Abstract
ASYMPTOMATIC ELEVATION OF THE INTERNATIONAL normalized ratio (INR) is a common problem associated with hemorrhage. Evidence from randomized controlled trials supports the use of low-dose oral vitamin K therapy as a treatment that promptly reduces the INR. Vitamin K given orally is more effective than subcutaneous vitamin K injection, and as effective as intravenous administration when INR values are compared 24 hours after administration. A 1.0-mg vitamin K dose is likely most appropriate for patients with INR values between 4.5 and 10. The fear of over-correction of the INR has limited the widespread use of vitamin K; however, our review suggests that this occurs infrequently when small doses are administered orally.
Asymptomatic elevation of the international normalized ratio (INR) is a common and important clinical problem encountered by all health care professionals who supervise patients taking warfarin. Patients in typical outpatient practices have INRs outside the desired range 50% of the time.1,2 One randomized controlled trial (RCT) suggested that, despite measures to ensure an appropriate level of anticoagulation, 14% of total patient-time was spent with INR values above the therapeutic range.3 There is a strong relation between the degree of INR elevation and the risk of hemorrhage. Serious warfarin-associated bleeding usually occurs from the gastrointestinal or genitourinary system;4 the risk of such bleeding may as much as double for each 1-point increase in the INR.5 Investigators of a prospective cohort study6 followed 114 consecutive patients who presented to an anticoagulation clinic with an INR greater than 6 and found that abnormal bleeding developed in 10 (8.8%) of them and life-threatening hemorrhage in 5 (4.4%; 2 fatal) over the 2-week follow-up period. Therefore, interventions leading to a prompt reduction of the INR may reduce the risk of serious bleeding in patients taking warfarin.
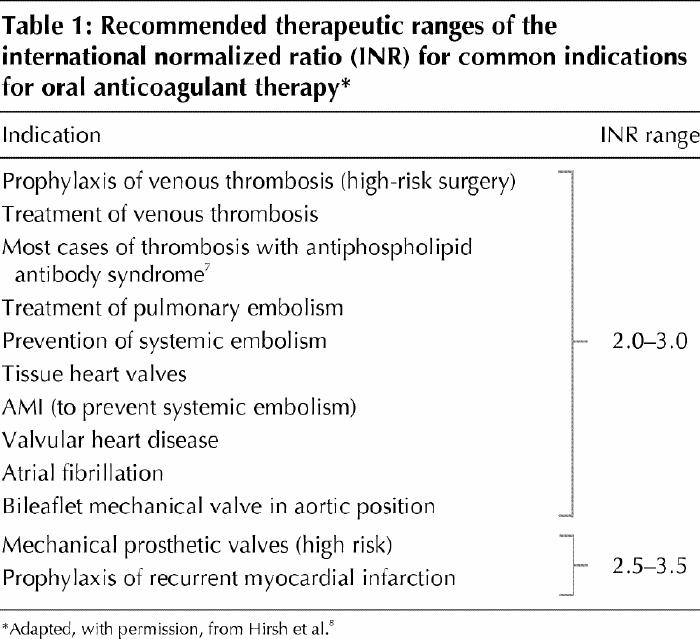
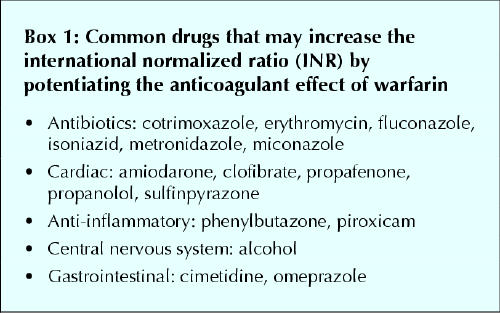
Most indications for warfarin anticoagulation have a target therapeutic INR range of 2.0 to 3.0. However, some indications, such as mechanical heart valves, require a higher intensity of anticoagulation. Table 1 lists the therapeutic INR ranges for common indications for warfarin anticoagulation.7,8 An elevated INR is one that is above the therapeutic range. However, most studies that have evaluated interventions for asymptomatic elevation of the INR have examined INRs several points above the upper limit of the therapeutic range, usually selecting a lower limit for intervention between 4.5 and 6.0. In assessing patients with an elevated INR, one should consider potential causes such as noncompliance, inappropriate dosing, fluctuations in vitamin K intake, hepatic dysfunction, laboratory errors, drug interactions (Box 1) and alcohol intake.
