Abstract
The continuous release of bone-stored growth factors following bone resorption promotes the colonization of circulating cancer cells. However, the precise role of each of the various growth factors remains unclear. In this study, we investigated the role of bone-derived insulin-like growth factor (IGF) in the development of bone metastases in an animal model of breast cancer. We found that local stimulation of calvarial bone resorption prior to cell inoculation stimulated subsequent bone metastases to that site in vivo, while inhibition of bone resorption inhibited bone metastases. Anchorage-independent growth of cancer cells was stimulated by the culture supernatants from resorbed bones, which contained elevated levels of IGF type I (IGF-1). This stimulation was blocked by IGF-1 receptor (IGF1R) neutralizing antibody, but not antibody targeting other bone-stored growth factors including TGFβ, fibroblast growth factors, and platelet derived growth factors. While recombinant human IGF-I caused IGFIR tyrosine autophosphorylation, followed by activation of Akt and NF-κB in cancer cells, dominant-negative inhibition of IGFIR, Akt, or NF-κB significantly reduced bone metastases with increased apoptosis and decreased mitosis in metastatic cells. Together, our findings suggest that bone-derived IGF-I bridges the crosstalk between bone and metastasized cancer cells via activation of the IGFIR/Akt/NF-κB pathway. Disruption of this pathway therefore may represent a promising therapeutic intervention for bone metastasis.
Keywords: IGF receptor signaling, Akt, NF-κB, apoptosis, mitosis
INTRODUCTION
Bone is one of the most common target sites of distant metastasis of breast, prostate and lung cancer (1–3). Bone metastasis represents one of the major causes of morbidity such as intractable bone pain, pathological fractures, spinal cord compression, and hypercalcemia in cancer patients. Accumulated clinical and experimental data that specific inhibitors of osteoclasts including bisphosphonates (BPs) effectively suppress osteolytic bone metastases (4, 5) suggest that osteoclastic bone destruction plays a critical role in the development and progression of bone metastases.
Bone is a storehouse of a variety of growth factors such as insulin-like growth factors (IGFs), TGFβ, fibroblast growth factors (FGFs), platelet-derived growth factors (PDGFs), and bone morphogenetic proteins (BMPs) (6, 7). Our group showed that TGFβ is released in active forms following bone resorption in organ cultures of neonatal mouse calvarial bones (8), verifying that bone-stored growth factors are released by osteoclastic bone resorption.
Several lines of evidence suggest that colonization of cancer cells in bone is under the influence of bone-derived growth factors. For example, bone-derived TGFβ has been shown to activate TGFβ-Smad signaling pathway in metastatic breast cancer cells in bone leading to increased parathyroid hormone-related protein (PTHrP) production in these breast cancer cells (9, 10), which in turn enhances osteoclastogenesis and bone destruction through an up-regulation of receptor activator of NF-κB ligand (RANKL) expression in neighboring osteoblasts (11). RANKL in osteoblasts then functionally interacts with RANK expressed in pre-osteoclasts and mature osteoclasts, causing increased osteoclast formation and bone resorption. Consequently, growth factors are further released from resorbing bone and promote colonization of metastatic cancer cells in bone. Accordingly, it has been proposed that an establishment of so-called “vicious cycle” between metastatic cancer cells and bone is a requisite for the development of bone metastases (1–3). However, the contributions of bone-stored growth factors other than TGFβ to bone metastasis are still poorly understood. Moreover, dissection of cancer cell responses to these bone-derived growth factors in the development of bone metastases is important to understand the mechanism of bone metastases and to design novel therapeutic approaches for bone metastases.
IGFs, which are the most abundant growth factors stored in bone (6, 7), have been implicated in the development, progression and aggressiveness of many types of cancers including breast cancer (12, 13). Therefore, the role of IGFs in bone metastasis is of particular interest and worthwhile studying. IGFs initiate its actions primarily through binding to IGF type I receptors (IGFIR) (12, 13). Clinical studies described that the majority of cancers express IGFIR (14) and that the expression levels are significantly higher in tumors than neighboring normal tissues (15). Experimental studies demonstrated that the activation of IGFIR signaling pathways promotes cancer growth and metastasis (16). Conversely, inhibition of IGFIR signaling suppressed tumor aggressiveness (17). These results suggest that IGFIR expression and activation of its signaling pathway are critical to the promotion of malignant behaviors of cancers. Accordingly, IGFIR and its downstream pathway have been thought to be promising targets for cancer therapy and varieties of antagonists, inhibitors or neutralizing antibodies are currently under clinical evaluation (12, 13).
In the present study, we attempted to determine the role of bone-derived IGFs and IGFIR signaling pathway in responding breast cancer cells in the development of bone metastases in a pre-clinical setting using a well-characterized animal model (4). We found that the bone-derived IGFs stimulated bone metastases of MDA-MB-231 human breast cancer cells through stimulation of cell proliferation and inhibition of apoptosis. These effects of IGFs were elicited via the activation of the serine/threonine kinase Akt and the transcription factor NF-κB. Akt and NF-κB are known to be activated by IGFs and promote cell survival (12, 13, 18–21). Disruption of the activation of IGFIR, Akt or NF-κB significantly inhibited bone metastases. Our results suggest that an activation of IGFIR signaling by bone-derived IGFs promotes bone metastases of breast cancer. IGFIR signaling pathway could thus be a well-rationalized target in the development of pharmacological therapeutic agents for bone metastasis.
MATERIALS AND METHODS
Cytokines and Antibodies
Recombinant human TGFβ1, IGF-I, IGF-II, FGF-1, FGF-2, BMP-2, PDGF-BB and interleukin-1β (IL-1β), and neutralizing polyclonal antibodies to TGFβ, FGF-1, FGF-2 and PDGF-BB were purchased from R & D Systems (Minneapolis, MN). A neutralizing mouse monoclonal antibody to IGFIR (αIR3) was from Oncogene Research Products (Cambridge, MA). Rabbit polyclonal antibodies to IGFIRα and NF-κB (p50 and p65) were from Santa Cruz Biotechnology (Santa Cruz, CA). Rabbit polyclonal antibodies to Akt and phospho-Akt (pAkt) were from Cell Signaling Technology (Beverly, MA). Anti-phosphotyrosine (pY) polyclonal antibody was described previously (22). The BP zoledronic acid (ZOL) was from Novartis Pharma (Tokyo, Japan). All other chemicals used in this study were purchased from Sigma-Aldrich (St. Louis, MO) or Wako Pure Chemical Industries (Osaka, Japan) unless otherwise described.
Cell Culture
Human breast cancer cell line MDA-MB-231 was obtained from the American Type Culture Collection (Rockville, MD). The cells were expanded and stored according to the supplier’s instructions, and used within 2 months after resuscitation of frozen aliquots. MDA-231AD cells, a MDA-MB-231 clone that is reproducibly and highly metastatic to bone and adrenal glands, was described previously (23). These cells were cultured in Dulbecco’s Modified Eagle’s Medium (DMEM) supplemented with 10% FBS (Hyclone, Logan, UT) and 1% penicillin-streptomycin solution (Life Technologies, Grand Island, NY) in a humidified atmosphere of 5% CO2 in air.
Stimulation of Calvarial Bone Resorption in Organ Culture
The details of this culture technique have been described previously (24). In brief, calvariae were excised from 6-day-old pups of BALB/c mice (Harlan, Indianapolis, IN), dissected free of adjacent connective tissues, placed in serum-free Biggers-Gwatokin-Jackson medium (BGJb, Sigma-Aldrich) containing 0.1% BSA and cultured with or without 100 pM IL-1β for 48 hours in the absence or presence of 1 μM ZOL. The conditioned medium (CM) harvested from IL-1β-treated or -untreated calvarial bones was designated resorbed or unresorbed bone CM, respectively and frozen at −20°C until use.
