Abstract
Background and Objectives
B-type natriuretic peptide (BNP) is an important marker for the diagnosis of heart failure and is useful towards predicting morbidity and mortality after non-cardiac surgery. Nevertheless, information on the relationship between postoperative BNP levels and perioperative prognosis after non-cardiac surgery is scarce. The purpose of the study was to assess whether postoperative BNP levels could be used as a predictor of prolonged hospitalization in elderly hypertensive patients after non-cardiac surgery.
Subjects and Methods
Ninety-seven (97) patients, aged 55 years or older (mean age: 73.12±10.05 years, M : F=24 : 73) were enrolled in a prospective study from May 2005 through August 2010. All patients underwent total knee or hip replacement. Postoperative BNP and other diagnostic data were recorded within 24 hours of surgery. Patients that required a prolonged hospital stay due to operative causes, such as wound infection and re-operation, were excluded.
Results
The length of hospital stay was significantly correlated with postoperative BNP levels (p=0.031). Receiver operating characteristic curves demonstrated postoperative BNP levels as predictors of hospital stay ≥30 days with areas under the curve of 0.774 (95% confidence interval: 0.679-0.87, p<0.0001). A BNP cut-off value above 217.5 pg/mL had a sensitivity of 80.6% and a specificity of 66.7% for predicting postoperative hospital stays of 30 days or more.
Conclusion
Postoperative BNP levels may predict the length of hospital stays after non-cardiac surgery in hypertensive patients. Elevated BNP levels were associated with prolonged hospitalization after elective orthopedic surgery.
Keywords: Natriuretic peptin, brain; Hospitalization; Postoperative period; Hypertension
Introduction
Perioperative cardiac complications, such as cardiac death, myocardial infarction, unstable angina, pulmonary edema and serious ventricular arrhythmia, are potentially avoidable causes of morbidity and mortality in patients undergoing non-cardiac surgery or vascular surgery.1-3) Hypertension is a risk factor for potential coronary artery disease. Thus, evaluation of the cardiovascular system in patients with hypertension is important to predict perioperative morbidity and mortality before undertaking non-cardiac surgery. A variety of scoring systems and imaging strategies have been developed to predict such adverse cardiovascular events.4-8) However, low predictive accuracy and poor clinical utility have limited the use of risk indices in current clinical practice and currently, there is no gold standard to effectively predict postoperative complications, length of hospital stay, or the possibility of mortality. Preoperative evaluations of the cardiovascular system that use chest radiography, electrocardiogram (ECG), echocardiography and laboratory studies are limited. For example, one limitation is the timing of an evaluation; if an evaluation is made during a time during which that particular parameter is stable, there is difficulty in detecting a small but significant deterioration in cardiovascular functional. While echocardiography has been utilized to assess cardiac risks, adding echocardiographic results have not demonstrated to improve risk assessment.9) Therefore, postoperative measurements of B-type natriuretic peptide (BNP) in certification of patients for perioperative events are clinically important but still not evaluated.
The purpose of this study is to evaluate the relationship between post-operative BNP levels and the duration of hospital stay in hypertensive patients. In addition, this study attempts to assess normal left ventricular (LV) systolic function after elective orthopedic surgery.
Subjects and Methods
Study population
This prospective investigation was a single-center, observational cohort study. A total of ninety-seven consecutive patients with hypertension fulfilled the inclusion criteria and underwent scheduled orthopedic surgery (total hip or knee replacement) at the author's university hospital from May 2005 through August 2010.
The enrolled subjects were divided into 2 groups. Group I included patients that were hospitalization for 30 days or longer, while Group II included patients that were hospitalized for less than thirty days.
Cardiovascular risks were evaluated before surgery for spinal, epidural or general anesthesia by a cardiologist and an anesthetist according to the American College of Cardiology/American Heart Association (ACC/AHA) guidelines.10) These operations were performed in a usual manner without any clinical evidence of a significant fluid and electrolyte imbalance or cardiac failure.
This study excluded patients with the following: had undergone an emergency operation; had a LV dysfunction (ejection fraction <50%), renal insufficiency (serum creatinine level >2.0 mg/dL); or had a history of ischemic heart disease, stroke, severe valvular heart disease, or peripheral vascular disease. In addition, patients were excluded patients if they had experienced a prolonged postoperative hospital stay due to operative causes such as a wound infection, bilateral operations, or re-operation. The study was approved by the local ethics committee and written informed consent was obtained from each study participant.
Data collection
Preoperative data were obtained within 7 days before a patient's scheduled operation, which included demographic data, 12-lead ECG recording, chest posteroanterior, medical and medication history, surgical history, physical examination and other biochemical tests. Age, gender, the presence of diabetes mellitus and dyslipidemia, blood pressure, body mass index, pre-and-postoperative BNP and preoperative hemoglobin levels were verified. The following clinical data were recorded: intravenous fluid intake, urinary output on the day of operation, and the total amount of blood transfused.
