Abstract
Background
The incidence of cancer continues to rise all over the world and current projections show that there will be 1.27 million new cases and almost 1 million deaths by 2030. In view of the rising incidence of cancer in sub-Saharan Africa, urgent steps are needed to guide appropriate policy, health sector investment and resource allocation. We posit that hospital based cancer registries (HBCR) are fundamental sources of information on the frequent cancer sites in limited resource regions where population level data is often unavailable. In regions where population based cancer registries are not in existence, HBCR are beneficial for policy and planning.
Materials and Methods
Nineteen of twenty-one cancer registries in Nigeria met the definition of HBCR, and from these registries, we requested data on cancer cases recorded from January 2009 to December 2010. 16 of the 19 registries (84%) responded. Data on year hospital was established; year cancer registry was established, no of pathologists and types of oncology services available in each tertiary health facility were shown. Analysis of relative frequency of cancers in each HBCR, the basis of diagnosis recorded in the HBCR and the total number of cases recorded by gender was carried out.
Results
The total number of cancers registered in these 11 hospital based cancer registries in 2009 and 2010 was 6484. The number of new cancer cases recorded annually in these hospital based cancer registries on average were 117 cases in males and I77 cases in females. Breast and cervical cancer were the most common cancers seen in women while prostate cancer was the commonest among men seen in these tertiary hospitals.
Conclusion
Information provided by HBCR is beneficial and can be utilized for the improvement of cancer care delivery systems in low and middle income countries where there are no population based cancer registries.
Keywords: Hospital based cancer registries (HBCR), population based cancer registries (PBCR), low and middle income countries (LMIC)
Background
Cancer has become a major global public health problem. In 2008, there were 12.7 million new cases of cancer and 7.6 million cancer related deaths worldwide.(1) Africa, with a population of approximately 1 billion people (15% of the world’s population) contributed 681,000 new cancer cases (5% of all cases worldwide) and 512,000 deaths (7% of all cancer deaths) to the worldwide estimates in 2008.(2)The incidence of cancer continues to rise all over the world and current projections show that there will be 1.27 million new cases and almost 1 million deaths by 2030.(2) Low and middle income countries (LMIC) will contribute more than 80% of the new cases worldwide.(2)
Africa continues to face challenges arising from sustained epidemics of infectious diseases such as malaria, HIV/AIDS and Tuberculosis.(3)In the past decades, as life expectancy on the continent improved and the risk of death from infectious diseases declined, the incidence of non-communicable diseases including cancer has been rising significantly.(4)Most of the increase in cancer incidence in Africa is attributable to this increase in life expectancy but changing dietary and physical activity patterns, tobacco use, and the advent of the HIV-AIDS epidemic are major contributors.(2, 5, 6)
In view of the rising incidence of cancer in sub-Saharan Africa, urgent steps are needed to guide appropriate policy, health sector investment and resource allocation. To be effective, these interventions need to be guided by data on the incident and prevalent cancers so that limited resources can be used effectively and efficiently. Monitoring cancer incidence is an important part of this requirement and the classic approach has been through implementation of cancer registration.
Cancer registration can either be population or hospital based. Population based cancer registries (PBCR) are the gold standard for obtaining accurate cancer incidence in any given population but they are more resource intensive compared to hospital based registries. There are 62 PBCRs in Africa but only 5 produced data of sufficient quality to be included in the IARC publication of worldwide cancer incidence – Cancer in Five Continents (CIV) in 2007.(7) As of 2006, almost 80% of the world’s populations were not covered by PBCR and most of these live in low and middle income countries (LMIC).(8)
Efforts at sustainable PBCR in developing countries are stymied by inadequate funding, lack of personnel and a general lack of understanding of the need of PBCR. In contrast there is a large number of Hospital Based Cancer Registries (HBCR) in LMIC but literature describing their role and how best data obtained from them can be used is sparse. We posit that HBCR are fundamental sources of information in limited resource regions where population based cancer registries are lacking. Although HBCR are not useful to monitor the effects of cancer screening, they give an indication of the demand for cancer care services and other information that is useful for policy and planning. They are recognized in the literature as an integral part of hospital cancer control programs and have an indispensable role in a country’s health care delivery system.(9)
This paper provides information on HBCR in Nigeria, Africa’s most populous and diverse country. We analyze data from 11 HBCR that are part of the National Cancer Registry Program in Nigeria from 2009 to 2010 and describe the role of hospital cancer registries and how their data can be beneficial to improve health care systems in low and middle income countries in general.
