Abstract
Background
Although expenditures on health care are continually increasing and often said to be unsustainable, few studies have examined these trends at the level of services delivered to individual patients. We analyzed trends in the various components that contributed to changes in overall expenditures for physician services in British Columbia from 1985/86 to 1996/97.
Methods
We obtained data on all fee-for-service payments to physicians in each study year using the British Columbia Linked Health Data set and analyzed these at the level of individual patients. We disaggregated overall billing levels by year into the following components: number of physicians seen by each patient, number of visits per physician, number of services rendered on each visit and average price of those services. We removed the effect of inflation on fees by adjusting to those in 1988. We used direct age-standardization to isolate and measure the effect of demographic changes. We used the Consumer Price Index to determine the effects of inflation.
Results
Total payments to fee-for-service physicians in British Columbia rose 86.3% over the study period. The increase was entirely accounted for by the combined effects of population growth (28.9%), aging (2.1%) and general inflation (41.4%). Service use per capita rose 10.5%; this increase was offset by a decline of 9.4% in inflation-adjusted fees. The average cost of age-adjusted per-capita services rendered by general or family practitioners (GP/FPs) increased very little (3.3%) over the 11-year period, compared with a nearly one-third (31.8%) increase for medical specialists. Although there was a dramatic increase in the number of GP/FPs seen on average by each patient (32.9%), this increase was offset by the combination of decreases in the number of visits per physician (–14.9%), the number of services provided per visit (–8.0%) and the “real cost” of each service provided (–3.5%). Visits to medical specialists increased by about 20% over the study period in all age groups. However, for each person 65 years of age or over receiving any services, the average fee-adjusted expenditures increased 24.8%, almost 4 times the rate of increase for people younger than 65. The use of surgical services grew 26.5% for seniors while declining –2.0% for people under age 65.
Interpretation
These findings suggest a form of “homeostasis” in aggregate-level service use and cost. The supposed inflationary effects of population aging and increasing “abuse of the system” by patients were not found.
The conventional wisdom, said John Kenneth Galbraith, is always wrong.1 For decades, conventional wisdom, as presented in the national media, has held that health care costs are spiralling out of control because of an aging population and rising public expectations. The latest rhetoric is that the Canadian health care system is unsustainable. The objective of our study was to examine evidence from recent physician-service use in British Columbia to ascertain whether there is more than just rhetoric behind the claims.
A number of previous studies exploring trends in expenditure on the various components of health care demonstrated the limited effect of demographic change.2,3,4,5 Our study has reinforced those findings but extended the earlier work in 2 ways. First, the British Columbia Linked Health Data (BCLHD) set6 enabled the use of data for the individual, nonidentifiable patient rather than patient groups (e.g., age-specific) as our fundamental unit of analysis, which made it possible to do a more detailed exploration of the components underlying changes in aggregate expenditures. Second, our analysis covered a particularly turbulent period (1985/86 through 1996/97) for health care financing in British Columbia. A number of policies were introduced in the province in an attempt to contain the growth of medical care costs.7,8 These might have been expected to be reflected in changes in the mix and numbers of patients seeing physicians and the types of services received. We disaggregated trends in overall expenditures into components representing changes in fee levels, practice patterns and activity levels.
Methods
All fee-for-service payments to physicians in 1985/86 and 1996/97 are contained in the Payment Information Masterfile of the Medical Services Plan in British Columbia, a core file of the British Columbia Linked Health Data. In both years of the study, fee-for-service payments accounted for more than 90% of all payments to physicians in the province, and the linkage rate (the percentage of Medical Service Plan payment records that could be associated with a BC resident eligible for health benefits) was greater than 99%.6
The payments recorded in the working data set totalled approximately $780 million in 1985/86 and $1.45 billion in 1996/97. We removed the effects of fee changes over this period by valuing fee items in both years at the fee level in effect Apr. 1, 1988. (Details are described elsewhere.7) This yielded an aggregate measure of physicians' service output in which the individual services were weighted by their relative fees at a single point in time. This permitted a comparison of expenditures after removing the effects of changes in fees. We refer to this measure subsequently as “fee-adjusted expenditures.” Change in the real value of fees was calculated by adjusting growth attributable to increases in fees by the BC Consumer Price Index.9
To isolate the effects of population aging, we multiplied the 5-year age-specific rates of per-capita use in 1985/86 by the proportion of the provincial population in each age category in each year and summed these values for each year (direct standardization). The change in this total represents the effects of aging on fee-adjusted expenditures.
