blood pressure of 6.1–7.2 mmHg and 1.2–3.9 mmHg, respectively.25 Other studies reported either no orthostatic symptoms in dapagliflozin groups20,21,23 or the incidence was the same as in controls.19
Bone mineral density
There was no change in serum 25 hydroxyvitamin D and 1,25-dihydroxyvitamin D levels when compared with baseline in one study.19 Mean changes in 24-hour urine calcium to creatinine ratio were the same as in the placebo group. Parathyroid hormone levels were slightly increased from baseline, ranging from 0.6 pg/mL to 7 pg/mL in the dapagliflozin groups compared with 0.8 pg/mL in the placebo group.19 Only one study reported bone mineral density data in a subset of postmenopausal patients. There was no difference in the dapagliflozin group compared with controls at the end of 24 weeks: a 0.194 g/cm2 reduction from baseline versus 0.200 g/cm2, respectively.22
Special populations and drug interactions
Dapagliflozin 10 mg was well tolerated by patients with mild, moderate, or severe hepatic impairment. However, patients with severe hepatic impairment had higher exposure to dapagliflozin. 30 Dapagliflozin may be less effective in patients with chronic kidney disease, and the recommendation from the Committee for Medicinal Products for Human Use is to avoid its use in patients with moderate to severe renal impairment.31 No clinically meaningful drug–drug interactions have been identified between dapagliflozin and commonly used medications in type 2 diabetes, ie, simvastatin, valsartan, warfarin, and digoxin.32 Dapagliflozin can be coadministered with pioglitazone, metformin, glimepiride, or sitagliptin without dose adjustments.33
Adverse events
The most commonly associated and important adverse effects associated with dapagliflozin are an increased incidence of hypoglycemia, and genital and lower urinary tract infections compared with placebo.
Hypoglycemia
Minor hypoglycemic episodes were increased (6%–10%) in the dapagliflozin-treated groups compared with placebo (4%–4.8%) in a few studies,18,24,25 with no patients being discontinued because of hypoglycemia.20,22–25 In another study, there was a slight increase in minor hypoglycemic events in the placebo group (3.3%) when compared with the dapagliflozin group (2.2%).22 In two other studies, there was no difference in the incidence of hypoglycemia on dapagliflozin when compared with placebo.20,21 The incidence of hypoglycemia was about equal when five different doses of dapagliflozin monotherapy were compared with metformin monotherapy, ie, 6%–10% versus 9%, respectively.18 Use of dapagliflozin with insulin therapy was associated with a greater incidence of hypoglycemia in the dapagliflozin 10 mg and 20 mg groups compared with placebo (25% and 29.2% versus 13%, respectively), despite a reduction in the baseline insulin dose by 50%.25
When dapagliflozin or glipizide was added to metformin monotherapy, there was a 10-fold lower rate of hypoglycemia in the dapagliflozin group compared with the glipizide group (3.4% versus 39.7%).23 There were no severe hypoglycemic episodes in the dapagliflozin group compared with three such episodes in the glipizide group. Six patients discontinued glipizide secondary to hypoglycemia, but none did so in the dapagliflozin group.23 No severe hypoglycemic episodes were reported in the dapagliflozin groups in other studies.19–25,28
Genital infections
There was an increase in genital infections in the dapagliflozin groups compared with controls in almost all the studies, with the incidence increasing with higher doses of dapagliflozin.20,23–25 The reported incidence varied from 3% to 13% versus 0% to 5% in the placebo group,20–25 except for one study where an incidence of 20.8% was reported in the dapagliflozin 20 mg group.25 When dapagliflozin monotherapy was compared with metformin monotherapy, the incidence of genital infections was 2%–7% versus 2%, respectively.19 Similarly, in two studies, treatment-naïve patients randomized to metformin + dapagliflozin, dapagliflozin alone, or metformin alone, showed incidences of 6.7%–8.5% versus 6.9%–12.8% versus 2.0%–2.4%, respectively. 28 The number of events in each patient was 1–3, and each event responded well to conventional therapy. There was only one discontinuation secondary to vulvovaginal pruritus,22 but genital infections rarely led to discontinuation of the study drug in the trials.21,23
Urinary tract infections