The following postoperative evaluations were performed for each patient within 24 hours of completing surgery: physical examination, chest PA, ECG, and laboratory tests. All patients underwent aconventional 2-dimensional and Doppler echocardiographic examinations for the assessment of ventricular systolic and diastolic functions. The Framingham criteria were used for defining postoperative heart failure.11)
B-type natriuretic peptide measurement and assay
Plasma BNP and hemoglobin levels were measured on preoperative and postoperative day 1. A venous blood sample, taken for BNP measurement, was collected in a tube containing lithium-heparin and transported to the laboratory at room temperature. Patients were asked to lie at rest in a supine position for thirty (30) minutes, in order to eliminate any confounding effect of posture and exercise on plasma levels to the extent possible, before taking a preoperative blood sample. The Bayer ADVIA Centaur™ immunoassay operation (Bayer Healthcare LLC, Diagnostic division, Leverkusen, Germany) was used to measure plasma BNP levels.
Clinical outcome
The clinical outcomes of this study were evaluated during the hospitalization and follow-up periods. The primary end point was the predictive power of BNP levels for postoperative length of hospital stay. The secondary end point included non-cardiac death, cardiac death, myocardial infarction, development of congestive heart failure, and re-hospitalization. Cardiac death was defined as having experienced 1) sudden death that could not be explained by any other non-cardiovascular complications, or 2) gradual death caused by progressive heart failure and other known cardiac risk factors.
Myocardial infarction was defined as having a cardiac Troponin I (cTnI) increase above the 99th percentile of the upper limit (cTnI >0.032 ng/mL). Congestive heart failure was diagnosed by physical examination and interpretation of chest X-ray images by a radiologist as consistent with these complications.
Statistical analysis
Normally distributed continuous variables are expressed as the mean and standard deviation. Categorical data are presented as the absolute value and percentage. The Student's t-test and chi-square test, or Fisher's exact test, were used for normally distributed continuous and categorical variables, respectively. Variables that appeared to be significant on univariate analysis were entered into the model of multivariate analysis to determine independent factors associated with prolonged hospitalization. The odds ratios (OR) were given with 95% confidence intervals (CI).
To establish a BNP cut-off value with the appropriate sensitivity and specificity, receiver operating characteristic (ROC) curves were plotted and the area under the curve was estimated. Statistical analysis was performed using Statistical Package for the Social Sciences (SPSS). All data have been analyzed with SPSS correlation and multiple linear regression models (SPSS v.18.0; SPSS Inc., Chicago, IL, USA). ROC curve was made using Medcalc version 9.6.
Results
Patient characteristics and echocardiographic data
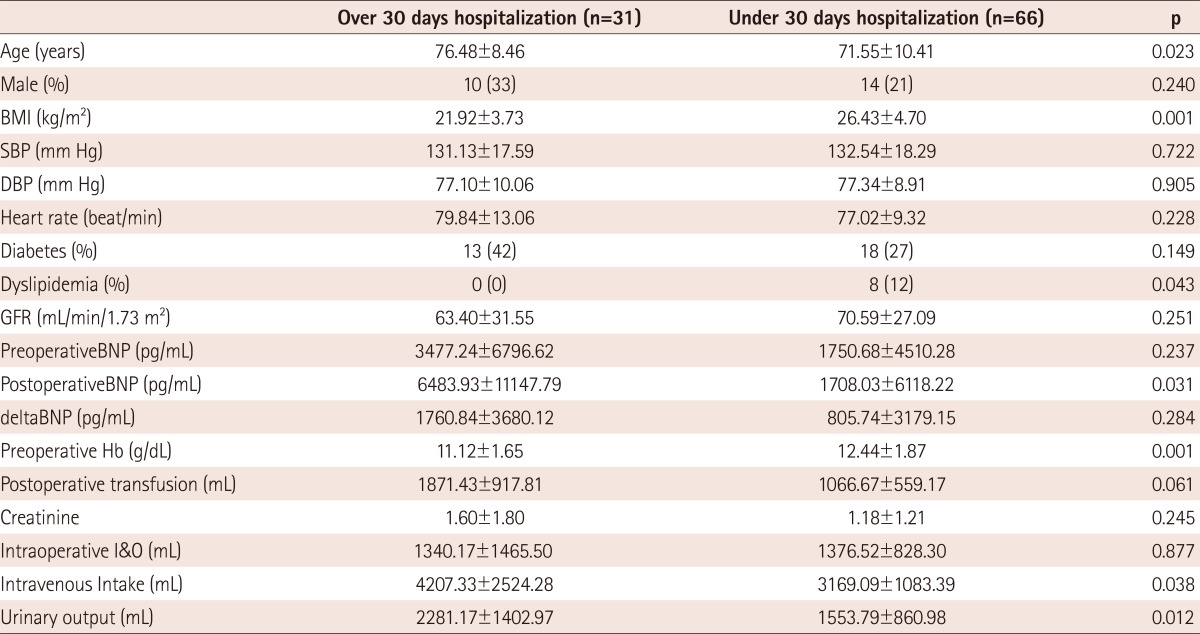
The age of patients ranged from 52 to 70 years with a mean age of 73.12±10.05 years, while the female and male ratio was 73 : 24. The mean duration of hospital admission was 33.24±37.37 days. Group I had a significantly longer period of hospital duration than Group II (64±50.54 days for Group I vs. 18.38±8.94 days for Group II, p=0.0001). The baseline demographic data of patients were summarized in Table 1. Between these 2 groups, Group I had the tendency of being older (76.48±8.46 years old for Group I vs. 71.55±10.41 years old for Group II, p=0.023). However, Group II had a higher level of obese and a greater frequency of dyslipidemia compared to Group I. The preoperative hemoglobin level of Group II was higher than that of Group I (11.12±1.65 g/dL for Group I vs. 12.44±1.87 g/dL for Group II, p=0.001). The total intravenous fluid intake or urinary output of Group I was more frequently maintained than that of Group II (p=0.038 and p=0.012).