Colony Formation Assay
Anchorage-independent growth of MDA-MB-231 cells was determined by colony formation in soft agar as described (25). MDA-MB-231 cells (500 cells/well/24-well plate) were cultured in DMEM supplemented with 2% FBS and control bone or resorbed bone CM (20%, v/v) in the absence or presence of 5 μg/ml neutralizing antibodies to TGFβ, IGFIR, FGF-1, FGF-2, or PDGF-BB in soft agar for 14 days. CM and antibodies were added to the cultures every three and seven days, respectively. At the end of culture, colonies >200 μm in diameter were manually counted under inverted microscope.
Measurements of PTHrP and IGF-I
PTHrP production by MDA-MB-231 clones was measured as described (9). PTHrP concentrations were determined using a two-site immunoradiometric assay (IRMA) (Nichols Institute, San Juan Capistrano, CA or Mitsubishi Chemical, Tokyo, Japan) according to manufacturer’s instruction. IGF-I concentrations were measured using a commercial RIA kit (American Laboratory Products Company, Windham, NH).
Transfection
Cell transfection was performed as described in Supplementary Materials and Methods. Wild-type IGFIR gene was stably transfected into parental MDA-MB-231 cells and dominant-negative mutants of IGFIR (IGFIR/486STOP), Akt (DN-Akt), and inhibitor of κBα (IκBαΔN) were into MDA-231AD cells.
Tumor Inoculation
Tumor cell inoculation was performed as described in Supplementary Materials and Methods. All animal protocols were approved by the Institutional Animal Care and Use Committee at Osaka University Graduate School of Dentistry and the University of Texas Health Science Center at San Antonio.
Radiographic Analysis
Development of bone metastases was monitored by X-rays as described previously (4).
Histological and Histomorphometric Analysis
Paraffin sections of the hindlimbs were made following conventional methods. Histomorphometric analyses of metastatic tumor burden in bone, apoptosis and mitosis of MDA-MB-231 cells, and osteoclast number in bone metastases were performed as described previously (4).
IGFIR Immunohistochemistry
Fifteen clinical samples of bone metastases were obtained at the time of surgery at Osaka University Hospital (Osaka, Japan). The study was approved by the Institutional Review Board of the Osaka University Graduate School of Medicine. Immunohistochemical staining of paraffin sections was performed using Histofine Simple Stain Kit (Nichirei Biosciences, Tokyo, Japan) according to the manufacturer’s protocol. Chromogen was developed using DAB Liquid System (Dako Japan, Kyoto, Japan). The slides were counterstained with hematoxylin. The immunoreactivity was evaluated as negative (−) or positive (+).
Immunoprecipitation and Western Blotting
Immunoprecipitation (IP) and western blotting (WB) were performed as described previously (26).
Electrophoretic Mobility Shift Assay (EMSA)
EMSA was performed as described in Supplementary Materials and Methods.
Statistical Analysis
Data are expressed as the mean ± SEM. The data were analyzed by one-way ANOVA followed by Fisher’s PLSD post-hoc test (StatView; SAS Institute, Cary, NC) for determination of differences between groups. Student’s t-test or Welch’s t-test was conducted when two groups were compared. P values of < 0.05 were considered significant.
RESULTS
Effects of Bone Resorption on the Development of Bone Metastases
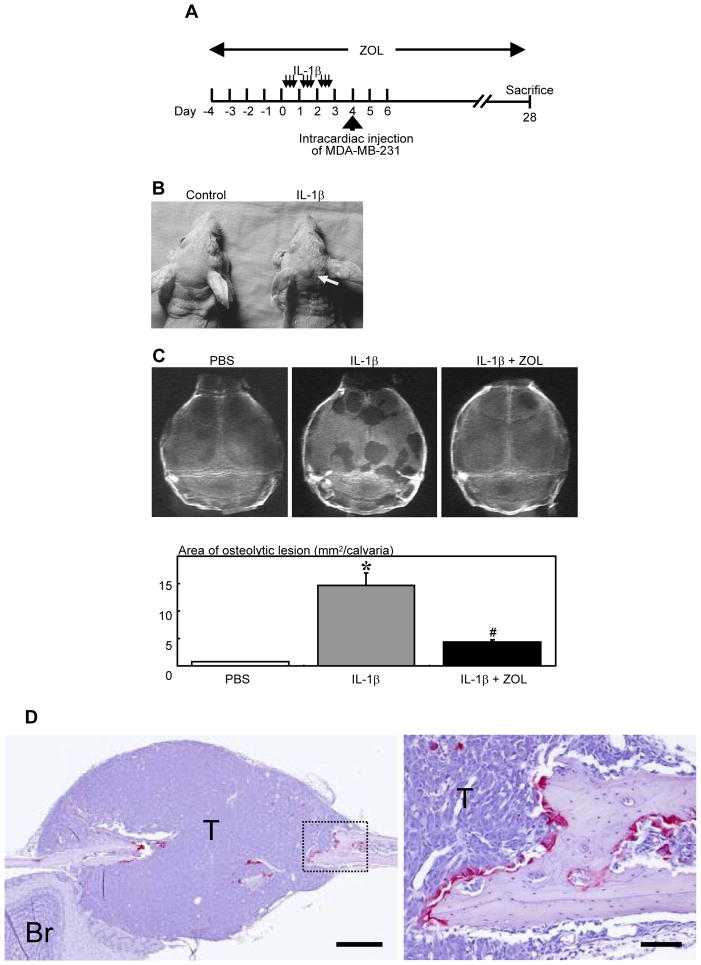
We previously described that MDA-MB-231 cells rarely metastasized to calvarial bones following intracardiac inoculation for unknown reasons (7). Taking advantage of this feature, we examined whether stimulation of calvarial bone resorption in advance modulates the subsequent development of bone metastases to this rare site. Bone resorption was stimulated by the repeated subcutaneous injections of IL-1β over the calvariae (Figure 1A). This treatment induced no evident stimulation of bone resorption in other bones than calvariae at radiologic and histological levels and did not cause hypercalcemia (27). Thus, the effects of IL-1β were restricted to the calvarial bones. Twenty-four hours after the last injection of IL-1β, MDA-MB-231 cells were inoculated into the left cardiac ventricle in female nude mice (Figure 1A). At day 28, mice treated with IL-1β prior to cell inoculation showed macroscopic tumor formation on the calvariae (Figure 1B). Radiographic examination revealed multiple osteolytic lesions on the calvarial bones (Figure 1C). Quantitative assessment of these osteolytic lesions demonstrated that stimulation of calvarial bone resorption by IL-1β prior to cell inoculation significantly increased osteolytic area (Figure 1C). Histological examination showed that these osteolytic lesions were colonized by metastatic cancer cells with destruction of calvarial bones by numerous osteoclasts (Figure 1D), verifying that these osteolytic lesions represent bone metastases. Mice received repeated IL-1β injections on their calvarial bone but no subsequent intracardiac inoculation of cancer cells exhibited no development of osteolytic lesions at day 28 (data not shown). However, we observed discernible increase in calvarial bone formation probably as a consequence of IL-1β-stimulated bone resorption as described in the previous report (27). IL-1β administered together with the BP ZOL, a potent and specific inhibitor of osteoclastic bone resorption (5), showed significant reduction of osteolytic bone metastases on calvarial bones (Figure 1C). ZOL alone with no IL-1β injections, followed by intracardiac inoculation of MDA-MB-231 cells showed no effects on calvarial bones, since no osteolytic bone metastases were developed on the calvarial bones in the absence of IL-1β injections. However, under these circumstances, osteolytic bone metastases developed in the proximal tibiae that are one of the representative sites of bone metastasis in this animal model and zoledronic acid significantly reduced these osteolytic bone metastases (data not shown). These results suggest that the stimulation of bone resorption stimulates bone metastases, while inhibition of bone resorption inhibits them.
FIGURE 1. Effects of bone resorption on the development of bone metastases of MDA-MB-231 human breast cancer cells in nude mice.
