Abstract
Adults with intellectual disability (ID) experience more falls than their non-disabled peers. A gait analysis was conducted to quantify normal walking, and an additional slip trial was performed to measure slip response characteristics for adults with ID as well as a group of age-and gender-matched controls. Variables relating to gait pattern, slip propensity, and slip severity were assessed to compare the differences between groups. The ID group was found to have significantly slower walking speed, shorter step lengths, and increased knee flexion angles at heel contact. These gait characteristics are known to reduce the likelihood of slip initiation in adults without ID. Despite a more cautious gait pattern, however, the ID group exhibited greater slip distances indicating greater slip severity. This study suggests that falls in this population may be due to deficient slip detection or insufficient recovery response.
Keywords: Intellectual disability, fall accidents, gait analysis, biomechanics
1.0 INTRODUCTION
Roughly 1.3 million adults in the U.S. have an intellectual disability (ID) (U.S. Census, 2008). Individuals with ID are known to be more prone to fall injuries than their non-disabled peers (Sherrard et al., 2001 & 2002; Hsieh et al., 2001) and the cause of their falls is multifactorial (Hale et al., 2007). Both Hsieh et al. (2001) and Sherrard et al. (2002) have reported psychological and behavioral problems as determinants of injury risk for the intellectually disabled. Other research groups have acknowledged that deficits in physical mobility may also be a contributing factor in falls for adults with ID (Sparrow et al., 1998; Hale et al., 2007). Although above epidemiological studies clearly link higher fall risk with individuals with ID, mechanisms associated with increased fall rate seen in this population remain elusive.
Biomechanical analysis has been used to identify stability and gait characteristics for populations including the elderly, individuals with neuromuscular disorders, and Alzheimer’s patients (Lockhart et al., 2003 & 2005; Plotnik et al., 2007; Frzovic et al., 2000; Wittwer et al., 2008). The ID population has not received as much attention regarding mobility limitations (Cleaver et al., 2009). Sparrow et al. (1998) reported more exaggerated movements with regard to obstacle negotiation, and individuals with ID demonstrated greater intra-individual variability during walk-to-run and run-to-walk gait transitions (Agiovlastitis et al., 2008). Adults with ID have also been reported to exhibit greater mediolateral than anteroposterior sway while controls do not (Carmeli et al., 2008). The current study addresses the need for more biomechanical evaluation of gait among the ID population. Specifically, this study will investigate slip-induced falls. It’s hypothesized that individuals with intellectual disability will exhibit significantly different gait patterns than non-disabled age- and gender-matched controls, and that the ID group will exhibit greater slip propensity and severity as measured by required coefficient of friction and slip distance parameters.
2.0 METHODS
2.1 Participants
Fifteen participants (11 males, 4 females, (mean ± SD) 38.5 ± 10.0 years, 168.4 ± 8.2 cm, 76.3 ± 12.8 kg) were recruited from the Southwestern Virginia Training Center (SWVTC) in Galax, VA. Each participant was previously diagnosed with ID, and participants were distributed among all ID classifications (Table 1). This study was approved by the IRB at Virginia Tech, and informed consent was obtained from legal guardians, doctors, and SWVTC staff. Medical histories were obtained, and participants were excluded if they had a history of surgery on their feet, ankles, knees, hips, neck, or back. Arthritis, osteoporosis, uncorrected vision problems, vertigo, peripheral neuropathy, or a history of shortness of breath, chronic fatigue, Parkinson’s disease, or dementia were all additional causes for exclusion. Participants also had to be capable of sustained, unassisted walking.
Table 1.
Intellectual disability (ID) group participant information.
| Participant ID | ID Classification ∓ | Concomitant Disorders |
|---|---|---|
| P01 | Severe | Impulse control disorder |
| P02 | Severe | Autism |
| P03 | Profound | Bipolar, depressed |
| P04 | Severe | Generalized anxiety |
| P05 | Moderate | Personality disorder (unspecified) |
| P06 | Severe | Disruptive behavior disorder, microcephaly, seizure disorder, sleep apnea, hypertension |
| P07 | Severe | Personality disorder (unspecified), histrionic traits |
| P08 | Severe | Undifferentiated schizophrenia |
| P09 | Mild | Dysthymia |
| P10 | Profound | Psychotic disorder due to seizures with hallucinations |
| P11 | Severe | None |
| P12 | Moderate | Personality disorder (unspecified), antisocial, narcissism |
| P13 | Moderate | Impulse control disorder, hypertension, seizure disorder |
| P14 | Moderate | Autism |
| P15 | Profound | None |
Based on Intelligence Quotient (IQ). Mild = 55 ≤ IQ ≤ 69; Moderate = 40 ≤ IQ ≤ 54; Severe = 25 ≤ IQ ≤ 39; Profound = IQ < 25.