Table 1.
Demographic and clinical characteristics of subjects
Data are expressed as mean±SD or number (%) of patients. BMI: body mass index, SBP: systolic blood pressure, DBP: diastolic blood pressure, GFR: glomerular filter rate, BNP: B-type natriuretic peptide, Hb: hemoglobin, I&O: intake and output
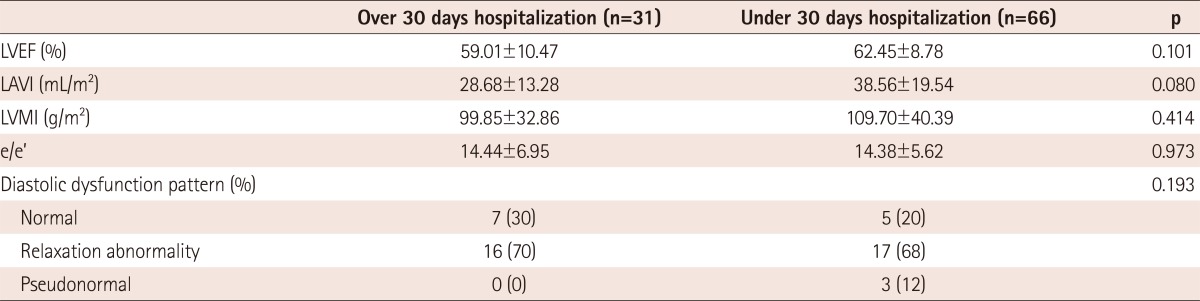
The transfusion and intraoperative Intake and Output data showed no significant differences between these 2 groups. Table 2 showed differences in echocardiographic parameters between the 2 groups; however, this difference was not statistically significant.
Table 2.
Baseline echocardiographic data of study cohort
LVEF: left ventricle ejection fraction, LAVI: left ventricular volume index, LVMI: left ventricular mass index, e/e: the ratio of early transmitral flow velocity to early diastolic septal mitral annulus velocity
B-type natriuretic peptide level and prolonged hospital stay
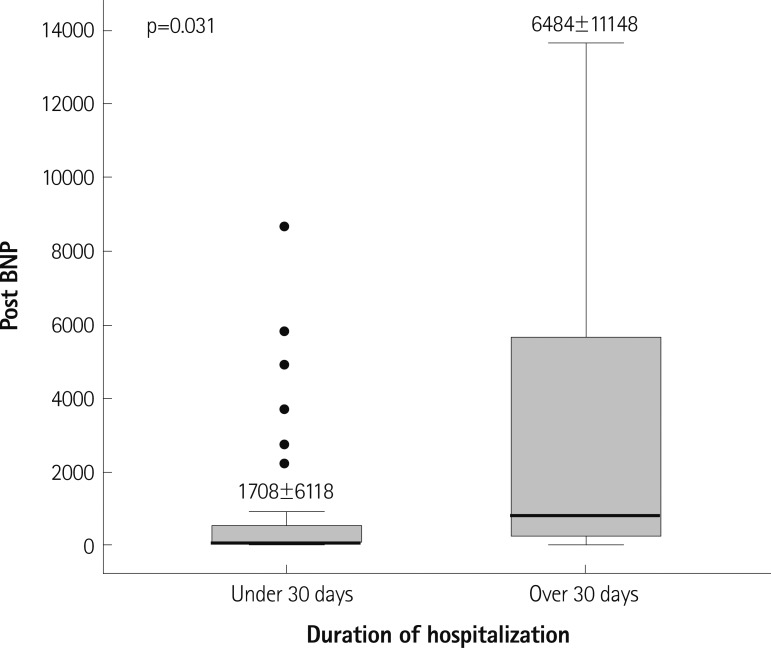
A correlation between postoperative BNP level and prolonged hospital stay was remarkable, as shown in Table 1. Fig. 1 shows a box-plot of postoperative BNP levels in each group. There was a significant difference noted in the postoperative BNP level between the 2 groups. The mean postoperative BNP level of Group I was 6483.93±11147.79 pg/mL as compared to that of Group II was 1708.03±6118.22 pg/mL (p=0.031). The preoperative BNP levels of Group I tended to be higher, but there was no statistical difference in the preoperative BNP level between these 2 groups (3477.24±6796.62 pg/mL for Group I vs. 1750.68±4510.28 pg/mL for Group II, p=0.24). Thus far, this study has illustrated that a significant correlation was displayed between the length of hospitalization and the postoperative BNP level.