The incidence of lower urinary tract infections was higher in the dapagliflozin groups compared with those on placebo and on the other oral hypoglycemics used in the various studies,20,21,23,25 but was reported to be the same in one study.24 Reported urinary tract infection rates were 1%–12.9% in the dapagliflozin groups versus 0%–6.2% in controls19–24 and 9% on metformin monotherapy.19 Similarly, in treatment-naïve patients who were randomized to metformin + dapagliflozin, dapagliflozin alone, or metformin alone, the incidences were 7.6%–7.7% versus 7.9%–11.0% versus 4.3%–7.5%, respectively.27 Most urinary tract infections were single events,23 mild to moderate in intensity, and responded to routine management.23,24 There were two discontinuations secondary to dysuria and urinary tract infection,22,24 in contrast with most studies, in which urinary tract infections rarely led to study discontinuation.20,21,23,24 There were two cases of pyelonephritis in the glipizide group but none in the dapagliflozin group.23
Incidence of cancer
There were nine cases of bladder cancer in 5478 patients (0.16%) on dapagliflozin versus one in 3156 patients on placebo (0.03%, P = 0.15).34,35 This was extrapolated to be 207 cases per 100,000 person-years of exposure in dapagliflozin-treated patients versus 53 cases per 100,000 person-years of exposure in controls. Moreover, nine of 2223 women developed breast cancer in the dapagliflozin group (0.4%) versus one of 1053 women on placebo (0.09%, P = 0.27).34,35 The breast cancer incidence was extrapolated to 224.5 cases per 100,000 person-years.35
Based on evaluation of the Surveillance Epidemiology and End Results database and review of the literature on incidence rates for cancer in type 2 diabetes, it was determined that the number of observed breast and bladder cancers in the dapagliflozin-treated group exceeded the expected number of cases in the general population with type 2 diabetes. All bladder cancers in subjects receiving dapagliflozin were reported within 2 years (43–727 days) of starting this therapy.35 In two of the nine subjects with breast cancer, the diagnosis was made within 6 weeks of initiation of dapagliflozin therapy. Seven of these subjects were older than 60 years. Risk factors for breast and bladder cancer at baseline were similar between the dapagliflozin-treated patients and controls.35
Serious adverse events
In one of the initial Phase III trials comparing dapagliflozin monotherapy with placebo, there was a low overall incidence of serious adverse events in the various dapagliflozin groups (0%–1.6% versus 4% in controls).20 One death occurred in the dapagliflozin 10 mg group as a result of a motor vehicle accident.20 One study had an increased incidence of serious adverse events in the dapagliflozin group compared with controls (6.6% versus 1.1%),22 while another study had a lower rate of serious adverse events (3% in three different dapagliflozin groups versus 4% on placebo).21 Serious adverse events were associated with an increased rate of drug discontinuation on dapagliflozin (4.4% versus 0% on placebo) and one death secondary to pneumonia and esophageal varices.22 When dapagliflozin was compared with glipizide, serious adverse event rates related to study treatments were 1.5% versus 1%, respectively, with three deaths in the glipizide group compared with none in the dapagliflozin groups.23 Serious adverse events in another study were observed in 4.8% of patients on placebo, 7.1% on dapagliflozin 2.5 mg, and 6.9% and 6% on dapagliflozin 5 mg and 10 mg, respectively, with two deaths (one each on dapagliflozin 2.5 mg and 10 mg).24 Two other studies showed similar serious adverse event rates for dapagliflozin and controls.19,25
Adverse events leading to study discontinuation were slightly more common in the dapagliflozin groups compared with placebo (4.4%–7.1% versus 0%–2.1%, respectively).20,22,24 When compared with glipizide, the discontinuation rate was still high (9.1% versus 5.9%, respectively),23 with the majority of discontinuations being secondary to a decrease in calculated creatinine clearance.23 However, when baseline weight was used for calculation, there was no change,23 and the authors concluded that dapagliflozin was not associated with clinically relevant impairment of kidney function.23 In other studies, the discontinuation rate was same for controls and for subjects on dapagliflozin,25 or was higher in controls (4% versus 3%).21 Some studies reported no discontinuation at all.19
Other SGLT2 inhibitors
Canagliflozin