Table 1
Box 1.
A common strategy for lowering an elevated INR is simply to withhold warfarin. In some cases parenteral vitamin K therapy may be administered. Recent interest has focused on the use of vitamin K orally as a simple, safe and effective way of normalizing an excessively elevated INR. Although no tablet form of vitamin K is currently available in Canada, the intravenous formulation (see Fig. 1) can be given orally, either undiluted or after mixing with orange juice to mask its unpleasant taste. We reviewed the literature to ascertain whether or not oral vitamin K therapy is effective, to identify the degree of INR abnormality that is best managed with oral therapy, to identify the dose that is most appropriate and to identify the relative risks of hemorrhage and thrombosis with this regimen as compared with other management approaches.

Fig. 1: Ampule of vitamin K. Because the tablet form of vitamin K is not currently available in Canada, the parenteral formulation can be given orally. It is dispensed in ampules of 0.5 mL (equivalent to 1.0 mg) and 1.0 mL (equivalent to 10.0 mg). The cost of treatment with 1.0 mg of parenteral vitamin K is as low as 10 cents when dispensed from an ampule of 10.0 mg/mL. Patient self-management may be a promising avenue for the use of oral vitamin K therapy in anticoagulation control.
Literature review
The MEDLINE database was searched for articles published between 1966 and Jan. 1, 2004, using the following terms: “vitamin K” or “phytonadione,” “oral” and “anticoagulation.” The search, limited to human studies published in English, identified 118 articles. We included studies if the patients had INRs above the therapeutic range due to warfarin; low-dose oral vitamin K therapy (1.0–2.5 mg) was used in addition to the suspension of warfarin therapy; the INR method was used to standardize prothrombin time results; the change in the INR was reported 24 hours after vitamin K administration; and the study design was prospective. We found 17 studies of the use of oral vitamin K therapy to reverse excessive anticoagulation that met these criteria. A manual search of the bibliographies of the retrieved articles identified 4 additional studies. Of these 21 studies, 13 were excluded for the following reasons: inclusion of patients with therapeutic INR values,9 warfarin therapy not suspended,9,10 vitamin K use in doses greater than 2.5 mg,11 use of anticoagulants other than warfarin,12,13,14 published before the development of the INR system,15 no INR measurement 24 hours following treatment16 and lack of prospective data collection.17,18,19,20 One review paper21 was also excluded because it lacked original data. Eight studies,22,23,24,25,26,27,28,29 with a total of 344 patients, met all of the inclusion criteria and were included in this review (Tables 2 and 3). We used these articles to answer 4 questions, which are addressed below.