Fig. 1.
A comparison of postoperative BNP levels in patients with over 30 days hospitalization and under 30 days hospitalization. Central lines represent medians, box represent 25th and 75th precentiles. Postoperative BNP level was higher in Group I than Group II (Group I vs. Group II: 6483.93±1147.79 pg/mL vs. 1708.03±6118.22 pg/mL, p=0.031). BNP: B-type natriuretic peptide.
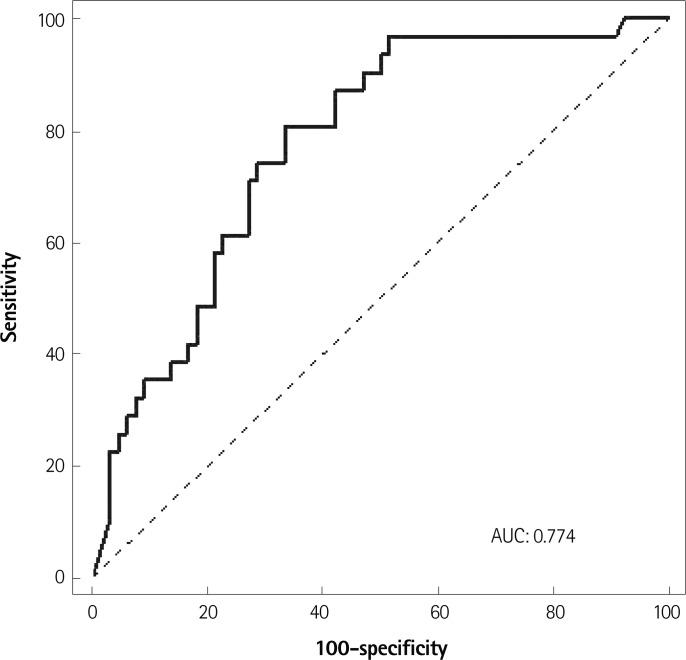
Receiver operating characteristic curves demonstrated postoperative BNP levels as the predictors of hospital stay of 30 days or more with areas under the curve of 0.774 (95% CI, 0.679-0.070, p<0.001) (Fig. 2). A BNP over 217.5 pg/mL had a sensitivity of 80.6% and specificity of 66.7% for predicting a postoperative hospital stay of 30 days or more.
Fig. 2.
Receiver operating characteristics curve was constructed to determine the postoperative B type natriuretic peptide cut-off value for predictive power of predicting the prolonged hospital stay. A cut-off of 217.5 pg/mL yielded the maximal combined sensitivity of 80.6% and specificity of 66.7%. Area under the curve=0.774 (95% confidence interval=0.679-0.870, p<0.0001). AUC: area under the curve, BNP: B-type natriuretic peptide.
