Abstract
Cancer cells generally have a high rate of glycolysis and produce larger quantities of lactate as compared to the surrounding normal cells. Monocarboxylate transporter 4 (MCT4) is one of the proton pumps exchanging the lactate through the plasma membrane. The prognostic significance of MCT4 expression has not been evaluated in patients with colorectal cancer (CRC). Surgical specimens from 105 CRC patients were immunohistochemically stained using a polyclonal anti-MCT4 antibody. The relationships among the MCT4 expression, clinicopathological factors and prognosis were evaluated. A total of 53 (50.5%) of the 105 patients with CRC were determined to have tumors positive for MCT4 expression. The expression of MCT4 significantly correlated with the tumor size, depth of invasion, lymph node metastasis, distant metastasis and TNM staging. The survival rate of the patients who were positive for MCT4 expression was significantly lower than that of patients with negative MCT4 expression. Positive MCT4 expression was a significantly poor prognostic factor, as determined by both univariate and multivariate analyses. Therefore, positive MCT4 expression appears to be a useful marker for tumor progression and prognosis in patients with CRC.
Keywords: monocarboxylate transporter, monocarboxylate transporter 4, colorectal cancer
Introduction
Colorectal cancer (CRC) is one of the most lethal cancers in the world. In Japan, cancer-related death from CRC was estimated to be the most frequent cause of female cancer-related death, and the third most frequent cause of male cancer-related death in 2008 (1). Recent advances in chemotherapy have been improving the overall survival of patients with metastatic CRC, however, the prognosis of patients with metastatic CRC remains relatively low. Therefore, identification of prognostic factors that could select CRC patients at a high risk of recurrence would be helpful for planning better treatment strategies.
Cancer cells generally are hyper-proliferative, have a high rate of glycolysis and exert anti-apoptotic effects compared to surrounding normal cells. Glycolysis is a key step for the acquisition of ATP in all mammalian cells, including cancer tissues. Metabolism of glucose via glycolysis results in the production of high concentrations of lactate, which must be transported out of cells (2). This transport of lactate across the plasma membrane is mediated by a family of protone-coupled monocarboxylate transporters (MCTs) (3).
The MCT family has 14 members (3). Of these members, only MCT1-MCT4 catalyze the proton-coupled transport of lactate (4–8). The distribution of MCTs is different by cell type. While MCT1 is expressed in most cells (3,4), the highest expression of MCT2 is observed in the testis (9), and MCT3 expression is largely restricted to the retinal pigment epithelium (3,4). On the other hand, MCT4 is strongly expressed in highly glycolytic cells, such as white muscle (10), white blood cells (4,7) and tumors (11–13). Recently, we reported that MCT4 expression of lung cancer cell lines are strongly correlated with invasion activity in Matrigel (14).
Cancer cells produce a large amount of lactic acid (2), which is generated through glucose metabolism and inefficient vascular clearing, resulting in an acidic microenvironment within many solid tumors (15). The partial pressure of oxygen within human cancer is frequently much lower than that of the surrounding normal tissue, and intratumoral hypoxia is associated with an increased risk of local spread, metastasis and patient mortality (16).
In order to prevent apoptosis due to cellular acidosis, tumor cells increase their proton efflux through pH regulators, such as proton pumps, sodium-proton exchangers, bicarbonate transporters and MCTs, which have been described as being up-regulated in tumor cells (17). However, only few studies have evaluated the immunohistochemical expression of MCT4 in cancer specimens (11–13). The significance of MCT4 expression in CRC has not been fully evaluated, especially with regard to its relationship to prognosis. Therefore, the present study investigated the relationship between clinicopathological factors and the immunohistochemical MCT4 expression on the plasma membrane of the primary CRC cells, and prognostic factors of primary CRC patients.
Patients and methods
Patients
A total of 105 patients with primary CRC who underwent surgery at the Department of Surgery 1 of the University Hospital of Occupational and Environmental Health, Japan, from 1997 to 2000, were recruited for this study. The clinical data of these patients are summarized in Table I. Informed consent was obtained from all patients prior to the study. No patients had received chemotherapy or radiotherapy before surgery. The clinicopathological findings were determined according to UICC tumor-node-metastasis (TNM) classifications (18).