Table 2
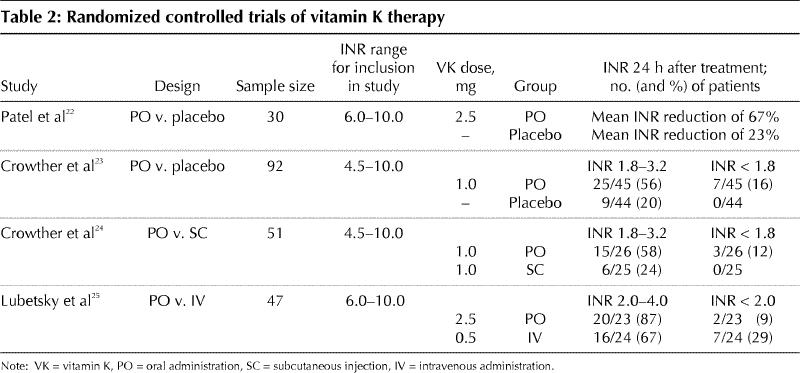
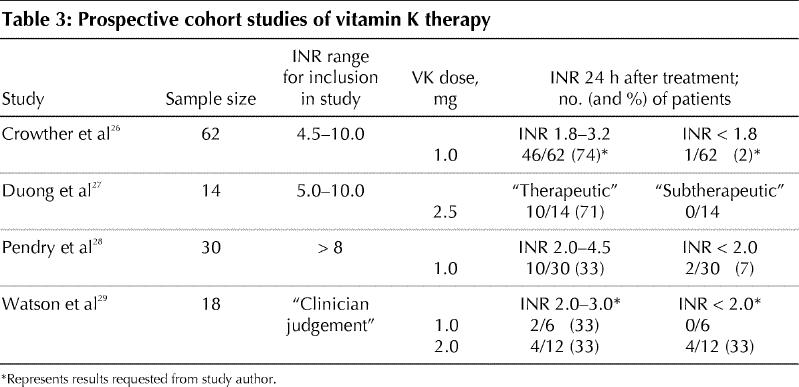
Table 3
Is oral vitamin K therapy effective compared with other management approaches?
Four RCTs compared oral vitamin K therapy with placebo or with other methods of vitamin K administration (Table 2).22,23,24,25 Two double-blind, placebo-controlled RCTs demonstrated that oral vitamin K therapy reduces the INR more promptly than does the withholding of warfarin alone.22,23 Despite the evidence that oral vitamin K therapy is effective, chart reviews and physician surveys have shown that physicians prefer to administer vitamin K subcutaneously.30,31,32 This preference exists despite evidence from randomized trials that the subcutaneous route is less effective than either the oral24 or intravenous route.33,34 The only RCT comparing oral and subcutaneous vitamin K administration showed that patients who received vitamin K orally were significantly more likely than those treated by subcutaneous injection to have a therapeutic INR on the day following treatment (p = 0.015).24 The evidence supporting oral administration of vitamin K was further strengthened by a recent RCT that demonstrated an equivalent ability of oral and intravenous vitamin K therapies to return a prolonged INR to the therapeutic range at 24 hours.25 The intravenous route resulted in an immediate effect, as compared with a lag time of 4 hours with the oral route.25 Despite this, the intravenous route is not the preferred route of administration because its use is associated with a low but finite risk of anaphylactoid reactions.35
What range of INRs should be managed with oral vitamin K therapy?
The INR values at which vitamin K was administered orally varied between the studies we reviewed. However, studies that restricted enrolment to patients with INRs below 10 tended to have a greater proportion of patients with therapeutic INRs at 24 hours22,23,24,25,26,27 than did studies without such restrictions28,29(Tables 2 and 3). This evidence suggests that the use of low-dose oral vitamin K therapy should be confined to patients with INRs below 10. Among the studies that examined INR values below 10, the threshold for intervention with vitamin K ranged from 4.5 to 6.0. This included 4 RCTs involving patients with INR values between 4.5 and 10,23,24 or between 6.0 and 10.22,25 The decision to treat with oral vitamin K therapy is influenced by patient variables, including, but not limited to, the INR. However, on the basis of the RCTs reviewed, oral vitamin K would be an appropriate treatment option for an INR between 4.5 and 10.
What dose of oral vitamin K therapy is most appropriate?
The fear of over-correcting the INR has been cited as one barrier to the widespread use of vitamin K.6 However, our review suggests that this occurs infrequently when small doses of vitamin K are administered orally. Oral doses between 1.0 mg and 2.5 mg appear to produce similar, and low, rates of over-correction (Tables 2 and 3). One study29 found that the INR fell below 2.0 in 33% of patients who received 2.0 mg of vitamin K orally, as compared with 0%–16% of patients in studies in which a 1.0-mg oral dose was used. This suggests that the preferred dose for patients with INR values between 4.5 and 10 is 1.0 mg.
What is the risk of bleeding or thrombosis if vitamin K is given?