Materials and Methods
Over the past 3 years, the Institute of Human Virology, Nigeria and the Nigerian Federal Ministry of Health have collaborated on training and streamlining the activities of cancer registries in Nigeria. During this period, 21 institutions have been trained and provided support for cancer registration. Of these 19 met the definition of HBCR (2 met the criteria for Population Based Cancer Registries) and we requested data on cancer cases recorded by these registries from January 2009 to December 2010. Most, 16 of the 19 registries (84%) responded.
No data was received from 3 cancer registries - University of Uyo Teaching Hospital, Uyo (UUTH), Federal Medical Centre, Lokoja and Federal Medical Centre, Keffi. No data on hospital facilities could be obtained from one hospital – Lagos State University Teaching Hospital, Ikeja (LASUTH).We excluded data from 5 institutions namely Lagos University Teaching Hospital, Suru-Lere (LUTH), Jos University Teaching Hospital, Jos (JUTH), Aminu Kano Teaching Hospital, Kano (AKTH), Federal Medical Centre, Gombe and University of Benin Teaching Hospital, Benin (UBTH)because of incomplete data (>50% missing entries for incidence date and age).
We analyzed data from 11 HBCR namely; University of Nigeria Teaching Hospital, Enugu (UNTH), University of Ilorin Teaching Hospital, Ilorin (UITH), University of Port Harcourt Teaching Hospital, Port Harcourt (UPTH), Federal Medical Centre,Ekiti (FMC IdoEkiti), University of Calabar Teaching Hospital, Calabar (UCTH), Obafemi Awolowo University Teaching Hospital, Ile-Ife, (OAUTH) Nnamdi Azikiwe University Teaching Hospital, Nnewi (NAUTH), Lagos State University Teaching Hospital, Ikeja(LASUTH), University of Abuja Teaching Hospital Gwagwalada(UATH), and the Ahmadu Bello University Teaching Hospital, Zaria (ABUTH).
All these registries used Canreg4 software for data entry and management and ICD-O 3 for classification and coding. CANREG4 software prevents the use of non-existent codes and performs checks forinternal consistency between variables. Data abstracted by the hospital cancer registries included information on name, age, morphology and topography of tumor, tribe, address, treatment, education level, marital status, religion and cause of death. We supplemented these data with information from unpublished work (reports and direct correspondence with the Federal Ministry of Health).
Analysis
We analyzed data on year hospital was established; year cancer registry was established, no of beds, no of pathologists and types of oncology services available in each tertiary health facility. We also analyzed relative frequency of cancers in each HBCR. We describe the basis of diagnosis recorded in the HBCR, the total number of cases recorded by gender and relative frequencies of the most common cancers seen. We attempted to estimate incidence rates using the population of the region covered by the HBCR and then using residential addresses to exclude cases referred from other regions. We also excluded cases with incomplete or inaccurate address entries, but after the exclusions the cases left were too few for any meaningful analysis.
Results
Most HBCR in Nigeria started functioning about 10 years with 6 of the 11 HBCR described in this study established in 2009, when the Nigerian National Cancer Registry program began. The average bed capacity of the hospitals where these HBCR are located is 469 beds per hospital. There were an average of 5 pathologists and 24 surgeons per hospital, excluding surgeons in training. The term, ‘surgeon’ as used in this communication is inclusive of all surgical subspecialties. All these hospitals offer chemotherapy services (Table 1).
Table 1.
