Summary
Background
Statins reduce LDL cholesterol and prevent vascular events, but their net effects in people at low risk of vascular events remain uncertain.
Methods
This meta-analysis included individual participant data from 22 trials of statin versus control (n=134 537; mean LDL cholesterol difference 1·08 mmol/L; median follow-up 4·8 years) and five trials of more versus less statin (n=39 612; difference 0·51 mmol/L; 5·1 years). Major vascular events were major coronary events (ie, non-fatal myocardial infarction or coronary death), strokes, or coronary revascularisations. Participants were separated into five categories of baseline 5-year major vascular event risk on control therapy (no statin or low-intensity statin) (<5%, ≥5% to <10%, ≥10% to <20%, ≥20% to <30%, ≥30%); in each, the rate ratio (RR) per 1·0 mmol/L LDL cholesterol reduction was estimated.
Findings
Reduction of LDL cholesterol with a statin reduced the risk of major vascular events (RR 0·79, 95% CI 0·77–0·81, per 1·0 mmol/L reduction), largely irrespective of age, sex, baseline LDL cholesterol or previous vascular disease, and of vascular and all-cause mortality. The proportional reduction in major vascular events was at least as big in the two lowest risk categories as in the higher risk categories (RR per 1·0 mmol/L reduction from lowest to highest risk: 0·62 [99% CI 0·47–0·81], 0·69 [99% CI 0·60–0·79], 0·79 [99% CI 0·74–0·85], 0·81 [99% CI 0·77–0·86], and 0·79 [99% CI 0·74–0·84]; trend p=0·04), which reflected significant reductions in these two lowest risk categories in major coronary events (RR 0·57, 99% CI 0·36–0·89, p=0·0012, and 0·61, 99% CI 0·50–0·74, p<0·0001) and in coronary revascularisations (RR 0·52, 99% CI 0·35–0·75, and 0·63, 99% CI 0·51–0·79; both p<0·0001). For stroke, the reduction in risk in participants with 5-year risk of major vascular events lower than 10% (RR per 1·0 mmol/L LDL cholesterol reduction 0·76, 99% CI 0·61–0·95, p=0·0012) was also similar to that seen in higher risk categories (trend p=0·3). In participants without a history of vascular disease, statins reduced the risks of vascular (RR per 1·0 mmol/L LDL cholesterol reduction 0·85, 95% CI 0·77–0·95) and all-cause mortality (RR 0·91, 95% CI 0·85–0·97), and the proportional reductions were similar by baseline risk. There was no evidence that reduction of LDL cholesterol with a statin increased cancer incidence (RR per 1·0 mmol/L LDL cholesterol reduction 1·00, 95% CI 0·96–1·04), cancer mortality (RR 0·99, 95% CI 0·93–1·06), or other non-vascular mortality.
Interpretation
In individuals with 5-year risk of major vascular events lower than 10%, each 1 mmol/L reduction in LDL cholesterol produced an absolute reduction in major vascular events of about 11 per 1000 over 5 years. This benefit greatly exceeds any known hazards of statin therapy. Under present guidelines, such individuals would not typically be regarded as suitable for LDL-lowering statin therapy. The present report suggests, therefore, that these guidelines might need to be reconsidered.
Funding
British Heart Foundation; UK Medical Research Council; Cancer Research UK; European Community Biomed Programme; Australian National Health and Medical Research Council; National Heart Foundation, Australia.
Introduction
The Cholesterol Treatment Trialists' (CTT) Collaboration previously reported meta-analyses of individual data from 170 000 individuals in 21 trials of standard statin regimens versus control and five trials of more intensive versus less intensive regimens.1 That report showed that lowering of LDL cholesterol by 1 mmol/L with a standard statin regimen reduced the incidence of major vascular events (defined as non-fatal myocardial infarction or coronary death, any stroke, or coronary revascularisation procedure) by around a fifth, and that further reductions in LDL cholesterol with more intensive statin regimens yielded further reductions in risk. There was no evidence that lowering of LDL cholesterol increased the risk of non-vascular death or of cancer, even in participants with baseline LDL cholesterol less than 2 mmol/L (in whom LDL cholesterol was reduced from about 1·7 mmol/L [65 mg/dL] to 1·3 mmol/L [50 mg/dL]).2
In those analyses, reduction of LDL cholesterol with a statin in participants with no previous history of vascular disease reduced the risk of major vascular events by about a fifth,1 but there remains uncertainty about whether statin therapy is of overall net benefit in primary prevention.3–5 This question is important because, although individuals without previous vascular disease are at lower absolute risk, at least half of all vascular events occur among them.6 The availability of individual participant data from each trial within the CTT database (allowing the inclusion of information from both primary prevention trials and low-risk participants in other trials) allows a more complete assessment of the effects of lowering of LDL cholesterol in low-risk people than was possible in previous meta-analyses of published data.3,4
Methods
Trials
The methods of the CTT collaboration have been described in detail elsewhere.1,7,8 In the present analyses, a trial was eligible if it reported by the end of 2009 and provided data before June, 2011, and met three criteria: (1) it included at least one intervention whose main effect was to lower LDL cholesterol concentration; (2) it was unconfounded with respect to this intervention (ie, no other differences in risk factor modification between the treatment groups were intended); and (3) it recruited at least 1000 participants with scheduled treatment duration of at least 2 years. The main outcomes of interest were major vascular events, major coronary events (defined as non-fatal myocardial infarction or coronary death), stroke (subdivided by type), coronary revascularisation procedures, cancers, and cause-specific mortality.
Statistical analysis
Two different Cox proportional hazards models were developed to allow risk to be modelled separately in trials of statin versus control (22 trials; model 1) and in trials of more versus less intensive statin regimens (five trials; model 2). Both models incorporated terms derived from characteristics measured at the time of randomisation, terms that modelled average differences in risk between trials (as well as within specific periods of time within each trial), and interaction terms (appendix pp 1–2). On the basis of these risk prediction models, participants in both treatment groups of each study were assigned to one of five baseline categories of 5-year risk of a major vascular event: <5%; ≥5% to <10%; ≥10% to <20%; ≥20% to <30%; or ≥30%. Further details of model development are shown in the appendix pp 15–16.
Analyses included all participants who were randomly assigned to treatment groups, irrespective of whether they received their allocated treatment (ie, intention-to-treat). Analyses of the effects on disease rates within each trial are derived from the logrank (o–e) statistic and its variance (v) for first events. Meta-analyses were weighted by the absolute LDL cholesterol difference in that trial at 1 year (d mmol/L), and are reported as effects per 1·0 mmol/L reduction in LDL cholesterol. In a meta-analysis of several trials, the log of the rate ratio (RR) per 1·0 mmol/L was calculated as S/V with variance 1/V (and hence, for example, with 95% CI of S/V±1·96/√V), where S is the sum over all trials of d(o–e) and V is the sum over all trials of d2v. For most subgroup analyses, the weight for a particular subgroup was the LDL cholesterol difference observed in the whole trial, but analyses by baseline LDL cholesterol concentration used LDL weights specific to a particular subgroup of a particular trial.1 In trials comparing more versus less intensive statin therapy, the relevant baseline lipid values were those achieved on the less intensive regimen. In three of these trials,9–11 however, any statin therapy was stopped before randomisation, so we estimated their relevant baseline values by multiplying the values at the randomisation visit (ie, off statin treatment) by the mean proportional reduction observed at 1 year in participants allocated the less intensive regimen.1 Proportional risk reductions in different subgroups were compared by standard χ2 tests for heterogeneity or, where appropriate, trend. To allow for multiple testing by subdivisions, only overall summary rate ratios have 95% CIs; all other rate ratios have 99% CIs. Analyses used SAS version 9.1 (SAS Institute, Cary, NC, USA), Stata version 11.2 (StataCorp, TX, USA), and R version 2.11.1.
Role of the funding sources
The funding sources had no involvement in the study design, data collection, analysis and interpretation, the writing of the report, or the decision to submit for publication. The writing committee had full access to all data and accepts full responsibility for the content of this report.
Results
Individual participant data were available from 27 trials in 174 149 participants. 22 trials compared a standard statin regimen versus control (134 537 participants; mean baseline LDL cholesterol 3·70 [SD 0·7] mmol/L; mean difference at 1 year 1·08 mmol/L; median follow-up duration in survivors 4·8 years)12–33 and five trials assessed a more intensive versus a less intensive statin regimen (39 612 participants; mean baseline LDL cholesterol 2·53 [SD 0·6] mmol/L; mean difference at 1 year 0·51 mmol/L; median follow-up duration in survivors 5·1 years).9–11,34,35 Individual participant data were unavailable from only two eligible trials in 6331 higher-risk patients with pre-existing vascular disease (SPARCL36 and GREACE37).