Convincing evidence that oral vitamin K therapy reduces the risk of bleeding is not yet available. Similarly, although widely discussed, there is no evidence that transient vitamin K-associated over-correction of the INR causes thrombosis. In the 8 studies reviewed, only one thrombotic event was described among the 344 patients who received oral, subcutaneous or intravenous vitamin K therapy. This patient had a myocardial infarction 3 days after receiving 1 mg of vitamin K orally.23
Only 2 of the studies specifically examined the effect of vitamin K on the risk of bleeding. Patel and colleagues22 found a nonsignificant reduction in the rate of minor bleeding among 3 of 15 patients randomly assigned to receive vitamin K, as compared with 1 of 15 given placebo (p = 0.30). How bleeding events were determined was not described. The larger sample in Crowther and colleagues' RCT of 1.0 mg of vitamin K had greater power to detect differences in bleeding; after 3 months of follow-up, the difference in bleeding events between the vitamin K arm (2/45) and the placebo arm (8/45) was at the margins of statistical significance (p = 0.0499).23 Other than these 2 small studies, there is at present no clinical evidence that oral vitamin K therapy reduces the risk of bleeding. However, the association between the use of oral vitamin K therapy and a reduced INR, an established proxy measure for a decreased risk of bleeding, is supported by all of the studies we reviewed. Furthermore, findings from studies of 1.0 mg of vitamin K given orally suggest that this dose can reduce the INR without an increased risk of a subtherapeutic INR, an established proxy measure for thrombotic complications.
Conclusions
Asymptomatic elevation of the INR is a common and clinically important problem, carrying with it a real risk of hemorrhage. Evidence from 4 RCTs suggests that low-dose oral vitamin K therapy promptly reduces an elevated INR. This evidence also suggests that 1.0 mg may be the most appropriate dose, particularly for patients with an INR between 4.5 and 10. Although a theoretical risk of thrombosis exists with the use of low-dose oral vitamin K therapy, how this risk compares with the risk of hemorrhage associated with an untreated elevated INR is not yet clear.
Despite these remaining questions, many health care professionals supervising warfarin therapy routinely supply their patients with vitamin K, to ensure the prompt treatment of an elevated INR without the patient having to visit a health care setting. Patient self-management with the use of oral vitamin K therapy may represent a promising avenue for the use of vitamin K in anticoagulation control.
Acknowledgments
Mark Crowther holds a Research Scholarship from the Canadian Institutes of Health Research.
Footnotes
This article has been peer reviewed.
Contributors: Sarah Wilson contributed substantially to the analysis and interpretation of the literature review and prepared the initial draft of this article. Mark Crowther and Henry Watson contributed substantially to the conception of the review. All authors revised the draft critically for important intellectual content and gave final approval of the version to be published.
Competing interests: None declared.
Correspondence to: Dr. Mark A. Crowther, St. Joseph's Hospital, Rm. L208, 50 Charlton Ave. E, Hamilton ON L8N 4A6; fax 905 521-6034; crowthrm@mcmaster.ca
References
- 1.McMahan DA, Smith DM, Carey MA, Zhou XH. Risk of major hemorrhage for outpatient treatment with warfarin. J Gen Intern Med 1998;13(5):311-6. [DOI] [PMC free article] [PubMed]
