Abstract
Objective
To investigate the feasibility of using noninvasive EEG source imaging approach to image continuous seizure activity in pediatric epilepsy patients.
Methods
Nine pediatric patients with medically intractable epilepsy were included in this study. Eight of the patients had extratemporal lobe epilepsy and one had temporal lobe epilepsy. All of the patients underwent resective surgery and seven of them underwent intracranial EEG (iEEG) monitoring. The ictal EEG was analyzed using a noninvasive dynamic seizure imaging (DSI) approach. The DSI approach separates scalp EEGs into independent components and extracts the spatio-temporal ictal features to achieve dynamic imaging of seizure sources. Surgical resection and intracranial recordings were used to validate the noninvasive imaging results.
Results
The DSI determined seizure onset zones (SOZs) in these patients were localized within or in close vicinity to the surgically resected region. In the seven patients with intracranial monitoring, the estimated seizure onset sources were concordant with the seizure onset zones of iEEG. The DSI also localized the multiple foci involved in the later seizure propagation, which were confirmed by the iEEG recordings.
Conclusions
Dynamic seizure imaging can noninvasively image the seizure activations in pediatric patients with both temporal and extratemporal lobe epilepsy.
Significance
EEG seizure imaging can potentially be used to noninvasively image the SOZs and aid the pre-surgical planning in pediatric epilepsy patients.
Keywords: Pediatric patients, Epilepsy, EEG, Dynamic seizure imaging, Intracranial recording, Surgical resection
1. Introduction
Epilepsy is one of the most important chronic neurological diseases that affect children. Approximately 0.5% to 1% of all children under 16 years experience seizure events (Shinnar and Pellock, 2002). Children that suffer from epilepsy may face intellectual developmental issues and encounter other brain developmental problems. Seizure control and treatment are of vital importance to pediatric patients in order to improve their quality of life as well as ensure normal brain development. In contrast to adult patients, pediatric patients are more likely to experience seizures that originate from extratemporal lobe regions, which tend to have a less favorable surgical outcome compared to temporal lobe epilepsy (Gilliam et al., 1997; Sperli et al., 2006). It is thus important to accurately localize the epileptogenic zone of pediatric epilepsy patients in order to achieve improved surgery success.
Pre-surgical planning techniques from multiple aspects are necessary in order to plan a successful surgical resection. Among various techniques, intracranial recordings including electrocorticography (ECoG) and depth electrode recordings are still the gold standards to identify the seizure onset zones (Engel, 1987; Lai et al., 2007; Wilke et al., 2009, 2010, 2011). However, as iEEG has been restricted by its invasive nature and limited spatial coverage, noninvasive structural and functional imaging techniques, such as magnetic resonance imaging (MRI), positron emission tomography (PET), and single photon emission computed tomography (SPECT), have been actively developed and utilized to delineate the epileptogenic zones. Due to the limited temporal resolution and uncertain correlation between the imaging response and neuronal activity, these techniques alone may not provide sufficient information to identify the seizure onset zone. Additional information from other imaging modalities is thus necessary to fully understand the epileptic brains and identify the epileptogenic zones.
Scalp EEG has been widely used in clinical settings to characterize seizure activity in epilepsy patients. Patients typically undergo long-term video EEG monitoring to capture their seizures and to help lateralize or localize seizure onset regions. The recent advancement in the EEG source imaging techniques has made it possible to study the activity in the brain source space in addition to the traditional scalp EEG trace inspection. Many studies have shown the capability of EEG source imaging to localize the brain sources associated with interictal epileptiform discharges (He et al., 1987; Ebersole, 2000; Lantz et al., 2003; Zhang et al., 2003; Michel et al., 2004; Gavaret et al., 2004; Sperli et al., 2006; Plummer et al., 2008; Brodbeck et al., 2010; Wang et al., 2010; Lai et al., 2011). Imaging of seizure activity still remains a major challenge due to the various types of ictal patterns and contamination of motion artifacts in EEG (Assaf and Ebersole, 1997; Worrell et al., 2000; Lantz et al., 2001; Ding et al., 2007; Koessler et al., 2010; Yang et al., 2011; He et al., 2011). Among the seizure imaging studies, temporal lobe epilepsy is the most investigated epilepsy type. In the present study, we investigate the feasibility of using a dynamic seizure imaging technique to identify seizure generators in pediatric epilepsy patients. To evaluate the source imaging results, we compare the estimated source with surgical resections and intracranial recordings of the patients.
2. Methods
2.1 Patients and data analysis
The study design is illustrated in Fig. 1. Nine pediatric patients with drug-resistant partial epilepsy were included in this study. The pediatric patients were selected according to the following criteria: (1) seizures were captured during the long-term EEG recording, (2) pre-surgical MRI images were scanned, (3) the patient underwent resective surgery and the age of patient was below nineteen when the surgery was performed, (4) the patient had either a post-operative MRI scan or intracranial recordings. The patients were studied under the approved protocol by the Institutional Review Boards of the University of Minnesota and the Mayo Clinic. The clinical information for these patients is included in Table 1.
Fig. 1.