The baseline prognostic factors that were strong predictors of major vascular event risk (ie, at the 1% significance level) were broadly similar in the trials of statin versus control and the trials of more versus less intensive statin regimens (appendix pp 1–2). Predicted risk compared well with observed risk for each trial, as well as within each 5-year risk group (appendix p 3). When trials were ordered by their median 5-year predicted risk of a major vascular event, the five trials with the lowest median predicted risks (all <10%) were primary prevention trials (table 1).13,15,22,29,31 By contrast, almost all participants with predicted 5-year risk of 20% or higher were recruited into trials in patients with a definite history of vascular disease.12,14,16–19,25,28 The predicted 5-year risk of a major vascular event was also 20% or higher in most dialysis patients.26,30 In two trials in patients with heart failure,32,33 there was a high risk of sudden death, but such deaths were categorised differently, with a much smaller proportion of such deaths thought to be due to coronary occlusion in the GISSI-HF trial33 than in CORONA;32 this difference is the main reason why the predicted 5-year risk of major vascular events was more than twice as high in CORONA (23%) as in GISSI-HF (10%).
Table 1.
Numbers of participants and number of first major vascular events (MVEs) in each study contributing to vascular disease risk categories
| Median predicted 5-year MVE risk |
Estimated 5-year MVE risk |
Total | |||||
|---|---|---|---|---|---|---|---|
| <5% | ≥5% to <10% | ≥10% to <20%* | ≥20% to <30% | ≥30% | |||
| Statin vs control | |||||||
| MEGA† | 2·7% | 7247 (147) | 925 (91) | 42 (4) | 0 (0) | 0 (0) | 8214 (242) |
| JUPITER | 4·4% | 11 212 (118) | 6117 (162) | 472 (19) | 1 (0) | 0 (0) | 17 802 (299) |
| AFCAPS/TexCAPS | 5·2% | 2944 (72) | 3329 (225) | 331 (47) | 1 (0) | 0 (0) | 6605 (344) |
| ASCOT-LLA | 8·1% | 1505 (25) | 5383 (229) | 3168 (245) | 234 (22) | 15 (3) | 10 305 (524) |
| WOSCOPS | 9·2% | 34 (0) | 3848 (219) | 2576 (293) | 134 (36) | 3 (2) | 6595 (550) |
| GISSI-HF | 9·6% | 875 (34) | 1523 (78) | 1789 (171) | 357 (52) | 30 (11) | 4574 (346) |
| ALERT | 10·2% | 286 (8) | 740 (54) | 705 (105) | 237 (59) | 134 (49) | 2102 (275) |
| CARDS | 10·9% | 156 (0) | 1043 (43) | 1524 (144) | 109 (16) | 6 (1) | 2838 (204) |
| ASPEN | 13·6% | 108 (0) | 648 (13) | 980 (99) | 517 (90) | 157 (48) | 2410 (250) |
| ALLHAT-LLT | 14·0% | 92 (2) | 2331 (144) | 5468 (803) | 1871 (438) | 593 (183) | 10 355 (1570) |
| Post-CABG | 17·0% | 0 (0) | 24 (2) | 1022 (128) | 279 (44) | 26 (5) | 1351 (179) |
| GISSI-P | 18·3% | 0 (0) | 14 (1) | 2816 (272) | 1268 (140) | 173 (26) | 4271 (439) |
| HPS | 18·6% | 320 (14) | 2041 (134) | 9424 (1267) | 6722 (1488) | 2029 (651) | 20 536 (3554) |
| LIPID | 22·1% | 0 (0) | 27 (3) | 2946 (484) | 5144 (1278) | 897 (324) | 9014 (2089) |
| PROSPER | 22·4% | 0 (0) | 108 (13) | 2208 (224) | 1858 (293) | 1630 (396) | 5804 (926) |
| CORONA | 23·2% | 11 (1) | 194 (16) | 1463 (144) | 2151 (292) | 1192 (177) | 5011 (630) |
| CARE | 26·1% | 0 (0) | 0 (0) | 362 (58) | 2776 (615) | 1021 (313) | 4159 (986) |
| ALLIANCE | 26·3% | 0 (0) | 0 (0) | 288 (46) | 1419 (298) | 735 (203) | 2442 (547) |
| LIPS | 29·5% | 0 (0) | 0 (0) | 118 (28) | 770 (158) | 789 (173) | 1677 (359) |
| AURORA | 31·7% | 0 (0) | 61 (8) | 546 (85) | 676 (136) | 1490 (501) | 2773 (730) |
| SSSS | 33·1% | 0 (0) | 0 (0) | 139 (13) | 1159 (275) | 3146 (1063) | 4444 (1351) |
| 4D | 38·2% | 0 (0) | 6 (1) | 117 (20) | 273 (52) | 859 (233) | 1255 (306) |
| Subtotal, 22 trials | 13·7% | 24 790 (421) | 28 362 (1436) | 38 504 (4699) | 27 956 (5782) | 14 925 (4362) | 134 537 (16 700) |
| More vs less statin | |||||||
| SEARCH | 16·2% | .. | .. | 9665 (1969) | 2157 (680) | 242 (104) | 12 064 (2753) |
| A to Z | 17·3% | .. | .. | 3097 (307) | 1191 (180) | 209 (52) | 4497 (539) |
| TNT | 21·8% | .. | .. | 3507 (520) | 5078 (1075) | 1416 (458) | 10 001 (2053) |
| IDEAL | 24·1% | .. | .. | 1754 (326) | 5257 (1125) | 1877 (593) | 8888 (2044) |
| PROVE-IT | 33·8% | .. | .. | 27 (3) | 1125 (185) | 3010 (676) | 4162 (864) |
| Subtotal, five trials | 20·8% | .. | .. | 18 050 (3125) | 14 808 (3245) | 6754 (1883) | 39 612 (8253) |
Data are median risk or number of participants (number of first major vascular events). Studies are shown in order of increasing median predicted 5-year MVE risk. The predicted risk for the trials of more versus less statin is that under the less intensive statin regimen. We imputed missing data for age, sex, treatment for hypertension, lipids, and blood pressure at baseline for the purpose of predicting 5-year MVE risk and for risk stratification. MEGA=Management of Elevated Cholesterol in the Primary Prevention Group of Adult Japanese. JUPITER=Justification for the Use of Statins in Prevention: an Intervention Trial Evaluating Rosuvastatin. AFCAPS/TexCAPS=Air Force/Texas Coronary Atherosclerosis Prevention Study. ASCOT-LLA=Anglo-Scandinavian Cardiac Outcomes Trial-Lipid Lowering Arm. WOSCOPS=West of Scotland Coronary Prevention Study. GISSI-HF=Gruppo Italiano per lo Studio della Sopravvivenza nell'Insufficienza cardiaca. ALERT=Assessment of Lescol in Renal Transplantation. CARDS=Collaborative Atorvastatin Diabetes Study. ASPEN=Atorvastatin Study for Prevention of Coronary Heart Disease Endpoints in Non-Insulin-Dependent Diabetes Mellitus. ALLHAT-LLT=Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial. Post-CABG=Post-Coronary Artery Bypass Graft. GISSI-P=Gruppo Italiano per lo Studio della Sopravvivenza nell'Infarto Miocardico. HPS=Heart Protection Study. LIPID=Long-term Intervention with Pravastatin in Ischaemic Disease. PROSPER=PROspective Study of Pravastatin in the Elderly at Risk. CORONA=Controlled Rosuvastatin Multinational Trial in Heart Failure. CARE=Cholesterol And Recurrent Events. ALLIANCE=Aggressive Lipid-Lowering Initiation Abates New Cardiac Events. LIPS=Lescol Intervention Prevention Study. AURORA=A Study to Evaluate the Use of Rosuvastatin in Subjects on Regular Hemodialysis: an Assessment of Survival and Cardiovascular Events. SSSS=Scandinavian Simvastatin Survival Study. 4D=Die Deutsche Diabetes Dialyse Studie. SEARCH=Study of the Effectiveness of Additional Reductions in Cholesterol and Homocysteine. A to Z=Aggrastat to Zocor. TNT=Treating to New Targets. IDEAL=Incremental Decrease in End Points Through Aggressive Lipid Lowering Study Group. PROVE-IT=Pravastatin or Atorvastatin Evaluation and Infection Therapy.
For trials of more versus less statin, this category includes 141 participants (48 [4 MVEs] from A to Z and 93 [11 MVEs] from SEARCH) with an estimated 5-year risk of MVE between 5% and 10%.
Includes 382 patients who were excluded from the original publication.
Among the 22 trials of statin versus control, the observed annual major vascular event rate ranged from 0·6% in the lowest predicted risk category to 9·5% in the highest risk category, whereas in trials of more versus less intensive statin therapy (which were undertaken solely in patients with previous coronary disease) the observed annual event rate varied between 3·7% and 10·7% across the categories studied (table 2). In both sets of trials, the achieved reduction in LDL cholesterol at 1 year with statin therapy or more intensive statin therapy was greater in people with higher predicted 5-year risk of major vascular events (appendix p 4).