Description of facilities at 11 hospitals with HBCR in Nigeria, 2011
| Hospital Cancer Registry |
Year Hospital was founded |
Year cancer registry began |
Hospital Capacity (No of Beds) |
No of Pathologists |
No of Surgeons |
Radiotherapy/unit | Chemotherapy /Surgery Services |
|---|---|---|---|---|---|---|---|
| NAUTH | 1990 | 2009 | 350 | 5 | 29 | No | Yes |
| UMTH | 1983 | 2003 | 400 | 4 | 20 | No | Yes |
| UCTH | 1979 | 1983 | 451 | 5 | 29 | No | Yes |
| FMC Ido-EKITI | 1998 | 2009 | 276 | 5 | 10 | No | Yes |
| UNTH | 1966 | 1988 | 500 | 5 | 29 | Yes (Not Functional) | Yes |
| UATH | 1993 | 2009 | 350 | 2 | 18 | No | Yes |
| ABUTH | 1967 | 1970 | 593 | 6 | 18 | Yes | Yes |
| UITH | 1980 | 1990 | 445 | 6 | 17 | No | Yes |
| LASUTH | - | 2009 | - | - | No | Yes | |
| OAUTH | 1975 | 1989 | 617 | 6 | 25 | No | Yes |
| UPTH | 1980 | 2009 | 700 | 7 | 40 | No | Yes |
The total number of cancers registered in these 11 hospital based cancer registries in 2009 and 2010 was 6 484 (Table 2 and Figure 1). Overall, more cases were recorded in women (3 903 – 60.2%) than in men (2 581 – 39.8%). Two hospitals, UNTH Enugu and ABUTH Zaria recorded the highest number of cases (Table 2). These were also the only hospitals out of the 11 that offer radiotherapy services. However, the radiotherapy service at UNTH was not functional at the time of writing this report. The number of new cancer cases recorded annually in these hospital based cancer registries on average were 106 cases in males and I64 cases in females (Table 2).The commonest basis for cancer diagnosis was histology of the primary tumor accounting for 70% while cytology accounted for 16.6% and clinical diagnosis was the basis in 9.5% of all cases (Table 3).
Table 2.
Number and proportion of cancer cases reported by 11 Nigerian hospital based cancer registries, 2009–2010
| Hospital Registry | Male | Female | Total |
|---|---|---|---|
| NAUTH | 197 (41.9%) | 273 (58.1%) | 470 |
| UMTH | 251 (45.6%) | 299 (54.4) | 550 |
| UCTH | 137 (37.6%) | 227 (62.4%) | 364 |
| FMC EKITI | 102 (28.7%) | 253 (71.3%) | 355 |
| UNTH | 660 (43.3%) | 865 (56.7%) | 1525 |
| UATH | 89 (37.8%) | 146 (62.2%) | 235 |
| ABUTH | 474 (40.5%) | 696 (59.5%) | 1170 |
| UITH | 187 (38.3%) | 301 (61.7%) | 488 |
| LASUTH | 93 (20.3%) | 365 (79.7%) | 458 |
| OAUTH | 262 (44.7%) | 325 (55.3%) | 587 |
| UPTH | 129 (45.7%) | 153 (54.3%) | 282 |
| Total | 2 581 (39.8%) | 3 903 (60.2%) | 6 484 |
Figure 1.