Patients' use of physician services may be described in ways that reveal considerably more about patterns of use than summary statistics such as expenditures or use per capita. Specifically, for each person who contacts at least 1 physician during the period, it may be of interest to know how many physicians were seen and, for each such physician, how many times the patient was seen, as well as the service patterns per visit. This disaggregation is shown in the following equation.
Fee-adjusted expenditure = #MDs х contacts/#MDs х services/contact х fee-adjusted expenditure/service
In this equation “#MDs” is the number of physicians providing services to a given patient, and “contacts” refers to any interactions between a patient and a physician associated with 1 or more billable “services.” “Fee-adjusted expenditure/service” measures the average (constant-dollar) fee per service provided to that patient; compared over time, this measure indicates whether the mix of services provided is becoming more or less expensive. Changes in fee-adjusted expenditure for a given patient will be the product of changes in each of these 4 components.
Aggregating this equation across all individual patients in the province, and accounting for the fact that not all residents will see a physician in a given period, yields the following identity, which expresses the range of factors whose changes collectively determine changes in per-capita (fee-adjusted) expenditure.
Adjusted expenditure/population = patients/population х MDPPs/patient х contacts/MDPP х services/contact х fee-adjusted expenditure/service
In this equation, patients are individuals who see at least 1 physician during the year in question. Population figures are from the PEOPLE projection model prepared by BC Stats,10 with adjustment for mortality. Henceforth we refer to “patients/population” as an exposure rate: the proportion of a population that is “exposed” to physician services. “MDPP” refers to the total number of unique physician–patient combinations (“MD–patient pairs”).
Because we were interested in variation in each of these terms both over time and across types of physician service, we disaggregated MDPPs into 4 categories: general and family practitioners (GP/FPs), medical specialists (dermatologists, neurologists, psychiatrists, neuropsychiatrists, pediatricians, pediatric cardiologists, and specialists in internal medicine, physical medicine, emergency medicine or osteopathy), surgical specialists (obstetrician/gynecologists, ophthalmologists, otolaryngologists, general surgeons, neurosurgeons, orthopedic surgeons, plastic surgeons, thoracic and cardiovascular surgeons, urologists and anesthesiologists), and diagnostic specialists (radiologists, pathologists, medical microbiologists and nuclear medicine specialists). Each physician was assigned to one of these categories in each of the 2 study years on the basis of the predominant concentration of billings, not college certification.
Results
Fee-for-service payments for physician services in British Columbia grew 86.3% from 1985/86 to 1996/97, fee increases accounting for 28.1% and growth in fee-adjusted expenditures for 45.4% (Table 1). Population growth (28.9%) and population aging (2.1%) accounted for 70% of the increase in use. Use per (age-adjusted) capita grew only 10.5%, or 0.9% per annum. This increase, however, was almost precisely offset by the 9.4% decline in the real value of fees (relative to the BC Consumer Price Index). Remarkably, the combined effects of population growth, aging and general inflation (86.1%) were virtually identical to the overall increase in physician expenditures.
Table 1

The impact of changes in the age structure of the BC population over this period was a barely detectable 0.2% per year, even smaller than the 0.4% found in previous studies.3 Most of the growth in average per-capita use of services came through changes in age-specific rates of use (Fig. 1), changes that are characteristic of the relation between age and use of physician services.2,5 Increasing rates of use are found primarily among seniors. For example, per-capita use did not change for those in the age range 1–30 years; in contrast, a 77-year-old person would have used, on average, about 25% more services during 1996/97 than her 77-year-old counterpart did during 1985/86.