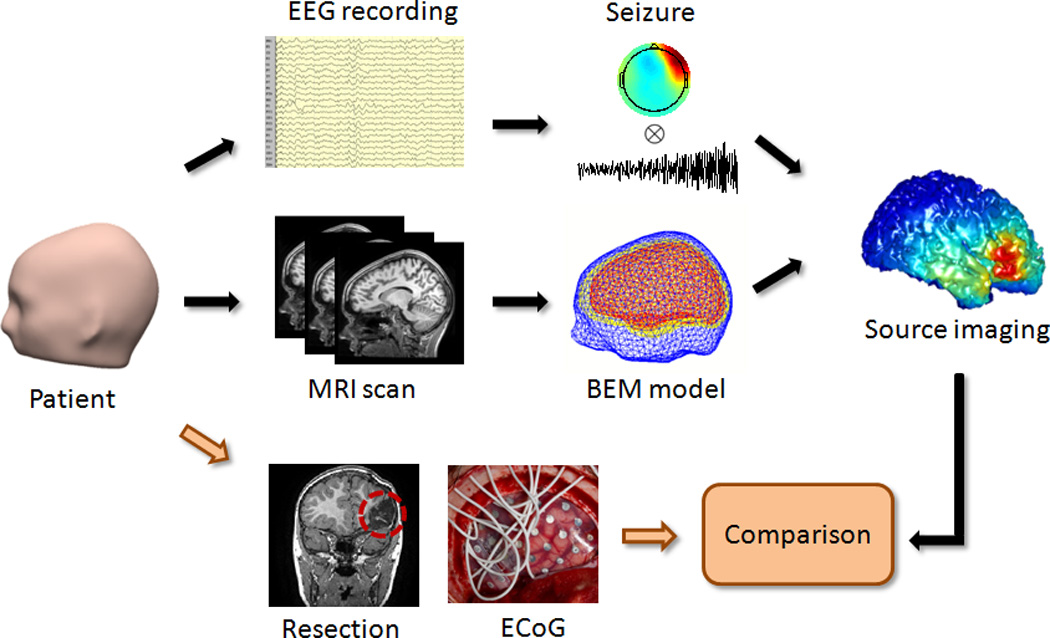
Schematic diagram of seizure source imaging and the study design. Seizure activity from scalp EEG recordings was analyzed to image seizure sources. Patient-specific boundary element head models were created from the pre-operative MRI images of the patients. Surgical resections and intracranial recordings were used to validate the seizure source imaging results.
Table 1.
Clinical information for all pediatric patients.
| Patient | Age at onset |
Age | MRI | SPECT |
|---|---|---|---|---|
| 1 | 10 months |
2 | Normal | Inferolateral right frontal lobe; left inframedial occipital lobe |
| 2 | 1 month |
16 | Parieto-occipital encephalomalacia |
Anterior commissure, right intraparietal sulcus, and lateral left occipital lobe |
| 3 | - | 18 | left frontal cortical dysplasia or subcortical gliosis |
- |
| 4 | 7 | 9 | Mild Chiari I malformation |
Mild increase in anterior right cingulate cortex |
| 5 | 6 | 17 | Normal | No clear focus |
| 6 | 13 | 16 | Normal | Mesial right temporal, right frontal cortex, and right basal ganglia |
| 7 | 5 | 10 | Right frontal hemorrhage related to cavernoma |
Bilateral left more than right frontal, and right temporal lobe |
| 8 | 7 | 12 | Left hippocampal atrophy |
- |
| 9 | 4 | 5 | Normal | - |
The pre-surgical scalp EEG in the patients was recorded using a long-term video monitoring system. The EEG data were filtered with a band-pass filter of 1–70Hz and sampled at 200 Hz. The scalp EEG was recorded with 32 channels and the electrodes were positioned according to the modified international 10–20 system. The EEG data were carefully reviewed and seizures marked by experienced epileptologists. High resolution structural magnetic resonance imaging was also performed in all of these patients before their surgery. These MRI images (voxel size: 0.9375* 0.9375* 1.0 mm3) were obtained from a 1.5 Tesla or 3 Tesla GE Signa scanner (General Electric Medical Systems, Milwaukee, WI). Patient-specific realistic geometry boundary element method (BEM) head models (He et al., 1987; Hämäläinen and Sarvas, 1989) were constructed from the MRI images using Curry software (Compumedics, Charlotte, NC).
2.2 Dynamic seizure imaging
The dynamic seizure imaging (DSI) approach separates the scalp EEG into independent components (ICs) in sensor space and recombines seizure components in the source space to form a spatiotemporal reconstruction of the seizure activity (Yang et al., 2011). The scalp EEG is a mixture of activity from various sources, which include functional cortical activations, background brain activity, artifacts and measurement noise. In the analysis, the seizure EEG was decomposed into temporally independent and spatially fixed components using the independent component analysis (ICA) in the following format (Nam et al., 2002; Delorme and Makeig, 2004; Jung et al., 2009; Yang et al., 2011)
| (1) |
where Φ is the recorded scalp EEG, NC is the number of independent components, wi is the ith weighting element, and Mi and Ti represent the spatial map and temporal activation of ith component, respectively.
Components that correspond to artifacts, such as eye blinks and motion artifacts, were removed from the decomposed ICs (Jung et al., 2000). Components characterized by temporal-spectral patterns of ictal activity were selected for the source analysis. Correlations of spectrogram between IC components and scalp ictal EEG were computed. The spectrogram was calculated using a short-time Fourier transform with the time window of 200 samples and 50% overlapping. The empirical correlation distribution was then created for each IC by computing the spectrogram correlation of surrogated IC time series and EEG data (Yang et al., 2011). The ICs with significant correlation (p < 0.1) in the surrogated statistical test were selected. The IC components with more than 20% residual variances of dipole fitting were excluded for the seizure source imaging (Delorme and Makeig, 2004; Jung et al., 2009). After selecting the seizure components in Eq. (1), the ictal EEG Φ can be written as (where NS is the number of seizure components).
By solving the inverse problem, the estimated source activity Ŝ can thus be expressed as
| (2) |
where A−1 is the inverse of the transfer matrix A , Ŝi = A−1Mi is the estimated source for ith seizure component. The spatiotemporal source distribution Ŝ could then be obtained by combining the IC sources Ŝi and time courses Ti in the source domain. To estimate the Ŝi, the cortical current density model with unconstrained sources (Dale and Sereno, 1993) and minimum norm estimation (Hämäläinen and Ilmoniemi, 1984) were used to reconstruct the source distribution. The cortex was segmented from high-resolution structural MRI of the patients, and the transfer matrix was computed from the patient-specific realistic geometry BEM head model (Hämäläinen and Sarvas, 1989). The BEM model consisted of three layers (scalp, skull, brain) and the conductivities were set as 0.33 S/m, 0.0165 S/m, and 0.33 S/m, respectively (Oostendorp et al., 2000; Lai et al., 2005; Zhang et al., 2006).