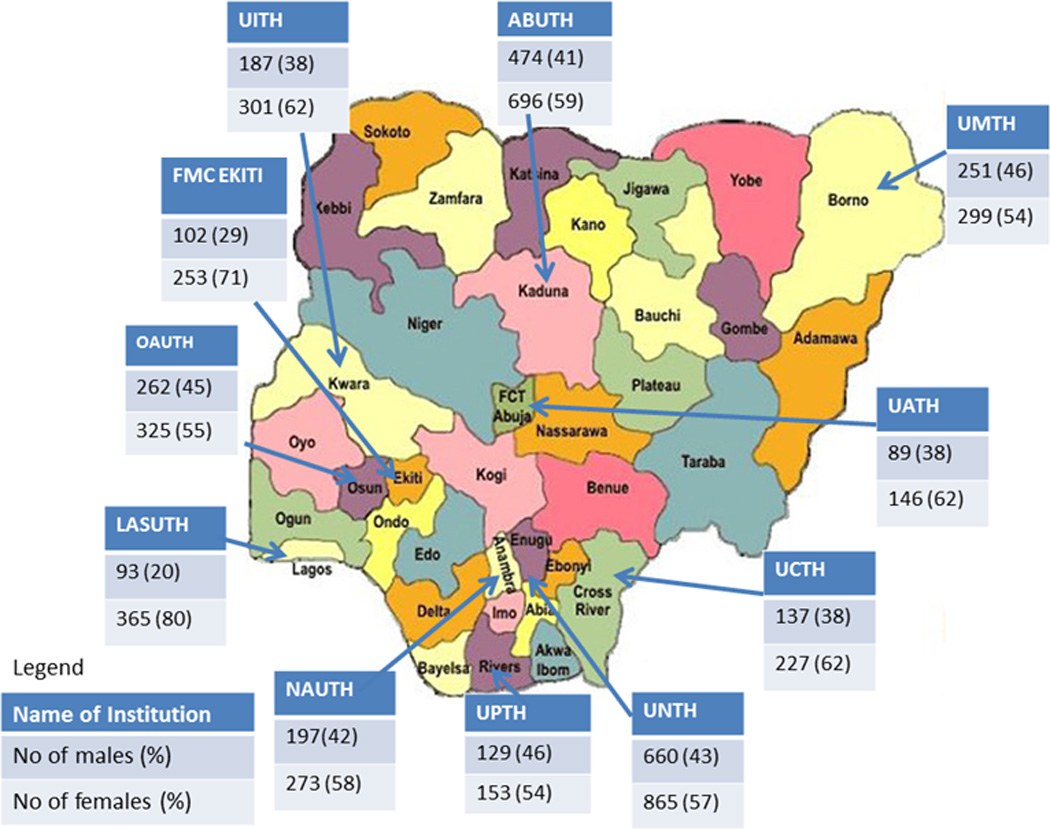
Map of Nigeria showing HBCR and total number of cases recorded by gender in each registry
Table 3.
The basis of diagnosis reported by 11 HBCR in Nigeria, 2009–2010
| Basis of diagnosis |
Clinical | Death Certificate |
Cytology | Histology of Metastases |
Histology of Primary |
Unknown | Total |
|---|---|---|---|---|---|---|---|
| HBCR | |||||||
| NAUTH | 296 | - | 1 | 1 | 172 | - | 470 |
| UMTH | - | 13 | - | - | 537 | - | 550 |
| UCTH | 12 | 8 | 55 | 10 | 279 | - | 364 |
| FMC EKITI | - | - | 107 | 3 | 244 | 1 | 355 |
| UNTH | 206 | 0 | 321 | 1 | 997 | - | 1525 |
| UATH | 4 | 1 | 104 | 26 | 100 | - | 235 |
| ABUTH | 2 | - | 164 | 25 | 979 | - | 1170 |
| UITH | 11 | - | 126 | 37 | 314 | - | 488 |
| LASUTH | 3 | 1 | 47 | 10 | 332 | 65 | 458 |
| OAUTH | - | - | - | - | 587 | - | 587 |
| UPTH | - | 6 | 39 | - | 237 | - | 282 |
| TOTAL | 534 (8.3%) | 29 (0.4%) | 964 (14.9%) | 113 (1.7%) | 4778 (73.7%) | 66 (1.0%) | 6484 (100%) |
We identified the 5 most common cancers registered by gender in the 2 year period under review. In males, cancer of the prostate (29.2%) was the most common cancer reported followed by colorectal cancer (7.0%), lymphomas (6.8%), liver cancer (4.0%) and skin cancer (3.8%) (Table 4).In women, breast cancer was by far the most common cancer constituting 40.3% of all cancers followed by cervical cancer (17.3%), cancer of the ovary (3.7%), lymphomas (3.1%) and skin cancer (2.1%) (Table 4).Overall, all other anatomical cancer sites excluding the 5 commonest cancers, accounted for 50% of all cancers in males and 33% in females.
Table 4.