Clinical outcome and predictors
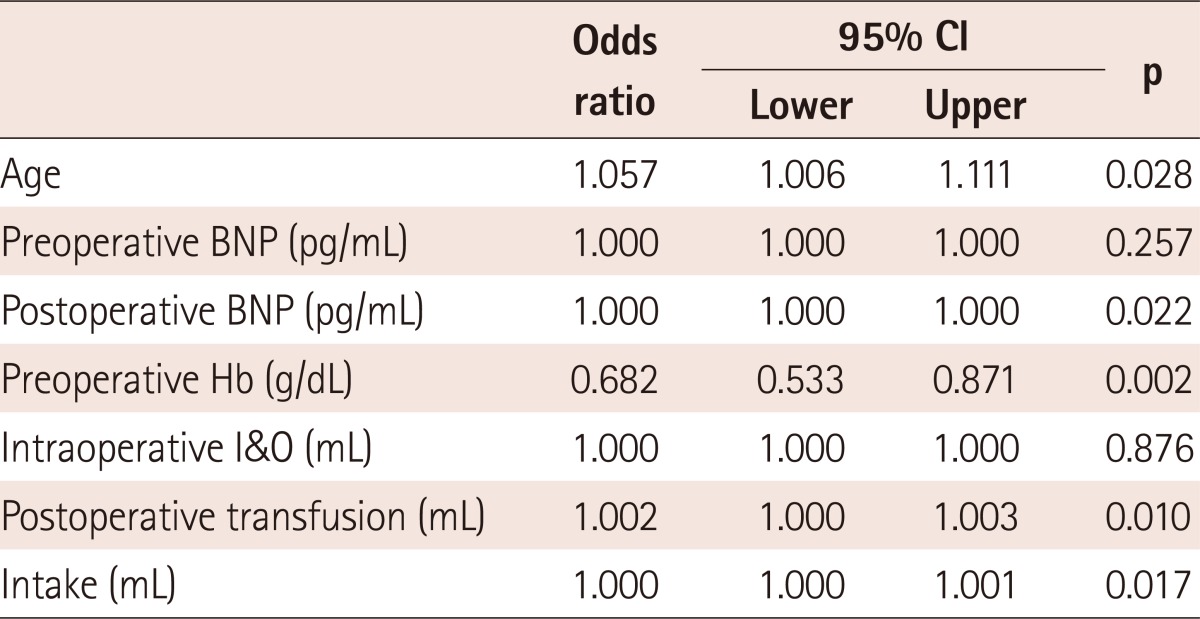
Postoperative cardiac events occurred in 8 patients during the follow-up period (8.2%): one patient with cardiac death, 2 patients with myocardial infarction, one patient with cerebral infarction, and 4 patients required re-hospitalization due to congestive heart failure. There were 10 non-cardiac deaths, which were caused by either disease progression or surgical complications (10.3%). There was no statistically difference in the postoperative cardiac events between these two groups. Using logistic regression analysis, the univariate predictors of prolonged hospitalization were older age, postoperative elevated BNP level, preoperative lower hemoglobin and intravenous fluid intake (Table 3).
Table 3.
Univariate predictors of prolonged hospitalization
CI: confidence interval, BNP: B-type natriuretic peptide, Hb: hemoglobin, I&O: intake and output
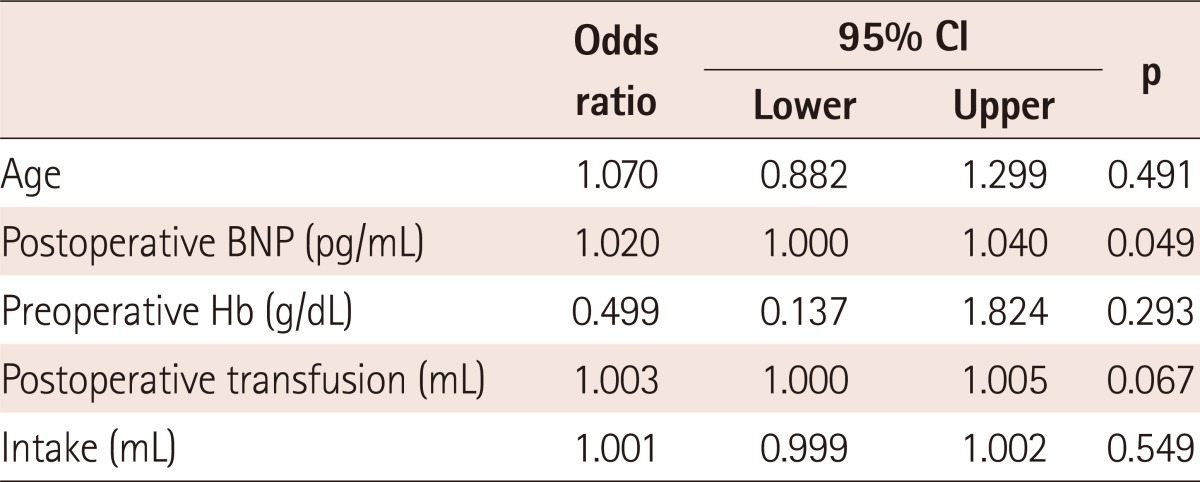
The only independent predictor of prolonged hospitalization through the multivariate regression analysis model adjusting for age, postoperative BNP level, preoperative hemoglobin, postoperative transfusion and intravenous fluid intake was a postoperative elevated BNP level (OR; 1.020, 95% CI; 1.002-1.050, p=0.049) (Table 4).
Table 4.
Mulitivariate predictors of prolonged hospitalization
BNP: B-type natriuretic peptide, Hb: hemoglobin, CI: confidence interval
Discussion
This prospective study proves the value of postoperative BNP level, which may play a role in predicting clinical outcome. Postoperative BNP levels are significantly associated with prolonged hospital stay, especially in hospitalization of over 30 days after non-cardiac surgery in hypertensive patients. Nevertheless, postoperative BNP levels are not predictive of postoperative cardiac events. The usefulness of the postoperative BNP cut-off level of 217.5 pg/mg was associated with an increased postoperative hospital stay.