2.3 Evaluation of imaging results
The seizure imaging results were obtained from the nine patients and the results were compared with the surgical resection of the patients. The estimated seizure sources were distributed over the cortical surface, and the cortical source location with the maximal source strength was considered as the location of the estimated seizure activity. All of the patients had both resective surgery and post-operative MRIs following the surgery. The surgically resected areas were segmented from the post-operative MRI images and used to evaluate the DSI results. The results were considered to be concordant to the surgical resection if the estimated source maximum was located within the resection regions.
In the seven patients with intracranial recordings, we quantitatively evaluated the seizure imaging results at seizure onset by comparing the location of the estimated sources with the SOZs of the intracranial recordings. The SOZs were identified from ECoG by experienced epileptologists. The accurate locations of the intracranial electrodes were segmented from CT images and co-registered with structural MRI images. The distance between the estimated source maximum and the nearest SOZ electrode was calculated. The unit of the distance was defined as the inter-electrode-distance, which was the distance between two adjacent ECoG electrodes. The estimated seizure activity following seizure onset were also displayed and qualitatively compared to the iEEG recordings.
3. Results
Nine pediatric patients with medically intractable epilepsy were analyzed in this study. Among the nine patients, eight of them experienced seizures from extratemporal lobes and one of them had seizures from temporal lobe. The seizure imaging results in all of the patients were evaluated by comparing them with the surgical resection zones of the patients. In seven patients who had intracranial ECoG recordings, the DSI determined SOZ was also compared with the SOZ determined from the intracranial recordings.
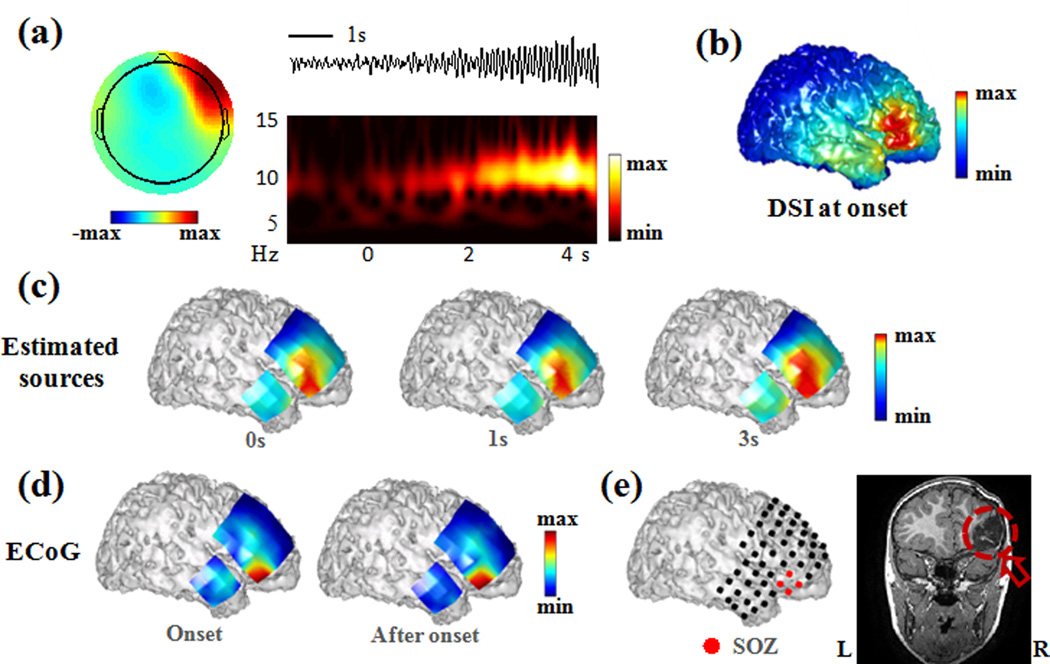
Patient 1 was a 2-year-old patient who had extratemporal lobe epilepsy. The seizures were characterized as paroxysmal fast activity in the frontotemporal head region. Fig. 2 shows the seizure imaging results of this patient in comparison with the surgical resection and the intracranial recording. Multiple seizure components were extracted and the seizure component showing the earliest ictal activation is shown in Fig. 2a. The scalp map suggests right frontotemporal focus of the activity. Both the time course and time-frequency representation show source activity at the alpha frequency band following the onset of the seizure. The cortical distribution of the estimated seizure activity (Fig. 2b) indicates seizure onset in the right lateral frontal region. Intracranial recordings were performed on this patient, which covered the right frontal lobe and right temporal lobe of the patient. Part of the estimated cortical source distribution that overlaps with the intracranial grids is plotted and projected onto the grid surface (Fig. 2c). Both estimated seizure sources, and the power distribution of recorded ECoG activity (Fig. 2d) show that the seizure was consistently active in the right lateral frontal lobe. The seizure onset zone marked on Fig. 2e shows that the seizure started from the right frontal grid of this patient. The red circle on the post-operative MRI image (Fig. 2e) shows that part of the right frontal lobe was removed during the surgery. These results suggest that the estimated seizure source in the right frontal lobe is in concordance with the surgically resected region and the SOZ that was delineated from the intracranial recordings.
Fig. 2.