- 2.Samsa GP, Matchar DB, Goldstein LB, Bonito AJ, Lux LJ, Witter DM, et al. Quality of anticoagulation management among patients with atrial fibrillation: results of a review of medical records from 2 communities. Arch Intern Med 2000;160(7):967-73. [DOI] [PubMed]
- 3.Kearon C, Gent M, Hirsh J, Weitz J, Kovacs MJ, Anderson DR, et al. A comparison of three months of anticoagulation with extended anticoagulation for a first episode of idiopathic venous thromboembolism. N Engl J Med 1999;340(12):901-7. [DOI] [PubMed]
- 4.Palareti G, Leali N, Coccheri S, Poggi M, Manotti C, D'Angelo A, et al. Bleeding complications of oral anticoagulant treatment: an inception-cohort, prospective collaborative study (ISCOAT). Lancet 1996;348(7372):423-8. [DOI] [PubMed]
- 5.Oden A, Fahlen M. Oral anticoagulation and risk of death: a medical record linkage study. BMJ 2002;325(7372):1073-5. [DOI] [PMC free article] [PubMed]
- 6.Hylek EM, Chang Y, Skates SJ, Hughes RA, Singer DE. Prospective study of the outcomes of ambulatory patients with excessive warfarin anticoagulation. Ann Intern Med 2000;160(11):1612-7. [DOI] [PubMed]
- 7.Crowther MA, Ginsberg JS, Julian J, Denburg J, Hirsh J, Douketis J, et al. A comparison of two intensities of warfarin for the prevention of recurrent thrombosis in patients with the antiphospholipid antibody syndrome. N Engl J Med 2003;349(12):1133-8. [DOI] [PubMed]
- 8.Hirsh J, Dalen JE, Anderson DR, Pollex L, Bussey H, Ansell J, et al. Oral anticoagulants: mechanism of action, clinical effectiveness, and optimal therapeutic range [review]. Chest 2001;119(1 Suppl):8S-21S. [DOI] [PubMed]
- 9.White RH, Minton SM, Andya MD, Hutchinson R. Temporary reversal of anticoagulation using oral vitamin K. J Thromb Thrombolysis 2000;10(2):149-53. [DOI] [PubMed]
- 10.Pengo V, Banzato A, Garelli E, Zasso A, Biasiolo A. Reversal of excessive effect of regular anticoagulation: low oral dose of phytonadione (vitamin K1) compared with warfarin discontinuation. Blood Coagul Fibrinolysis 1993;4(5):739-41. [PubMed]
- 11.Wentzien TH, O'Reilly RA, Kearns PJ. Prospective evaluation of anticoagulant reversal with oral vitamin K1 while continuing warfarin therapy unchanged. Chest 1998;114(6):1546-50. [DOI] [PubMed]
- 12.Penning-van Beest FJ, Rosendaal FR, Grobbee DE, van Meegen E, Stricker BH. Course of the International Normalized Ratio in response to oral vitamin K1 in patients overanticoagulated with phenprocoumon. Br J Haematol 1999;104(2):241-5. [DOI] [PubMed]
- 13.Fondevila CG, Grosso SH, Santarelli MT, Pinto MD. Reversal of excessive oral anticoagulation with a low oral dose of vitamin K1 compared with acenocoumarin discontinuation. A prospective, randomized, open study. Blood Coagul Fibrinolysis 2001;12(1):9-16. [DOI] [PubMed]
- 14.Ortin M, Olalla J, Marco F, Velasco N. Low-dose vitamin K1 versus short-term withholding of acenocoumarol in the treatment of excessive anticoagulation episodes induced by acenocoumarol. A retrospective comparative study. Haemostasis 1998;28(2):57-61. [DOI] [PubMed]
- 15.Cosgriff SW. The effectiveness of an oral vitamin K1 in controlling excessive hypoprothrombinemia during anticoagulant therapy. Ann Intern Med 1956;45 (1):14-22. [DOI] [PubMed]
- 16.Poli D, Antonucci E, Lombardi A, Gensini GF, Abbate R, Prisco D, et al. Safety and effectiveness of low dose oral vitamin K1 administration in asymptomatic out-patients on warfarin or acenocoumarol with excessive anticoagulation. Haematologica 2003;88(2):237-8. [PubMed]