(A) Experimental protocol. Four-week-old female athymic nude mice received repeated subcutaneous injections of IL-1β (thin arrows, 2 μg/10 μl/injection) over the calvariae 3 times a day for 3 days. Twenty-four hours after the last injection, MDA-MB-231 cells were inoculated into the left cardiac ventricle (thick arrow). In one group of animals ZOL (4 μg/mouse, s. c., daily) was given from 4 days before the IL-1β injection to the end of the experiments. Mice were sacrificed at day 28.
(B) Macroscopic view of tumor formation at the time of sacrifice. Note tumor formation on the head of IL-1β-treated mouse (arrow).
(C) Representative radiographic view of calvariae and quantitative analysis of osteolytic lesions in PBS-, IL-1β-, and IL-1β + ZOL-treated mice. Data are mean from two separate experiments (n = 6 mice x 2 experiments = 12 for each group).
* Significantly greater than PBS group (p < 0.01).
# Significantly less than IL-1β group (p < 0.01).
(D) Left: Representative histological view of metastasis in calvariae. Right: Higher magnification of the dashed rectangle area. Tumor colonization (T) is associated with calvarial bone destruction with numerous TRAP-positive osteoclasts along the surface of adjacent bone. (TRAP staining, Br: brain, scale bars = 500 μm (left), 100 μm (right)).
Effects of Resorbed Bone CM on MDA-MB-231 Cells
We next attempted to identify a bone-derived factor that is released following stimulation of bone resorption and is responsible for stimulation of bone metastases. To study this, neonatal mouse calvarial bones were placed in organ cultures in the presence or absence of IL-1β with or without ZOL, and the CM was harvested and tested for their capacity to stimulate MDA-MB-231 cell behaviors. Earlier studies from our group reported that bone resorption of neonatal mouse calvariae was stimulated under this experimental condition (24) and that bone-stored growth factors are released in the culture medium in active forms (8).
To examine the effects of the CM on cell growth, we performed the colony formation assay in soft agar. This assay has been widely used for determining in vitro tumorigenicity of cancer cells (28) and shown to correlate well with in vivo tumorigenicity. The resorbed bone CM (20%, v/v) markedly stimulated the anchorage-independent growth of MDA-MB-231 cells in soft agar compared with the control bone CM (Figure 2A). The effects of the resorbed bone CM were dose-dependent between concentrations of 10 to 50% (v/v) (data not shown). The CM harvested from the cultures treated with both IL-1β and ZOL showed profoundly reduced activity compared with those treated with IL-1β alone (Figure 2A). Of note, the neutralizing antibody to IGFIR but not TGFβ, FGF-1, FGF-2 and PDGF-BB significantly inhibited the colony formation that was stimulated by the resorbed bone CM (Figure 2B). In separate experiments, we found that 5 μg/ml TGFβ, IGFIR, FGF-1, FGF-2 or PDGF-BB antibodies could neutralize growth-modulating activity of 10 ng/ml TGFβ, 100 ng/ml IGFIR, 25 ng/ml FGF-1, 25 ng/ml FGF-2 and 25 ng/ml PDGF-BB, respectively (data not shown). The concentrations of IGF-I were significantly greater in the resorbed bone CM than control bone CM and were significantly decreased in the presence of ZOL (Figure 2C). Furthermore, recombinant human IGFs showed the greatest dose-dependent stimulation of the colony formation among the growth factors tested (Figure 2D). These results collectively suggest that IGFs released from bone as a consequence of bone resorption are responsible for the promotion of anchorage-independent growth in MDA-MB-231 breast cancer cells.
FIGURE 2. Effects of bone-derived growth factors on the anchorage-independent growth of MDA-MB-231 cells.
(A) Effects of the CM obtained from neonatal mouse calvariae cultures treated without (control bone CM) or with (resorbed bone CM) IL-1β (100 pM) in the absence or presence of ZOL (1 μM) on colony formation of MDA-MB-231 cells (n = 4/group).
* Significantly greater than control bone CM without ZOL (p < 0.01).
# Significantly less than control bone CM without ZOL (p < 0.01).
(B) Effects of neutralizing antibodies (Ab) to various growth factors on colony formation of MDA-MB-231 cells stimulated by resorbed bone CM (n = 4/group).
* Significantly greater than control (p < 0.01).
# Significantly less than resorbed bone CM alone (p < 0.01).
(C) IGF-I production in organ cultures of neonatal mouse calvariae treated without or with IL-1 β in the absence or presence of ZOL (n = 6/group).
* Significantly greater than control bone CM without ZOL (p < 0.01).
# Significantly less than control bone CM without ZOL (p < 0.01).
(D) Effects of growth factors on colony formation of MDA-MB-231 cells. The highest concentration of TGFβ1, IGF-I, IGF-II, FGF-1, FGF-2, PDGF-BB, and BMP-2 was 20, 100, 100, 50, 50, 50, and 100 ng/ml, respectively. These growth factors were serially diluted at 1 to 5 to examine dose-responsiveness (n = 4/group). CM: resorbed bone CM, 20% v/v.
* Significantly different from control (p < 0.01).
Role of IGF/IGFIR in Bone Metastases of MDA-MB-231 Cells
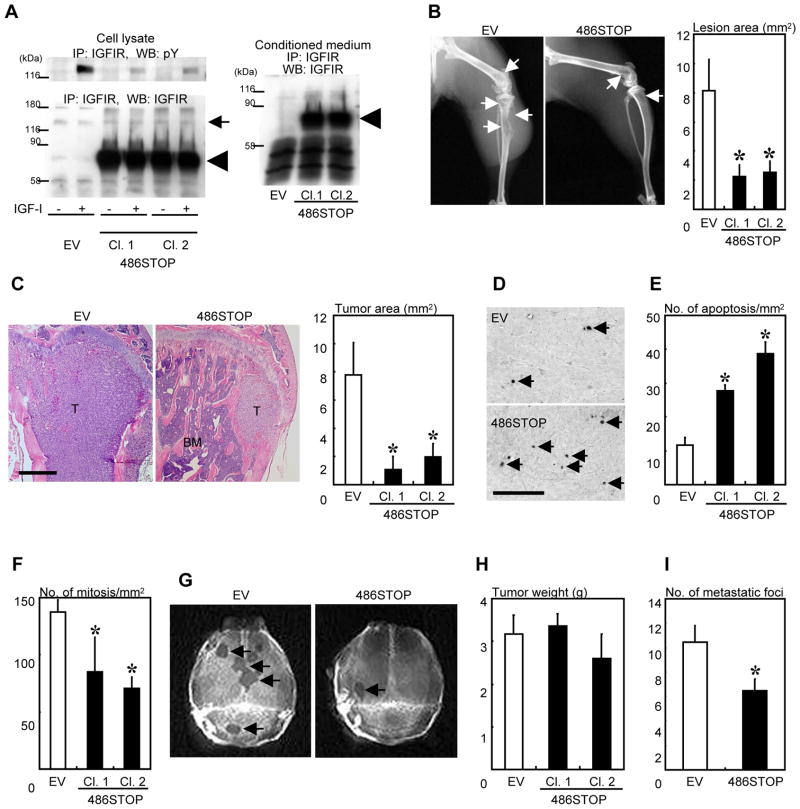
To examine the role of IGFs in the development of bone metastases in vivo, we firstly established two MDA-MB-231 clones (Cl. 1 and Cl. 2) stably transfected with the dominant-negative IGFIR (MDA/486STOP). In MDA/486STOP cells, expression of the endogenous IGFIR was not altered compared with the empty vector-transfected cells (MDA/EV) (Figure 3A, bottom left, thin arrow); however, tyrosine autophosphorylation of IGFIR induced by IGF-I was almost abolished (Figure 3A, top left) in conjunction with the expression of large amounts of the dominant-negative IGFIR (IGFIR/486STOP) (Figure 3A, bottom left, thick arrow). IGFIR/486STOP was secreted into the culture medium from MDA/486STOP cells due to a lack of transmembrane domain (Figure 3A, right), which competitively inhibited the binding of IGFs to the endogenous IGFIR (17).