Seizure source imaging results in Patient 1. (a) Example of scalp topography, activity, and time-frequency representation of a seizure component. (b) Estimated source at seizure onset. (c) Estimated seizure sources following seizure onset. The estimated sources were displayed by projecting them onto the cortical grid surface. (d) Power distribution of recorded ECoG activity following seizure onset. (e) Seizure onset zone (red color) marked on ECoG grid and surgical resection circled on post-operative MRI image of the patient.
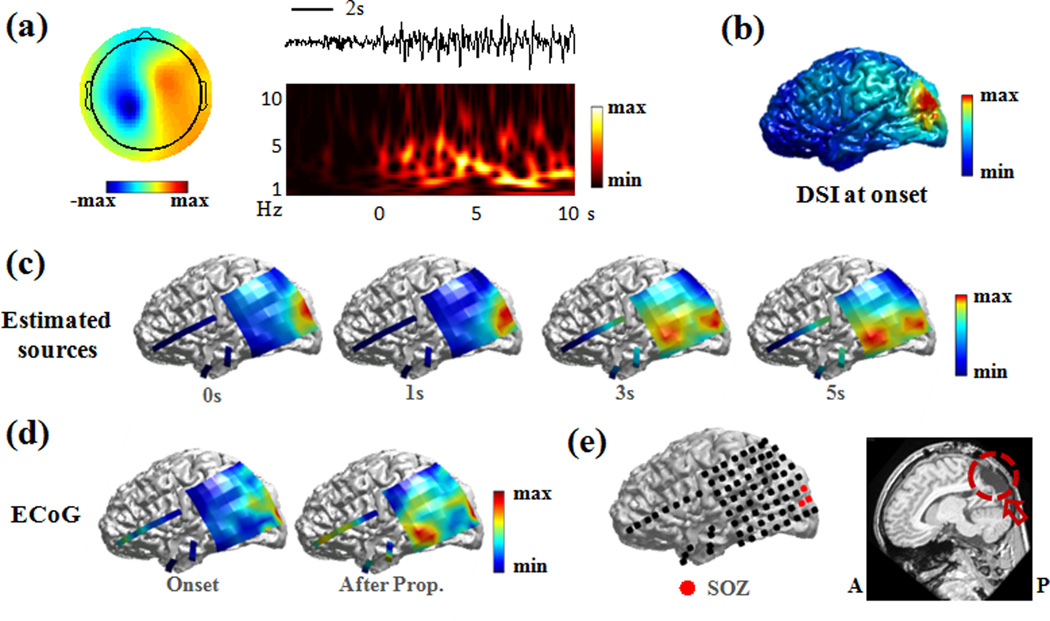
Patient 2 was another extratemporal lobe patient whose seizure activity involved multiple brain regions. The scalp EEG of the analyzed seizure showed occipital and temporal lobe activity. Multiple seizure components were extracted and the seizure component showing the earliest ictal activation is shown in Fig. 3a. The spatial map indicates parieto-occipital lobe focus of seizure activity. The time course and time-frequency representation show seizure activity in theta band following the seizure onset. The estimated seizure onset source over the cortex (Fig. 3b) shows that the seizure sources were activated in the occipital lobe of the patient. The seizure onset zone marked in Fig. 3e shows that the seizure started from the occipital region of this patient. The post-operative MRI image in Fig. 3e shows that part of the occipital region of this patient was resected during the surgery. The estimated sources in Fig. 3c show that the seizure sources were firstly activated in occipital lobe and then sources in the posterior temporal lobe were also activated, which was confirmed by the power distribution of the recorded seizure activity from intracranial electrodes (Fig. 3d). The seizure development involving multiple regions was successfully tracked by the seizure imaging approach. The estimated seizure onset source is located in the left occipital region and is concordant with the surgical resection and the SOZ determined from the intracranial recording.
Fig. 3.
Seizure source imaging results in Patient 2. (a) Example of scalp topography, activity, and time-frequency representation of a seizure component. (b) Estimated source at seizure onset. (c) Estimated seizure sources following seizure onset. The estimated sources were displayed by projecting them onto the cortical grid surface. (d) Power distribution of recorded ECoG activity at seizure onset and after propagation. (e) Seizure onset zone (red color) marked on ECoG grid and surgical resection circled on post-operative MRI image of the patient.
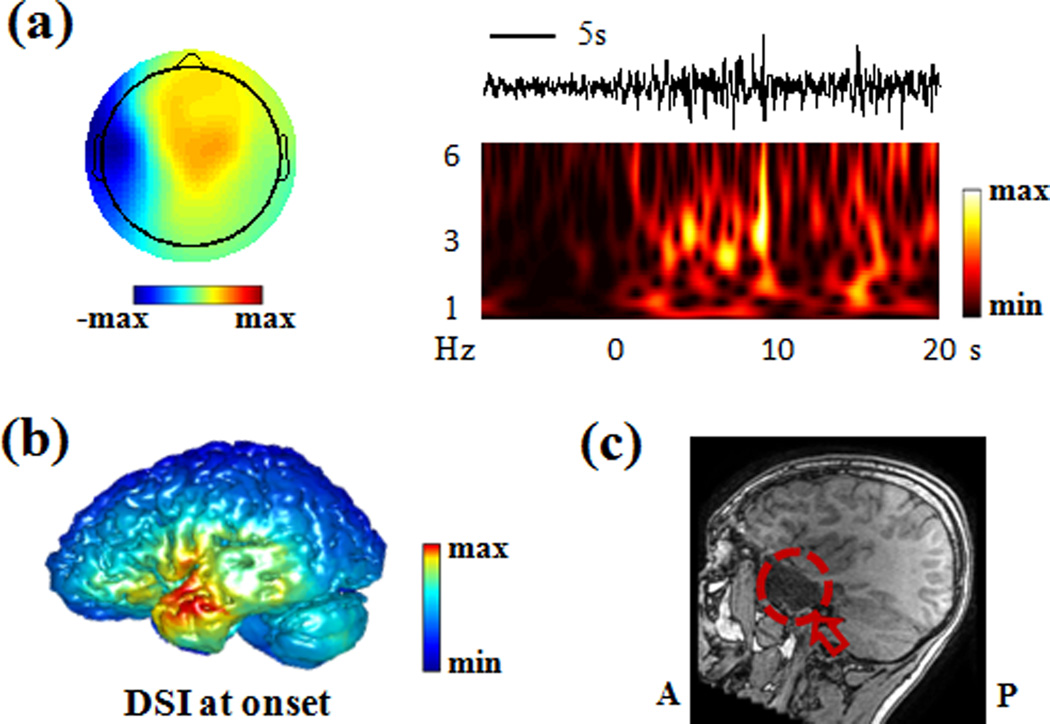
Patient 8 was an epilepsy patient with temporal lobe epilepsy. The scalp EEG of the patient showed delta frequency activity over the left temporal region. Multiple seizure components were extracted and the seizure component showing the earliest ictal activation is shown in Fig. 4a. The spatial map indicates left temporal seizure activity. The time course and time-frequency representation show seizure activity in the delta frequency band following the seizure onset. The estimated seizure sources in Fig. 4b show that the seizure source is active in the left temporal lobe of this patient. The post-operative MRI image of this patient (Fig. 4c) shows that part of the left temporal lobe was resected during the surgery. The estimated seizure source in the left temporal lobe is concordant with the surgical resection zone that is shown in the post-operative MRI image. Since the intracranial recording was not available in this patient, a comparison between the source imaging results and the SOZ was not performed.