The commonest five cancers in males and females reported by 11 HBCR in Nigeria, 2009–2010
| Males | Number | % | Females | Number | % |
|---|---|---|---|---|---|
| Prostate | 754 | 29.2 | Breast | 1446 | 40.0 |
| Colorectal | 181 | 7.0 | Cervix | 645 | 17.9 |
| Lymphomas | 177 | 6.8 | Ovary | 134 | 3.7 |
| Liver | 104 | 4.0 | Lymphomas | 110 | 3.1 |
| Skin Cancer* (Excluding Melanoma of the skin) | 98 | 3.8 | Skin Cancer* (Excluding Melanoma of the skin) | 83 | 2.1 |
Discussion
Our study showed that cancer registration is growing in Nigeria with many of the HBCR reported in this paper starting in the last few years. Over the 2 years covered by this report, about 6000 new cancer cases were reported by 11 hospital based cancer registries in Nigeria. The commonest cancer in women was breast cancer while prostate cancer was the commonest cancer in men. The hospitals commonly used histology of the primary tumor as basis of diagnosis but cytology and clinical diagnosis were also reported by some hospitals while registration by death certificate only, is negligible.(10) While HBCR data are prone to referral bias and cannot give a reliable measure of cancer incidence or provide information on cancer trends in a given population, they can provide data on the most frequent cancers managed in the hospitals that provide cancer care services.
Our finding of high prevalence of prostate cancer is consistent with studies from other parts of the world (11, 12) and with data from our population based cancer registry (manuscript in press). Colorectal cancer is the 2nd commonest cancer in males but the proportion is substantially less common compared to prostate cancer. The 3rd and 4th commonest cancers in men (lymphomas and liver cancer) were those associated with oncogenic virus infections.(13)
Breast cancer was the commonest female cancer recorded by these HBCR. This cancer is also the commonest incident cancer in Nigerian women as reported by population based cancer registries in Nigeria. (data not shown) Incidence of breast cancer in LMIC is expected to continue to rise with increasing life expectancy, changing obstetrics and gynecology practices, diet and physical activity.(14–16) It was responsible for almost half of all cancers reported in women and is the most common cancer reported in both sexes combined. The biggest challenge of breast cancer management in LMIC is low awareness and limited access to diagnosis and treatment(17). Given the high prevalence and high case fatality rates of breast cancer in LMIC, increased awareness, early detection and prevention should be priority control strategies for LMIC.(17)
Cancer of the cervix is the 2nd most common female cancer (18%) reported by these hospital based cancer registries. This is consistent with the GLOBOCAN 2008 data and data from our population based cancer registries (data not shown). [1] Cervical cancer prevention has been effective in developed countries (18, 19) but has been a challenge in LMIC. [16] [17] Recent efforts using “screen and treat”, leveraging resources for HIV/AIDS prevention and HPV diagnosis based screening methods may prove more successful.(20–24)
Skin cancer was the fifth most common cancer treated at these hospitals and it was more common in males (3.8%) than in females (2.1%). This was surprising since black populations have a low incidence of skin cancer. All cases recorded by the HBCR were basal cell and squamous cell carcinoma. This suggests that non-melanoma skin cancer (NMSC) may not be as rare as claimed in black populations. Similar findings were described in the early nineties in Uganda. [18] Albinism, a risk factor for NMSC in Africa may be a major contributing factor.(25, 26)
The 11 hospitals based cancer registries discussed in this paper are located in major tertiary health institutions that serve large populations and are referral sites for cancer management in Nigeria. Many of these hospitals lack radiotherapy services similar to the situation in many other LMIC.(27–29) Of the 54 Federal Health Institutions in Nigeria, only 3 (UCH Ibadan, National Hospital Abuja and ABUTH Zaria provide radiotherapy services and even in these hospitals, services are frequently episodic. All the hospitals reported availability of chemotherapy but none reported having medical oncology services or specialized chemotherapy units.
Taken together, cancers of the breast and cervix constitute about 60 % of all cancers presenting among Nigerian women treated in major tertiary health centers. Our population based cancer registry data also show that these 2 cancers were the commonest cancers affecting Nigerian women. (data not shown) Health care delivery models that incorporate prevention and care of these 2 cancers into women’s health care services are likely to contribute to significant reductions in cancer morbidity in Nigeria.