Table 2.
Baseline characteristics of participants, by predicted 5-year risk of a major vascular event (MVE)
| Number of participants | Observed annual MVE rate in those allocated control or less statin | Observed annual MCE rate in those allocated control or less statin | Median follow-up in survivors (years)* | Women (%) | Mean age (SD; years) | Baseline LDL cholesterol (mmol/L)* | Diabetes (%) |
Baseline history of vascular disease (%) |
|||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Previous CHD | Other vascular† | None‡ | |||||||||
| Statin vs control | |||||||||||
| <5% | 24 790 | 0·6% | 0·2% | 4·0 | 54% | 59 (8) | 3·43 | 7% | 0% | 4% | 96% |
| ≥5% to <10% | 28 362 | 1·6% | 0·8% | 4·3 | 27% | 61 (9) | 3·68 | 18% | 2% | 11% | 87% |
| ≥10% to <20% | 38 504 | 3·4% | 1·5% | 4·7 | 29% | 64 (9) | 3·61 | 24% | 43% | 22% | 44% |
| ≥20% to <30% | 27 956 | 5·7% | 2·6% | 5·0 | 16% | 65 (9) | 3·72 | 19% | 80% | 28% | 13% |
| ≥30% | 14 925 | 9·5% | 5·1% | 4·9 | 14% | 66 (9) | 3·92 | 44% | 86% | 39% | 7% |
| Subtotal, 22 trials | 134 537 | 3·6% | 1·8% | 4·8 | 29% | 63 (9) | 3·70 | 21% | 39% | 20% | 52% |
| More vs less statin§ | |||||||||||
| ≥10% to <20%¶ | 18 050 | 3·7% | 1·6% | 5·9 | 22% | 60 (10) | 2·37 | 4% | 100% | 1% | 0% |
| ≥20% to <30% | 14 808 | 5·9% | 2·4% | 5·2 | 17% | 62 (9) | 2·59 | 17% | 100% | 12% | 0% |
| ≥30% | 6754 | 10·7% | 4·2% | 2·4 | 18% | 64 (10) | 2·81 | 35% | 100% | 35% | 0% |
| Subtotal, five trials | 39 612 | 5·3% | 2·2% | 5·1 | 19% | 62 (10) | 2·53 | 14% | 100% | 11% | 0% |
CHD=coronary heart disease. MCE=major coronary event.
Estimated using standard Kaplan-Meier methods with participants censored at their date of death; median follow-up and baseline LDL cholesterol for trial subgroups weighted by trial subgroup-specific variances of observed logrank (o–e) for major vascular events.
History of intracerebral bleed, transient ischaemic attack, ischaemic stroke, unknown stroke, peripheral artery disease or heart failure (if known).
No known history of CHD or other vascular disease.
The estimated 5-year major vascular event risk is with the less intensive statin regimen and observed MVE and MCE rates are for participants allocated the less intensive statin regimen; in three more versus less statin trials (A to Z, PROVE-IT, and IDEAL) there was no active run-in period before randomisation and so for the purpose of risk stratification and presentation of results the LDL cholesterol at baseline for the participants in these trials was adjusted for the observed LDL cholesterol reduction from baseline to year 1 in those allocated low intensity statin in the respective trial.
Includes 141 participants (48 [4 MVEs] from A to Z and 93 [11 MVEs] from SEARCH) with an estimated 5-year risk of MVE between 5% and 10%.
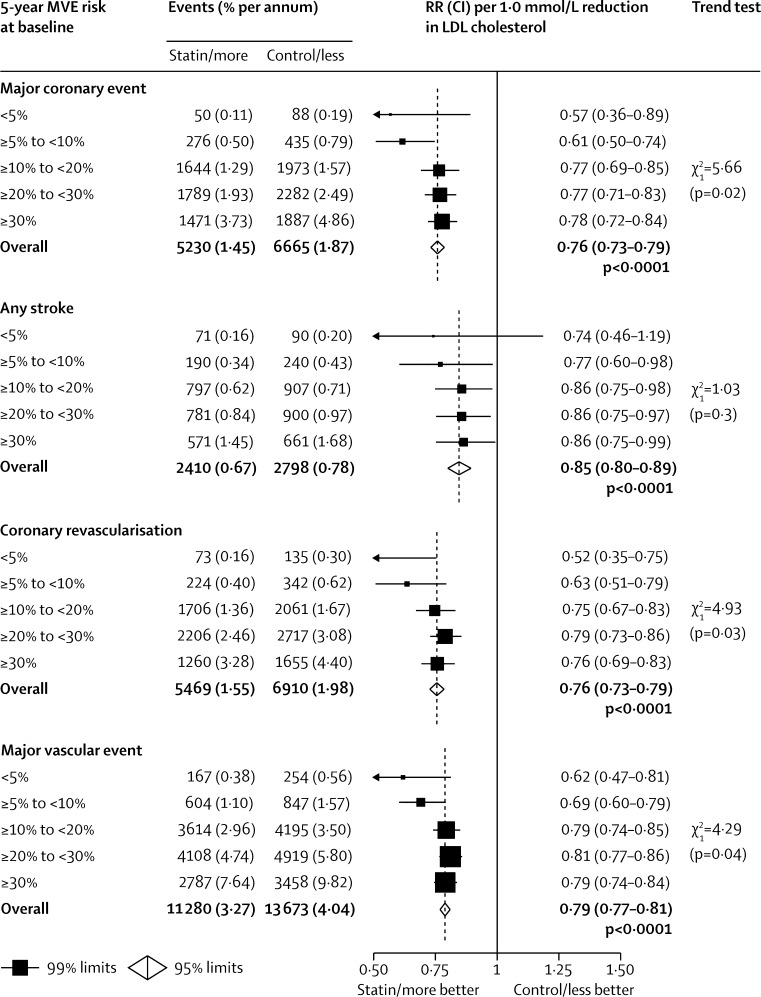
Among all 27 trials, statins reduced the risk of major vascular events by 21% per 1·0 mmol/L LDL cholesterol reduction (RR 0·79, 95% CI 0·77–0·81, p<0·0001), with separately significant proportional reductions in each risk group (figure 1). In particular, there were significant reductions in major vascular event risk in each of the two lowest risk categories (RR per 1·0 mmol/L LDL cholesterol reduction 0·62, 99% CI 0·47–0·81, for 5-year predicted risk <5%, and 0·69, 99% CI 0·60–0·79, for 5-year predicted risk ≥5% to <10%; both p<0·0001; figure 1). These results were qualitatively similar after exclusion of five trials12,15,22,24,31 that ended early on the advice of their data monitoring committees (data not shown). The proportional reductions in major vascular events per 1·0 mmol/L LDL cholesterol reduction in the two lowest risk categories seemed to be at least as large as for other participants (figure 1), even after further stratification by age and sex (appendix p 6) or by baseline LDL cholesterol (appendix p 7).
Figure 1.
Effects on major coronary events, strokes, coronary revascularisation procedures, and major vascular events per 1·0 mmol/L reduction in LDL cholesterol at different levels of risk
MVE=major vascular event. RR=rate ratio. CI=confidence interval.
The reductions in risk of major vascular events among the two categories of participant at lowest risk reflected reductions in major coronary events (RR per 1·0 mmol/L LDL cholesterol reduction 0·57, 99% CI 0·36–0·89, p=0·0012, and 0·61, 99% CI 0·50–0·74, p<0·0001), mainly non-fatal myocardial infarction, and in coronary revascularisations (RR 0·52, 99% CI 0·35–0·75, and 0·63, 99% CI 0·51–0·79; both p<0·0001), that were at least as large as those seen in higher risk participants (trend p=0·02 for major coronary events and p=0·03 for coronary revascularisations; figure 1, appendix p 8). The reduction in stroke risk per 1·0 mmol/L LDL cholesterol reduction (RR 0·85, 95% CI 0·80–0·89) was similar at all levels of baseline major vascular event risk (trend p=0·3; figure 1). In particular, the reduction in stroke risk in those with predicted 5-year major vascular event risk lower than 10% (ie, the two lowest risk groups combined; RR 0·76, 99% CI 0·61–0·95; p=0·0012) was similar to that seen in higher risk categories. The proportional reductions in ischaemic stroke (RR per 1·0 mmol/L LDL cholesterol reduction 0·79, 95% CI 0·74–0·85) and in strokes of unknown cause (RR 0·87, 95% CI 0·79–0·97) were similar irrespective of baseline major vascular event risk, and there was no evidence that the RR for haemorrhagic stroke (1·15, 95% CI 0·97–1·38) varied by baseline risk (appendix p 9). Separate analyses of major vascular events and its components in the trials that tested statin versus control and the trials that tested more versus less intensive statin regimens are shown in the appendix pp 10–11.