Table I.
Patient characteristics.
| No. of patients | 105 |
| Gender (M/F) | 59/46 |
| Age (years; mean ± SD) | 65.3±12.1 |
| Tumor size (cm; mean ± SD) | 5.3±2.1 |
| Histological type | |
| Differentiated | 99 |
| Undifferentiated | 6 |
| Depth of invasion | |
| T1/T2/T3/T4a/T4b | 1/19/40/17/28 |
| Lymph node metastasis (−/+) | 50/55 |
| Distant metastasis (−/+) | 82/23 |
| TNM stage | |
| I/II/III/IV | 17/31/34/23 |
| Lymphatic invasion (weak/strong) | 64/41 |
| Venous invasion (−/+) | 62/43 |
The weak group of lymphatic invasion indicated score 0 and 1, and the strong group indicated score 2 and 3 by the Japan Classification of Colorectal Cancer.
Antibody
For the immunohistochemical staining of monocarboxylate transporter 4 (MCT4), an anti-MCT4 rabbit polyclonal antibody (H-90) (sc-50329) was purchased from Santa Cruz Biotechnology, Inc.
Immunohistochemical staining of MCT4
The immunohistochemical staining (IHC) of MCT4 was performed on formalin-fixed 2-μm sections of tissues embedded in paraffin. The 2-μm sections were deparaffinized in xylene and then rehydrated. Endogenous peroxidase was blocked with 3% hydrogen peroxidase in methanol for 10 min. After washing with phosphate-buffered saline (PBS), the sections were pre-incubated with 10% rabbit serum albumin in PBS for 10 min at room temperature. The slides were then incubated with the MCT4 antibody for 1 h at room temperature (dilution 1:100). Antibody binding was visualized using the EnVision+ Dual link system and diaminobenzidine as chromogen (Dako Cytomation, Kyoto, Japan). The slides were counterstained with methyl green and mounted.
Staining evaluation
Immunostained slides were analyzed independently by two authors. Slight differences were resolved by simultaneous viewing. The expression of MCT4 in the CRC specimens was evaluated according to the methods described by Pinheiro et al (13). Sections were scored semi-quantitatively for the extent of immunoreaction as follows: 0, 0% immunoreactive cells; 1, <5% immunoreactive cells; 2, 5–50% immunoreactive cells; and 3, >50% immunoreactive cells. In addition, the intensity of staining was scored semi-quantitatively as 0, negative; 1, weak; 2, intermediate; and 3, strong. The final immunoreactions score was defined as the sum of both parameters (extension and intensity), and samples were grouped as negative (0), weak staining (1–2), moderate staining (3) and strong staining (4–6). For statistical purposes, only moderate and strong final immunoreaction scores were considered to be positive. The other final scores were considered to be negative.
Clinicopathological assessment
The tumors were staged by two pathologists, who had no prior knowledge of the results of the assays, according to UICC TNM classifications 7th edition (18). Clinicopathological factors, such as age, gender, tumor size, histological type, depth of invasion, lymph node metastasis, distant metastasis and TNM staging, were analyzed for an association with MCT4 expression.
Statistical analysis
The relationships between the parameters were also statistically assessed using the Chi-square test with the Stat View-J statistical package (version 5.0; SAS Institute, Inc., Cary, NC, USA). The Kaplan-Meier method was applied to determine survival, and statistical significance was calculated using the log-rank test. Both univariate and multivariate analyses of survival were conducted using the Cox proportional hazards model. Since the number of patients with TNM stage IV was the same as the number of patients with distant metastasis, distant metastasis was excluded as a variable from the multivariate analysis. Statistical significance was established at p≤0.05.
Results
Table I shows the profiles of the 105 patients diagnosed with primary CRC recruited for the present study.
IHC staining of endogenous MCT4 was performed on 105 CRC specimens. Expression of MCT4 was mainly observed on the plasma membrane of the normal colonic mucosa (Fig. 1). Positive signals for MCT4 were mainly observed on the plasma membrane and slightly observed in the cytoplasm in the cancer cells (Fig. 2A). The MCT4 expression on the plasma membrane was graded as weak in 49.5% of all cases, moderate in 8.6% and strong in 41.9% of all cases, and none of the patients had negative staining. A total of 53 (50.5%) of the 105 patients with CRC were determined to have positive MCT4 expression, and 52 cases (49.5%) had negative MCT4 expression.