The control group was selected from archived data and included 15 non-ID, age- and gender-matched adults (11 males, 4 females, 39.2 ± 10.4 years, 174.5 ± 9.7 cm, 73.9 ± 15.7 kg). The standard deviation of the signed age difference between the matched pairs was 4.5 years. Each of these 15 control participants had been involved in a prior research study at the Locomotion Research Lab (Liu and Lockhart, 2006), had met the same medical history requirements, and experienced the same normal walking and slip perturbation conditions to be described.
2.2 Protocols
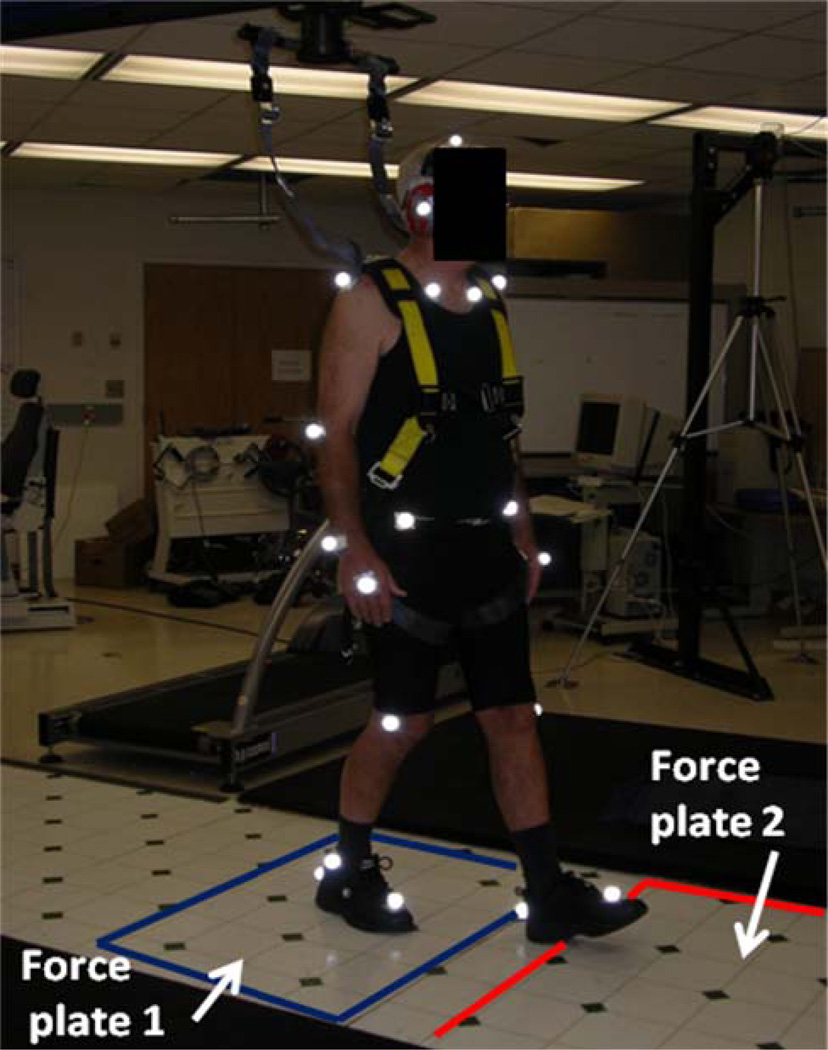
Gait characteristics were determined from ground reaction force and motion analysis data collected while participants walked over an instrumented, vinyl-covered walkway at a self-selected pace. The linear walkway (1.5m × 15.5m) was equipped with 2 force plates (Bertec Corporation, Columbus, OH) embedded in the center of the walkway (Figure 1). Participants wore laboratory clothing and shoes to eliminate effects of individual shoe type or wear. A set of 23 retro-reflective markers were used (Lockhart et al., 2003), and a six-camera Pro-Reflex motion analysis system (Qualysis, East Windsor, CT, USA) collected kinematic data at 120 Hz. An external trigger enabled simultaneous collection of kinetic data at a sampling rate of 1200 Hz using LabVIEW™ system software (National Instruments, Inc., Austin, TX, USA). An overhead fall-arresting harness was used at all times to prevent injury from an unexpected fall.
Figure 1.
Experimental setup.