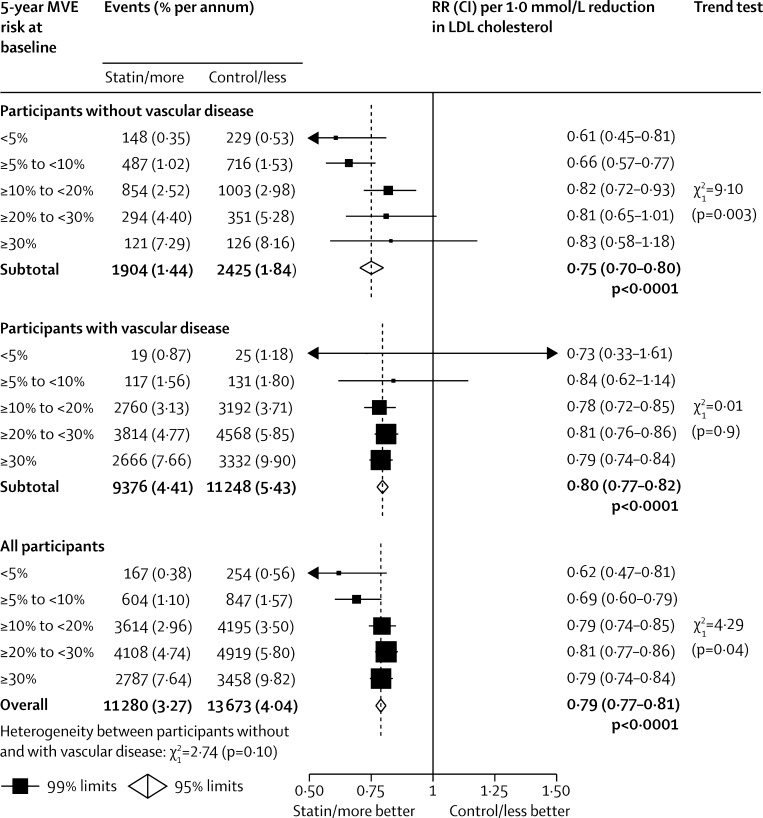
For participants with previous vascular disease, the proportional reductions in major vascular event risk were broadly similar irrespective of predicted risk of these events (figure 2). In participants with no history of vascular disease, the proportional reduction in major vascular events was at least as large in the two lowest risk groups (RR per 1·0 mmol/L LDL reduction 0·61, 99% CI 0·45–0·81, and 0·66, 99% CI 0·57–0·77) as in those at higher risk. Further exclusion from these lowest risk groups of participants with diabetes or chronic kidney disease had little effect on the proportional reductions in major vascular events (RR per 1·0 mmol/L LDL cholesterol reduction 0·63, 99% CI 0·46–0·85, for 5-year predicted risk <5%; 0·64, 99% CI 0·54–0·76, for 5-year predicted risk ≥5% to <10%). The LDL-weighted proportional reduction in major coronary events in participants with no history of vascular disease was also at least as large in the two lowest risk groups as in those at higher risk (appendix p 12).
Figure 2.
Effects on major vascular events per 1·0 mmol/L reduction in LDL cholesterol at different levels of risk, by history of vascular disease
MVE=major vascular event. RR=rate ratio. CI=confidence interval.
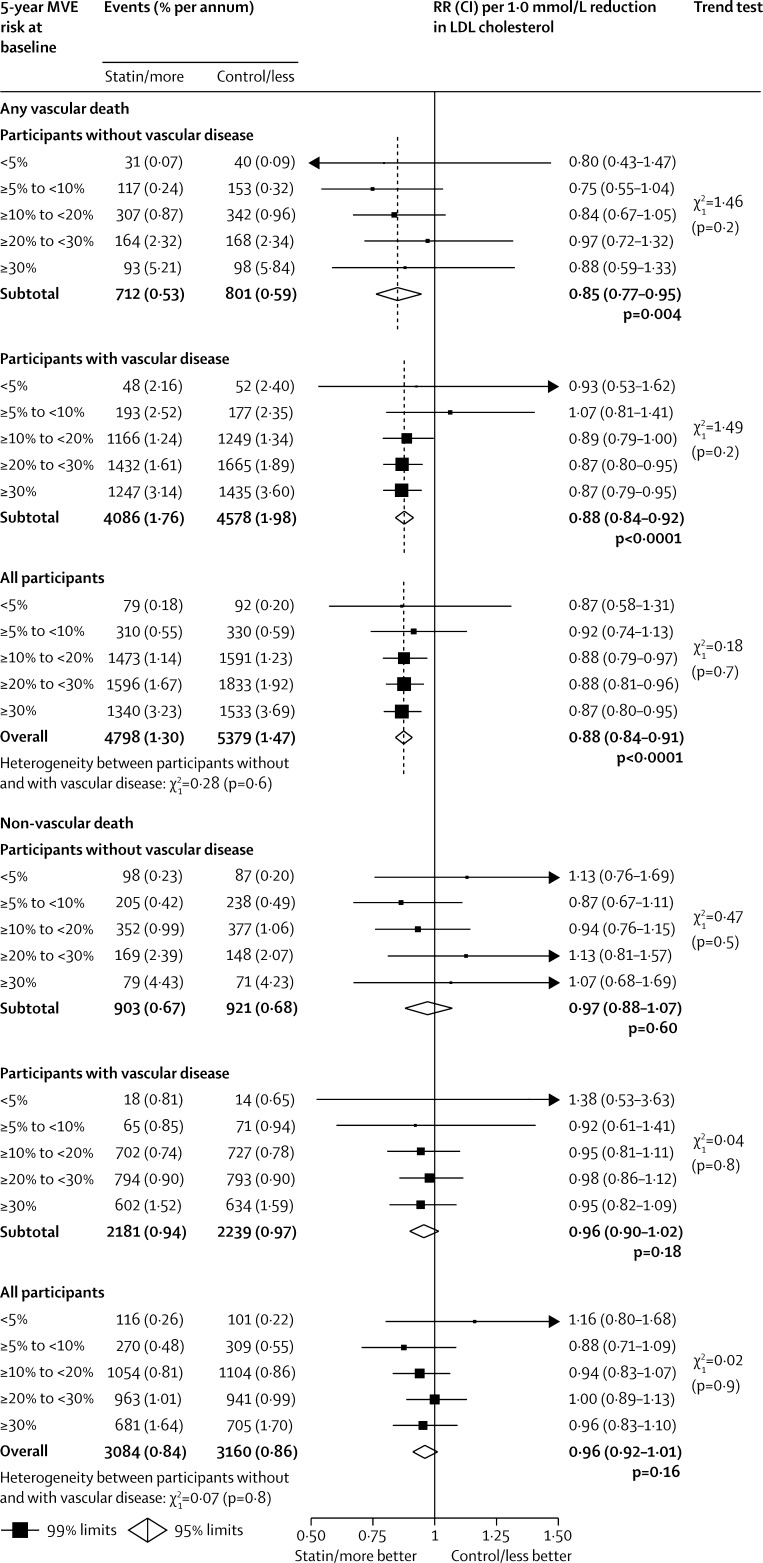
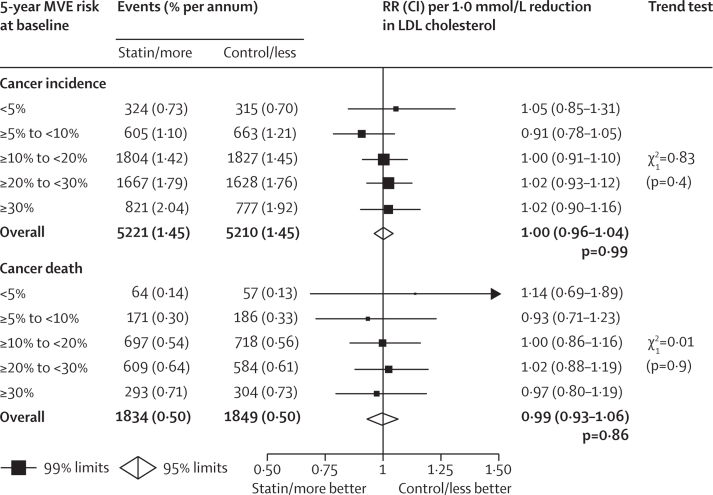
In all participants, there was a proportional reduction in vascular mortality of 12% per 1·0 mmol/L LDL cholesterol reduction (RR 0·88, 95% CI 0·84–0·91; figure 3), which was chiefly attributable to reductions in coronary deaths of 20% (RR 0·80, 95% CI 0·76–0·85) and in other cardiac deaths of 8% (RR 0·92, 95% CI 0·87–0·98; appendix p 13). There were too few deaths among the lower risk participants to allow reliable direct assessment of the effects of statin therapy (appendix p 13). However, the LDL-weighted proportional reductions seemed similar in each risk category both for the aggregate of all vascular deaths (trend p=0·7; figure 3) and for each specific cause of vascular death (all trend p=NS; appendix p 13), and there was no significant trend towards an increase in non-vascular mortality in those at lower risk (trend p=0·9; figure 3). In participants with no history of vascular disease, reduction of LDL cholesterol with statin therapy reduced the risk of vascular mortality (RR per 1·0 mmol/L reduction 0·85, 95% CI 0·77–0·95, p=0·004; figure 3) and, since there was no increase in the risk of non-vascular causes of death (RR 0·97, 95% CI 0·88–1·07; figure 3), reduced the risk of all-cause mortality (RR 0·91, 95% CI 0·85–0·97, p=0·007; appendix p 14). These mortality benefits remained even after further exclusion of participants with diabetes or chronic kidney disease at baseline (vascular death, RR 0·80, 95% CI 0·67–0·95; any death, 0·87, 95% CI 0·78–0·95). There was no evidence of an increase in cancer incidence (RR per 1·0 mmol/L LDL reduction 1·00, 95% CI 0·96–1·04) or of cancer death (RR 0·99, 95% CI 0·93–1·06) at any level of major vascular event risk (figure 4).