Figure 1.
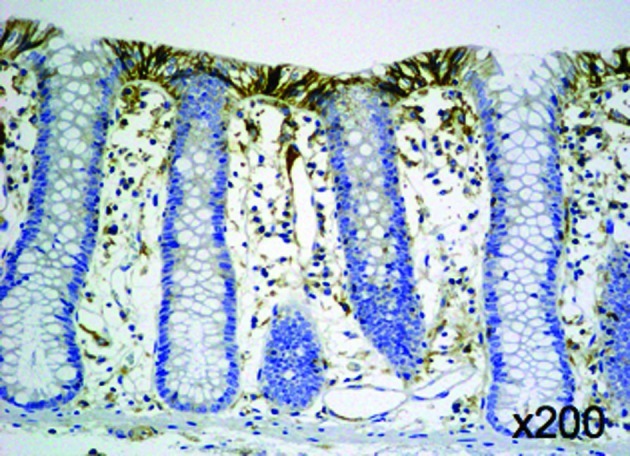
Immunohistochemical staining of MCT4 in normal colonic mucosa.
Figure 2.
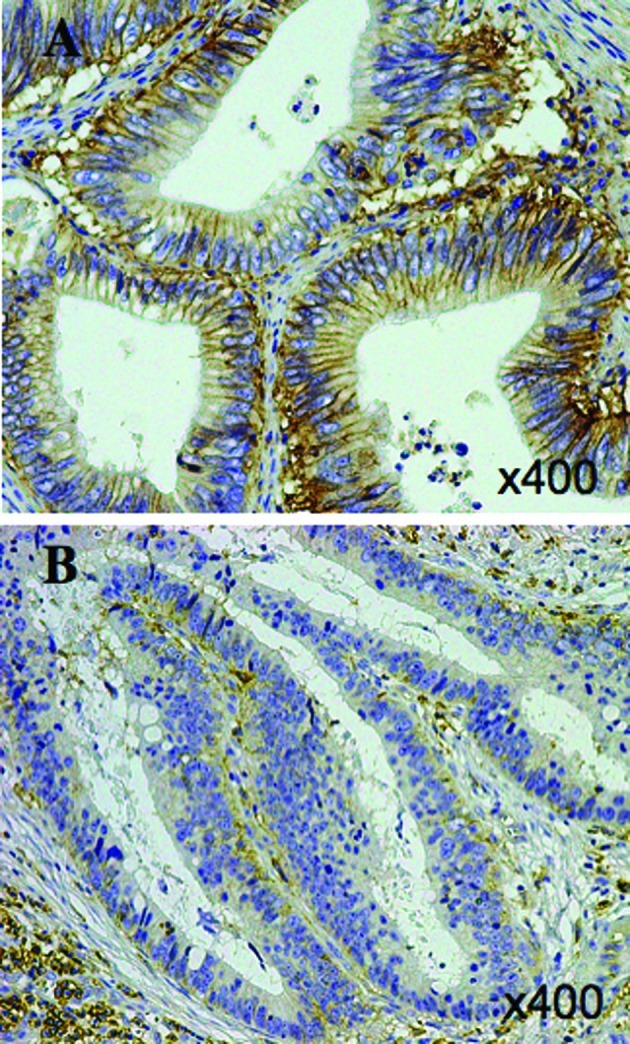
Immunohistochemical staining of MCT4 in colorectal cancer. (A) Positive expression (final score 6) of MCT4; (B) negative expression (final score 0) of MCT4.
According to the evaluation of the MCT4 immunostaining, the expression of MCT4 was found to significantly correlate with the tumor size, depth of invasion, lymph node metastasis, distant metastasis and TNM staging. However, the expression of MCT4 did not correlate with age, gender or histopathological type (Table II).
Table II.