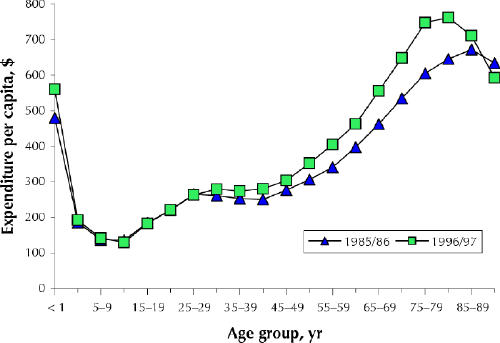
Fig. 1: Physician-service expenditures per capita in British Columbia by age group, 1985/86 and 1996/97. [Source: Payment Information Masterfile of the provincial Medical Services Plan.]
But a more comprehensive understanding of the underlying service dynamics requires the detailed disaggregation provided in the second equation. The results are presented in Table 2. Perhaps the most striking feature is the difference in the patterns of change across the categories of physician.
Table 2
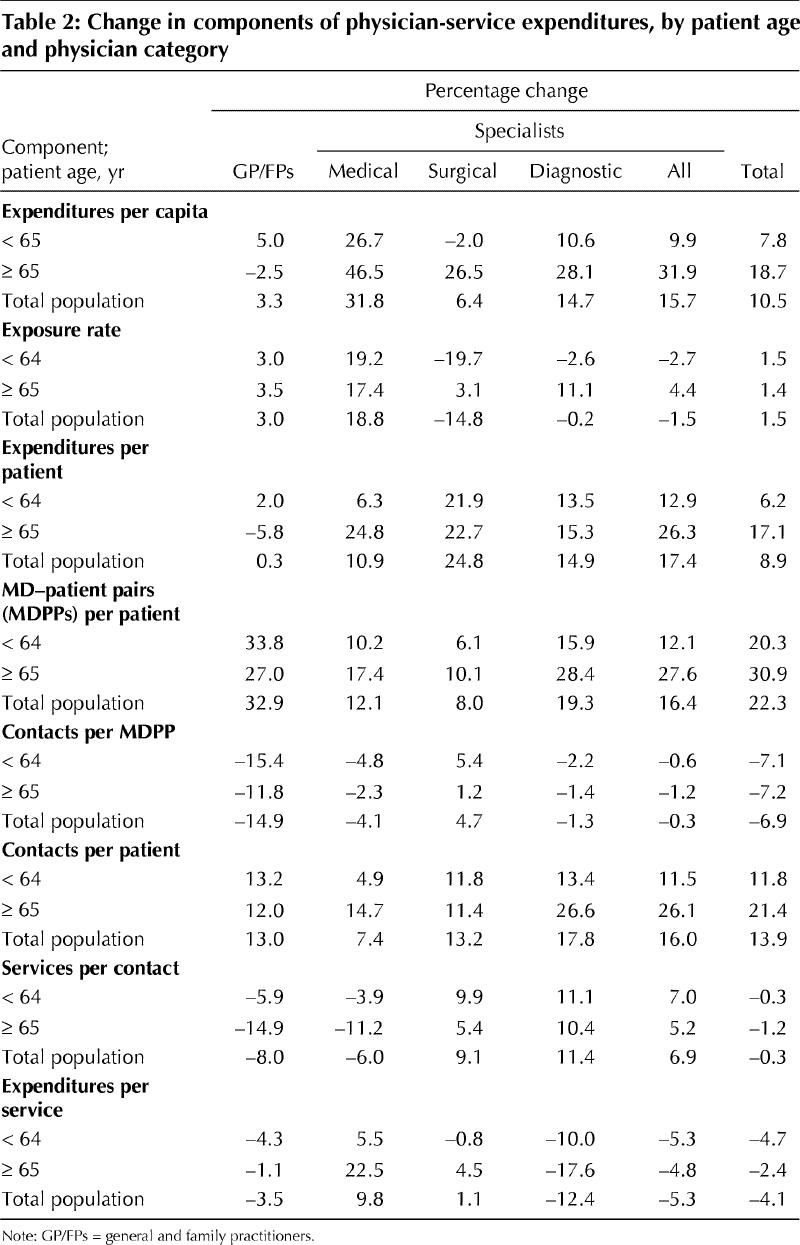
Per-capita use of GP/FP services rose very little overall (3.3%) and actually fell for seniors. The striking increase in the number of GP/FPs seen by each patient (about one-third) was offset by reductions in the number of contacts with each physician seen, the number of services provided in each contact and the “real price” of the average service.