Figure 3.
Effects on vascular and non-vascular deaths per 1·0 mmol/L reduction in LDL cholesterol at different levels of risk, by history of vascular disease
MVE=major vascular event. RR=rate ratio. CI=confidence interval. There were a further 179 (statin/more statin) versus 210 (control/less statin) deaths of unknown cause among participants without vascular disease and 309 (statin/more statin) versus 338 (control/less statin) deaths of unknown cause among participants with vascular disease.
Figure 4.
Effects on cancer incidence and cancer mortality per 1·0 mmol/L reduction in LDL cholesterol at different levels of risk
MVE=major vascular event. RR=rate ratio. CI=confidence interval.
Discussion
The most recent CTT meta-analysis of individual participant data from randomised trials showed that lowering of LDL cholesterol with standard statin regimens safely reduced the 5-year incidence of major coronary events, coronary revascularisations, and ischaemic strokes by about one fifth per 1·0 mmol/L reduction in LDL cholesterol, and that additional reductions in LDL cholesterol obtained with more intensive statin regimens further reduced the incidence of these major vascular events.1 The present results show that reduction of LDL cholesterol with statin therapy significantly reduced the risk of major vascular events in individuals with 5-year risk lower than 10% (in whom the mean risks were 2·6% for major coronary events plus 3% for other major vascular events), even in those with no previous history of vascular disease, diabetes, or chronic kidney disease (panel).
Panel. Research in context.
Systematic review
Lowering of LDL cholesterol with a statin reduces the risk of myocardial infarction, coronary death, ischaemic stroke, and coronary revascularisation by about one fifth per 1 mmol/L LDL cholesterol reduction in a wide range of people.1 However, tabular meta-analyses of people at low risk of these events, studied predominantly in primary prevention trials, have concluded that statin therapy might not result in worthwhile net benefit in this group.3,4
Interpretation
Individual participant data in the Cholesterol Treatment Trialists' Collaboration of 27 trials involving 175 000 participants showed that statin therapy reduces the risk of major vascular events (non-fatal myocardial infarction, coronary death, coronary revascularisation, or stroke) in people with 5-year risk of such an event lower than 10% (and, separately, in those at 5-year risk <5%), and in these people each 1·0 mmol/L reduction in LDL cholesterol produces 11 fewer major vascular events per 1000 treated over 5 years, a benefit that greatly exceeds any known hazards of statin therapy.
The estimated absolute reduction in major vascular events in participants with 5-year risk of these events lower than 10% was around 11 per 1000 over 5 years for each 1·0 mmol/L reduction in LDL cholesterol (4·1% statin or more intensive statin regimen vs 5·2% control or less intensive regimen). Modern statin regimens, however, can often reduce LDL cholesterol by more than 1 mmol/L,38,39 which would yield even larger absolute reductions in major vascular events. The avoidance of life-threatening or potentially disabling events in apparently healthy low-risk people might be deemed worthwhile provided that they are not accompanied by any definite hazard that is of comparable severity. Although there was no evidence of any increased risk of death from non-vascular causes or of cancer in those at low risk (which is consistent with previous detailed analyses of the effect of statins on cancer2), several known or potential hazards of statin therapy need to be considered when estimating the net effects of statin therapy in people at lowest risk.
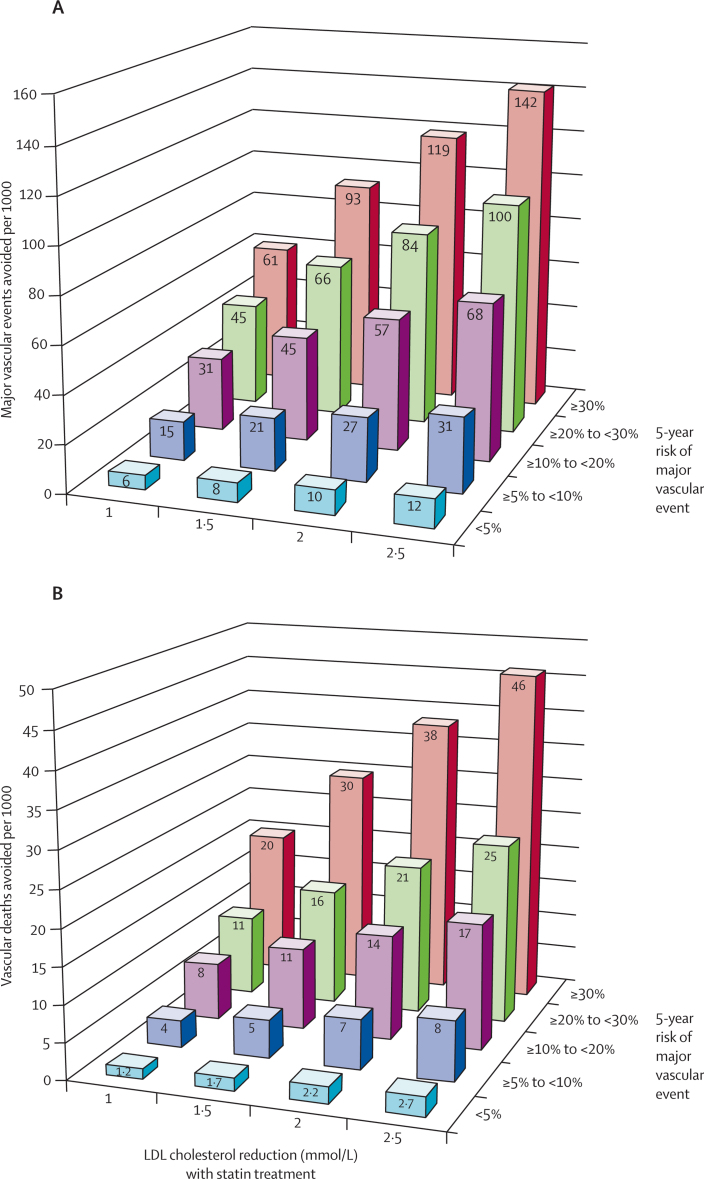
First, statin therapy is associated with a small increased risk of myopathy (excess incidence of about 0·5 per 1000 over 5 years) and, more rarely, of rhabdomyolysis (excess incidence of about 0·1 per 1000 over 5 years).38 The risks of myopathy are dose-related but, with the exception of simvastatin 80 mg daily (or lower doses in Asian populations), intensive statin regimens have not been shown to result in substantial myopathy risks.38 Second, the most recent CTT report raised the possibility that statin therapy might increase the risk of haemorrhagic stroke.1 The present analyses suggest that the annual excess risk of haemorrhagic strokes per 1·0 mmol/L LDL cholesterol reduction might be of the order of 0·5 per 1000 people treated over 5 years (appendix p 9), although it might be higher in populations in which haemorrhagic stroke accounts for a higher proportion of strokes (eg, Asian populations40). But, since statin therapy produced a clear reduction in overall stroke that was independent of predicted risk, such an increase in haemorrhagic stroke risk would typically be outweighed by the reduction in the risk of ischaemic stroke (as well as the reduction in other occlusive vascular events and deaths) even in individuals whose 5-year risk of major vascular events is lower than 5%. Third, recent meta-analyses have suggested that statin therapy might be associated with a proportional increase in the diagnosis of diabetes mellitus of about 10%41 and that more intensive statin therapy produces a bigger increase.42 The observed incidence of diabetes recorded in the primary prevention trials was about 5% over 5 years, so the absolute excess was about 0·1% per year.41 If new diagnoses of diabetes were associated with an immediate doubling in cardiovascular risk43 in individuals with 5-year risk of major vascular events lower than 10%, then the expected effect would be only about 0·2 fewer events avoided per 1000 individuals treated over 5 years. Such an effect is more than 50-times smaller than the absolute benefit observed with statin therapy in such individuals (about 11 fewer major vascular events per 1000 treated over 5 years per 1·0 mmol/L reduction in LDL cholesterol; see figure 5 for absolute benefits corresponding to particular reductions in LDL cholesterol in individuals at different levels of major vascular event risk). Moreover, long-term follow-up of statin trials has shown that the absolute reductions in major vascular events increase while the statin treatment is continued1 and that these benefits persist for at least 5 years after the treatment has stopped, with no evidence of any adverse effects emerging with extended follow-up.44–47 These findings would suggest that any long-term effects of any small excesses in haemorrhagic strokes and in diagnoses of diabetes are not associated with long-term effects on major vascular events that are sufficiently large to outweigh the persistent benefits of statin therapy.