Prior to the experiment, participants were told they may encounter a slippery surface during testing. Participants then walked continuously for approximately 10 minutes prior to data collection to allow them time to acclimatize to the testing apparatus. At all times, SWVTC staff was present to comfort participants and also to provide mild distraction. The control group had performed a counting task while focusing on a screen located at the end of the walkway. Because many ID participants were unable to perform this task, conversation with the SWVTC staff was used to achieve the same effect of directing attention forward and shifting focus from the primary walking task. Staff members provided confirmation of natural gait before data collection began. Following the warm-up period, participants continued walking as 6–10 trials were collected.
For the slip trial, the vinyl floor surface overlying the second force plate was replaced, via a sliding hidden floor mechanism, with an identical floor surface (84cm × 105cm) coated with a slippery, gel-based solution (dynamic coefficient-of-friction ≈ 0.07). This switch was done without the participant’s knowledge. A final data trial was recorded as participants encountered the slip hazard. Second slip perturbations were attempted only when the first perturbation was unsuccessful at eliciting a slip response due to improper foot placement.
2.3 Data Processing and Dependent Variables
The archived control data for normal walking consisted of a single representative trial, as the control data also included a slip trial. The trial selected was the first for which critical markers were visible and a clear, single footfall occurred on the second force plate as confirmed by vertical ground reaction forces.
Kinematic and kinetic data for all trials analyzed were smoothed using a 4th order, zero-lag Butterworth filter with a 6 Hz cutoff frequency (residual analysis determined cutoff frequency). Analysis of normal walking trials included determination of walking speed, step length, heel contact velocity, required coefficient of friction, and sagittal plane knee and ankle angles at heel contact. Walking speed (WS) was calculated over the duration of the trial for which the hip markers were visible. Step length (SL) was the distance, in the direction of progression, between consecutive right and left heel contacts. SL was averaged for three consecutive steps preceding contact with the second force plate. Heel contacts were identified by minima of the heel marker data.
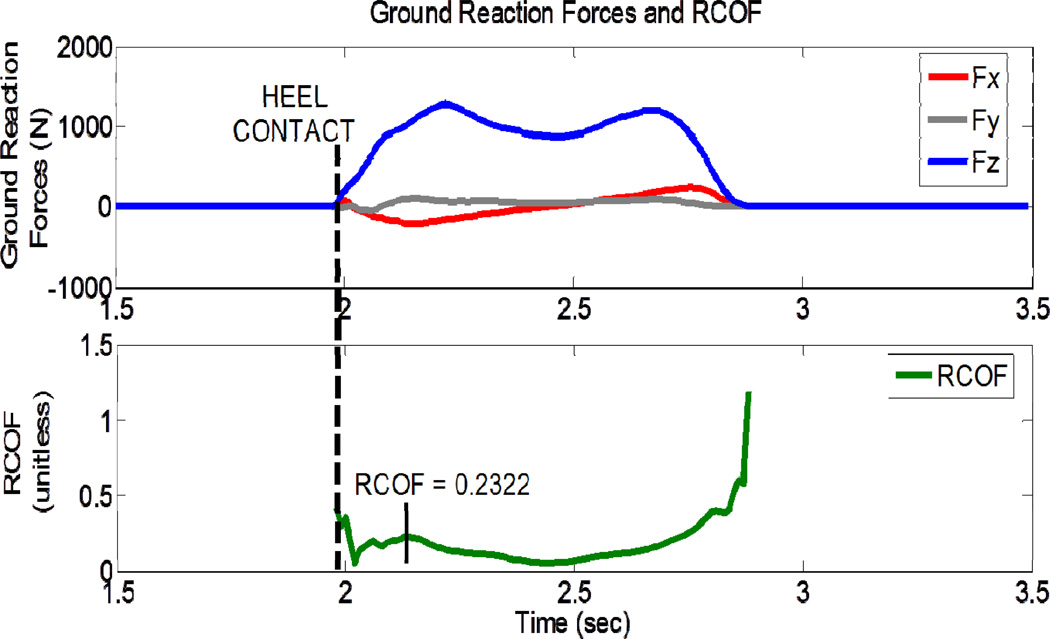
The remaining measures related to the instant of heel contact on the second force plate. Heel contact was defined as the instant vertical ground reaction forces exceeded 10 N. Heel contact velocity (HCV) was the instantaneous anteroposterior velocity of the heel between time epochs 1/60 second prior to and following heel contact. Knee flexion and ankle dorsiflexion angles were determined using the approach described by Winter (1991) and the hip joint center corrections of Seidel et al. (1995). Required coefficient of friction (RCOF), a slip-propensity measure indicating slip potential (Redfern et al., 2001), was the ratio of the horizontal shear force to the vertical ground reaction force (Figure 2). The RCOF value of interest is the absolute value of the peak occurring about 50–100 ms after heel contact (Perkins, 1978; Lockhart et al., 2003). Greater RCOF values indicate greater potential for slip initiation.
Figure 2.