For medical specialists, however, the per-capita (age-adjusted) use of services increased rapidly, up 31.8% over the 11 years, and the increase was nearly twice as great for seniors as for the rest of the population. The proportion of the population contacting a medical specialist (the exposure rate) rose by nearly 20%, for seniors and nonseniors alike. But for each senior receiving any services, the average fee-adjusted expenditure per service increased by one-quarter, about 4 times the rate of increase for nonseniors. Although each senior saw, on average, 14.7% more medical specialists, this increase was largely offset by reductions in the number of contacts per specialist seen and in the number of services per contact.
The most striking trend in surgical services over the period studied was the remarkable contrast between the large increase in fee-adjusted expenditures per capita for seniors and the small decline for nonseniors. Expenditures per patient increased by similar amounts, more than 20%, in both age groups, the result of increases in the number of contacts per patient and services per contact. However, the proportion of the population seeing at least 1 surgical specialist fell by almost 20% among nonseniors, while increasing slightly among seniors.
The key feature for the diagnostic specialists is, again, to be found among the seniors, although there were also nontrivial increases for the rest of the population. The proportion of seniors receiving any diagnostic services increased about 11%, and the fee-adjusted expenditure for each senior patient increased more than 15%. The latter increase was the product of a 26.6% increase in the number of “contacts” per patient (discrete occurrences of patients, or their tissue or fluid samples, going to diagnostic facilities for testing) and a decline in the average cost of the diagnostic services provided during each such occurrence.
Interpretation
The data used in our analyses precluded any attempt to ascertain changes in the quality of care provided by physicians in British Columbia over the period analyzed or in the health impact of the services provided. Because of limitations in the content of the administrative data collected for the purpose of reimbursing physicians, we were also not able to examine changes in the length or detailed clinical content (including “costliness”) of contacts with patients. And our decision to examine changes in patterns of use for 4 broad categories of physician may mask different trends for particular specialties.
The most prominent feature of the physician-services landscape in British Columbia over this period is what did not happen. Costs did not spiral out of control, the aging population did not create unsustainable pressures on the sector, and the growth in physician supply did not fall behind the age-adjusted population growth. Although total expenditures nearly doubled (rising 86.3%), the explanation is simple. Population growth, routinely built into budgets, accounted for over half the increase; the rest of the increase just matched the general rate of inflation. Use of services did rise modestly: 12.8%, or 1.1% per year on average. But this was almost exactly offset by the decline in the real value of fees. Population aging accounted for only about 0.2% of the growth in expenditures per year, or 2.1% over the 11 years.
Beneath this calm surface, however, there were significant changes in both the distribution of total physician workload and the processes of care provision. Services provided by specialists took on increasing importance as a proportion of all physician services, despite the fact that the number of physicians in the 2 groups increased at almost the same rate.
Over the period studied, GP/FPs appeared to focus increasingly on less time-consuming (younger) patients, referring more complex (older) patients for specialty attention after initial contact. Patients in general saw more different GP/FPs in 1996/97 than in 1985/86, seeing each GP/FP fewer times and for less expensive services. Whether these changes have affected continuity or quality of care seems an important question, worthy of examination.