FIGURE 3. Effects of dominant-negative IGFIR introduction in MDA-MB-231 cells on bone metastases.
(A) Establishment of MDA/486STOP. Tyrosine phosphorylation (left, top) and protein expression (left, bottom) of IGFIR in MDA/EV (EV) and MDA/486STOP (486STOP) were determined by IP-western analysis. Two clones (Cl. 1 and Cl. 2) of MDA/486STOP were examined in the following experiments. After overnight serum starvation, cells were treated with or without 100 ng/ml IGF-I for 10 minutes. The dominant-negative IGFIR (IGFIR/486STOP) was also detected in the conditioned medium of MDA/486STOP (right). (thin arrow: endogenous IGFIR, thick arrow: IGFIR/486STOP)
(B) Radiologic analysis of osteolytic lesions of MDA/EV and MDA/486STOP in the hindlimbs (arrows: osteolytic lesions, n = 10/group).
(C) Histological analysis of bone metastases of MDA/EV and MDA/486STOP (n= 10/group, H-E staining, T: tumor, BM: bone marrow, scale bar = 500 μm).
(D) Representative histological view of apoptotic cancer cells in bone determined by TUNEL staining. (arrows: TUNEL-positive cells, scale bar = 100 μm)
(E) Apoptosis and (F) mitosis in MDA/EV and MDA/486STOP cells colonizing bone (n = 9 for EV and n= 8 for 486STOP clones).
(G) Representative radiographic view of osteolytic lesions in calvariae (arrows) in IL-1β-pretreated mice that were subsequently inoculated with MDA/EV or MDA/486STOP.
(H) Tumor growth of MDA/EV and MDA/486STOP in the orthotopic mammary fat pad in nude mice (n = 5/group).
(I) Lung metastasis of MDA/EV and MDA/486STOP (Clone 1) (n = 7/group). (B, C, E, F, I) * Significantly different from EV (p < 0.05)
We then examined the capacity of MDA/486STOP cells to develop bone metastases. Radiographic analysis showed that the development of osteolytic lesions was markedly suppressed in MDA/486STOP (Figure 3B). Histological examination also demonstrated that the metastatic tumor burden of MDA/486STOP in bone was significantly reduced compared with MDA/EV (Figure 3C). Osteoclast number was not different between the groups (data not shown). Terminal deoxynucleotidyl transferase-mediated dUTP nick end labeling (TUNEL) staining revealed that apoptosis was increased in MDA/486STOP (Figure 3D, E), whereas cell mitosis was significantly decreased (Figure 3F). In addition, IL-1β-induced metastases to calvarial bones, as determined according to the same method as Figure 1A, were markedly reduced in MDA/486STOP (Figure 3G). These results suggest that IGFIR activation by bone-derived IGF facilitates the development of bone metastases by decreasing apoptosis and increasing proliferation of cancer cells colonizing bone.
To determine whether these effects of IGF/IGFIR are specific for bone metastases, tumor growth in the orthotopic mammary fat pad and the capacity to develop lung metastases were examined. Tumor growth of MDA/486STOP in the orthotopic site was not different from that of MDA/EV (Figure 3H). Lung metastases were marginally reduced in MDA/486STOP (Figure 3I).
Since IGFIR/486STOP is a secreted form of IGFIR, the possibility remains that it decreases bone metastasis via inhibition of IGFIR signaling not only in MDA-MB-231 cells but also other neighboring bone-resident cells. To exclude this, we established MDA-MB-231 clones in which IGFIR was stably knocked down (MDA/shIGFIR) and tested their ability to develop bone metastases. Consistent with the results of MDA/486STOP, IGFIR knockdown also significantly reduced bone metastases (Supplementary Figure 1), suggesting the primary role of IGFIR signals in cancer cells in the development of bone metastasis.
As an alternative approach to verify the involvement of bone-derived IGF and IGFIR activation in bone metastasis, we performed experiments using MDA-MB-231 cells overexpressing wild-type IGFIR (MDA/IGFIR). The expression of IGFIR protein (Figure 4A, bottom) and its tyrosine autophosphorylation induced by IGF-I (Figure 4A, top) were markedly increased in MDA/IGFIR compared with MDA/EV. MDA/IGFIR showed marked increases in osteolytic lesions (Figure 4B and 4C) and tumor area in bone (Figure 4D). MDA/IGFIR rarely showed metastases to calvarial bones (data not shown). Metastasis to lung was not different between MDA/IGFIR and MDA/EV (data not shown). Tumor growth at the mammary fat pad did not significantly differ between MDA/IGFIR and MDA/EV (Figure 4E). Taken together, these results are in support of the notion that IGF/IGFIR axis plays a role selectively in bone metastasis of MDA-MB-231 breast cancer cells.
FIGURE 4. Effects of wild-type IGFIR overexpression in MDA-MB-231 cells on bone metastases.
(A) Tyrosine phosphorylation and expression of IGFIR in MDA/EV (EV) and MDA/IGFIR (IGFIR) determined by IP-western analysis. After overnight serum starvation, cells were treated with or without 100 ng/ml IGF-I for 10 minutes.
(B, C) Radiologic analysis of osteolytic lesions of MDA/EV and MDA/IGFIR in the hindlimbs (arrows: osteolytic lesions, n = 5 for EV and n= 7 for IGFIR clones).
(D) Histomorphometric analysis of tumor burden of MDA/EV and MDA/IGFIR in the hindlimbs (n = 5 for EV and n= 7 for IGFIR clones).
(E) Tumor development of MDA/EV and MDA/IGFIR in the orthotopic mammary fat pad in nude mice (n= 3/group).
(C, D) * Significantly different from EV (p < 0.05).
IGFIR Expression in Bone Metastases in Cancer Patients
To explore the clinical relevance of these findings obtained in preclinical settings, we examined the expression of IGFIR in cancer cells in bone metastases in patients with several types of cancers. Immunohistochemical study revealed that 13 out of 15 cases (86.7%) (Figure 5A) showed strong expression of IGFIR (Figure 5B) in cancer cells colonizing bone, suggesting an important role of IGF/IGFIR axis in bone metastases in cancer patients regardless of the primary site of tumors.
FIGURE 5. Expression of IGFIR in bone metastases in cancer patients.
(A) Summary of the clinical samples.