Fig. 4.
Seizure source imaging results in Patient 8. (a) Example of scalp topography, activity, and time-frequency representation of a seizure component. (b) Estimated source at seizure onset. (c) Post-operative MRI image of the patient. The surgical resection is marked by red circle.
The seizure imaging results in all nine epilepsy patients are summarized in Table 2. The source imaging result is considered to be concordant to the surgical resection if the estimated source maximum is located within the resection zones. In seven of the nine patients, the estimated source maxima were located inside the surgical resection zones. The estimated source maxima of the other two patients were within 2 cm distance to the resection boundary. Intracranial recordings are available in seven of the nine patients. In five patients, the estimated source was either smaller than one or only one inter-electrode-distance away from the SOZ. Note that a distance smaller than 1 inter-electrode distance does not necessarily indicate a localization error, because activity between two electrodes cannot be directly measured by the iEEG. The average distance to the SOZ of the seven patients is 1.4 inter-electrode-distances. These results demonstrate that the seizure imaging results are co-localized with the surgical resection and intracranial recordings of the studied patients.
Table 2.
Source imaging results in all pediatric patients.
| Patient | Surgery | Location of source maximum | Concordance to resection |
|---|---|---|---|
| 1 | Right frontal lobe | Right posterior frontal | + |
| 2 | Left occipital lobe | Left occipital | + |
| 3 | Left frontal lobe | Left posterior frontal | ++ |
| 4 | Left frontal lobe | Left superior frontal | + |
| 5 | Right frontal lobe | Right superior frontal | + |
| 6 | Right frontal/right tempo | Rrailg lhotb seu perior frontal | + |
| 7 | Right frontal lobe | Right anterior frontal | + |
| 8 | Left temporal lobe | Left temporal | + |
| 9 | Left parietal lobe | Left parietal | ++ |
+: Source maximum is located inside surgical resection; ++: Source maximum is close to surgical resection;
4. Discussion
Long-term EEG monitoring can non-invasively capture seizure activity with wide spatial coverage. The advancement of source imaging approaches has made it possible to study the underlying brain source activity in addition to the traditional EEG trace interpretation. Several source analysis methods have been applied to study ictal activity of epilepsy patients (Assaf and Ebersole, 1997; Lantz et al., 2001; Worrell et al., 2000; Merlet and Gotman, 2001; Koessler et al., 2010; Holmes et al., 2010). However, the localization of seizure activity remains challenging because ictal EEG signals are usually contaminated by artifacts and measurement noise. The ictal discharge can change in time, space and frequency, which increases the difficulty for the source imaging. To separate the spatial, temporal and spectral patterns from seizure activity, blind source separation techniques (Nam et al., 2002; Patel et al., 2008; Jung et al., 2009) have been used to decompose seizure activity into independent components. Along this line, a dynamic seizure imaging approach (Yang et al., 2011) has recently been developed to image the continuous change of ictal activity. Instead of solving the inverse problem on discrete EEG time instants, the dynamic seizure imaging approach extracts seizure components with temporal-spectral features and recombines the components in the source domain to form spatiotemporal imaging. In this study, the dynamic seizure imaging approach was applied in nine pediatric patients and the DSI was able to extract the activity of the seizure sources. The estimated seizure sources were consistent with the surgical resections and the intracranial recordings of the patients.
EEG source imaging techniques can noninvasively study brain activity by modeling the brain sources and volume conductor (He et al., 1987; Michel et al., 2004; Plummer et al., 2008; He et al., 2011). In the present study, patient-specific BEM head models were obtained from individual MRIs, and used for EEG source analysis to improve the spatial resolution. Studies have shown that more precise source localization results can be obtained in realistic-geometric head models compared to simple spherical head models (Herrendorf et al., 2000; Wang et al., 2010). The performance of EEG source imaging could further be improved by incorporating a prior information such as anisotropic conductivities (Michel et al., 2004) and fMRI constrains (He & Liu, 2008; Liu and He, 2008; Yang et al., 2010).