Alternative methods of perioperative cardiac risk evaluation
Determination of preoperative risks in the elderly patients remains an important challenge for cardiology. Several indices have been developed, including the ACC/AHA guidelines, the revised cardiac index, the Goldman index, and preoperative echocardiography. However, these indices have limitations as prognostic value and some are quite complicated.6) As previous studies have demonstrated that changes in N-terminal pro-B-type BNP (NT-proBNP) were related to adverse outcomes in acute coronary syndromes and acute decompensated heart failure,12),13) NT-proBNP levels should contribute to the evaluation of prognosis during the perioperative period.
The median preoperative NT-proBNP level of patients who had expired during the follow-up period was significantly higher than that of the survivors (795 pg/mL vs. 269 pg/mL, p=0.002). The median difference between pre- and postoperative NT-proBNP levels of expired patients was significantly higher than that of the survivors (5336 pg/mL vs. 665 pg/mL, p=0.010).14) Preoperative NT-proBNP levels above the optimal discriminatory threshold of 457 pg/mL, determined by ROC curve analysis were associated with occurrences of postoperative cardiac events (OR; 10.5, 95% CI; 1.9 to 56.6; p=0.006).15)
Another study demonstrated that both high sensitivity C-reactive protein (hs-CRP) and NT-proBNP had additional value in the prediction of postoperative cardiac events in patients undergoing vascular surgery. In addition, a combined elevation of hs-CRP and NT-proBNP carried a seven-fold higher risk for postoperative cardiac events.16)
Previous studies and the advantages of the B-type natriuretic peptide levels
B-type natriuretic peptide was first discovered in the porcine brain. However, it is actually secreted by both atrial and ventricular myocytes.17) This prohormone is released during hemodynamic stress, that is, when the ventricle is dilated, hypertrophic, or subjected to increased cardiac wall tension.
Prohormone BNP is cleaved into 2 polypeptides: inactive NT-pro-BNP and bioactive peptide BNP. BNP causes arterial vasodilation, diuresis, and natriuresis, and reduces activities of the renin-angiotensin-aldosterone and the sympathetic nervous system.18)
Assays for BNP levels are commercially available and these biomarkers for heart failure are the most extensively used. Such testing is recommended among the current guidelines for hospital admission, discharge and re-hospitalization of heart failure patients.
Plasma BNP levels are powerful predictors of death and major ad-verse cardiovascular events in patients with a stable coronary artery disease, acute coronary syndrome, and congestive heart failure.19),20)
Recently, several studies have confirmed that elevated preoperative BNP levels in patients, who had undergone non-cardiac or cardiac surgery, were associated with increased risks for mortality and morbidity during the follow-up period.21-24) An additional study has suggested that preoperative BNP and/or cTnI levels might assist in differentiating patients who are at very low risk for perioperative cardiac events from those who would require more detailed cardiovascular tests and optimization of therapies before undergoing major non-cardiac surgery.25)
A significant study concerning postoperative BNP levels as a predictor of postoperative complications and outcomes in patients after open heart surgery was published.
Hutfless et al.26) found that the highest postoperative BNP level had been associated with a prolonged hospital stay and one-year mortality. They documented that there had been a significant difference in the highest postoperative BNP level between the group that was hospitalized <10 days postoperatively and the group that had prolonged hospital stay for 10 days or more (750 pg/mL vs. 1190 pg/mL; p<0.001).
They also documented significant differences in median levels of the highest postoperative BNP level between 11 patients who had deceased within a year (1265 pg/mL) and patients who had undergone open-heart surgery but were alive after one year (793 pg/mL) (p<0.01).
In consideration of the mechanism of elevated BNP levels after non-cardiac surgery, surgery by itself can cause stress such as anemia, blood pressure fluctuation, fluid imbalance and activation of the sympathetic nervous system, especially, in hypertensive patients.
B-type natriuretic peptide is released in response to ventricular wall stress. Thus, the consideration is that increased net (including intraoperative fluids) intravenous fluids are associated with increas-ed postoperative BNP levels after surgery. Therefore, the assumption is that postoperative BNP levels may be related to diastolic dysfunction of the heart.
Though small in scale, the theoretical mechanism on the increased BNP levels postoperatively may well be explained in this manner.
In conclusion, a moderately elevated postoperative BNP level above 217.5 pg/mL would predict delayed discharge from hospital for these 97 hypertensive patients with normal systolic function undergoing non-cardiac surgery. This study documented that postoperative BNP levels were not associated with perioperative cardiac complications, but could predict the length of hospital stay after non-cardiac surgery in hypertensive patients.