Association between the expression of MCT4 and clinicopathological factors of all patients with colorectal cancer.
| MCT4 expression
|
p-value | |||
|---|---|---|---|---|
| Negative | Positive | |||
| Age (years) | 0.7763 | |||
| Young | 24 | 23 | ||
| Old | 28 | 30 | ||
| Gender | 0.7587 | |||
| Male | 30 | 29 | ||
| Female | 22 | 24 | ||
| Tumor size (cm) | 0.0220 | |||
| Small | 36 | 25 | ||
| Large | 16 | 28 | ||
| Histological type | 0.9808 | |||
| Differentiated | 49 | 50 | ||
| Undifferentiated | 3 | 3 | ||
| Depth of invasion (T) | 0.0096 | |||
| ≤T4a | 44 | 33 | ||
| T4b | 8 | 20 | ||
| Lymph node metastasis (N) | 0.0148 | |||
| (−) | 31 | 19 | ||
| (+) | 21 | 34 | ||
| Distant metastasis (M) | 0.0110 | |||
| (−) | 46 | 36 | ||
| (+) | 6 | 17 | ||
| TNM stage | 0.0110 | |||
| I, II, III | 46 | 36 | ||
| IV | 6 | 17 | ||
| Lymphatic invasion | 0.0850 | |||
| Weak | 36 | 28 | ||
| Strong | 16 | 25 | ||
| Venous invasion | 0.3623 | |||
| (−) | 33 | 29 | ||
| (+) | 19 | 24 | ||
The patients were divided into young and old groups of age assessed with the mean value of 65.3 years as the cut-off value. The patients were divided into small and large tumor groups assessed with the mean value of 5.3 cm in diameter as the cut-off value. The weak group of lymphatic invasion indicated score 0 and 1, and the strong group indicated score 2 and 3 by the Japan Classification of Colorectal Cancer.
The results of the Kaplan-Meier analyses for overall survival based on MCT4 expression are shown in Fig. 3. The median follow-up time was 71 months (range 1.4–115.9). The survival rate of the patients who had negative MCT4 expression was significantly higher than that of patients with positive MCT4 expression (5-year survival rate, 88.2 vs. 55%, p=0.0001; Fig. 3).
Figure 3.
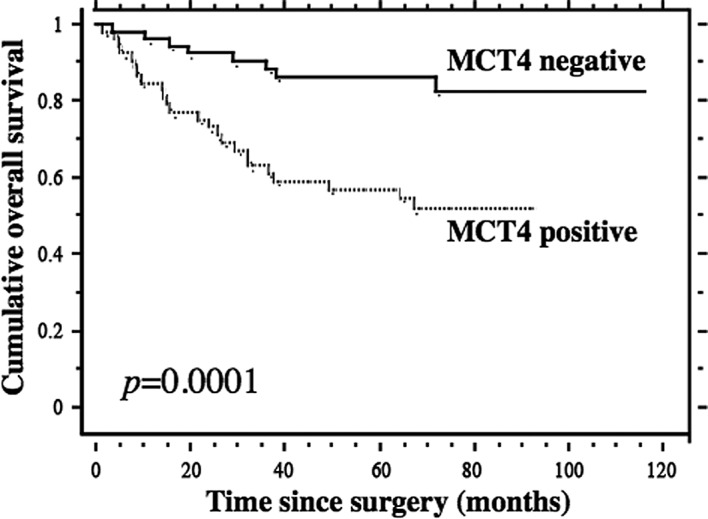
The prognostic significance of MCT4 expression was analyzed using the Kaplan-Meier method in the patients with colorectal cancer (n=105). The patients were divided into negative and positive groups according to the previous classification. The patients in the MCT4-negative group showed a significantly more favorable prognosis in comparison to those in the MCT4-positive group (p=0.0001).
Univariate analysis indicated that the TNM stage, depth of invasion, presence of lymph node metastasis, presence of distant metastasis, MCT4 expression and histological type were significant prognostic factors for CRC (Table III). As the data for TNM staging were related to the presence of distant metastasis, the data for the distant metastasis were omitted from the multivariate analysis.
Table III.