Figure 5.
Predicted 5-year benefits of LDL cholesterol reductions with statin treatment at different levels of risk
(A) Major vascular events and (B) vascular deaths. Lifetable estimates using major vascular event risk or vascular death risk in the respective risk categories and overall treatment effects per 1·0 mmol/L reduction in LDL cholesterol with statin.
The observed event rates shown in the figures for each risk category can be readily compared with risk thresholds used in treatment guidelines. For example, under present guidelines, including those of the Adult Treatment Panel III,48,49 the Fourth Joint Task Force of the European Society of Cardiology,50 the Task Force for the management of dyslipidaemias of the European Society of Cardiology and the European Atherosclerosis Society,51 and the UK National Institute of Clinical Excellence,52 people with 5-year risk of major vascular events lower than 10% (ie, the lowest two categories of risk in these analyses) would typically not be judged suitable for statin treatment (table 3, appendix p 5). Judgments about the appropriateness of widespread prescription of statins for the primary prevention of vascular events in patients at lower risk also depend on the cost effectiveness of such a strategy, which in turn depends on the local availability and cost of therapy. Generic statin interventions, if effective, are likely to be cost-effective in individuals at annual vascular disease risk down to at least about 1%.53–55 The present report shows that statins are indeed both effective and safe for people with 5-year risk of major vascular events lower than 10% and, therefore, suggests that these guidelines might need to be reconsidered.
Table 3.
Eligibility of CTT participants without a history of vascular disease for statin therapy under existing major guidelines, by estimated 5-year major vascular event risk
| Observed MCE event rate (% per annum)* | Observed vascular death rate (% per annum)* |
Broad eligibility under current guidelines |
||||
|---|---|---|---|---|---|---|
| ATP-III† | ESC task force‡ | NICE§ | ||||
| CTT risk category | ||||||
| <5% | 0·2 | 0·1 | × | × | × | |
| ≥5% to <10% | 0·8 | 0·3 | × | × | × | |
| ≥10% to <20% | 1·6 | 1·0 | P | P | P | |
| ≥20% to <30% | 3·2 | 2·3 | P | P | P | |
| ≥30% | 5·6 | 5·8 | P | P | P | |
CTT=Cholesterol Treatment Trialists'. MCE=major coronary event.
Among control-allocated participants without a history of vascular disease.
The Adult Treatment Panel III (ATP III) of the National Cholesterol Education p rogram in the USA.
The Fourth Joint Task Force of the European Society of Cardiology (ESC) and Other Societies on Cardiovascular Disease Prevention in Clinical Practice and the ESC/EAS Guidelines for the management of dyslipidaemias.
The National Institute for Health and Clinical Excellence (NICE) in the National Health Service in England and Wales.
Acknowledgments
Acknowledgments
The Clinical Trial Service Unit & Epidemiological Studies Unit (CTSU) in the UK and the National Health and Medical Research Council Clinical Trials Centre (CTC) in Australia coordinate this collaboration jointly. The present meta-analysis work is supported at the Health Economics Research Centre, University of Oxford (writing committee members B Mihaylova, A Gray) by a British Heart Foundation research grant (Grant No PG/08/063/25397), and at the CTSU (writing committee members J Emberson, L Blackwell, R Collins, C Baigent) by the UK Medical Research Council, British Heart Foundation, Cancer Research UK and, previously, the European Community Biomed Programme. The CTC is supported by a programme grant from the Australian National Health and Medical Research Council, and a grant from the National Heart Foundation, Australia. JE acknowledges support from the BHF Centre of Research Excellence, Oxford, UK (RE/08/04).
Contributors
The writing committee accepts full responsibility for the content of this paper. All of the members contributed to collection and analysis of the data and to the preparation of the report. All collaborators had an opportunity to contribute to the interpretation of the results and to drafting of the report.
Current membership of the CTT Collaboration
Writing committee: B Mihaylova, J Emberson, L Blackwell, A Keech, J Simes, E H Barnes, M Voysey, A Gray, R Collins, C Baigent.
Collaborating trialists: A to Z trial (phase Z) J de Lemos, E Braunwald, M Blazing, S Murphy; AFCAPS/TEXCAPS (AirForce/Texas Coronary Atherosclerosis Prevention Study) J R Downs, A Gotto, M Clearfield; ALERT (Assessment of Lescol in Transplantation) H Holdaas; ALLHAT (Antihypertensive Lipid Lowering Heart Attack Trial) D Gordon, B Davis; ALLIANCE (Aggressive Lipid-Lowering Initiation Abates New Cardiac Events) M Koren; ASCOT (Anglo-Scandinavian Cardiac Outcomes Trial) B Dahlof, N Poulter, P Sever; ASPEN (Atorvastatin Study for the Prevention of Coronary Heart Disease Endpoints in Non-Insulin Dependent Diabetes Mellitus) R H Knopp (deceased); AURORA (A study to evaluate the Use of Rosuvastatin in subjects On Regular haemodialysis: an Assessment of survival and cardiovascular events) B Fellström, H Holdaas, A Jardine, R Schmieder, F Zannad; BIP (Bezafibrate Infarction Prevention Study) U Goldbourt, E Kaplinsky; CARDS (Collaborative Atorvastatin Diabetes Study) H M Colhoun, D J Betteridge, P N Durrington, G A Hitman, J Fuller, A Neil; 4D (Die Deutsche Diabetes Dialyse Studie) C Wanner, V Krane; CARE (Cholesterol And Recurrent Events Study) F Sacks, L Moyé, M Pfeffer; C M Hawkins, E Braunwald; CORONA (Rosuvastatin in Older Patients with Systolic Heart Failure) J Kjekshus, H Wedel, J Wikstrand; FIELD (Fenofibrate Intervention and Event Lowering in Diabetes) P Barter, A Keech; GISSI (Gruppo Italiano per lo Studio della Sopravvivenza nell'Infarto miocardico)–Heart Failure L Tavazzi, A Maggioni; GISSI–Prevention R Marchioli, G Tognoni, M G Franzosi, A Maggioni; HIT (Veteran Administration Low HDL Intervention Trial) H Bloomfield, S Robins; HPS (Heart Protection Study) R Collins, J Armitage, A Keech, S Parish, R Peto, P Sleight; IDEAL (Incremental Decrease in Endpoints through Aggressive Lipid-lowering) T R Pedersen; JUPITER (Justification for the Use of Statins in Prevention: an Intervention Trial Evaluating Rosuvastatin) P M Ridker; LDS (Lipids in Diabetes Study) R Holman; LEADER (Lower Extremity Arterial Disease Event Reduction trial) T Meade; LIPID (Long-term Intervention with Pravastatin in Ischaemic Disease) J Simes, A Keech, S MacMahon, I Marschner, A Tonkin, J Shaw; LIPS (Lescol Intervention Prevention Study) P W Serruys; MEGA (Management of Elevated cholesterol in the primary prevention Group of Adult Japanese) H Nakamura; Post-CABG (Post-Coronary Artery Bypass Graft Study) G Knatterud; PPP (Pravastatin Pooling Project) C Furberg, R Byington; PROSPER (Prospective Study of Pravastatin in the Elderly at Risk) P Macfarlane, S Cobbe, I Ford, M Murphy, G J Blauw, C Packard, J Shepherd; 4S (Scandinavian Simvastatin Survival Study) J Kjekshus, T Pedersen, L Wilhelmsen; PROVE-IT (Pravastatin or Atorvastatin Evaluation and Infection Therapy) E Braunwald, C Cannon, S Murphy; SEARCH (Study of Effectiveness of Additional Reductions in Cholesterol and Homocysteine) R Collins, J Armitage, L Bowman, S Parish, R Peto, P Sleight; SHARP (Study of Heart and Renal Protection) C Baigent, M Landray, R Collins; TNT (Treating to New Targets) J La Rosa; WHI (Women's Health Initiative) J Rossouw, J Probstfield; WOSCOPS (West of Scotland Coronary Prevention Study) J Shepherd, S Cobbe, P Macfarlane, I Ford.