Apart from lymphomas in men, there was no evidence of the expected marked increase in AIDS associated cancers in this data.(30, 31) The prevalence of HIV/AIDS in Nigeria is 3.6% with an estimated 2 900 000 [95% CI 2 600 000– 3 200 000] persons living with HIV/AIDS.(32, 33) Of these, about 50% are receiving care and treatment.(33) It is therefore expected that a significant number of AIDS Associated cancers will be found in this population, although there is insufficient data on the actual incidence and prevalence.(6) This may be due to poor linkage of data and records between cancer and HIV programs, non-diagnosis of cancers in HIV patients and high fatality rate among the HIV+ populations with poorly controlled HIV infection.(6, 14) As health care services for this population improves, it becomes important to promote awareness of cancer and early diagnosis while strengthening the referral systems at the primary and secondary levels (34, 35).
While HBCR data are limited by inability to provide incidence data, they provide useful information that can guide resource allocation, cancer care policies and priorities, and investment in cancer prevention services. HBCR can be useful in describing patterns of referral and thus can define the catchment area of a given hospital. These data can be used to calculate the success of follow-up of cancer patients in a given hospital. In addition, HBCR data may be reflective of the nature and sophistication of services available within the health care system. Easily biopsied cancers like breast and skin maybe over-represented in HBCR data particularly where pathology is the commonest diagnostic tool used.
Despite these limitations, the findings of the most frequent cancers reported by HBCR in this study is similar to the findings from Nigerian population-based cancer registries and the most common cancers in Nigeria reported in GLOBOCAN 2008. [1]
Conclusion
Cancers are a new threat to the already overburdened health care system in many low and middle income countries.(28) Most LMIC have poor cancer surveillance systems and lack financial, human and infrastructural resources for effective cancer prevention, management and control.(36) Our study has important implications for cancer management in these settings. We propose the use of HBCR as sources of actionable cancer information and highlight their activities in a typical LMIC. Establishing and sustaining HBCR or PBCR in developing countries is difficult but need not be an either or proposition since both types of registries can provide useful information for cancer prevention and control. Nevertheless, upgrading hospital based cancer registries to population based registries in these regions should be paramount, despite the challenges.
Acknowledgements
This research was supported by the IHV-UM Capacity Development for Research into AIDS Associated Malignancies (NIH/NCI D43CA153792-01).
Special thanks are due to all the cancer registrars in the 11 hospital based cancer registries of the Nigerian National System of Cancer Registries for their data collection and reporting activities.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest Statement
The authors declare no conflict of interests.
Contributors
EJA and MPC analyzed and interpreted the data and wrote the first draft and subsequent revisions. CAA contributed to the methodological approach, revised several versions of the draft, obtained funding and guided all aspects of this report. All other authors contributed equally to this study by providing feedback and contributing to the final draft.
References
- 1.Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893–2917. doi: 10.1002/ijc.25516. [DOI] [PubMed] [Google Scholar]
- 2.Sylla BS, Wild CP. A million africans a year dying from cancer by 2030: What can cancer research and control offer to the continent? Int J Cancer. 2011 doi: 10.1002/ijc.26333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mamotte N, Wassenaar D, Koen J, Essack Z. Convergent ethical issues in HIV/AIDS, tuberculosis and malaria vaccine trials in Africa: Report from the WHO/UNAIDS African AIDS Vaccine Programme's Ethics, Law and Human Rights Collaborating Centre consultation, 10–11 February 2009, Durban, South Africa. BMC Med Ethics. 2010;11:3. doi: 10.1186/1472-6939-11-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McCarthy M, Maher D, Ly A, Ndip A. Developing the agenda for European Union collaboration on non-communicable diseases research in Sub-Saharan Africa. Health Res Policy Syst. 2010;8:13. doi: 10.1186/1478-4505-8-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Holmes MD, Dalal S, Volmink J, Adebamowo CA, Njelekela M, Fawzi WW, Willett WC, Adami HO. Non-communicable diseases in sub-Saharan Africa: the case for cohort studies. PLoS Med. 2010;7:e1000244. doi: 10.1371/journal.pmed.1000244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mbulaiteye SM, Bhatia K, Adebamowo C, Sasco AJ. HIV and cancer in Africa: mutual collaboration between HIV and cancer programs may provide timely research and public health data. Infect Agent Cancer. 2011;6:16. doi: 10.1186/1750-9378-6-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Curado MP, B. Edwards HRS, Storm H, Ferlay J, Heanue M, Boyle P, editors. [accessed 18th October 2011];Cancer Incidence in Five Continents Vol. IX IARC Scientific Publications No. 160. 2008 http://www.iarc.fr/en/publications/pdfs-online/epi/sp160/CI5vol9-A.pdf.