Univariate analysis of the clinicopathological factors and the expression of MCT4 in patients with colorectal cancer.
| Factor | p-value of univariate analysis |
|---|---|
| TNM stage (I, II, III vs. IV) | <0.0001 |
| T (T1, T2, T3, T4a vs. T4b) | <0.0001 |
| N (− vs. +) | <0.0001 |
| M (− vs. +) | <0.0001 |
| Lymphatic invasion (weak vs. strong) | <0.0001 |
| Venous invasion (− vs. +) | <0.0001 |
| MCT4 expression (negative vs. positive) | 0.0001 |
| Histological type (diff. vs. undiff.) | 0.0003 |
| Gender (M vs. F) | 0.0936 |
| Tumor size (small vs. large) | 0.3086 |
| Age (young vs. old) | 0.5735 |
The patients were divided into young and old groups of age assessed with the mean value of 65.3 years as the cut-off value. The patients were divided into small and large tumor groups assessed with the mean value of 5.3 cm in diameter as the cut-off value. The weak group of lymphatic invasion indicated score 0 and 1, and the strong group indicated score 2 and 3 by the Japan Classification of Colorectal Cancer.
Therefore, the multivariate analysis indicated that the TNM stage, lymph node metastasis and MCT4 expression were significant prognostic factors for patients with CRC (Table IV).
Table IV.
Multivariate analysis of the clinicopathological factors and the expression of MCT4 in patients with colorectal cancer.
| Factor | p-value | Hazard ratio | 95% CI |
|---|---|---|---|
| TNM stage (I, II, III vs. IV) | <0.0001 | 0.108 | 0.040–0.290 |
| N (− vs. +) | 0.0120 | 0.124 | 0.024–0.632 |
| MCT4 expression (negative vs. positive) | 0.0201 | 3.163 | 1.198–8.356 |
| Histological type (diff. vs. undiff.) | 0.1302 | 0.438 | 0.150–1.276 |
| Venous invasion (− vs. +) | 0.1820 | 0.544 | 0.223–1.330 |
| T (T1, T2, T3, T4a vs. T4b) | 0.7348 | 1.160 | 0.491–2.744 |
| Lymphatic invasion (weak vs. strong) | 0.8877 | 0.934 | 0.361–2.417 |
The weak group of lymphatic invasion indicated score 0 and 1, and the strong group indicated score 2 and 3 by the Japan Classification of Colorectal Cancer.
Discussion
Only a few studies that have evaluated the IHC expression of MCT4 in cancer specimens have been reported (11–13). In the present study, we demonstrated that 53 (50.5%) of 105 patients with CRC were clearly determined to have positive MCT4 expression, and 52 cases (49.5%) had negative MCT4 expression (no or weak IHC staining) on the plasma membrane. The other reports indicated controversial results concerning the IHC expression of MCT4 in CRC (11–13). One report indicated an absence of MCT4 expression in CRC (11), while another report indicated the presence of weak MCT4 expression in the tumor environment (12). The third report indicated that 96% of 126 patients with CRC were determined to have positive MCT4 expression in the cytoplasm or on the plasma membrane, and 38.1% of 126 patients were determined to have positive expression on the plasma membrane (13). These discrepancies may be due to the different antibodies which were used in these studies. Cellular protein recognized by our antibody against MCT4 was completely abolished by transfection of two different types of specific MCT4 siRNA (14).
Our study indicated that positive MCT4 expression on the plasma membrane significantly correlated with tumor size, depth of invasion, lymph node metastasis, distant metastasis and TNM staging. However, positive MCT4 expression did not correlate with age, gender, lymphatic invasion, venous invasion or the histopathological type (Table II). These data indicate that positive MCT4 expression on the plasma membrane may reflect the tumor progression in CRC. Several studies have indicated that the behavior of cancer cells which express MCT4 is different from cells not expressing MCT4. According to an experimental study using lung cancer cell lines, the invasion of the lung cancer cells was reduced by knockdown of MCT4 using MCT4 siRNA (14). Gallagher et al indicated that the silencing of MCT4 in MDA-MB-231 cells impaired their migration (19). Since lactate is co-transported out of the cells with a proton, silencing MCT would be expected to decrease the intracellular pH and increase the extracellular pH. Integrin-mediated cell migration is pH-sensitive, and is inhibited by alkalization of the extracellular environment (20,21). Therefore, these studies indicated that a high expression of MCT4 may induce tumor progression.