A Phase I study investigated seven different doses of oral canagliflozin once daily (10, 30, 100, 200, 400, 600, or 800 mg) and one dose of 400 mg twice daily in 63 healthy adult men.36 Canagliflozin was absorbed rapidly and had a half-life of 15–16 hours, indicating that once-daily dosing is appropriate.37 The mean renal threshold for glucose was decreased in a dose-dependent manner, with an increase in 24-hour glucose excretion (up to 70 g). Eight percent of subjects reported transient postural dizziness, and in two of them, there was transient postural hypotension. Canagliflozin was generally well tolerated, with no hypoglycemic events, and all subjects completed the study.36,37
Another Phase IB study randomized 29 patients with suboptimally controlled type 2 diabetes on insulin and one oral agent to oral canagliflozin 100 mg or 300 mg twice daily or to placebo for 28 days.37 At the end of the study, HbA1c had decreased by 0.73%, 0.92%, and 0.19%, respectively. Similar reductions were seen in body weight, ie, a 0.03 kg increase on placebo compared with reductions of 0.73 kg and 1.19 kg with the two canagliflozin doses. There was a reduction in both systolic and diastolic blood pressure of up to 10.7 mmHg and 4.5 mmHg from baseline, respectively, compared with reductions of 2.1 mmHg and 0.9 mmHg in controls. Nine patients in the canagliflozin group and three in the placebo group reported mild to moderate hypoglycemic events. No serious adverse events were noted, and there were no discontinuations from the study.37
A recent Phase II double-blind, placebo-controlled, parallel-group, multicenter, dose-ranging study randomized 451 subjects with type 2 diabetes inadequately controlled with metformin monotherapy to canagliflozin 50, 100, 200, or 300 mg once daily or 300 mg twice daily, sitagliptin 100 mg once daily, or placebo.38 There was a significant reduction in HbA1c at 12 weeks compared with baseline of 0.79%, 0.76%, 0.70%, 0.92%, and 0.95% for canagliflozin 50, 100, 200, and 300 mg once daily and 300 mg twice daily, respectively, versus 0.22% for placebo and 0.74% for sitagliptin. Fasting plasma glucose was reduced by 16–27 mg/dL and body weight by 2.3%–3.4% in the canagliflozin groups. A dose-independent increase in symptomatic genital and urinary tract infections was seen with canagliflozin (3%–8% and 3%–9%, respectively) compared with the placebo and sitagliptin arms. Other adverse events were transient, mild to moderate, and balanced across all treatment arms, and the overall incidence of hypoglycemia was low.38
Ipragliflozin
A preliminary Phase I study in healthy patients indicated that ipragliflozin was absorbed rapidly, with a half-life of 12 hours, suggesting that it can be used once daily.39 Ipragliflozin was evaluated for over 4 weeks in 61 patients with type 2 diabetes given four different oral daily doses (50, 100, 200 and 300 mg) versus placebo. Mean HbA1c reduction was 0.61%–0.84% compared with 0.10% for placebo. Fasting plasma glucose reduced by 0.58 mmol/L (10.45 mg/dL) on placebo and by 2.7–3.9 mmol/L (48.6–70.2 mg/dL) on the various doses of ipragliflozin. Weight reduction with ipragliflozin was 3.0–3.8 kg versus a gain of 1.6 kg in the placebo group.40 Maximum urinary glucose excretion was 90 g daily in this study. Of 48 patients receiving ipragliflozin, two experienced urinary tract infections by days 9 and 14 that were treated with antibiotics. There were no reports of genital infections and there were two serious adverse events (one each on ipragliflozin and placebo).40
Others
Three different doses of remogliflozin etabonate (100 mg twice daily, 1000 mg daily, or 1000 mg twice daily) versus placebo were evaluated in 36 patients with type 2 diabetes who were either treatment-naïve or had been on stable doses of metformin for at least 3 months. Mean fasting plasma glucose reduction was 2.1–2.3 mmol/L (37.8–41.4 mg/dL) on the various doses of remogliflozin. Weight reduction with remogliflozin was 2.3–4.5 kg versus a gain of 1.6 kg in the placebo group. Urinary glucose excretion was nonlinear, with apparent saturation on higher doses, and was approximately 90 g daily in the 100 mg twice-daily group.14
Empagliflozin, sergliflozin, and tofogliflozin have some preliminary animal and cell line data available, and some of these agents have not been further developed for unspecified reasons.13,41–43 Several other SGLT2 inhibitors (BI 44847, PF-04971729, TS-071) are still in development, and no published data are available as yet.