Determination of required coefficient of friction (RCOF =(√(Fx2 + Fy2)/Fz)). The top graph shows the mediolateral (Fy) and anteroposterior (Fx) shear forces and the vertical ground reaction force (Fz), during stance, and the bottom graph displays the ratio of horizontal shear force divided by vertical ground reaction force throughout stance. RCOF is defined by the absolute value of the second peak after heel contact.
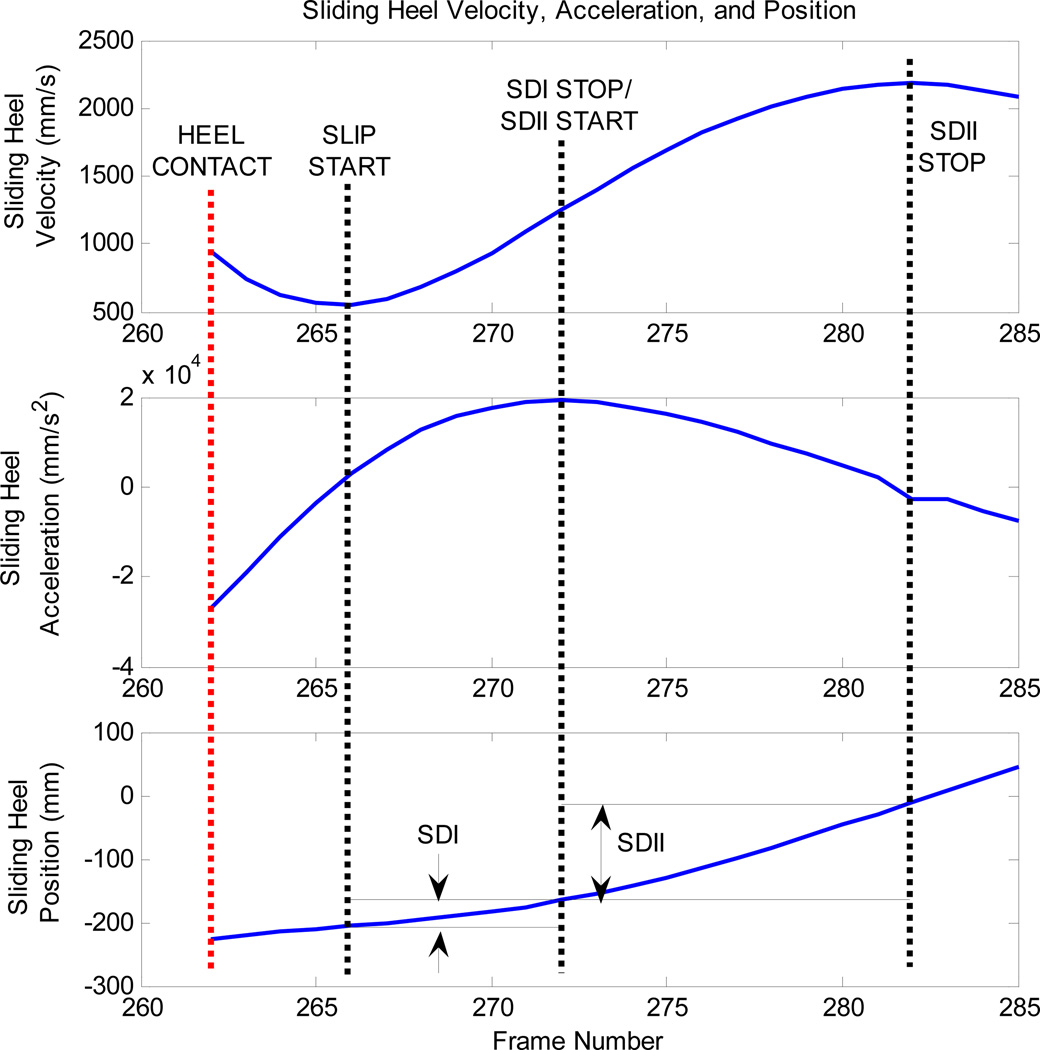
Slip trial analysis included measures of walking speed (calculated from the instant the hip markers appeared to the time of heel contact with the first force plate) and, step length as well as two slip severity parameters including initial slip distance (SDI) and slip distance II (SDII) (Lockhart et al., 2003). SDI is the distance traveled before the sliding heel velocity is effectively controlled by the recovery reaction. SDII then describes the distance covered before the reactive recovery response begins to slow the foot. The start and endpoints for SDI and SDII are defined by features of the anteroposterior motion of the sliding heel. SDI begins after heel contact when the first forward acceleration of the foot is identified (Slip Start) and ends at the time of the first peak in heel acceleration (SDI Stop; Figure 3). Slip distance II begins at the point of SDI Stop. The endpoint for SDII (SDII Stop) is the first maximum in forward heel velocity after the start of SDII. Both slip distances are calculated in the horizontal plane using the straight-line general distance formula and the mediolateral and anteroposterior positions of the heel.