Other members: M Flather, J Kastelein, C Newman, C Shear, J Tobert, J Varigos, H White, S Yusuf.
Observers: Bristol-Myers Squibb M Mellies, M McGovern, J Barclay, R Belder; Merck Y Mitchel, T Musliner; Laboratoires Fournier J-C Ansquer; Bayer M Llewellyn; Novartis Pharma M Bortolini; AstraZeneca G Brandrup-Wognsen, B Bryzinski, G Olsson, J Pears; Pfizer D DeMicco.
CTT secretariat: C Baigent, E H Barnes, A Baxter, N Bhala, L Blackwell, G Buck, R Collins, J Emberson, W G Herrington, L E Holland, P M Kearney, A Keech, A Kirby, D A Lewis, I Marschner, C Pollicino, C Reith, J Simes, T Sourjina.
Conflicts of interest
Most of the trials in this report were supported by research grants from the pharmaceutical industry. Some members of the writing committee have received reimbursement of costs to participate in scientific meetings from the pharmaceutical industry. AK and JS have also received honoraria from Solvay for lectures related to these studies.
Supplementary Material
References
- 1.Cholesterol Treatment Trialists' (CTT) Collaboration Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170 000 participants in 26 randomised trials. Lancet. 2010;376:1670–1681. doi: 10.1016/S0140-6736(10)61350-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cholesterol Treatment Trialists' (CTT) Collaboration Lack of effect of lowering LDL cholesterol on cancer: meta-analysis of individual data from 175,000 people in 27 randomised trials of statin therapy. PLoS One. 2012;7:e29849. doi: 10.1371/journal.pone.0029849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ray KK, Seshasai SR, Erqou S. Statins and all-cause mortality in high-risk primary prevention: a meta-analysis of 11 randomized controlled trials involving 65,229 participants. Arch Intern Med. 2010;170:1024–1031. doi: 10.1001/archinternmed.2010.182. [DOI] [PubMed] [Google Scholar]
- 4.Taylor F, Ward K, Moore TH. Statins for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2011;1 doi: 10.1002/14651858.CD004816.pub4. CD004816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Redberg RF, Katz M, Grady D. Editor's Note—to make the case—evidence is required: comment on “Making the case for selective use of statins in the primary prevention setting”. Arch Intern Med. 2011;171:1594. doi: 10.1001/archinternmed.2011.409. [DOI] [PubMed] [Google Scholar]
- 6.Kerr AJ, Broad J, Wells S, Riddell T, Jackson R. Should the first priority in cardiovascular risk management be those with prior cardiovascular disease? Heart. 2009;95:125–129. doi: 10.1136/hrt.2007.140905. [DOI] [PubMed] [Google Scholar]
- 7.Cholesterol Treatment Trialists' (CTT) Collaboration Protocol for a prospective collaborative overview of all current and planned randomized trials of cholesterol treatment regimens. Am J Cardiol. 1995;75:1130–1134. doi: 10.1016/s0002-9149(99)80744-9. [DOI] [PubMed] [Google Scholar]
- 8.Cholesterol Treatment Trialists' (CTT) Collaboration Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90 056 participants in 14 randomised trials of statins. Lancet. 2005;366:1267–1278. doi: 10.1016/S0140-6736(05)67394-1. [DOI] [PubMed] [Google Scholar]
- 9.de Lemos JA, Blazing MA, Wiviott SD. Early intensive vs a delayed conservative simvastatin strategy in patients with acute coronary syndromes: phase Z of the A to Z Trial. JAMA. 2004;292:1307–1316. doi: 10.1001/jama.292.11.1307. [DOI] [PubMed] [Google Scholar]
- 10.Cannon CP, Braunwald E, McCabe CH. Intensive versus moderate lipid lowering with statins after acute coronary syndromes. N Engl J Med. 2004;350:1495–1504. doi: 10.1056/NEJMoa040583. [DOI] [PubMed] [Google Scholar]
- 11.Pedersen TR, Faergeman O, Kastelein JJP. High-dose atorvastatin vs usual-dose simvastatin for secondary prevention after myocardial infarction: the IDEAL study: a randomized controlled trial. JAMA. 2005;294:2437–2445. doi: 10.1001/jama.294.19.2437. [DOI] [PubMed] [Google Scholar]
- 12.Scandinavian Simvastatin Survival Study Group Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S) Lancet. 1994;344:1383–1389. [PubMed] [Google Scholar]
- 13.Shepherd J, Cobbe SM, Ford I. Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia. West of Scotland Coronary Prevention Study Group. N Engl J Med. 1995;333:1301–1307. doi: 10.1056/NEJM199511163332001. [DOI] [PubMed] [Google Scholar]
- 14.The Post Coronary Artery Bypass Graft Trial Investigators The effect of aggressive lowering of low-density lipoprotein cholesterol levels and low-dose anticoagulation on obstructive changes in saphenous-vein coronary-artery bypass grafts. N Engl J Med. 1997;336:153–162. doi: 10.1056/NEJM199701163360301. [DOI] [PubMed] [Google Scholar]
- 15.Downs JR, Clearfield M, Weis S. Primary prevention of acute coronary events with lovastatin in men and women with average cholesterol levels: results of AFCAPS/TexCAPS. Air Force/Texas Coronary Atherosclerosis Prevention Study. JAMA. 1998;279:1615–1622. doi: 10.1001/jama.279.20.1615. [DOI] [PubMed] [Google Scholar]
- 16.The Long-Term Intervention with Pravastatin in Ischaemic Disease Study Group Prevention of cardiovascular events and death with pravastatin in patients with coronary heart disease and a broad range of initial cholesterol levels. N Engl J Med. 1998;339:1349–1357. doi: 10.1056/NEJM199811053391902. [DOI] [PubMed] [Google Scholar]
- 17.GISSI Prevenzione Investigators Results of the low-dose (20 mg) pravastatin GISSI Prevenzione trial in 4271 patients with recent myocardial infarction: do stopped trials contribute to overall knowledge? GISSI Prevenzione Investigators (Gruppo Italiano per lo Studio della Sopravvivenza nell'Infarto Miocardico) Ital Heart J. 2000;1:810–820. [PubMed] [Google Scholar]
- 18.Serruys PW, de Feyter P, Macaya C. Fluvastatin for prevention of cardiac events following successful first percutaneous coronary intervention: a randomized controlled trial. JAMA. 2002;287:3215–3222. doi: 10.1001/jama.287.24.3215. [DOI] [PubMed] [Google Scholar]
- 19.Heart Protection Study Collaborative Group MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20 536 high-risk individuals: a randomised placebo-controlled trial. Lancet. 2002;360:7–22. [Google Scholar]
- 20.Shepherd J, Blauw GJ, Murphy MB, on behalf of the PROSPER study group Pravastatin in elderly individuals at risk of vascular disease (PROSPER): a randomised controlled trial. Lancet. 2002;360:1623–1630. doi: 10.1016/s0140-6736(02)11600-x. [DOI] [PubMed] [Google Scholar]
- 21.The Allhat Officers and Coordinators for the ALLHAT Collaborative Research Group Major outcomes in moderately hypercholesterolemic, hypertensive patients randomized to pravastatin vs usual care: the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT-LLT) JAMA. 2002;288:2998–3007. doi: 10.1001/jama.288.23.2998. [DOI] [PubMed] [Google Scholar]
- 22.Sever PS, Dahlöf B, Poulter NR, for the ASCOT investigators Prevention of coronary and stroke events with atorvastatin in hypertensive patients who have average or lower-than-average cholesterol concentrations, in the Anglo-Scandinavian Cardiac Outcomes Trial—Lipid Lowering Arm (ASCOT-LLA): a multicentre randomised controlled trial. Lancet. 2003;361:1149–1158. doi: 10.1016/S0140-6736(03)12948-0. [DOI] [PubMed] [Google Scholar]
- 23.Holdaas H, Fellström B, Jardine AG, on behalf of the Assessment of LEscol in Renal Transplantation (ALERT) Study Investigators Effect of fluvastatin on cardiac outcomes in renal transplant recipients: a multicentre, randomised, placebo-controlled trial. Lancet. 2003;361:2024–2031. doi: 10.1016/S0140-6736(03)13638-0. [DOI] [PubMed] [Google Scholar]
- 24.Colhoun HM, Betteridge DJ, Durrington PN, on behalf of the CARDS investigators Primary prevention of cardiovascular disease with atorvastatin in type 2 diabetes in the Collaborative Atorvastatin Diabetes Study (CARDS): multicentre randomised placebo-controlled trial. Lancet. 2004;364:685–696. doi: 10.1016/S0140-6736(04)16895-5. [DOI] [PubMed] [Google Scholar]