Clinical potential of SGLT2 inhibitors
The mechanism of SGLT2 inhibition is independent of β-cell function or mass and insulin sensitivity, and hence can be used in eligible patients, regardless of duration of diabetes, in combination with other oral agents and insulin. They lower the HbA1c level by 0.5%–1.5% from baseline, and the available data suggest a good tolerability profile. Furthermore, SGLT2 inhibitors are associated with clinically significant weight reductions averaging 2.5–3.0 kg or more, which have been attributed to glucosuria, with a loss of approximately 200–300 calories per day.19 The available data also suggest that the weight loss is associated with fat mass reduction.22 The weight loss seen with SGLT2 inhibitors is similar to that seen with glucagon-like peptide 1 analogs, and may be more acceptable because they are oral agents. The reduction in visceral and subcutaneous adipose tissue areas may be an advantage in patients with type 2 diabetes who have associated insulin resistance. In addition, dapagliflozin in patients on oral sulfonylureas and/or insulin therapy may help to attenuate the weight gain associated with these agents.
Genetic mutations leading to renal glucosuria support the long-term safety of SGLT2 inhibition in humans. However, the long-term efficacy and safety of these drugs in patients with type 2 diabetes remains to be seen. Serious adverse event rates (including death) were low and no episodes of severe hypoglycemia were observed. The most commonly reported side effects in the clinical trials were urinary and/or genital tract infections, which were reported as mild to moderate, and either self-limited or resolving with appropriate treatment.
In July 2011 and January 2012, the US Food and Drug Administration voted against the approval of dapagliflozin, and asked for more data from ongoing studies and new clinical trials to assess better the drug’s risk-benefit profile, especially in view of the reported increase in incidence of breast and bladder cancer.34,35 However, a cause and effect relationship has not been established, and the possibility of diagnostic bias has been raised. It has been suggested that due to the glucosuria and/or increased symptoms of urinary tract infection, patients may have undergone more urinalyses, leading to early findings of hematuria or abnormalities and an earlier diagnosis of bladder cancer. It was also suggested that breast masses were better identified after the weight loss seen in patients on dapagliflozin.34,35
The Committee for Medicinal Products for Human Use of the European Medicines Agency has recently recommended approval of dapagliflozin for the treatment of type 2 diabetes, as an adjunct to diet and exercise, in combination with other glucose-lowering medicinal products including insulin, and as a monotherapy in metformin-intolerant patients.31 It is uncertain whether dapagliflozin treatment is associated with an increased risk of breast and bladder cancer on the basis of currently available data. However, continued surveillance for bladder and breast cancer will be needed. Continued followup of all participants in the dapagliflozin trials and further analysis directly between the dapagliflozin therapy and the comparator should be done to evaluate the relative risk of breast and bladder cancer. Further, there are limited data in the elderly population (aged >75 years) and in patients who are at risk of volume depletion, hypotension, and electrolyte imbalances. The use of dapagliflozin in patients with moderate to severe renal impairment is not recommended by the Committee for Medicinal Products for Human Use.31
Conclusion
As our understanding of the pathophysiology of type 2 diabetes evolves, new concepts will emerge with new potential treatment modalities. Optimal management of type 2 diabetes requires a multifaceted approach targeting multiple aspects of glucose homeostasis. SGLT2 inhibitors have an insulin-independent action, are efficacious, promote weight loss, have a low incidence of hypoglycemia, complement the action of other antidiabetic agents, and can be used regardless of duration of diabetes. In this era of obesity, an oral medication promoting weight loss would be a welcome addition to the diabetes armamentarium. However, due to the side effects of repeated urinary tract infections, genital infections, increased hematocrit, and decreased blood pressure, patient selection appears to be important. Physicians may need to be careful when initiating this drug in the elderly, in patients with impaired kidney function, and in those with high cardiovascular and/or cancer risk. If initiated in such groups, close monitoring would be required to prevent any serious adverse events.