- 8.Cancer registries. 2011. Boston: Global Task Force on Expanded Access to Cancer Care and Control in Developing Countries; 2011. Global Task Force on Expanded Access to Cancer Care and Control in Developing Countries. [Google Scholar]
- 9.Young JL. The hospital-based cancer registry. IARC Sci Publ. 1991:177–184. [PubMed] [Google Scholar]
- 10.Oluwasola OA, Fawole OI, Otegbayo AJ, Ogun GO, Adebamowo CA, Bamigboye AE. The autopsy: knowledge, attitude, and perceptions of doctors and relatives of the deceased. Arch Pathol Lab Med. 2009;133:78–82. doi: 10.5858/133.1.78. [DOI] [PubMed] [Google Scholar]
- 11.Hsing AW, Devesa SS. Trends and patterns of prostate cancer: what do they suggest? Epidemiol Rev. 2001;23:3–13. doi: 10.1093/oxfordjournals.epirev.a000792. [DOI] [PubMed] [Google Scholar]
- 12.Hsing AW, Tsao L, Devesa SS. International trends and patterns of prostate cancer incidence and mortality. Int J Cancer. 2000;85:60–67. doi: 10.1002/(sici)1097-0215(20000101)85:1<60::aid-ijc11>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 13.Sitas F, Parkin DM, Chirenje M, Stein L, Abratt R, Wabinga H. Part II: Cancer in Indigenous Africans--causes and control. Lancet Oncol. 2008;9:786–795. doi: 10.1016/S1470-2045(08)70198-0. [DOI] [PubMed] [Google Scholar]
- 14.Adebamowo C, Akarolo-Anthony S. Cancer in Africa: Opportunities for collaborative research and training. Afr J Med Med Sci. 2009;38(Suppl):5–13. [PubMed] [Google Scholar]
- 15.Adebamowo CA, Ajayi OO. Breast cancer in Nigeria. West Afr J Med. 2000;19:179–191. [PubMed] [Google Scholar]
- 16.Akarolo-Anthony SN, Ogundiran TO, Adebamowo CA. Emerging breast cancer epidemic: evidence from Africa. Breast Cancer Res. 2010;12(Suppl 4):S8. doi: 10.1186/bcr2737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Anderson BO, Cazap E, El Saghir NS, Yip CH, Khaled HM, Otero IV, Adebamowo CA, Badwe RA, Harford JB. Optimisation of breast cancer management in low-resource and middle-resource countries: executive summary of the Breast Health Global Initiative consensus, 2010. Lancet Oncol. 2011;12:387–398. doi: 10.1016/S1470-2045(11)70031-6. [DOI] [PubMed] [Google Scholar]
- 18.Canavan TP, Doshi NR. Cervical cancer. Am Fam Physician. 2000;61:1369–1376. [PubMed] [Google Scholar]
- 19.Armstrong EP. Prophylaxis of cervical cancer and related cervical disease: a review of the cost-effectiveness of vaccination against oncogenic HPV types. J Manag Care Pharm. 2010;16:217–230. doi: 10.18553/jmcp.2010.16.3.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mwanahamuntu MH, Sahasrabuddhe VV, Kapambwe S, Pfaendler KS, Chibwesha C, Mkumba G, Mudenda V, Hicks ML, Vermund SH, Stringer JS, Parham GP. Advancing cervical cancer prevention initiatives in resource-constrained settings: insights from the Cervical Cancer Prevention Program in Zambia. PLoS Medicine. 2011;8:e1001032. doi: 10.1371/journal.pmed.1001032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mwanahamuntu MH, Sahasrabuddhe VV, Stringer JSA, Parham P. Integrating cervical cancer prevention in HIV/AIDS treatment and care programmes. Bulletin of the WHO. 2008;86:D–E. doi: 10.2471/BLT.08.056275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sankaranarayanan R, Boffetta P. Research on cancer prevention, detection and management in low- and medium-income countries. Ann Oncol. 2010;21:1935–1943. doi: 10.1093/annonc/mdq049. [DOI] [PubMed] [Google Scholar]