Nevertheless, this investigation could not document the fact that preoperative BNP levels were associated with prolonged hospital stays or cardiac events.
Measurements of postoperative BNP concentrations may aid in monitoring or actively guiding the level of therapeutic adjustment after surgery.
Post-operative BNP levels are comprehensive predictive factors in the postoperative period that is affected by preoperative BNP levels, fluid intake and output, underlying cardiovascular disease, and multiple risk factors.
Limitations
There are several limitations to this study. The first limitation is in the interpretation of changes in BNP levels over surgery. It is the lack of reliable estimates of volume overload and the aspect that a postoperative elevation of the BNP level is to the result of exposure to volume loading rather than to the progression of underlying cardiac disease. For example, in cases of orthopedic surgery with complicated lesions that require a larger volume of transfusion, the postoperative BNP level would be affected without doubt.
Second, owing to the fact that preoperative BNP levels have been noticed by clinicians prior to surgery for the purpose of managing patients, the results have been substantially confounded.
Third, the preoperative BNP level is found to have no correlation with prolonged hospitalization. Also, it cannot be documented that postoperative BNP level is associated with clinical outcomes, such as death, heart failure, or late prognosis.
Last, long-term follow-up observations and studies on the mechanism of how non-cardiac surgeries could affect postoperative BNP levels are required.
Acknowledgments
This study was performed by the research fund of Ewha Womans University (No. 2005-0997-1-1).
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Eagle KA, Berger PB, Calkins H, et al. ACC/AHA guideline update for perioperative cardiovascular evaluation for noncardiac surgery: executive summary a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1996 Guidelines on Perioperative Cardiovascular Evaluation for Noncardiac Surgery) Circulation. 2002;105:1257–1267. [PubMed] [Google Scholar]
- 2.Goldman L. Cardiac risks and complications of noncardiac surgery. Ann Intern Med. 1983;98:504–513. doi: 10.7326/0003-4819-98-4-504. [DOI] [PubMed] [Google Scholar]
- 3.Mangano DT. Perioperative cardiac morbidity. Anesthesiology. 1990;72:153–184. doi: 10.1097/00000542-199001000-00025. [DOI] [PubMed] [Google Scholar]
- 4.Goldman L, Caldera DL, Nussbaum SR, et al. Multifactorial index of cardiac risk in noncardiac surgical procedures. N Engl J Med. 1977;297:845–850. doi: 10.1056/NEJM197710202971601. [DOI] [PubMed] [Google Scholar]
- 5.Detsky AS, Abrams HB, Forbath N, Scott JG, Hilliard JR. Cardiac assessment for patients undergoing noncardiac surgery: a multifactorial clinical risk index. Arch Intern Med. 1986;146:2131–2134. [PubMed] [Google Scholar]
- 6.Lee TH, Marcantonio ER, Mangione CM, et al. Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation. 1999;100:1043–1049. doi: 10.1161/01.cir.100.10.1043. [DOI] [PubMed] [Google Scholar]
- 7.Poldermans D, Boersma E, Bax JJ, et al. The effect of bisoprolol on perioperative mortality and myocardial infarction in high-risk patients undergoing vascular surgery: Dutch Echocardiographic Cardiac Risk Evaluation Applying Stress Echocardiography Study Group. N Engl J Med. 1999;341:1789–1794. doi: 10.1056/NEJM199912093412402. [DOI] [PubMed] [Google Scholar]
- 8.Eagle KA, Coley CM, Newell JB, et al. Combining clinical and thallium data optimizes preoperative assessment of cardiac risk before major vascular surgery. Ann Intern Med. 1989;110:859–866. doi: 10.7326/0003-4819-110-11-859. [DOI] [PubMed] [Google Scholar]
- 9.Halm EA, Browner WS, Tubau JF, Tateo IM, Mangano DT. Echocardiography for assessing cardiac risk in patients having noncardiac surgery: Study of Perioperative Ischemia Research Group. Ann Intern Med. 1996;125:433–441. doi: 10.7326/0003-4819-125-6-199609150-00001. [DOI] [PubMed] [Google Scholar]
- 10.Auerbach A, Goldman L. Assessing and reducing the cardiac risk of noncardiac surgery. Circulation. 2006;113:1361–1376. doi: 10.1161/CIRCULATIONAHA.105.573113. [DOI] [PubMed] [Google Scholar]