Results of ongoing clinical studies of the effect of SGLT2 inhibitors on microvascular and macrovascular complications and on cardiovascular safety are still needed. Clinical research also remains to be carried out on the long-term effects of glucosuria and other potential effects of SGLT2 inhibitors, especially in view of the observed increase in incidence of bladder and breast cancer. Nonetheless, these compounds represent a very promising approach for the treatment of diabetes.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.American Diabetes Association. Diabetes Statistics. Data from the 2011 National Diabetes Fact Sheet. [Accessed May 30, 2012]. Available from: http://www.diabetes.org/diabetes-basics/diabetes-statistics/
- 2.Singh S, Loke YK, Furberg CD. Long-term risk of cardiovascular events with rosiglitazone: a meta-analysis. JAMA. 2007;298(10):1189–1195. doi: 10.1001/jama.298.10.1189. [DOI] [PubMed] [Google Scholar]
- 3.Hummel CS, Lu C, Loo DD, Hirayama BA, Voss AA, Wright EM. Glucose transport by human renal Na+/D-glucose cotransporters SGLT1 and SGLT2. Am J Physiol Cell Physiol. 2011;300(1):C14–C21. doi: 10.1152/ajpcell.00388.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sabino-Silva R, Mori RC, David-Silva A, Okamoto MM, Freitas HS, Machado UF. The Na (+)/glucose cotransporters: from genes to therapy. Braz J Med Biol Res. 2010;43(11):1019–1026. doi: 10.1590/s0100-879x2010007500115. [DOI] [PubMed] [Google Scholar]
- 5.Wright EM. Renal Na (+)-glucose cotransporters. Am J Physiol Renal Physiol. 2001;280(1):F10–F18. doi: 10.1152/ajprenal.2001.280.1.F10. [DOI] [PubMed] [Google Scholar]
- 6.Santer R, Calado J. Familial renal glucosuria and SGLT2: from a Mendelian trait to a therapeutic target. Clin J Am Soc Nephrol. 2010;5(1):133–141. doi: 10.2215/CJN.04010609. [DOI] [PubMed] [Google Scholar]
- 7.Santer R, Kinner M, Lassen CL, et al. Molecular analysis of the SGLT2 gene in patients with renal glucosuria. J Am Soc Nephrol. 2003;14(11):2873–2882. doi: 10.1097/01.asn.0000092790.89332.d2. [DOI] [PubMed] [Google Scholar]
- 8.Wright EM, Hirayama BA, Loo DF. Active sugar transport in health and disease. J Intern Med. 2007;261(1):32–43. doi: 10.1111/j.1365-2796.2006.01746.x. [DOI] [PubMed] [Google Scholar]
- 9.Tabatabai NM, Sharma M, Blumenthal SS, Petering DH. Enhanced expressions of sodium-glucose cotransporters in the kidneys of diabetic Zucker rats. Diabetes Res Clin Pract. 2009;83(1):e27–e30. doi: 10.1016/j.diabres.2008.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rahmoune H, Thompson PW, Ward JM, Smith CD, Hong G, Brown J. Glucose transporters in human renal proximal tubular cells isolated from the urine of patients with non-insulin-dependent diabetes. Diabetes. 2005;54(12):3427–3434. doi: 10.2337/diabetes.54.12.3427. [DOI] [PubMed] [Google Scholar]
- 11.Ehrenkranz JR, Lewis NG, Kahn CR, Roth J. Phlorizin: a review. Diabetes Metab Res Rev. 2005;21(1):31–38. doi: 10.1002/dmrr.532. [DOI] [PubMed] [Google Scholar]
- 12.Najafian M, Jahromi MZ, Nowroznejhad MJ, et al. Phloridzin reduces blood glucose levels and improves lipids metabolism in streptozotocin-induced diabetic rats. Mol Biol Rep. 2012;39(5):5299–5306. doi: 10.1007/s11033-011-1328-7. [DOI] [PubMed] [Google Scholar]