- 17.Harrell CC, Kline SS. Oral vitamin K1: an option to reduce warfarin's activity. Ann Pharmacother 1995;29(12):1228-32. [DOI] [PubMed]
- 18.Cruickshank J, Ragg M, Eddey D. Warfarin toxicity in the emergency department: recommendations for management. Emerg Med (Fremantle) 2001;13(1):91-7. [DOI] [PubMed]
- 19.Weibert RT, Le DT, Kayser SR, Rapaport SI. Correction of excessive anticoagulation with low-dose oral vitamin K1. Ann Intern Med 1997;126(12):959-62. [DOI] [PubMed]
- 20.Whitling AM, Bussey HI, Lyons RM. Comparing different routes and doses of phytonadione for reversing excessive anticoagulation. Arch Intern Med 1998;158(19):2136-40. [DOI] [PubMed]
- 21.Taylor CT, Chester EA, Byrd DC, Stephens MA. Vitamin K to reverse excessive anticoagulation: a review of the literature. Pharmacotherapy 1999;19(12):1415-25. [DOI] [PubMed]
- 22.Patel RJ, Witt DM, Saseen JJ, Tillman DJ, Wilkinson DS. Randomized, placebo-controlled trial of oral phytonadione for excessive anticoagulation. Pharmacotherapy 2000;20(10):1159-66. [DOI] [PubMed]
- 23.Crowther MA, Julian J, McCarty D, Douketis J, Kovacs M, Biagoni L, et al. Treatment of warfarin-associated coagulopathy with oral vitamin K: a randomised controlled trial. Lancet 2001;356(9241):1551-3. [DOI] [PubMed]
- 24.Crowther MA, Douketis JD, Schnurr T, Steidl L, Mera V, Ultori C, et al. Oral vitamin K lowers the international normalized ratio more rapidly than subcutaneous vitamin K in the treatment of warfarin-associated coagulopathy. A randomized, controlled trial. Ann Intern Med 2002;137(4):251-4. [DOI] [PubMed]
- 25.Lubetsky A, Yonath H, Olchovsky D, Loebstein R, Halkin H, Ezra D. Comparison of oral versus intravenous phytonadione (Vitamin K1) in patients with excessive anticoagulation: a prospective randomized controlled study. Arch Intern Med 2003;163(20):2469-73. [DOI] [PubMed]
- 26.Crowther MA, Donovan D, Harrison L, McGinnis J, Ginsberg J. Low-dose oral vitamin K reliably reverses over-anticoagulation due to warfarin. Thromb Haemost 1998;79(6):1116-8. [PubMed]
- 27.Duong TM, Plowman BK, Morreale AP, Janetzky K. Retrospective and prospective analyses of the treatment of overanticoagulated patients. Pharmacotherapy 1998;18(6):1264-70. [PubMed]
- 28.Pendry K, Bhavnani M, Shwe K. The use of oral vitamin K for reversal of over-warfarinization [letter]. Br J Haematol 2001;113(3):839-40. [DOI] [PubMed]
- 29.Watson HG, Baglin T, Laidlaw SL, Makris M, Preston E. A comparison of the efficacy and rate of response to oral and intravenous vitamin K in reversal of over-anticoagulation with warfarin. Br J Haematol 2001;115(1):145-9. [DOI] [PubMed]
- 30.Lousberg TR, Witt DM, Beall DG, Carter BL, Malone DC. Evaluation of excessive anticoagulation in a group model health maintenance organization. Arch Intern Med 1998;158(5):528-34. [DOI] [PubMed]
- 31.Glover JJ, Morrill GB. Conservative treatment of overanticoagulated patients. Chest 1995;108(4):987-90. [DOI] [PubMed]
- 32.Wilson SE, Douketis JD, Crowther MA. Treatment of warfarin-associated coagulopathy: a physician survey. Chest 2001;120(6):1972-6. [DOI] [PubMed]
- 33.Nee R, Doppenschmidt D, Donovan DJ, Andrews TC. Intravenous versus subcutaneous vitamin K1 in reversing excessive oral anticoagulation. Am J Cardiol 1999;83(2):286-8. [DOI] [PubMed]
- 34.Raj G, Kumar R, McKinney WP. Time course of reversal of anticoagulant effect of warfarin by intravenous and subcutaneous phytonadione. Arch Intern Med 1999;159(22):2721-4. [DOI] [PubMed]
- 35.Martinez-Abad M, Delgado F, Palop V, Morales-Olivas FJ. Vitamin K and anaphylactic shock. Ann Pharmacother 1991;25(7-8):871-2. [DOI] [PubMed]