Figure 3.
Determination of slip distance endpoints. SDI and SDII are calculated as the displacement of the heel in the transverse plane between these bounds. Figure has been adapted from Lockhart et al. (2003).
2.4 Statistical Analyses
Statistical analyses of between-group differences in normal gait parameters involved independent t-tests with an alpha value set to 0.05. Additional paired t-tests were conducted within groups to verify that walking speed and step length were consistent between normal walking and slip trials (SDI and SDII). Finally, Analysis of Covariance (ANCOVA) was performed with walking speed as the covariate to determine if significant group differences exist while accounting for differences in walking speed.
3.0 RESULTS
In the initial independent t-tests, the ID group exhibited a significantly slower walking speed and shorter step length than the controls (Table 2). The ID group was also found to have a significantly lower RCOF (Table 2). Both joint angles at heel contact as well as heel contact velocity failed to reveal statistically significant differences between groups (Table 2).
Table 2.
Between group comparison of gait parameters (mean (SD)).
| ID | Control | p-values | ||
|---|---|---|---|---|
| n = 15 | n = 15 | t-test | ANCOVA | |
| WS (cm/s) | 61.7 (21.2) | 137.2 (15.1) | < 0.0001* | N/A |
| SL (cm) | 51.4 (14.5) | 76.5 (7.2) | < 0.0001* | 0.0216* |
| HCV (cm/s) | 72.7 (35.2) | 94.5 (23.0) | 0.0557 | 0.2442 |
| KAHC (deg) | 15.7 (10.4) | 9.6 (7.9) | 0.0810 | 0.0473* |
| AAHC (deg) | 12.1 (8.7) | 10.6 (3.5) | 0.5295 | 0.1774 |
| RCOF | 0.17 (0.04) | 0.21 (0.04) | 0.0225* | 0.9034 |
Variables are walking speed (WS) – also covariate, step length (SL), heel contact velocity (HCV), knee angle at heel contact (KAHC), ankle angle at heel contact (AAHC), and required coefficient of friction (RCOF: a slip-propensity measure indicating slip potential is the ratio of the horizontal shear force to the vertical ground reaction force).
denotes statistical significance of p < 0.05. ID denotes intellectual disability group.
After accounting for between-group differences in walking speed using ANCOVA, step length remained significantly lower for the ID group than the controls. Group differences in RCOF, however, failed to be significant following the ANCOVA, but statistical significance emerged for differences in knee angle at heel contact (Table 2).
Significant group differences were found for both slip distance measures (Table 3) with the ID group exhibiting greater SDI and SDII slip distances than the controls. As a qualitative comparison of potentially dangerous slips experienced by each group, hazardous slips were defined using a threshold of SDI ≥ 10 cm (Strandberg & Lanshammar, 1981). Using this criterion, the ID group experienced 6 hazardous slips while the control group had only 3. Of those in the ID group experiencing a hazardous slip, 3 had been diagnosed with moderate ID, and the other 3 had been diagnosed with each of mild, severe, and profound ID.
Table 3.
Slip parameters between groups (mean(SD)).
| ID | Control | ||
|---|---|---|---|
| n = 15 | n = 15 | p-value | |
| SDI (cm) | 10.0 (6.7) | 4.8 (4.4) | 0.0173* |
| SDII (cm) | 7.1 (6.8) | 2.9 (3.1) | 0.0426* |
Variables are slip distance I (SDI), slip distance II (SDII).
denotes statistical significance of p < 0.05. ID denotes intellectual disability group.
Within-subjects paired t-tests confirmed that walking speed and step length were not significantly different between normal walking and slip trials for either group (Table 4).
Table 4.
Within-group analysis of walking speed (WS) and step length (SL). ID denotes intellectual disability group.
| Normal Walk | Slip | ||
|---|---|---|---|
| n = 15 | n = 15 | p-value | |
| WS (cm/s) | |||
| ID | 61.7 (21.2) | 65.4 (20.6) | 0.6328 |
| Control | 137.2 (15.1) | 129.9 (21.0) | 0.2849 |
| SL (cm) | |||
| ID | 51.4 (14.5) | 62.3 (32.6) | 0.2442 |
| Control | 76.5 (7.2) | 84.7 (24.5) | 0.2553 |
4.0 DISCUSSION
4.1 Gait Characteristics and Joint Angle Comparison
The goal of this study was to provide a quantitative comparison of gait for adults with ID to understand possible biomechanical contributions to falls in this population. Results indicate that the ID group had a significantly slower walking speed than the controls. This differs from previous findings by Sparrow et al. (1998) who reported no differences in walking speed between ID and control groups for obstacle negotiation tasks. This discrepancy may be attributed to differences in walking tasks (i.e., obstacle negotiations vs. normal walking conditions).