While adult epilepsy patients are more likely to experience temporal lobe epilepsy, pediatric epilepsy patients suffer more from extratemporal lobe epilepsy (Gilliam et al., 1997; Sperli et al., 2006). The overlapping of the epileptogenic zone and the functional brain region makes it difficult to achieve favorable surgical outcome in extratemporal cases without jeopardizing the eloquent function of patients. As a result, it is important yet challenging in pediatric patients to correctly differentiate the epileptogenic zone from normal brain tissues. Among the eight studied extratemporal lobe epilepsy patients, the estimated seizure onset results of six patients were located within the resected region. In the remaining two patients with parietal and frontal seizures, the estimated source maxima were not located within the resected region but very close to the boundary of the resection. This could be due to the localization error of EEG source imaging and it could also be explained by the limited resection size in these two patients. One of the two patients had intracranial EEG, but only part of the iEEG-SOZ was removed because the patient experienced speech impairment during the surgery, which prevented the complete resection. The other patient had no intracranial data available. However the surgical follow-up outcome showed that this patient was not seizure free, which indicated that the epileptogenic zone was not completely resected during the surgery. Although it is important to remove the entire epileptogenic zone to obtain a seizure free outcome, resective surgery has to be conservative in extratemporal lobe epilepsy patients to preserve functional brain areas. Future studies of DSI in distinguishing functional brain regions could further help in separating eloquent cortex from pathological tissues and thus provide more information for surgical planning.
One of the challenging problems in the pre-surgical planning of epilepsy patients is the integration of the useful information from multiple modalities to better identify the epileptogenic zones, such as in the patients with normal MRI or SPECT results. With the advancement of MRI imaging techniques, MRI can reveal more mild changes in brain structures. However, it is not rare to have epilepsy patients with normal images in various MRI scan sequences (Rosenow and Lüders, 2001; Brodbeck et al., 2010). Furthermore, the MRI visible lesions or SPECT foci may not be epileptic and the true epileptic brain tissue may exist in regions that are distinct from the MRI visible lesions or SPECT foci. Noninvasive approaches that localize the epileptic regions are thus helpful in these patients with normal MRI or SPECT results. It is also beneficial to confirm the epileptic foci in the patients with multiple MRI lesions or SPECT abnormalities. Among the nine patients included in this study, five of them have MRI visible lesions and the remaining four patients have normal MRI images. The seizure source imaging results in three of the MRI-negative patients were within the resection zones and the results in the remaining patient were close to the resection boundary. Among the six patients with SPECT scans, five of these patients showed perfusion abnormities and one patient did not have clear focus of tracer uptake. The seizure source imaging approach localized the SOZ in the patient without clear SPECT tracer uptake, and it also identified the epileptic foci in the five patients with SPECT perfusion abnormities. While further investigations are needed with regard to the additional value of noninvasive EEG source imaging compared with other modalities, the present results suggest that the dynamic seizure imaging approach could potentially be helpful in localizing epileptic regions of patients with normal MRI or SPECT.
The scalp EEG has been widely used to capture the electrophysiological brain activity with high temporal resolution at millisecond scale. It has also been utilized in clinical settings to study the abnormal brain activity of epilepsy patients. The scalp EEG of our studied patients showed ictal activity over the corresponding scalp regions of seizure onset zone. Although the scalp EEG in these patients could suggest the general brain regions with seizure activity, the scalp EEG has limited spatial resolution due to the smearing effect of the volume conductor. The employment of EEG source imaging allows us to incorporate the anatomical information of patient MRI to model the electrical brain sources and their volume conduction to help localize the brain sources with high resolution. The dynamic seizure imaging approach also enables us to extract the spatio-temporal ictal features to accurately image the underlying seizure sources. This study demonstrates the usefulness of EEG source imaging in the localization and imaging of brain sources in a group of nine patients. Future studies in a larger patient population and in patients with indistinct ictal onset may be necessary to further assess the additional clinical value of including seizure source imaging in pre-surgical planning.
In conclusion, we applied a spatiotemporal seizure imaging approach to localize the seizure activity of nine drug-resistant pediatric epilepsy patients. This approach studied the time-frequency seizure features and imaged the onset as well as the continuous activations of seizures. The dynamic study of seizures is important to epilepsy patients in order to better understand the seizure characteristics and mechanism. The estimated seizure sources in the present study were compared with the surgical resections and intracranial recordings of the patients. Concordant results were obtained by comparing the source locations with the resection regions as well as the SOZ determined from ECoG. This study demonstrates that the dynamic seizure imaging technique can help noninvasive imaging and localization of seizure sources in pediatric patients. It also has the potential to help guide the implantation of intracranial electrodes and to provide additional information for the pre-surgical planning of epilepsy surgery patients.
Highlights.
-
-
Dynamic seizure imaging approach was applied to image the ictal activity in pediatric epilepsy patients, especially in more challenging extratemporal lobe pediatric patients.
-
-
The imaging results were evaluated with surgical resection and intracranial recordings, which indicated the merits of utilizing spatio-temporal ictal features to delineate the onset as well as the continuous activations of seizure activity.
-
-
The dynamic seizure imaging approach can noninvasively localize seizure sources and is potentially useful in aiding the pre-surgical planning of epilepsy.