- 13.Katsuno K, Fujimori Y, Takemura Y, et al. Sergliflozin, a novel selective inhibitor of low-affinity sodium glucose cotransporter (SGLT2), validates the critical role of SGLT2 in renal glucose reabsorption and modulates plasma glucose level. J Pharmacol Exp Ther. 2007;320(1):323–330. doi: 10.1124/jpet.106.110296. [DOI] [PubMed] [Google Scholar]
- 14.Dobbins RL, O’Connor-Semmes R, Kapur A, et al. Remogliflozin etabonate, a selective inhibitor of the sodium-dependent transporter 2 reduces serum glucose in type 2 diabetes mellitus patients. Diabetes Obes Metab. 2012;14(1):15–22. doi: 10.1111/j.1463-1326.2011.01462.x. [DOI] [PubMed] [Google Scholar]
- 15.Komoroski B, Vachharajani N, Boulton D, et al. Dapagliflozin, a novel SGLT2 inhibitor, induces dose-dependent glucosuria in healthy subjects. Clin Pharmacol Ther. 2009;85(5):520–526. doi: 10.1038/clpt.2008.251. [DOI] [PubMed] [Google Scholar]
- 16.Kasichayanula S, Chang M, Hasegawa M, et al. Pharmacokinetics and pharmacodynamics of dapagliflozin, a novel selective inhibitor of sodium- glucose co-transporter type 2, in Japanese subjects without and with type 2 diabetes mellitus. Diabetes Obes Metab. 2011;13(4):357–365. doi: 10.1111/j.1463-1326.2011.01359.x. [DOI] [PubMed] [Google Scholar]
- 17.Kasichayanula S, Liu X, Zhang W, et al. Effect of a high-fat meal on the pharmacokinetics of dapagliflozin, a selective SGLT2 inhibitor, in healthy subjects. Diabetes Obes Metab. 2011;13(8):770–773. doi: 10.1111/j.1463-1326.2011.01397.x. [DOI] [PubMed] [Google Scholar]
- 18.Komoroski B, Vachharajani N, Feng Y, Li L, Kornhauser D, Pfister M. Dapagliflozin, a novel, selective SGLT2 inhibitor, improved glycemic control over 2 weeks in patients with type 2 diabetes mellitus. Clin Pharmacol Ther. 2009;85(5):513–519. doi: 10.1038/clpt.2008.250. [DOI] [PubMed] [Google Scholar]
- 19.List JF, Woo V, Morales E, Tang W, Fiedorek FT. Sodium-glucose cotransport inhibition with dapagliflozin in type 2 diabetes. Diabetes Care. 2009;32(4):650–657. doi: 10.2337/dc08-1863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ferrannini E, Ramos SJ, Salsali A, Tang W, List JF. Dapagliflozin monotherapy in type 2 diabetic patients with inadequate glycemic control by diet and exercise: a randomized, double-blind, placebo-controlled, Phase 3 trial. Diabetes Care. 2010;33(10):2217–2224. doi: 10.2337/dc10-0612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bailey CJ, Gross JL, Pieters A, Bastien A, List JF. Effect of dapagliflozin in patients with type 2 diabetes who have inadequate glycaemic control with metformin: a randomised, double-blind, placebo-controlled trial. Lancet. 2010;375(9733):2223–2233. doi: 10.1016/S0140-6736(10)60407-2. [DOI] [PubMed] [Google Scholar]
- 22.Bolinder J, Ljunggren O, Kullberg J, et al. Effects of dapagliflozin on body weight, total fat mass, and regional adipose tissue distribution in patients with type 2 diabetes mellitus with inadequate glycemic control on metformin. J Clin Endocrinol Metab. 2012;97(3):20–31. doi: 10.1210/jc.2011-2260. http://jcem.endojournals.org/ [DOI] [PubMed] [Google Scholar]
- 23.Nauck MA, Del Prato S, Meier JJ, et al. Dapagliflozin versus glipizide as add-on therapy in patients with type 2 diabetes who have inadequate glycemic control with metformin: a randomized, 52-week, double-blind, active-controlled noninferiority trial. Diabetes Care. 2011;34(9):2015–2022. doi: 10.2337/dc11-0606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Strojek K, Yoon KH, Hruba V, Elze M, Langkilde AM, Parikh S. Effect of dapagliflozin in patients with type 2 diabetes who have inadequate glycaemic control with glimepiride: a randomized, 24-week, double-blind, placebo-controlled trial. Diabetes Obes Metab. 2011;13(10):928–938. doi: 10.1111/j.1463-1326.2011.01434.x. [DOI] [PubMed] [Google Scholar]