In addition to the difference in walking speed, initial t-test analyses indicated that the ID group exhibited significantly shorter SL and lower RCOF. Shorter SL and lower RCOF are adaptations known to reduce the likelihood of slip initiation (Lockhart et al., 2003; Cham and Redfern, 2002). Together with slower walking speeds, these gait parameters would suggest less potential for slip initiation among the ID group compared to controls. After accounting for group difference in walking speed, however, RCOF was not significantly different suggesting that at least an equal likelihood of slip initiation between groups. SL remained significantly different with the ID group having shorter step lengths.
Shorter step lengths permit the COM to remain in a more forward position with respect to the lead foot and provide protection against a backwards loss of balance during slip (Bhatt et al., 2005). However, slower walking velocity and the forward displacement of the COM afforded by shorter step lengths may not be sufficient to overcome the backward transition of the COM when a slip occurs at heel contact (Bhatt et al., 2005). Thus, reductions in walking speed and step length seen within the ID group may be an effort to resist loss of balance, but once slipping does begin, their more slowly transitioning COM may contribute to an inability to recover.
Joint angles at heel contact were also determined to compare posture-related slip potential at heel contact. Larger step lengths, larger foot-floor angles, and larger foot-floor angular velocities are all associated with hazardous slips (Moyer et al., 2006). Heel strike angle has also been shown to be a significant predictor of whether a slip results in a fall (Brady et al., 2000). The present study found significant differences in knee flexion angle at heel contact after accounting for group differences in walking speed. Increased knee flexion at heel contact has also been observed in the elderly as compared to young adults (Begg and Sparrow, 2006) and is thought to ease the transfer of the COM onto the lead leg. Greater knee flexion coupled with slower walking speeds and shorter step lengths suggests adults with ID exhibit a more cautious gait pattern than controls. Therefore, slip-related falls in the ID population are more likely due to an insufficient recovery response than to differences in gait characteristics. However, Sparrow et al. (1998) also suggests that adults with ID exhibit greater variability of gait parameters. Variability of movement within the ID group may be worth studying independently as a contributor to falls for the ID population.
4.2 Slip Characteristics
Initiation, detection, and response are the three phases of slip-related falls (Lockhart et al., 2005). Initiation refers to gait characteristics that predispose a person to slip. Detection describes the phase in which the body recognizes the slip perturbation through feedback from the visual, vestibular, and proprioceptive systems. Finally, response refers to the physical reaction to a slip. Within-group analyses determined that step length and walking speed were consistent between the normal walking and slip distance trials. Therefore, the slip perturbations were likely unanticipated and representative of a real-life slip. Longer SDI and SDII indicate poorer slip detection and either a delayed slip recovery or an insufficient reactive recovery response, respectively. A previous study reported that those with ID have delayed responses to postural perturbations (Hale et al., 2009). In the present study, the ID group displayed greater SDI and SDII values than the controls. This provides further support to the argument that slip-related fall occurrence for adults with ID may be due to insufficient recovery rather than an increased risk of slip initiation. Slip detection or active slip response may be delayed or lacking in the ID group contributing to more fall accidents.
4.3 Limitations
There were a few limitations in this study. The first is that intellectual disability is often accompanied by concurrent disorders (Table 1). These conditions could potentially influence gait characteristics. SWVTC staff members were present to confirm the participants’ typical gait pattern.
Normal walking gait analysis was done using a single trial from each participant as discussed in the Methods section. Standardization of trial selection, however, helped to limit bias in the analysis. Another limitation is that four second-attempt slip trials were included in the analysis (3 among the ID group, 1 among the controls). To minimize effects of anticipation, several normal walking trials were performed prior to the second perturbation. Walking speed and step length were equivalent for normal walking and slip trials indicating that the participants did not change their gait and were not aware of the impending slippery floor surface (Lockhart et al., 2003).
4.4 Summary
In summary, this study compared gait and slip characteristics between healthy adults with ID and healthy age- and gender-matched controls. Considering gait characteristics alone, results suggest that ID adults are no more likely to experience slip initiation than adults with ID. Instead, analysis of slip distance parameters suggests that falls for the ID group may be due to deficiencies in the detection and response phases of slip. This finding agrees with those of Hale et al. (2009) who found delayed reactions to balance perturbations in adults with ID. Future analysis should include electromyography analysis to compare muscle activation patterns during a slip. This could address whether sub-optimal magnitudes of muscle contraction or greater delays in muscle force development (Tang and Woollacott, 1998a & 1998b) are present. Previous studies have reported improved balance and mobility and decreased fall rates in the elderly following exercise training (Rubenstein et al., 2000; Judge et al., 1993; Weerdesteyn et al., 2006). Future studies should determine whether physical training interventions can improve slip response and reduce falls in the ID population.