- 25.Sacks FM, Pfeffer MA, Moye LA. The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. Cholesterol and Recurrent Events Trial investigators. N Engl J Med. 1996;335:1001–1009. doi: 10.1056/NEJM199610033351401. [DOI] [PubMed] [Google Scholar]
- 26.Wanner C, Krane V, Marz W. Atorvastatin in patients with type 2 diabetes mellitus undergoing hemodialysis. N Engl J Med. 2005;353:238–248. doi: 10.1056/NEJMoa043545. [DOI] [PubMed] [Google Scholar]
- 27.Knopp RH, d'Emden M, Smilde JG, Pocock SJ. Efficacy and safety of atorvastatin in the prevention of cardiovascular end points in subjects with type 2 diabetes: the Atorvastatin Study for Prevention of Coronary Heart Disease Endpoints in non-insulin-dependent diabetes mellitus (ASPEN) Diabetes Care. 2006;29:1478–1485. doi: 10.2337/dc05-2415. [DOI] [PubMed] [Google Scholar]
- 28.Koren MJ, Hunninghake DB, on behalf of the AI Clinical outcomes in managed-care patients with coronary heart disease treated aggressively in lipid-lowering disease management clinics: the ALLIANCE study. J Am Coll Cardiol. 2004;44:1772–1779. doi: 10.1016/j.jacc.2004.07.053. [DOI] [PubMed] [Google Scholar]
- 29.Nakamura H, Arakawa K, Itakura H. Primary prevention of cardiovascular disease with pravastatin in Japan (MEGA Study): a prospective randomised controlled trial. Lancet. 2006;368:1155–1163. doi: 10.1016/S0140-6736(06)69472-5. [DOI] [PubMed] [Google Scholar]
- 30.Fellstrom BC, Jardine AG, Schmieder RE. Rosuvastatin and cardiovascular events in patients undergoing hemodialysis. N Engl J Med. 2009;360:1395–1407. doi: 10.1056/NEJMoa0810177. [DOI] [PubMed] [Google Scholar]
- 31.Ridker PM, Danielson E, Fonseca FA. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med. 2008;359:2195–2207. doi: 10.1056/NEJMoa0807646. [DOI] [PubMed] [Google Scholar]
- 32.Kjekshus J, Apetrei E, Barrios V. Rosuvastatin in older patients with systolic heart failure. N Engl J Med. 2007;357:2248–2261. doi: 10.1056/NEJMoa0706201. [DOI] [PubMed] [Google Scholar]
- 33.Gissi-HF investigators Effect of rosuvastatin in patients with chronic heart failure (the GISSI-HF trial): a randomised, double-blind, placebo-controlled trial. Lancet. 2008;372:1231–1239. doi: 10.1016/S0140-6736(08)61240-4. [DOI] [PubMed] [Google Scholar]
- 34.LaRosa JC, Grundy SM, Waters DD. Intensive lipid lowering with atorvastatin in patients with stable coronary disease. N Engl J Med. 2005;352:1425–1435. doi: 10.1056/NEJMoa050461. [DOI] [PubMed] [Google Scholar]
- 35.Study of the Effectiveness of Additional Reductions in Cholesterol and Homocysteine (SEARCH) Collaborative Group Intensive lowering of LDL cholesterol with 80 mg versus 20 mg simvastatin daily in 12 064 survivors of myocardial infarction: a double-blind randomised trial. Lancet. 2010;376:1658–1669. doi: 10.1016/S0140-6736(10)60310-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Amarenco P, Bogousslavsky J, Callahan A., III High-dose atorvastatin after stroke or transient ischemic attack. N Engl J Med. 2006;355:549–559. doi: 10.1056/NEJMoa061894. [DOI] [PubMed] [Google Scholar]
- 37.Athyros VG, Papageorgiou AA, Mercouris BR. Treatment with atorvastatin to the National Cholesterol Educational Program goal versus ‘usual’ care in secondary coronary heart disease prevention. The GREek Atorvastatin and Coronary-heart-disease Evaluation (GREACE) study. Curr Med Res Opin. 2002;18:220–228. doi: 10.1185/030079902125000787. [DOI] [PubMed] [Google Scholar]
- 38.Armitage J. The safety of statins in clinical practice. Lancet. 2007;370:1781–1790. doi: 10.1016/S0140-6736(07)60716-8. [DOI] [PubMed] [Google Scholar]
- 39.Davidson MH, Robinson JG. Safety of aggressive lipid management. J Am Coll Cardiol. 2007;49:1753–1762. doi: 10.1016/j.jacc.2007.01.067. [DOI] [PubMed] [Google Scholar]
- 40.Cheung BMY, Lam KSL. Is intensive LDL-cholesterol lowering beneficial and safe? Lancet. 2010;376:1622–1624. doi: 10.1016/S0140-6736(10)61545-0. [DOI] [PubMed] [Google Scholar]
- 41.Sattar N, Preiss D, Murray HM. Statins and risk of incident diabetes: a collaborative meta-analysis of randomised statin trials. Lancet. 2010;375:735–742. doi: 10.1016/S0140-6736(09)61965-6. [DOI] [PubMed] [Google Scholar]
- 42.Preiss D, Seshasai SR, Welsh P. Risk of incident diabetes with intensive-dose compared with moderate-dose statin therapy: a meta-analysis. JAMA. 2011;305:2556–2564. doi: 10.1001/jama.2011.860. [DOI] [PubMed] [Google Scholar]
- 43.The Emerging Risk Factors Collaboration Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet. 2010;375:2215–2222. doi: 10.1016/S0140-6736(10)60484-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Strandberg TE, Pyorala K, Cook TJ, for the 4S Group Mortality and incidence of cancer during 10-year follow-up of the Scandinavian Simvastatin Survival Study (4S) Lancet. 2004;364:771–777. doi: 10.1016/S0140-6736(04)16936-5. [DOI] [PubMed] [Google Scholar]
- 45.LIPID Study Group Long-term effectiveness and safety of pravastatin in 9014 patients with coronary heart disease and average cholesterol concentrations: the LIPID trial follow-up. Lancet. 2002;359:1379–1387. doi: 10.1016/S0140-6736(02)08351-4. [DOI] [PubMed] [Google Scholar]
- 46.Ford I, Murray H, Packard CJ. Long-term follow-up of the West of Scotland Coronary Prevention Study. N Engl J Med. 2007;357:1477–1486. doi: 10.1056/NEJMoa065994. [DOI] [PubMed] [Google Scholar]
- 47.Heart Protection Study Collaborative Group Effects on 11 year mortality and morbidity of lowering LDL cholesterol with simvastatin for about 5 years in 20 536 high-risk individuals. Lancet. 2011;378:2013–2020. doi: 10.1016/S0140-6736(11)61125-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Grundy SM, Cleeman JI, Merz CNB. Implications of Recent Clinical Trials for the National Cholesterol Education Program Adult Treatment Panel III Guidelines. Circulation. 2004;110:227–239. doi: 10.1161/01.CIR.0000133317.49796.0E. [DOI] [PubMed] [Google Scholar]
- 49.Expert Panel on Detection Evaluation and Treatment of High Blood Cholesterol in Adults Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) JAMA. 2001;285:2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 50.Graham I, Atar D, Borch-Johnsen K. European guidelines on cardiovascular disease prevention in clinical practice: full text. Fourth Joint Task Force of the European Society of Cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of nine societies and by invited experts) Eur J Cardiovasc Prev Rehabil. 2007;14(suppl 2):1–113. doi: 10.1097/01.hjr.0000277983.23934.c9. [DOI] [PubMed] [Google Scholar]
- 51.Reiner Z, Catapano AL, De Backer G. ESC/EAS Guidelines for the management of dyslipidaemias: the Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS) Eur Heart J. 2011;32:1769–1818. doi: 10.1093/eurheartj/ehr158. [DOI] [PubMed] [Google Scholar]
- 52.Cooper A, Nherera L, Calvert N. Clinical guidelines and evidence review for lipid modification: cardiovascular risk assessment and the primary and secondary prevention of cardiovascular disease. National Collaborating Centre for Primary Care and Royal College of General Practitioners; London: 2008. [Google Scholar]
- 53.Heart Protection Study Collaborative Group Lifetime cost effectiveness of simvastatin in a range of risk groups and age groups derived from a randomised trial of 20,536 people. BMJ. 2006;333:1145–1148. doi: 10.1136/bmj.38993.731725.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lazar LD, Pletcher MJ, Coxson PG, Bibbins-Domingo K, Goldman L. Cost-effectiveness of statin therapy for primary prevention in a low-cost statin era. Circulation. 2011;124:146–153. doi: 10.1161/CIRCULATIONAHA.110.986349. [DOI] [PubMed] [Google Scholar]
- 55.Pletcher MJ, Lazar L, Bibbins-Domingo K. Comparing impact and cost-effectiveness of primary prevention strategies for lipid-lowering. Ann Intern Med. 2009;150:243–254. doi: 10.7326/0003-4819-150-4-200902170-00005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.