- 25.Wilding JP, Norwood P, T’joen C, Bastien A, List JF, Fiedorek FT. A study of dapagliflozin in patients with type 2 diabetes receiving high doses of insulin plus insulin sensitizers: applicability of a novel insulin-independent treatment. Diabetes Care. 2009;32(9):1656–1662. doi: 10.2337/dc09-0517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhang L, Feng Y, List J, Kasichayanula S, Pfister M. Dapagliflozin treatment in patients with different stages of type 2 diabetes mellitus: effects on glycaemic control and body weight. Diabetes Obes Metab. 2010;12(6):510–516. doi: 10.1111/j.1463-1326.2010.01216.x. [DOI] [PubMed] [Google Scholar]
- 27.Wilding JP, Woo V, Soler NG, et al. Long-term efficacy of dapagliflozin in patients with type 2 diabetes mellitus receiving high doses of insulin: a randomized trial. Ann Intern Med. 2012;156(6):405–415. doi: 10.7326/0003-4819-156-6-201203200-00003. [DOI] [PubMed] [Google Scholar]
- 28.Henry RR, Murray AV, Marmolejo MH, Hennicken D, Ptaszynska A, List JF. Dapagliflozin, metformin XR, or both: initial pharmacotherapy for type 2 diabetes, a randomised controlled trial. Int J Clin Pract. 2012;66(5):446–456. doi: 10.1111/j.1742-1241.2012.02911.x. [DOI] [PubMed] [Google Scholar]
- 29.Carlson GF, Tou CK, Parikh S, Birmingham BK, Butler K. Evaluation of the effect of dapagliflozin on cardiac repolarization: a thorough QT/QTc study. Diabetes Ther. 2011;2(3):123–132. doi: 10.1007/s13300-011-0003-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kasichayanula S, Liu X, Zhang W, Pfister M, LaCreta FP, Boulton DW. Influence of hepatic impairment on the pharmacokinetics and safety profile of dapagliflozin: an open-label, parallel-group, single-dose study. Clin Ther. 2011;33(11):1798–1808. doi: 10.1016/j.clinthera.2011.09.011. [DOI] [PubMed] [Google Scholar]
- 31.European Medicine’s Agency. Summary of opinion: Forziga. [Accessed May 30, 2012]. Available from: http://www.ema.europa.eu/docs/en_GB/document_library/Summary_of_opinion_-_Initial_authorisation/human/002322/WC500125684.pdf.
- 32.Kasichayanula S, Chang M, Liu X, et al. Lack of pharmacokinetic interactions between dapagliflozin and simvastatin, valsartan, warfarin, or digoxin. Adv Ther. 2012;29(2):163–177. doi: 10.1007/s12325-011-0098-x. [DOI] [PubMed] [Google Scholar]
- 33.Kasichayanula S, Liu X, Shyu WC, et al. Lack of pharmacokinetic interaction between dapagliflozin, a novel sodium-glucose transporter 2 inhibitor, and metformin, pioglitazone, glimepiride or sitagliptin in healthy subjects. Diabetes Obes Metab. 2011;13(1):47–54. doi: 10.1111/j.1463-1326.2010.01314.x. [DOI] [PubMed] [Google Scholar]
- 34.Jones D. Diabetes field cautiously upbeat despite possible setback for leading SGLT2 inhibitor. Nat Rev Drug Discov. 2011;10(9):645–646. doi: 10.1038/nrd3546. [DOI] [PubMed] [Google Scholar]
- 35.United States Food and Drug Administration. FDA briefing document: NDA 202293 dapagliflozin tablets, 5 and 10 mg sponsor: Bristol-Myers Squibb. [Accessed May 30, 2012]. Available from: http://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/drugs/EndocrinologicandMetabolicDrugsAdvisoryCommittee/ucm262994.pdf.