- 23.Sankaranarayanan R, Nene BM, Shastri SS, Jayant K, Muwonge R, Budukh AM, Hingmire S, Malvi SG, Thorat R, Kothari A, Chinoy R, Kelkar R, Kane S, Desai S, Keskar VR, Rajeshwarkar R, Panse N, Dinshaw KA. HPV Screening for Cervical Cancer in Rural India. New Engl J. Med. 2009;360:1385–1394. doi: 10.1056/NEJMoa0808516. [DOI] [PubMed] [Google Scholar]
- 24.Sankaranarayanan R, Nessa A, Esmy PO, Dangou J-M. Visual inspection methods for cervical cancer prevention. Best Practice & Research Clinical Obstetrics & Gynaecology. 2012;26:221–232. doi: 10.1016/j.bpobgyn.2011.08.003. [DOI] [PubMed] [Google Scholar]
- 25.Cruz-Inigo AE, Ladizinski B, Sethi A. Albinism in Africa: stigma, slaughter and awareness campaigns. Dermatol Clin. 2011;29:79–87. doi: 10.1016/j.det.2010.08.015. [DOI] [PubMed] [Google Scholar]
- 26.Hong ES, Zeeb H, Repacholi MH. Albinism in Africa as a public health issue. BMC Public Health. 2006;6:212. doi: 10.1186/1471-2458-6-212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Murthy NS, Chaudhry K, Rath GK. Burden of cancer and projections for 2016, Indian scenario: gaps in the availability of radiotherapy treatment facilities. Asian Pac J Cancer Prev. 2008;9:671–677. [PubMed] [Google Scholar]
- 28.Boyle P, Levin B. World Cancer Report. Geneva: International Agency for Research on Cancer; 2008. [Google Scholar]
- 29.IAEA. A silent crisis: Cancer Treatment in Developing Countries. Vienna, Austria: IAEA; 2003. [Google Scholar]
- 30.Mbulaiteye SM, Bhatia K, Adebamowo C, Sasco AJ. HIV and cancer in Africa: mutual collaboration between HIV and cancer programs may provide timely research and public health data. Infectious agents and cancer. 2011;6:16. doi: 10.1186/1750-9378-6-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Akinwande O, Ogundiran T, Akarolo-Anthony S, Mamadu I, Dakum P, Blattner W, Adebamowo C. Challenges in treating malignancies in HIV in Nigeria. Curr Opin Oncol. 2009;21:455–461. doi: 10.1097/CCO.0b013e32832e6385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. [accessed april 17th 2012];USAID HIV/AIDS Health Profile:Nigeria. 2007 http://www.usaid.gov/our_work/global_health/aids/Countries/africa/nigeria.pdf.
- 33. [accessed online 17th April 2012];UNAIDS Report on the Global AIDS Epidemic. 2010 http://www.unaids.org/globalreport/Global_report.htm.
- 34.McConigley R, Platt V, Holloway K, Smith J. Developing a sustainable model of rural cancer care: The Western Australian Cancer Network project. Aust J Rural Health. 2011;19:324–328. doi: 10.1111/j.1440-1584.2011.01236.x. [DOI] [PubMed] [Google Scholar]
- 35.Sankaranarayanan R. Cancer survival in Africa, Asia, the Caribbean and Central America. Introduction. IARC Sci Publ. 2011:1–5. [PubMed] [Google Scholar]
- 36.Gondos A, Brenner H, Wabinga H, Parkin DM. Cancer survival in Kampala, Uganda. Br J Cancer. 2005;92:1808–1812. doi: 10.1038/sj.bjc.6602540. [DOI] [PMC free article] [PubMed] [Google Scholar]