Acknowledgements
This work was supported by NIH RO1 EB007920, RO1 EB006433, NSF CBET-0933067, and a grant from the Minnesota Partnership for Biotechnology and Medical Genomics.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Assaf BA, Ebersole JS. Continuous source imaging of scalp ictal rhythms in temporal lobe epilepsy. Epilepsia. 1997;38:1114–1123. doi: 10.1111/j.1528-1157.1997.tb01201.x. [DOI] [PubMed] [Google Scholar]
- Brodbeck V, Spinelli L, Lascano AM, Pollo C, Schaller K, Vargas MI, et al. Electrical source imaging for presurgical focus localization in epilepsy patients with normal MRI. Epilepsia. 2010;51:583–591. doi: 10.1111/j.1528-1167.2010.02521.x. [DOI] [PubMed] [Google Scholar]
- Dale AM, Sereno MI. Improved localizadon of cortical activity by combining eeg and meg with mri cortical surface reconstruction: A linear approach. J. Cogn. Neurosci. 1993;5:162–176. doi: 10.1162/jocn.1993.5.2.162. [DOI] [PubMed] [Google Scholar]
- Delorme A, Makeig S. EEGLAB: an open source toolbox for analysis of single-trial EEG dynamics including independent component analysis. J.Neurosci.Methods. 2004;134:9–21. doi: 10.1016/j.jneumeth.2003.10.009. [DOI] [PubMed] [Google Scholar]
- Ding L, Worrell GA, Lagerlund TD, He B. Ictal source analysis: localization and imaging of causal interactions in humans. Neuroimage. 2007;34:575–586. doi: 10.1016/j.neuroimage.2006.09.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebersole JS. Noninvasive localization of epileptogenic foci by EEG source modeling. Epilepsia. 2000;41:S24–S33. doi: 10.1111/j.1528-1157.2000.tb01531.x. [DOI] [PubMed] [Google Scholar]
- Engel J., Jr . Approaches to localization of the epileptogenic lesion. In: Engel J Jr, editor. Surgical treatment of the epilepsies. New York: Raven Press; 1987. pp. 75–95. [Google Scholar]
- Gavaret M, Badier JM, Marquis P, Bartolomei F, Chauvel P. Electric source imaging in temporal lobe epilepsy. J. Clin. Neurophysiol. 2004;21:267–282. doi: 10.1097/01.wnp.0000139929.06455.82. [DOI] [PubMed] [Google Scholar]
- Gilliam F, Wyllie E, Kashden J, Faught E, Kotagal P, Bebin M, et al. Epilepsy surgery outcome: comprehensive assessment in children. Neurology. 1997;48:1368. doi: 10.1212/wnl.48.5.1368. [DOI] [PubMed] [Google Scholar]
- Hämäläinen MS, Ilmoniemi RJ. Helsinki Univ.Technol. Helsinki, Finland: Tech.Rep.TKK-F- A; 1984. Interpreting measured magnetic fields of the brain: estimates of current distributions. [Google Scholar]
- Hämäläinen MS, Sarvas J. Realistic conductivity geometry model of the human head for interpretation of neuromagnetic data. IEEE Trans. Biomed. Eng. 1989;36:165–171. doi: 10.1109/10.16463. [DOI] [PubMed] [Google Scholar]
- He B, Musha T, Okamoto Y, Homma S, Nakajima Y, Sato T. Electric dipole tracing in the brain by means of the boundary element method and its accuracy. IEEE Trans. Biomed. Eng. 1987;34:406–414. doi: 10.1109/tbme.1987.326056. [DOI] [PubMed] [Google Scholar]
- He B, Liu Z. Multimodal functional neuroimaging: Integrating functional MRI and EEG/MEG. IEEE Rev. Biomed. Eng. 2008;1:23–40. doi: 10.1109/RBME.2008.2008233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He B, Yang L, Wilke C, Yuan H. Electrophysiological Imaging of Brain Activity and Connectivity – Challenges and Opportunities. IEEE Trans. Biomed. Eng. 2011;58:1918–1931. doi: 10.1109/TBME.2011.2139210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrendorf G, Steinhoff B, Kolle R, Baudewig J, Waberski T, Buchner H, et al. Dipole-Source Analysis in a Realistic Head Model in Patients with Focal Epilepsy. Epilepsia. 2000;41:71–80. doi: 10.1111/j.1528-1157.2000.tb01508.x. [DOI] [PubMed] [Google Scholar]
- Holmes MD, Tucker DM, Quiring JM, Hakimian S, Miller JW, Ojemann JG. Comparing Noninvasive Dense Array and Intracranial Electroencephalography for Localization of Seizures. Neurosurgery. 2010;66:354–362. doi: 10.1227/01.NEU.0000363721.06177.07. [DOI] [PubMed] [Google Scholar]
- Jung KY, Kang JK, Kim JH, Im CH, Kim KH, Jung HK. Spatiotemporospectral characteristics of scalp ictal EEG in mesial temporal lobe epilepsy with hippocampal sclerosis. Brain Res. 2009;1287:206–219. doi: 10.1016/j.brainres.2009.06.071. [DOI] [PubMed] [Google Scholar]
- Jung TP, Makeig S, Humphries C, Lee TW, Mckeown MJ, Iragui V, et al. Removing electroencephalographic artifacts by blind source separation. Psychophysiology. 2000;37:163–178. [PubMed] [Google Scholar]
- Koessler L, Benar C, Maillard L, Badier JM, Vignal JP, Bartolomei F, et al. Source localization of ictal epileptic activity investigated by high resolution EEG and validated by SEEG. Neuroimage. 2010;51:642–653. doi: 10.1016/j.neuroimage.2010.02.067. [DOI] [PubMed] [Google Scholar]
- Lai Y, Van Drongelen W, Ding L, Hecox K, Towle V, Frim D, et al. Estimation of in vivo human brain-to-skull conductivity ratio from simultaneous extra-and intra-cranial electrical potential recordings. Clin. Neurophysiol. 2005;116:456–465. doi: 10.1016/j.clinph.2004.08.017. [DOI] [PubMed] [Google Scholar]
- Lai Y, van Drongelen W, Hecox K, Frim D, Kohrman M, He B. Cortical activation mapping of epileptiform activity derived from interictal ECoG spikes. Epilepsia. 2007;48:305–314. doi: 10.1111/j.1528-1167.2006.00936.x. [DOI] [PubMed] [Google Scholar]