- 11.McKee PA, Castelli WP, McNamara PM, Kannel WB. The natural history of congestive heart failure: the Framingham Study. N Engl J Med. 1971;285:1441–1446. doi: 10.1056/NEJM197112232852601. [DOI] [PubMed] [Google Scholar]
- 12.Bettencourt P, Azevedo A, Pimenta J, Friões F, Ferreira S, Ferreira A. N-terminal-pro-brain natriuretic peptide predicts outcome after hospital discharge in heart failure patients. Circulation. 2004;110:2168–2174. doi: 10.1161/01.CIR.0000144310.04433.BE. [DOI] [PubMed] [Google Scholar]
- 13.Heeschen C, Hamm CW, Mitrovic V, Lantelme NH, White HD Platelet Receptor Inhibition in Ischemic Syndrome Management (PRISM) In vestigators. N-terminal pro-B-type natriuretic peptide levels for dynamic risk stratification of patients with acute coronary syndromes. Circulation. 2004;110:3206–3212. doi: 10.1161/01.CIR.0000147611.92021.2B. [DOI] [PubMed] [Google Scholar]
- 14.Goei D, van Kuijk JP, Flu WJ, et al. Usefulness of repeated N-terminal pro-B-type natriuretic peptide measurements as incremental predictor for long-term cardiovascular outcome after vascular surgery. Am J Cardiol. 2011;107:609–614. doi: 10.1016/j.amjcard.2010.10.021. [DOI] [PubMed] [Google Scholar]
- 15.Schutt RC, Cevik C, Phy MP. Plasma N-terminal prohormone brain natriuretic peptide as a marker for postoperative cardiac events in high-risk patients undergoing noncardiac surgery. Am J Cardiol. 2009;104:137–140. doi: 10.1016/j.amjcard.2009.03.005. [DOI] [PubMed] [Google Scholar]
- 16.Goei D, Hoeks SE, Boersma E, et al. Incremental value of high-sensitivity C-reactive protein and N-terminal pro-B-type natriuretic peptide for the prediction of postoperative cardiac events in noncardiac vascular surgery patients. Coron Artery Dis. 2009;20:219–224. doi: 10.1097/MCA.0b013e3283219e47. [DOI] [PubMed] [Google Scholar]
- 17.Cowie MR, Mendez GF. BNP and congestive heart failure. Prog Cardiovasc Dis. 2002;44:293–321. doi: 10.1053/pcad.2002.24599. [DOI] [PubMed] [Google Scholar]
- 18.Nakagawa O, Ogawa Y, Itoh H, et al. Rapid transcriptional activation and early mRNA turnover of brain natriuretic peptide in cardiocyte hypertrophy: evidence for brain natriuretic peptide as an "emergency" cardiac hormone against ventricular overload. J Clin Invest. 1995;96:1280–1287. doi: 10.1172/JCI118162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kragelund C, Grønning B, Køber L, Hildebrandt P, Steffensen R. N-terminal pro-B-type natriuretic peptide and long-term mortality in stable coronary heart disease. N Engl J Med. 2005;352:666–675. doi: 10.1056/NEJMoa042330. [DOI] [PubMed] [Google Scholar]
- 20.De Lemos JA, Morrow DA, Bentley JH, et al. The prognostic value of B-type natriuretic peptide in patients with acute coronary syndromes. N Engl J Med. 2001;345:1014–1021. doi: 10.1056/NEJMoa011053. [DOI] [PubMed] [Google Scholar]
- 21.Leibowitz D, Planer D, Rott D, Elitzur Y, Chajek-Shaul T, Weiss AT. Brain natriuretic peptide levels predict perioperative events in cardiac patients undergoing noncardiac surgery: a prospective study. Cardiology. 2008;110:266–270. doi: 10.1159/000112411. [DOI] [PubMed] [Google Scholar]
- 22.Dernellis J, Panaretou M. Assessment of cardiac risk before non-cardiac surgery: brain natriuretic peptide in 1590 patients. Heart. 2006;92:1645–1650. doi: 10.1136/hrt.2005.085530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Berry C, Kingsmore D, Gibson S, et al. Predictive value of plasma brain natriuretic peptide for cardiac outcome after vascular surgery. Heart. 2006;92:401–402. doi: 10.1136/hrt.2005.060988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cuthbertson BH, Amiri AR, Croal BL, et al. Utility of B-type natriuretic peptide in predicting perioperative cardiac events in patients undergoing major non-cardiac surgery. Br J Anaesth. 2007;99:170–176. doi: 10.1093/bja/aem158. [DOI] [PubMed] [Google Scholar]
- 25.Cuthbertson BH, Amiri AR, Croal BL, Rajagopalan S, Brittenden J, Hillis GS. Utility of B-type natriuretic peptide in predicting medium-term mortality in patients undergoing major non-cardiac surgery. Am J Cardiol. 2007;100:1310–1313. doi: 10.1016/j.amjcard.2007.05.058. [DOI] [PubMed] [Google Scholar]
- 26.Hutfless R, Kazanegra R, Madani M, et al. Utility of B-type natriuretic peptide in predicting postoperative complications and outcomes in patients undergoing heart surgery. J Am Coll Cardiol. 2004;43:1873–1879. doi: 10.1016/j.jacc.2003.12.048. [DOI] [PubMed] [Google Scholar]