(B) Representative histological view of IGFIR expression in bone metastases by immunohistochemistry (Case 12: IGFIR-negative, Case 1, 10, and 13: IGFIR-positive, T: tumor, asterisk: bone, scale bar = 100 μm)
Role of Akt in Bone Metastases of MDA-MB-231 Cells
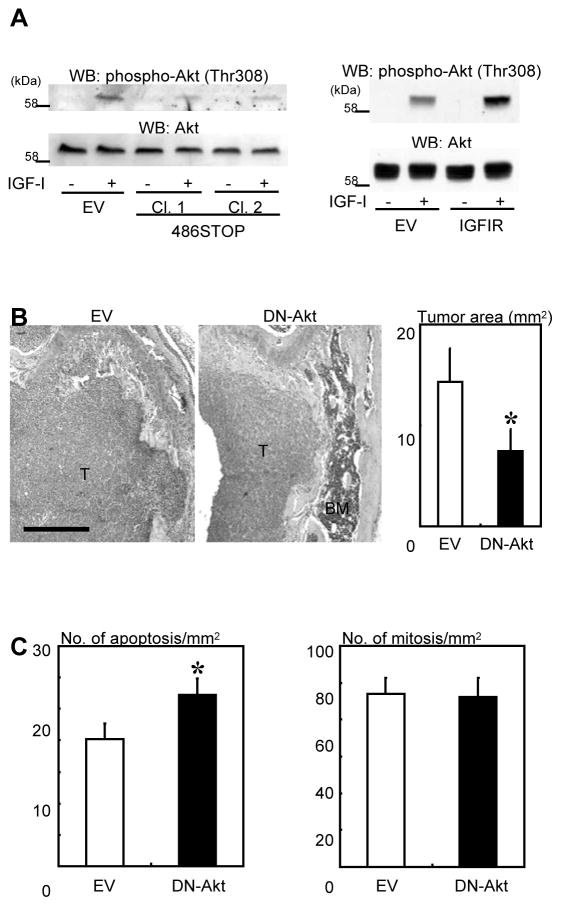
Since Figure 3D and 3E show that increased apoptosis in MDA/486STOP is associated with reduced bone metastases, we next studied the involvement of the serine/threonine kinase Akt in the development of bone metastases. Akt is a downstream molecule of IGFIR signaling and is widely recognized as a cell survival or an anti-apoptotic factor (12, 13, 21). Western blot analysis showed that IGF-I induced phosphorylation at threonine 308 (Figure 6A, top left) and serine 473 (data not shown) of Akt in MDA/EV. Phosphorylation at threonine 308 was abolished in MDA/486STOP (Figure 6A, top left) and increased in MDA/IGFIR (Figure 6A, top right). These results show that IGF-I/IGFIR axis activated Akt. To examine the role of Akt activation in bone metastasis, we established MDA-MB-231 cells expressing dominant-negative Akt (MDA/DN-Akt). Histological and histomorphometric analysis showed that tumor burden in bone was significantly reduced in MDA/DN-Akt compared with MDA/EV (Figure 6B). The number of apoptosis in MDA/DN-Akt cells in bone determined by TUNEL staining was significantly increased, while the number of mitotic cells was not changed (Figure 6C).
FIGURE 6. Role of Akt signaling in bone metastases of MDA-MB-231.
(A) Top: IGF-I-induced Akt phosphorylation at threonine 308 in MDA/486STOP (486STOP) (left) and MDA/IGFIR (IGFIR) (right) determined by western blot. After overnight serum starvation, cells were treated with or without 100 ng/ml IGF-I for 10 minutes. Bottom: Expression of Akt protein determined by western blot.
(B) Histological view (left) and histomorphometric analysis (right) of bone metastases of MDA-MB-231 cells stably transfected with dominant-negative Akt (MDA/DN-Akt) in nude mice (n = 15 for MDA/EV (EV) and n= 14 for MDA/DN-Akt (DN-Akt); H-E staining, T: tumor, BM: bone marrow, scale bar = 500 μm).
(C) Histomorphometric analysis of number of apoptosis and mitosis in MDA/EV and MDA/DN-Akt cells in bone metastases (n = 9 for MDA/EV and n= 7 for MDA/DN-Akt).
(B, C) * Significantly different from EV (p < 0.05)
In separate experiments, we observed that IGF-I caused tyrosine phosphorylation of insulin receptor substrate-1 (IRS-1) and p85 phosphatidylinositol 3-kinase (PI3K) (29), leading to a complex formation of IRS-1 with p85 PI3K upstream of Akt activation. Thus, the conventional IGF-I/IGFIR signaling pathway is propagated in MDA-MB-231 human breast cancer cells.
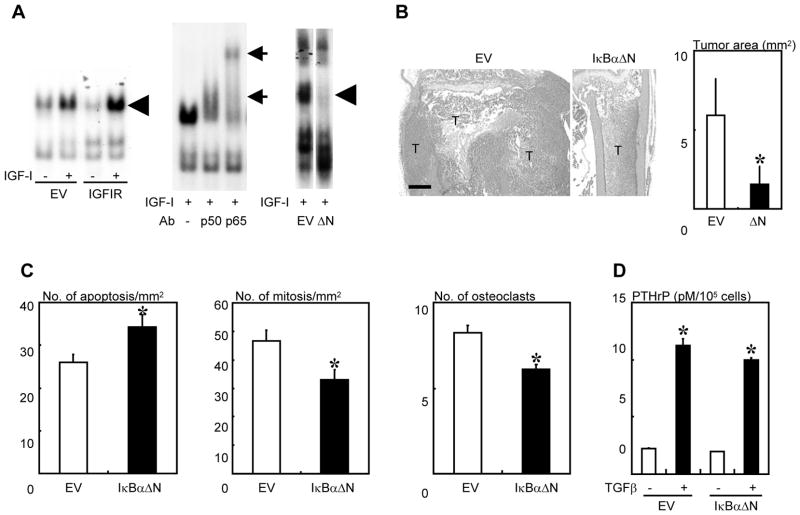
Role of NF-κB in Bone Metastases of MDA-MB-231 Cells
As another downstream molecule of IGFIR signaling whose activation is associated with survival of cancer cells, we examined the role of the transcription factor NF-κB in bone metastasis. EMSA analysis demonstrated that IGF-I activated the p50 and p65 subunit of NF-κB in MDA/EV (Figure 7A, left and center). MDA/IGFIR exhibited increased NF-κB activation (Figure 7A, left). IGF-I failed to activate NF-κB in MDA/486STOP cells (data not shown). NF-κB activation was also markedly suppressed in MDA-MB-231 cells expressing dominant-negative IκBα (MDA/IκBαΔN) (Figure 7A, right). Histological and histomorphometric analysis revealed that MDA/IκBαΔN developed significantly reduced bone metastases (Figure 7B). Apoptosis in MDA/IκBαΔN cells in bone metastases was significantly increased compared with MDA/EV cells (Figure 7C), whereas mitosis in MDA/IκBαΔN was significantly decreased (Figure 7C). Osteoclast number at tumor-bone interface was decreased in bone metastases of MDA/IκBαΔN (Figure 7C). Of note, however, production of PTHrP, a potent stimulator of osteoclastogenesis, in MDA/IκBαΔN cells in the absence or presence of TGFβ was not changed compared with MDA/EV cells (Figure 7D).
FIGURE 7. Role of NF-κB signaling in bone metastases of MDA-MB-231.
(A) IGF-I-induced activation of NF-κB in MDA/IGFIR (IGFIR, left) and MDA/IκBαΔN ( N, right) determined by EMSA (EV: MDA/EV). After overnight serum starvation, cells were treated with or without 500 ng/ml IGF-I for 4 hours. Thick arrows indicate specific bands for NF-κB. The specificity was confirmed by supershift assay using antibodies to NF-κB subunits p50 and p65 (center, thin arrows).
(B) Histological analysis of bone metastases of MDA/EV and MDA/IκBαΔN (IκBαΔN or N) (n = 6 for EV and n= 5 for IκBαΔN; H-E staining, T: tumor, BM: bone marrow, scale bar = 500 μm).
(C) Histomorphometric analysis of apoptosis and mitosis in MDA/EV and MDA/IκBαΔN cells colonizing bone and osteoclast number at tumor-bone interface in bone metastases (n = 6 for EV and n= 5 for IκBαΔN).
(D) Production of PTHrP by MDA/EV and MDA/IκBαΔN in culture in the presence or absence of TGF-β (5 ng/ml) (n = 4/group).
(B, C) * Significantly different from EV (p < 0.05).
(D) * Significantly different from EV in the absence of TGF-β (p < 0.01).
DISCUSSION
Bone is one of the most preferential target organs of cancer metastasis (1–3). Although the precise mechanism by which cancer cells preferentially spread to bone has not been fully understood, it has been suggested that bone-derived growth factors create favorable microenvironment for cancer cells to survive and colonize bone. Consistent with this notion, our in vivo study showed that stimulation of osteoclastic bone resorption in calvarial bones by repeated injections of IL-1β prior to cell inoculation markedly increased subsequent MDA-MB-231 breast cancer cell metastases to that local site. We previously described that MDA-MB-231 cells rarely metastasize to calvarial bones following intracardiac inoculation in this model for unknown reasons (7). In contrast, inhibition of bone resorption by co-treatment with IL-1β and the BP ZOL, a potent inhibitor of osteoclastic bone resorption, significantly decreased MDA-MB-231 metastases to calvarial bones. The CM harvested from resorbed bones increased anchorage-independent growth of MDA-MB-231 cell in soft agar compared to that of control bone. On the other hand, the anchorage-independent growth was not stimulated by the CM harvested from bones treated with IL-1β together with ZOL. We previously described that bone-stored growth factors are released from resorbed bone into the culture medium in active forms (8). Taken together, these results suggest that stimulation of bone resorption can induce bone metastases at this rare site via promotion of breast cancer cell colonization due to increased supply of bone-stored growth factors. Our experiments prove that cancer metastasis to bone is dependent on the extent of osteoclastic bone resorption.