- 36.Sha S, Devineni D, Ghosh A, et al. Canagliflozin, a novel inhibitor of sodium glucose co-transporter 2, dose dependently reduces calculated renal threshold for glucose excretion and increases urinary glucose excretion in healthy subjects. Diabetes Obes Metab. 2011;13(7):669–672. doi: 10.1111/j.1463-1326.2011.01406.x. [DOI] [PubMed] [Google Scholar]
- 37.Devineni D, Morrow L, Hompesch M, et al. Canagliflozin improves glycaemic control over 28 days in subjects with type 2 diabetes not optimally controlled on insulin. Diabetes Obes Metab. 2012;14(6):539–545. doi: 10.1111/j.1463-1326.2012.01558.x. [DOI] [PubMed] [Google Scholar]
- 38.Rosenstock J, Aggarwal N, Polidori D, et al. Dose-ranging effects of canagliflozin, a sodium-glucose cotransporter 2 inhibitor, as add-on to metformin in subjects with type 2 diabetes. Diabetes Care. 2012;35(6):1232–1238. doi: 10.2337/dc11-1926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Veltkamp SA, Kadokura T, Krauwinkel WJ, Smulders RA. Effect of ipragliflozin (ASP1941), a novel selective sodium-dependent glucose co-transporter 2 inhibitor, on urinary glucose excretion in healthy subjects. Clin Drug Investig. 2011;31(12):839–851. doi: 10.1007/BF03256922. [DOI] [PubMed] [Google Scholar]
- 40.Schwartz SL, Akinlade B, Klasen S, Kowalski D, Zhang W, Wilpshaar W. Safety, pharmacokinetic, and pharmacodynamic profiles of ipragliflozin (ASP1941), a novel and selective inhibitor of sodium-dependent glucose co-transporter 2, in patients with type 2 diabetes mellitus. Diabetes Technol Ther. 2011;13(12):1219–1227. doi: 10.1089/dia.2011.0012. [DOI] [PubMed] [Google Scholar]
- 41.Grempler R, Thomas L, Eckhardt M, et al. Empagliflozin, a novel selective sodium glucose cotransporter-2 (SGLT-2) inhibitor: characterisation and comparison with other SGLT-2 inhibitors. Diabetes Obes Metab. 2012;14(1):83–90. doi: 10.1111/j.1463-1326.2011.01517.x. [DOI] [PubMed] [Google Scholar]
- 42.Thomas L, Grempler R, Eckhardt M, et al. Long-term treatment with empagliflozin, a novel, potent and selective SGLT-2 inhibitor, improves glycaemic control and features of metabolic syndrome in diabetic rats. Diabetes Obes Metab. 2012;14(1):94–96. doi: 10.1111/j.1463-1326.2011.01518.x. [DOI] [PubMed] [Google Scholar]
- 43.Suzuki M, Honda K, Fukazawa M, et al. Tofogliflozin, a potent and highly specific sodium/glucose cotransporter 2 inhibitor, improves glycemic control in diabetic rats and mice. J Pharmacol Exp Ther. 2012;341(3):692–701. doi: 10.1124/jpet.112.191593. [DOI] [PubMed] [Google Scholar]
- 44.Nair S, Wilding JP. Sodium glucose co transporter 2 inhibitors as a new treatment for diabetes mellitus. J Clin Endocrinol Metab. 2010;95(1):34–42. doi: 10.1210/jc.2009-0473. http://jcem.endojournals.org/ [DOI] [PubMed] [Google Scholar]