Per-capita costs for medical specialists rose by nearly one-third for the entire population and by nearly 50% (after adjustment for fee increases and aging) for seniors. Many more people in both age groups were referred to specialists in 1996/97 than in 1985/86, and those who were referred saw more specialists. But seniors were also receiving a more costly basket of medical-specialist services. Seniors' per-capita use of surgical services also increased substantially, whereas the proportion of nonseniors seeing a surgical specialist fell about 20%. If there is concern about cost escalation within the physician-services sector, services provided by medical and surgical specialists to seniors would be good starting points for future examination.
Taken together, these findings definitively reject the common contention that costs are escalating because patients are increasingly “abusing the system,” running to physicians with frivolous demands. First, overall costs rose in line with population growth and general inflation. Second, per-capita use of GP/FPs grew almost not at all. If such abuse were rampant, surely this is where it would show up. The rapid increases in use were found among specialty services, to which access is by referral. The pattern of subsequent care is under professional control.
Acknowledgments
Funding for this work was provided by grant 6610-2117-602 from the National Health Research and Development Program and through the British Columbia Ministry of Health. Access to data was granted by the ministry through the BC Linked Health Data set, maintained at the Centre for Health Services and Policy Research at the University of British Columbia.
Footnotes
This article has been peer reviewed.
Contributors: Morris Barer and Robert Evans contributed substantially to the conception and design of the study and the interpretation of data; they also drafted the article. Kimberlyn McGrail was responsible for acquisition of data, assisted with interpretation of data and contributed to the writing of the article. Bo Green was responsible for data analysis and contributed to the interpretation of data. Clyde Hertzman and Samuel Sheps contributed to the conception and design of the study. All authors revised the article critically for important intellectual content and approved the version to be published.
Competing interests: None declared.
Correspondence to: Ms. Kimberlyn M. McGrail, Centre for Health Services and Policy Research, University of British Columbia, 2194 Health Sciences Mall, Vancouver BC V6T 1Z3; fax 604 822-5690; kmcgrail@chspr.ubc.ca
References
- 1.Galbraith JK. The affluent society. Boston: Houghton-Mifflin; 1958.
- 2.Barer ML, Pulcins IR, Evans RG, Hertzman C, Lomas J, Anderson GM. Trends in use of medical services by the elderly in British Columbia. CMAJ 1989; 141(1):39-45. [PMC free article] [PubMed]
- 3.Barer ML, Evans RG, Hertzman C. Avalanche or glacier? Health care and the demographic rhetoric. Can J Aging 1995;14:193-224.
- 4.Demers M. Factors explaining the increase in cost for physician care in Quebec's elderly population. CMAJ 1996;155(11):1555-60. [PMC free article] [PubMed]
- 5.Evans RG, McGrail KM, Morgan SG, Barer ML, Hertzman C. Apocalypse no: population aging and the future of health care systems. Can J Aging 2001; 20 (Suppl 1):160-91.
- 6.Chamberlayne R, Green B, Barer ML, Hertzman C, Lawrence WJ, Sheps SB. Creating a population-based linked health database: a new resource for health services research. Can J Public Health 1998;89:270-3. [DOI] [PMC free article] [PubMed]
- 7.Pascali MV. Controlling expenditures for physicians' services: an evaluation of British Columbia's cost containment policies, 1979–1991 [dissertation]. Berkeley (CA): University of California; 1995.
- 8.Barer ML, Lomas J, Sanmartin C. Re-minding our Ps and Qs: medical cost controls in Canada. Health Aff (Millwood) 1996;15:216-34. [DOI] [PubMed]
- 9.CANSIM. Consumer price indexes for British Columbia [annual]. Series P810000. Ottawa: CANSIM, Statistics Canada.
- 10.Population statistics — total and age/sex estimates. Victoria (BC): BC Stats; 2003. Available: www.bcstats.gov.bc.ca/data/pop/pop/estspop.htm (accessed 2003 Oct 29).