Acknowledgements
Funding from the NSF (grant #CBET-0756058) and NIOSH (grant #CDC/NIOSH-R01-OH009222) supported the research. We gratefully acknowledge Jian Liu, Sukwon Kim, and Prakriti Parijat for their assistance in data acquisition.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest
None
References
- Agiovlasitis S, Yun K, Pavol M, McCubbin J, Kim S. Gait transitions of persons with and without intellectual disability. Research Quarterly for Exercise and Sport. 2008;79(4):487–494. doi: 10.1080/02701367.2008.10599515. [DOI] [PubMed] [Google Scholar]
- Begg RK, Sparrow WA. Ageing effects on knee and ankle joint angles at key events and phases of the gait cycle. J Med Eng & Technol. 2006;30(6):382–389. doi: 10.1080/03091900500445353. [DOI] [PubMed] [Google Scholar]
- Bhatt T, Wening JD, Pai Y-C. Influence of gait speed on stability: recovery from anterior slips and compensatory stepping. Gait & Post. 2005;21(2):146–156. doi: 10.1016/j.gaitpost.2004.01.008. [DOI] [PubMed] [Google Scholar]
- Brady RA, Pavol MJ, Owings TM, Grabiner MD. Foot displacement but not velocity predicts the outcome of a slip induced in young subjects while walking. J Biomech. 2000;33:803–808. doi: 10.1016/s0021-9290(00)00037-3. [DOI] [PubMed] [Google Scholar]
- Bruckner J, Herge EA. Assessing the risk of falls in elders with mental retardation and developmental disabilities. Topics in Geriatr Rehab. 2003;19(3):206–211. [Google Scholar]
- Carmeli E, Zinger-Vaknin T, Morad M, Merrick J. Can physical training have an effect on well-being in adults with mild intellectual disability? Mechanisms of Ageing and Development. 2005;126:299–304. doi: 10.1016/j.mad.2004.08.021. [DOI] [PubMed] [Google Scholar]
- Carmeli E, Bar-Yossef T, Ariav C, Paz R, Sabbag H, Levy R. Sensorimotor impairments and strategies in adults with intellectual disabilities. Motor Control. 2008;12:348–361. doi: 10.1123/mcj.12.4.348. [DOI] [PubMed] [Google Scholar]
- Cham R, Redfern MS. Changes in gait when anticipating slippery floors. Gait & Post. 2002;15:159–171. doi: 10.1016/s0966-6362(01)00150-3. [DOI] [PubMed] [Google Scholar]
- Cleaver S, Hunter D, Ouellette-Kuntz H. Physical mobility limitations in adults with intellectual disabilities: a systematic review. J Intellectual Disabil Res. 2009;53(2):93–105. doi: 10.1111/j.1365-2788.2008.01137.x. [DOI] [PubMed] [Google Scholar]
- Frzovic D, Morris ME, Vowels L. Clinical tests of standing balance: performance of persons with multiple sclerosis. Arch Phys Med Rehabil. 2000;81:215–221. doi: 10.1016/s0003-9993(00)90144-8. [DOI] [PubMed] [Google Scholar]
- Hale L, Bray A, Littmann A. Assessing the balance capabilities of people with profound intellectual disabilities who have experienced a fall. JIDR. 2007;51(4):260–268. doi: 10.1111/j.1365-2788.2006.00873.x. [DOI] [PubMed] [Google Scholar]
- Hale L, Miller R, Barach A, Skinner M, Gray A. Motor control test responses to balance perturbations in adults with an intellectual disability. JIDD. 2009;34(1):81–86. doi: 10.1080/13668250802683810. [DOI] [PubMed] [Google Scholar]
- Hsieh K, Heller T, Miller AB. Risk factors for injuries and falls among adults with developmental disabilities. JIDR. 2001;45(1):76–82. doi: 10.1046/j.1365-2788.2001.00277.x. [DOI] [PubMed] [Google Scholar]
- Judge J, Lindsey C, Underwood M, Winsemius D. Balance improvements in older women: effects of exercise training. Phys Ther. 1993;73(4):254–264. doi: 10.1093/ptj/73.4.254. [DOI] [PubMed] [Google Scholar]