Next we studied which a bone-stored growth factor is responsible for promotion of anchorage-independent growth of MDA-MB-231 cells. To approach this, the effects of the neutralizing antibodies to the growth factors that are known to be stored in bone (6, 7) were examined in colony formation assay. Notably, anchorage-independent growth-stimulatory effects of the resorbed bone CM on MDA-MB-231 cells was blocked by the neutralizing antibody to IGFIR but not TGFβ, FGF and PDGF. Recombinant human IGF-I or IGF-II showed the greatest stimulation of anchorage-independent growth of the growth factors tested. The CM harvested from resorbed bone contained increased amounts of IGF-I compared with that harvested from control bone and IGF-I concentration was profoundly decreased in the CM harvested from bone in which bone resorption was inhibited by ZOL. Moreover, our in vivo studies demonstrated that the number of mitosis was decreased in MDA/486STOP cells in which IGFIR signaling was disrupted compared with that in MDA/EV. These results collectively suggest that IGF-I is at least one of the growth factors responsible for promotion of cancer cell colonization in bone.
Earlier clinical studies have reported that aggressive breast cancers express increased IGFIR (14). However, it has not been examined whether human cancers spread to bone express elevated IGFIR. Our immunohistochemical study using clinical specimens obtained at surgery exhibited that cancer cells colonizing bone were IGFIR-positive regardless of the primary site of tumors. Although it is unknown whether these cancers also express IGFIR at primary site, these observations suggest that IGFIR expression is a requisite for metastatic cancer cells to appropriately respond to bone-derived IGFs to lead to bone metastases. Indeed, disruption of IGF signaling by introducing dominant-negative IGFIR or short hairpin RNA against IGFIR in MDA-MB-231 human breast cancer cells (MDA/486STOP or MDA/shIGFIR) significantly reduced bone metastases. Similarly, an anti-IGF neutralizing monoclonal antibody decreases tumor burden of MCF-7 human breast cancer in bone (30). Conversely, overexpression of wild-type IGFIR in MDA-MB-231 cells (MDA/IGFIR) significantly increased bone metastases in this study. Furthermore, we previously reported that the bone-seeking clone of MDA-MB-231 cells exhibits higher IGFIR expression and responsiveness to IGF-I than parental cells (31). In contrast to these results, however, our in silico analysis of the published microarray database GSE14244 and GSE16554 that had been submitted to NCBI Gene Expression Omnibus (GEO) (32) showed no differences in IGFIR expression between bone-metastatic and parental MDA-MB-231 cells (data not shown). Thus, elevated expression of IGFIR in cancer cells may not always be a prerequisite for causing bone metastasis. Nonetheless, our data suggest an important role of IGF/IGFIR axis in the development of bone metastasis in breast cancer.
Although data are not shown here, we found that the CM of resorbed bone not only stimulated anchorage-independent growth but also PTHrP production in MDA-MB-231 cells. Of note, this effect was blocked by the neutralizing antibody to TGFβ but not IGFIR. There were increased amounts of TGFβ in the CM of resorbed bone as determined by the bioassay using mink lung epithelial cells (33). Recombinant TGFβ1 (0.5 – 5 ng/ml) increased PTHrP production in MDA-MB-231 cells in a dose-dependent manner, whereas IGF-I and IGF-II had no effects. These results are consistent with those previously reported from our group (9, 34). PTHrP is a potent stimulator of osteoclastic bone resorption and is one of the primary cytokines that play a critical role in the pathophysiology of bone metastasis of breast cancer (1–3). We have also reported that bone-derived TGFβ stimulates COX-2 expression in MDA-MB-231 cells and a COX-2 inhibitor reduces bone metastases (35). Moreover, it has recently been reported that bone-derived TGFβ increases Jagged1 expression in metastatic breast cancer cells, which directly stimulates osteoclast differentiation through activating Notch pathway (36). Taken together, our results suggest that osteoclastic bone resorption promotes bone metastasis at least in part through releasing IGFs that stimulate cell proliferation and TGFβ that increases PTHrP production and COX-2 and Jagged1 expression in breast cancer cells metastasized in bone, which consequently leads to the development and progression of bone metastases.
IGF has been also implicated in cell survival (12, 13). Our results showed that apoptosis in MDA/486STOP cells in bone was significantly increased compared with MDA/EV, suggesting that activation of IGFIR signaling by bone-derived IGFs protected cancer cells from apoptosis. Akt is a well-described survival factor that is activated by IGFs (12, 13, 21). We confirmed that IGF-I activated Akt in MDA-MB-231 cells and found that this IGF-I-induced Akt activation was suppressed or enhanced in MDA/486STOP or MDA/IGFIR cells, respectively. More importantly, suppression of Akt signals by introduction of dominant-negative Akt in MDA-MB-231 cells (MDA/DN-Akt) reduced bone metastases with increased numbers of apoptosis in cancer cells in bone. These results show that Akt is a downstream molecule of IGF/IGFIR signaling and mediates anti-apoptotic effects of IGFs on cancer cells in bone. Thus, IGF-induced Akt activation takes a part in the promotion of bone metastases.
NF-κB, another well-known survival factor (19), is one of the downstream signaling molecules of IGFIR/Akt pathway (18, 20). Our in vitro studies showed that IGF-I activated NF-κB in MDA-MB-231 cells and the IGF-I-induced NF-κB activation was enhanced or suppressed in MDA/IGFIR or MDA/486STOP, respectively. Our in vivo study demonstrated that the dominant-negative inhibition of NF-κB by introducing the truncated IκBα reduced bone metastases. Furthermore, apoptosis in MDA/IκBαΔN cells in bone was significantly increased compared with MDA/EV. These results suggest that the activation of NF-κB by IGF/IGFIR axis also promotes bone metastases through suppression of apoptosis in cancer cells. Propagation of IGFIR/Akt/NF-κB axis in breast cancer cells by bone-derived IGFs facilitates bone metastasis and disruption of this axis may be a promising approach to inhibit bone metastasis of breast cancer.
Since NF-κB is a transcription factor, identification of a transcriptional target molecule is important to further elucidate the molecular mechanism underlying bone metastasis of breast cancer. We have previously shown that hypoxia-inducible factor-1α (HIF-1α) promotes bone metastasis of MDA-MB-231 cells partly via increased osteoclastogenesis and that suppression of HIF-1α decreases bone metastases (37). It has also been reported that NF-κB regulates HIF-1α gene expression at transcriptional levels (38) and that NF-κB-HIF-1 interaction contributes to an increase in breast cancer metastatic capacity (39). Thus, HIF-1α could be one of the candidate target molecules of NF-κB that can be implicated in bone metastases.
NF-κB transcriptionally regulates the expression of a variety of cytokines including IL-1β, IL-6, TNFs, and macrophage colony-stimulating factor (M-CSF) (19), all of which are stimulators of osteoclastogenesis and bone resorption (40). Activation of NF-κB may augment cancer-induced bone destruction through increased production of these osteoclastogenic cytokines. The result that osteoclast number was decreased in bone metastases of MDA/IκBαΔN cells supports this notion. It should be noted that the production of PTHrP was not changed in MDA/IκBαΔN cells compared with MDA/EV cells. It is therefore unlikely that the reduced number of osteoclasts in bone metastases of MDA/IκBαΔN cells is due to decreased PTHrP production and that IGFIR/NF-κB pathway is involved in PTHrP-mediated osteoclastogenesis. In this context, Park et al. reported that granulocyte macrophage-colony stimulating factor (GM-CSF) is a target of NF-κB, which mediates osteolytic bone metastasis of breast cancer by stimulating osteoclast development (41). Contribution of NF-κB to osteoclast recruitment and bone resorption in the pathophysiology of bone metastasis remains to be elucidated.