Our study indicated that the TNM stage, depth of invasion, lymph node metastasis, distant metastasis, MCT4 expression, lymphatic invasion, venous invasion and histological type were significant prognostic factors by univariate analysis (Table III). Moreover, multivariate analysis indicated that the TNM stage, lymph node metastasis and MCT4 expression were significant prognostic factors for patients with CRC (Table IV). These data indicate that positive MCT4 expression on the plasma membrane correlates with the tumor progression of CRC and the poor survival of patients with CRC.
The accumulation of lactate within tumors has been reported to be associated with a poor clinical outcome (22,23). It is well established that increased rates of glycolysis in hypoxia are associated with greater expression of glycolytic enzymes, including the glucose transporter, Glut-1, due to a transcriptional mechanism involving a hypoxia inducible factor (HIF-1α) (24). Ullah et al indicated that MCT4, like other glycolytic enzymes, is up-regulated by hypoxia through a HIF-1α-mediated mechanism (25). Chronic hypobaric hypoxia has been reported to up-regulate MCT4, but not MCT1, in rat skeletal muscle (26), zebra fish gills (27) and certain tumor cells (28), at least in part, through a transcriptional mechanism. These studies suggest that the accumulation of lactate within tumors up-regulates MCT4 through a HIF-1α-mediated mechanism and that this correlates with a poor clinical outcome.
Certain studies have indicated the relationship between MCT4 and drug resistance. Overexpression of CD44v3-10, MDR1 and MCT4 was found in most primary prostate cancer tissues, and was significantly associated with prostate cancer progression (29). Another study indicated that the overexpression of CD147, MCT1 and MCT4 is correlated with the progression of epithelial ovarian cancer (EOC) (30). This suggests that the overexpression of MCT1/MCT4 is related to drug resistance during EOC metastasis, and that these proteins could be useful therapeutic targets to prevent the development of incurable, recurrent and drug-resistant EOC (30). These studies indicate that the overexpression of MCT4 may be related to drug-resistance through induction of the expression of MDR.
Many inhibitors of the MCT family have been reported (31). DDS is an anion transporter inhibitor and suppresses the function of all proteins in the MCT family. Quercetin and simvastatin inhibit human MCT1 and human MCT4, respectively. Simvastatin has been studied for the treatment of several malignancies, such as colon cancer, prostate cancer and chronic lymphocytic leukemia (32–35). In fact, a phase II study of simvastatin plus irinotecan, 5-fluoruracil and leucovorin as first-line chemotherapy has been carried out (33).
The mechanisms of MCT4 regulation are not fully understood. However, the regulation of MCT4 expression may be important, since CRC patients with negative MCT4 immuno-staining had a more favorable prognosis. More extensive studies concerning the regulation of MCT4 are therefore required.
Acknowledgments
The authors thank Ms. Yuko Ueda, Hitomi Arimasu and Miyuki Warashina for the technical assistance. This study was supported in part by a Grant-in-Aid for Scientific Research from the Ministry of Education, Science and Culture of Japan.
References
- 1.Center for Cancer Control and Information Services, National Cancer Center, Japan: Vital Statistics Japan (Ministry of Health, Labour and Welfare).