- Liu J, Lockhart TE. Comparison of 3D joint moments using local and global inverse dynamics approached among three different age groups. Gait & Posture. 2006;23(4):480–485. doi: 10.1016/j.gaitpost.2005.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lockhart TE, Smith JL, Woldstad JC. Effects of aging on the biomechanics of slips and falls. Human Factors. 2005;47(4):708–729. doi: 10.1518/001872005775571014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lockhart TE, Woldstad JC, Smith JL. Effects of age-related gait changes on the biomechanics of slips and falls. Ergonomics. 2003;46(12):1136–1160. doi: 10.1080/0014013031000139491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moyer BE, Chambers AJ, Redfern MS, Cham R. Gait parameters as predictors of slip severity in younger and older adults. Ergonomics. 2006;4(15):329–343. doi: 10.1080/00140130500478553. [DOI] [PubMed] [Google Scholar]
- Perkins PJ. Measurement of slip between the shoe and ground during walking. American Society of Testing Materials, Special Technical Publication. 1978;649:71–87. [Google Scholar]
- Plotnik M, Giladi N, Hausdorff JM. Bilateral coordination of walking and freezing of gait in Parkinson’s disease. European Journal of Neuroscience. 2007;27(8):1999–2006. doi: 10.1111/j.1460-9568.2008.06167.x. [DOI] [PubMed] [Google Scholar]
- Rubenstein LZ, Josephson KR, Trueblood PR, Loy S, Harker JO, Pietruszka FM, Robbins AS. Effects of a group exercise program on strength, mobility, and falls among fall-prone elderly men. J Gerentol. 2000;55A(6):M317–M321. doi: 10.1093/gerona/55.6.m317. [DOI] [PubMed] [Google Scholar]
- Redfern MS, Cham R, Gielo-Perczak K, Gronqvist R, Hirvonen M, Lanshammar H, Marpet M, Pai CYC, Powers C. Biomechanics of slips. Ergonomics. 2001;44(13):1138–1166. doi: 10.1080/00140130110085547. [DOI] [PubMed] [Google Scholar]
- Seidel GK, Marchinda DM, Dijkers M, Soutas-Little RW. Hip joint center location from palpable bony landmarks – a cadaver study. J Biomechanics. 1995;28(8):995–998. doi: 10.1016/0021-9290(94)00149-x. [DOI] [PubMed] [Google Scholar]
- Sherrard J, Tonge BJ, Ozanne-Smith J. Injury in young people with intellectual disability: descriptive epidemiology. Inj Prev. 2001;7:56–61. doi: 10.1136/ip.7.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherrard J, Tonge BJ, Ozanne-Smith J. Injury risk in young people with intellectual disabililty. JIDR. 2002;46(1):6–16. doi: 10.1046/j.1365-2788.2002.00346.x. [DOI] [PubMed] [Google Scholar]
- Sparrow WA, Shinkfield AJ, Summers JJ. Gait characteristics in individuals with mental retardation: unobstructed level-walking, negotiating obstacles, and stair climbing. Human Move Sci. 1998;17:167–187. [Google Scholar]
- Strandberg L, Lanshammar H. The dynamics of slipping accidents. J Occup Accidents. 1981;3:153–162. [Google Scholar]
- Tang PF, Woollacott MH. Inefficient postural responses to unexpected slips during walking in older adults. J Gerontol Med Sci. 1998a;53(A):M471–M480. doi: 10.1093/gerona/53a.6.m471. [DOI] [PubMed] [Google Scholar]
- Tang PF, Woollacott MH, Chong RKY. Control of reactive balance adjustments in perturbed human walking: roles of proximal and distal postural muscle activity. Exp Brain Res. 1998b;119:141–152. doi: 10.1007/s002210050327. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. Americans with Disabilities: 2005. U.S. Department of Commerce; 2008. Retrieved November 14, 2011. http://www.census.gov/prod/2008pubs/p70-117.pdf. [Google Scholar]
- Weerdesteyn V, Rijken H, Geurts ACH, Smits-Engelsman BCM, Mulder T, Duysens J. A five-week exercise program can reduce falls and improve obstacle avoidance in the elderly. Gerentol. 2005;52:131–141. doi: 10.1159/000091822. [DOI] [PubMed] [Google Scholar]
- Winter DA. The Biomechanics and Motor Control of Human Gait: Normal, Elderly and Pathological. Waterloo Biomechanics, Graphic Services; 1991. [Google Scholar]
- Wittwer JE, Webster KE, Andrews PT, Menz HB. Test-retest reliability of spatial and temporal gait parameters of people with Alzheimer’s disease. Gait Post. 2008;28(3):392–396. doi: 10.1016/j.gaitpost.2008.01.007. [DOI] [PubMed] [Google Scholar]