IGFs are well-known mitogenic factors (12, 13). Our present study showed that IGFs increased colony formation of MDA-MB-231 cells. Furthermore, mitotic cells were decreased in MDA/486STOP colonized bone. Similar results were also observed in bone metastases of MDA/IκBαΔN but not in MDA-DN-Akt. These results suggest that IGFIR signaling is not necessarily acting through Akt to activate NF-κB.
Despite that MDA/486STOP showed reduced bone metastases, tumor development of MDA/486STOP at the orthotopic mammary fat pad was not decreased compared to that of MDA/EV. Furthermore, pulmonary metastasis of MDA/486STOP or MDA/IGFIR was changed to a marginal extent. These results raise the possibility that IGF actions are relatively bone-selective. Murphy et al. reported that the expression of IGF-I and IGF-II in lung and mammary gland is rarely detectable (42). Wu et al. have shown that hepatic metastasis of colon cancer is reduced in the liver-specific IGF-I-deficient mice (43). From these earlier studies together with our results, it is possible that organ/tissue IGF concentration is influential on the behaviors of cancer cells arresting at the local site. In this regard, metastatic breast cancer cells with increased IGFIR expression can take advantage of bone in which IGFs are abundantly stored. It is therefore expected that blockade of IGF/IGFIR axis using agents including neutralizing monoclonal antibodies and small molecule tyrosine kinase inhibitors (12, 13) may suppress cancer cells in bone more effectively and selectively than other organs/tissues.
In conclusion, our data suggest that bone-derived IGFs, which are released from bone in substantial amounts by osteoclastic bone resorption, activate IGFIR, Akt, and NF-κB signaling pathway, thereby increasing proliferation and decreasing apoptosis in breast cancer cells that are colonizing bone. These events consequently lead to the development and progression of bone metastases. Given the abundance of IGFs in bone, targeting IGF/IGFIR/Akt/NF-κB signaling pathway may be a selective and effective approach for the treatment of bone metastases.
Supplementary Material
Acknowledgments
Grant support: This work was supported by Grants-in-aid 12771104, 14771020 (T. Hiraga), 11307041 (T. Yoneda), 12137205 (T. Yoneda), and 21st Century C. O. E. program (T. Yoneda) from the Ministry of Education, Culture, Sports, Science and Technology, Japan, and NIH grants PO1-CA40035 (T. Yoneda), RO1-AR28149 (T. Yoneda), and RO1-DK45229 (T. Yoneda).
The authors are grateful to Drs. Diane Prager, Renato Baserga, Sandeep R. Datta and Dean W. Ballard for providing wild-type IGFIR, IGFIR/486STOP, Akt (K179M) and N-terminus-truncated IκBα cDNA constructs, respectively.
Footnotes
Conflict of interest: All the authors have no potential conflicts of interest with regard to the manuscript submitted.
References
- 1.Roodman G. Mechanisms of bone metastasis. N Engl J Med. 2004;350:1655–64. doi: 10.1056/NEJMra030831. [DOI] [PubMed] [Google Scholar]
- 2.Yoneda T, Hiraga T. Crosstalk between cancer cells and bone microenvironment in bone metastasis. Biochem Biophys Res Commun. 2005;328:679–87. doi: 10.1016/j.bbrc.2004.11.070. [DOI] [PubMed] [Google Scholar]
- 3.Weilbaecher KN, Guise TA, McCauley LK. Cancer to bone: a fatal attraction. Nat Rev Cancer. 2011;11:411–25. doi: 10.1038/nrc3055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hiraga T, Williams P, Mundy G, Yoneda T. The bisphosphonate ibandronate promotes apoptosis in MDA-MB-231 human breast cancer cells in bone metastases. Cancer Res. 2001;61:4418–24. [PubMed] [Google Scholar]
- 5.Coleman R, Cook R, Hirsh V, Major P, Lipton A. Zoledronic acid use in cancer patients: more than just supportive care? Cancer. 2011;117:11–23. doi: 10.1002/cncr.25529. [DOI] [PubMed] [Google Scholar]
- 6.Hauschka P, Mavrakos A, Iafrati M, Doleman S, Klagsbrun M. Growth factors in bone matrix. Isolation of multiple types by affinity chromatography on heparin-Sepharose. J Biol Chem. 1986;261:12665–74. [PubMed] [Google Scholar]
- 7.Yoneda T, Sasaki A, Mundy G. Osteolytic bone metastasis in breast cancer. Breast Cancer Res Treat. 1994;32:73–84. doi: 10.1007/BF00666208. [DOI] [PubMed] [Google Scholar]
- 8.Pfeilschifter J, Mundy G. Modulation of type beta transforming growth factor activity in bone cultures by osteotropic hormones. Proc Natl Acad Sci U S A. 1987;84:2024–8. doi: 10.1073/pnas.84.7.2024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yin J, Selander K, Chirgwin J, Dallas M, Grubbs B, Wieser R, et al. TGF-beta signaling blockade inhibits PTHrP secretion by breast cancer cells and bone metastases development. J Clin Invest. 1999;103:197–206. doi: 10.1172/JCI3523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Korpal M, Yan J, Lu X, Xu S, Lerit DA, Kang Y. Imaging transforming growth factor-beta signaling dynamics and therapeutic response in breast cancer bone metastasis. Nat Med. 2009;15:960–6. doi: 10.1038/nm.1943. [DOI] [PubMed] [Google Scholar]
- 11.Thomas RJ, Guise TA, Yin JJ, Elliott J, Horwood NJ, Martin TJ, et al. Breast cancer cells interact with osteoblasts to support osteoclast formation. Endocrinology. 1999;140:4451–8. doi: 10.1210/endo.140.10.7037. [DOI] [PubMed] [Google Scholar]
- 12.Samani A, Yakar S, LeRoith D, Brodt P. The role of the IGF system in cancer growth and metastasis: overview and recent insights. Endocr Rev. 2007;28:20–47. doi: 10.1210/er.2006-0001. [DOI] [PubMed] [Google Scholar]
- 13.Maki RG. Small is beautiful: insulin-like growth factors and their role in growth, development, and cancer. J Clin Oncol. 2010;28:4985–95. doi: 10.1200/JCO.2009.27.5040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Peyrat J, Bonneterre J, Beuscart R, Djiane J, Demaille A. Insulin-like growth factor 1 receptors in human breast cancer and their relation to estradiol and progesterone receptors. Cancer Res. 1988;48:6429–33. [PubMed] [Google Scholar]
- 15.Resnik J, Reichart D, Huey K, Webster N, Seely B. Elevated insulin-like growth factor I receptor autophosphorylation and kinase activity in human breast cancer. Cancer Res. 1998;58:1159–64. [PubMed] [Google Scholar]
- 16.van Golen C, Schwab T, Kim B, Soules M, Su Oh S, Fung K, et al. Insulin-like growth factorI receptor expression regulates neuroblastoma metastasis to bone. Cancer Res. 2006;66:6570–8. doi: 10.1158/0008-5472.CAN-05-1448. [DOI] [PubMed] [Google Scholar]
- 17.Reiss K, D’Ambrosio C, Tu X, Tu C, Baserga R. Inhibition of tumor growth by a dominant negative mutant of the insulin-like growth factor I receptor with a bystander effect. Clin Cancer Res. 1998;4:2647–55. [PubMed] [Google Scholar]