- Lai Y, Zhang X, van Drongelen W, Korhman M, Hecox K, Ni Y, et al. Noninvasive cortical imaging of epileptiform activities from interictal spikes in pediatric patients. Neuroimage. 2011;54:244–252. doi: 10.1016/j.neuroimage.2010.07.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lantz G, Grave de Peralta R, Spinelli L, Seeck M, Michel CM. Epileptic source localization with high density EEG: how many electrodes are needed? Clin. Neurophysiol. 2003;114:63–69. doi: 10.1016/s1388-2457(02)00337-1. [DOI] [PubMed] [Google Scholar]
- Lantz G, Michel CM, Seeck M, Blanke O, Spinelli L, Thut G, et al. Space-oriented segmentation and 3-dimensional source reconstruction of ictal EEG patterns. Clin. Neurophysiol. 2001;112:688–697. doi: 10.1016/s1388-2457(01)00479-5. [DOI] [PubMed] [Google Scholar]
- Liu Z, He B. fMRI-EEG integrated cortical source imaging by use of time-variant spatial constraints. Neuroimage. 2008;39:1198–1214. doi: 10.1016/j.neuroimage.2007.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merlet I, Gotman J. Dipole modeling of scalp electroencephalogram epileptic discharges: correlation with intracerebral fields. Clin. Neurophysiol. 2001;112:414–430. doi: 10.1016/s1388-2457(01)00458-8. [DOI] [PubMed] [Google Scholar]
- Michel CM, Murray MM, Lantz G, Gonzalez S, Spinelli L, Grave de Peralta R. EEG source imaging. Clin. Neurophysiol. 2004;115:2195–2222. doi: 10.1016/j.clinph.2004.06.001. [DOI] [PubMed] [Google Scholar]
- Nam H, Yim TG, Han SK, Oh JB, Lee SK. Independent component analysis of ictal EEG in medial temporal lobe epilepsy. Epilepsia. 2002;43:160–164. doi: 10.1046/j.1528-1157.2002.23501.x. [DOI] [PubMed] [Google Scholar]
- Oostendorp TF, Delbeke J, Stegeman DF. The conductivity of the human skull: Results of in vivo and in vitro measurements. IEEE Trans Biomed Eng. 2000;47:1487–1492. doi: 10.1109/TBME.2000.880100. [DOI] [PubMed] [Google Scholar]
- Patel A, Alotaibi F, Blume WT, Mirsattari SM. Independent component analysis of subdurally recorded occipital seizures. Clin. Neurophysiol. 2008;119:2437–2446. doi: 10.1016/j.clinph.2008.07.276. [DOI] [PubMed] [Google Scholar]
- Plummer C, Harvey AS, Cook M. EEG source localization in focal epilepsy: Where are we now? Epilepsia. 2008;49:201–218. doi: 10.1111/j.1528-1167.2007.01381.x. [DOI] [PubMed] [Google Scholar]
- Rosenow F, Lüders H. Presurgical evaluation of epilepsy. Brain. 2001;124:1683. doi: 10.1093/brain/124.9.1683. [DOI] [PubMed] [Google Scholar]
- Shinnar S, Pellock JM. Update on the epidemiology and prognosis of pediatric epilepsy. J.Child Neurol. 2002;17:S4. doi: 10.1177/08830738020170010201. [DOI] [PubMed] [Google Scholar]
- Sperli F, Spinelli L, Seeck M, Kurian M, Michel CM, Lantz G. EEG source imaging in pediatric epilepsy surgery: a new perspective in presurgical workup. Epilepsia. 2006;47:981–990. doi: 10.1111/j.1528-1167.2006.00550.x. [DOI] [PubMed] [Google Scholar]
- Wang G, Worrell G, Yang L, Wilke C, He B. Interictal spike analysis of high-density EEG in patients with partial epilepsy. Clin. Neurophysiol. 2010;122:1098–1105. doi: 10.1016/j.clinph.2010.10.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilke C, Van Drongelen W, Kohrman M, He B. Identification of epileptogenic foci from causal analysis of ECoG interictal spike activity. Clin. Neurophysiol. 2009;120:1449–1456. doi: 10.1016/j.clinph.2009.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilke C, Van Drongelen W, Kohrman M, He B. Neocortical seizure foci localization by means of a directed transfer function method. Epilepsia. 2010;51:564–572. doi: 10.1111/j.1528-1167.2009.02329.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilke C, Worrell G, He B. Graph analysis of epileptogenic networks in human partial epilepsy. Epilepsia. 2011;52:84–93. doi: 10.1111/j.1528-1167.2010.02785.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Worrell GA, Lagerlund TD, Sharbrough FW, Brinkmann BH, Busacker NE, Cicora KM, et al. Localization of the epileptic focus by low-resolution electromagnetic tomography in patients with a lesion demonstrated by MRI. Brain Topogr. 2000;12:273–282. doi: 10.1023/a:1023407521772. [DOI] [PubMed] [Google Scholar]
- Yang L, Liu Z, He B. EEG-fMRI reciprocal functional neuroimaging. Clin. Neurophysiol. 2010;121:1240–1250. doi: 10.1016/j.clinph.2010.02.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang L, Wilke C, Brinkmann B, Worrell GA, He B. Dynamic imaging of ictal oscillations using non-invasive high-resolution EEG. Neuroimage. 2011;56:1908–1917. doi: 10.1016/j.neuroimage.2011.03.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X, van Drongelen W, Hecox KE, Towle VL, Frim DM, McGee AB, et al. High-resolution EEG: Cortical potential imaging of interictal spikes. Clin. Neurophysiol. 2003;114:1963–1973. doi: 10.1016/s1388-2457(03)00194-9. [DOI] [PubMed] [Google Scholar]
- Zhang Y, van Drongelen W, He B. Estimation of in vivo brain-to-skull conductivity ratio in humans. Appl.Phys.Lett. 2006;89:223903. doi: 10.1063/1.2398883. [DOI] [PMC free article] [PubMed] [Google Scholar]