- 18.Bertrand F, Philippe C, Antoine P, Baud L, Groyer A, Capeau J, et al. Insulin activates nuclear factor kappa B in mammalian cells through a Raf-1-mediated pathway. J Biol Chem. 1995;270:24435–41. doi: 10.1074/jbc.270.41.24435. [DOI] [PubMed] [Google Scholar]
- 19.Karin M. Nuclear factor-kappaB in cancer development and progression. Nature. 2006;441:431–6. doi: 10.1038/nature04870. [DOI] [PubMed] [Google Scholar]
- 20.Mitsiades C, Mitsiades N, Poulaki V, Schlossman R, Akiyama M, Chauhan D, et al. Activation of NF-kappaB and upregulation of intracellular anti-apoptotic proteins via the IGF-1/Akt signaling in human multiple myeloma cells: therapeutic implications. Oncogene. 2002;21:5673–83. doi: 10.1038/sj.onc.1205664. [DOI] [PubMed] [Google Scholar]
- 21.Manning BD, Cantley LC. AKT/PKB signaling: navigating downstream. Cell. 2007;129:1261–74. doi: 10.1016/j.cell.2007.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nishimura R, Moriyama K, Yasukawa K, Mundy G, Yoneda T. Combination of interleukin-6 and soluble interleukin-6 receptors induces differentiation and activation of JAK-STAT and MAP kinase pathways in MG-63 human osteoblastic cells. J Bone Miner Res. 1998;13:777–85. doi: 10.1359/jbmr.1998.13.5.777. [DOI] [PubMed] [Google Scholar]
- 23.Michigami T, Hiraga T, Williams PJ, Niewolna M, Nishimura R, Mundy GR, et al. The effect of the bisphosphonate ibandronate on breast cancer metastasis to visceral organs. Breast Cancer Res Treat. 2002;75:249–58. doi: 10.1023/a:1019905111666. [DOI] [PubMed] [Google Scholar]
- 24.Garrett I, Mundy G. Relationship between interleukin-1 and prostaglandins in resorbing neonatal calvaria. J Bone Miner Res. 1989;4:789–94. doi: 10.1002/jbmr.5650040520. [DOI] [PubMed] [Google Scholar]
- 25.Mbalaviele G, Dunstan C, Sasaki A, Williams P, Mundy G, Yoneda T. E-cadherin expression in human breast cancer cells suppresses the development of osteolytic bone metastases in an experimental metastasis model. Cancer Res. 1996;56:4063–70. [PubMed] [Google Scholar]
- 26.Hiraga T, Nakamura H. Imatinib mesylate suppresses bone metastases of breast cancer by inhibiting osteoclasts through the blockade of c-Fms signals. Int J Cancer. 2009;124:215–22. doi: 10.1002/ijc.23903. [DOI] [PubMed] [Google Scholar]
- 27.Boyce BF, Aufdemorte TB, Garrett IR, Yates AJ, Mundy GR. Effects of interleukin-1 on bone turnover in normal mice. Endocrinology. 1989;125:1142–50. doi: 10.1210/endo-125-3-1142. [DOI] [PubMed] [Google Scholar]
- 28.Freedman VH, Shin SI. Cellular tumorigenicity in nude mice: correlation with cell growth in semi-solid medium. Cell. 1974;3:355–9. doi: 10.1016/0092-8674(74)90050-6. [DOI] [PubMed] [Google Scholar]
- 29.Jackson JG, Zhang X, Yoneda T, Yee D. Regulation of breast cancer cell motility by insulin receptor substrate-2 (IRS-2) in metastatic variants of human breast cancer cell lines. Oncogene. 2001;20:7318–25. doi: 10.1038/sj.onc.1204920. [DOI] [PubMed] [Google Scholar]
- 30.Sangai T, Fujimoto H, Miyamoto S, Maeda H, Nakamura M, Ishii G, et al. Roles of osteoclasts and bone-derived IGFs in the survival and growth of human breast cancer cells in human adult bone implanted into nonobese diabetic/severe combined immunodeficient mice. Clin Exp Metastasis. 2008;25:401–10. doi: 10.1007/s10585-008-9144-8. [DOI] [PubMed] [Google Scholar]
- 31.Yoneda T, Williams P, Hiraga T, Niewolna M, Nishimura R. A bone-seeking clone exhibits different biological properties from the MDA-MB-231 parental human breast cancer cells and a brain-seeking clone in vivo and in vitro. J Bone Miner Res. 2001;16:1486–95. doi: 10.1359/jbmr.2001.16.8.1486. [DOI] [PubMed] [Google Scholar]
- 32.Lu X, Kang Y. Efficient acquisition of dual metastasis organotropism to bone and lung through stable spontaneous fusion between MDA-MB-231 variants. Proc Natl Acad Sci U S A. 2009;106:9385–90. doi: 10.1073/pnas.0900108106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jennings JC, Mohan S. Heterogeneity of latent transforming growth factor-beta isolated from bone matrix proteins. Endocrinology. 1990;126:1014–21. doi: 10.1210/endo-126-2-1014. [DOI] [PubMed] [Google Scholar]
- 34.Guise T, Yin J, Taylor S, Kumagai Y, Dallas M, Boyce B, et al. Evidence for a causal role of parathyroid hormone-related protein in the pathogenesis of human breast cancer-mediated osteolysis. J Clin Invest. 1996;98:1544–9. doi: 10.1172/JCI118947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hiraga T, Myoui A, Choi M, Yoshikawa H, Yoneda T. Stimulation of cyclooxygenase-2 expression by bone-derived transforming growth factor-beta enhances bone metastases in breast cancer. Cancer Res. 2006;66:2067–73. doi: 10.1158/0008-5472.CAN-05-2012. [DOI] [PubMed] [Google Scholar]
- 36.Sethi N, Dai X, Winter CG, Kang Y. Tumor-derived JAGGED1 promotes osteolytic bone metastasis of breast cancer by engaging notch signaling in bone cells. Cancer Cell. 2011;19:192–205. doi: 10.1016/j.ccr.2010.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hiraga T, Kizaka-Kondoh S, Hirota K, Hiraoka M, Yoneda T. Hypoxia and hypoxia-inducible factor-1 expression enhance osteolytic bone metastases of breast cancer. Cancer Res. 2007;67:4157–63. doi: 10.1158/0008-5472.CAN-06-2355. [DOI] [PubMed] [Google Scholar]
- 38.Majmundar AJ, Wong WJ, Simon MC. Hypoxia-inducible factors and the response to hypoxic stress. Mol Cell. 2010;40:294–309. doi: 10.1016/j.molcel.2010.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bendinelli P, Matteucci E, Maroni P, Desiderio MA. NF-kappaB activation, dependent on acetylation/deacetylation, contributes to HIF-1 activity and migration of bone metastatic breast carcinoma cells. Mol Cancer Res. 2009;7:1328–41. doi: 10.1158/1541-7786.MCR-08-0548. [DOI] [PubMed] [Google Scholar]
- 40.Asagiri M, Takayanagi H. The molecular understanding of osteoclast differentiation. Bone. 2007;40:251–64. doi: 10.1016/j.bone.2006.09.023. [DOI] [PubMed] [Google Scholar]
- 41.Park BK, Zhang H, Zeng Q, Dai J, Keller ET, Giordano T, et al. NF-kappaB in breast cancer cells promotes osteolytic bone metastasis by inducing osteoclastogenesis via GM-CSF. Nat Med. 2007;13:62–9. doi: 10.1038/nm1519. [DOI] [PubMed] [Google Scholar]
- 42.Murphy L, Bell G, Friesen H. Tissue distribution of insulin-like growth factor I and II messenger ribonucleic acid in the adult rat. Endocrinology. 1987;120:1279–82. doi: 10.1210/endo-120-4-1279. [DOI] [PubMed] [Google Scholar]
- 43.Wu Y, Yakar S, Zhao L, Hennighausen L, LeRoith D. Circulating insulin-like growth factor-I levels regulate colon cancer growth and metastasis. Cancer Res. 2002;62:1030–5. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.