- 2.Gullino PM, Clark SH, Grantham FH. The interstitial fluid of solid tumors. Cancer Res. 1964;24:780–796. [PubMed] [Google Scholar]
- 3.Halestrap AP, Meredith AP. The SLC16 gene family – from monocarboxylate transporters (MCTs) to aromatic amino acid transporters and beyond. Pflugers Arch Eur J Physiol. 2004;447:619–628. doi: 10.1007/s00424-003-1067-2. [DOI] [PubMed] [Google Scholar]
- 4.Halestrap AP, Price NT. The proton-linked monocarboxylate transporter (MCT) family: structure, function and regulation. Biochem J. 1999;343:281–299. [PMC free article] [PubMed] [Google Scholar]
- 5.Bröer S, Bröer A, Schneider HP, Stegen C, Halestrap AP, Deitmer JW. Characterization of the high-affinity monocarboxylate transporter MCT2 in Xenopus laevis oocyte. Biochem J. 1999;341:529–535. doi: 10.1042/0264-6021:3410529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grollman EF, Philp NJ, McPhie P, Ward RD, Sauer B. Determination of tranport kinetics of chick MCT3 monocarboxylate transporter from retinal pigment epithelium by expression in genetically modified yeast. Biochemistry. 2000;39:9351–9357. doi: 10.1021/bi000464+. [DOI] [PubMed] [Google Scholar]
- 7.Dimmer KS, Friedrich B, Lang F, Deitmer JW, Bröer S. The low-affinity monocarboxylate transporter MCT4 is adapted to the export of lactate in highly glycolytic cells. Biochem J. 2000;350:219–227. [PMC free article] [PubMed] [Google Scholar]
- 8.Manning Fox JE, Meredith D, Halestrap AP. Characterisation of human monocarboxylate transporter 4 substantiates its role in lactic acid efflux from skeletal muscle. J Physiol. 2000;529:285–293. doi: 10.1111/j.1469-7793.2000.00285.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lin RY, Vera JC, Chaganti RS, Golde DW. Human monocarboxylate transporter 2 (MCT2) is a high affinity pyruvate transporter. J Biol Chem. 1998;273:28959–28965. doi: 10.1074/jbc.273.44.28959. [DOI] [PubMed] [Google Scholar]
- 10.Juel C, Halestrap AP. Lactate transporter in skeletal muscle-role of regulation of the monocarboxylate transporter. J Physiol. 1999;517:633–642. doi: 10.1111/j.1469-7793.1999.0633s.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lambert DW, Wood IS, Ellis A, Shirazi-Beechey SP. Molecular changes in the expression of human colonic nutrient transporters during the transition from normality to malignancy. Br J Cancer. 2002;86:1262–1269. doi: 10.1038/sj.bjc.6600264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Koukourakis MI, Giatromanolaki A, Harris AI, Sivridis E. Comparison of metabolic pathways between cancer cells and stromal cells in colorectal carcinomas: a metabolic survival role for tumor-associated stroma. Cancer Res. 2006;66:632–637. doi: 10.1158/0008-5472.CAN-05-3260. [DOI] [PubMed] [Google Scholar]
- 13.Pinheiro C, Longatto-Filho A, Scapulatempo C, Ferreira L, Martins S, Pellerin L, Rodrigues M, Alves VAF, Schmitt F, Baltazar F. Increased expression of monocarboxylate transpoerters 1, 2 and 4 in colorectal carcinomas. Virchows Arch. 2008;452:139–146. doi: 10.1007/s00428-007-0558-5. [DOI] [PubMed] [Google Scholar]
- 14.Izumi H, Takahashi M, Uramoto H, Nakayama Y, Oyama T, Wang K-Y, Sasaguri Y, Nishizawa S, Kohno K. Monocarboxylate transporter 1 and 4 involved in the invasion activity of human lung cancer cells. Cancer Sci. 2011;102:1007–1013. doi: 10.1111/j.1349-7006.2011.01908.x. [DOI] [PubMed] [Google Scholar]
- 15.Gatenby RA, Gillies RJ. Why do cancers have high aerobic glycolysis? Nat Rev Cancer. 2004;4:891–899. doi: 10.1038/nrc1478. [DOI] [PubMed] [Google Scholar]
- 16.Vaupel P, Mayer A. Hypoxia and cancer: significance and impact on clinical outcome. Cancer Metastasis Rev. 2007;26:225–239. doi: 10.1007/s10555-007-9055-1. [DOI] [PubMed] [Google Scholar]
- 17.Izumi H, Torigoe T, Ishiguchi H, Uramoto H, Yoshida Y, Tanabe M, Ise T, Murakami T, Yoshida T, Nomoto M, Kohno K. Cellular pH regulators: potentially promising molecular targets for cancer chemotherapy. Cancer Treat Rev. 2003;29:541–549. doi: 10.1016/s0305-7372(03)00106-3. [DOI] [PubMed] [Google Scholar]
- 18.Sobin LH, Gospodarowicz MK, Wittekind C, editors. International Union Against Cancer (UICC) TNM Classification of Malignant Tumors. 7th edition. Wiley-Liss; New York: 2010. [Google Scholar]
- 19.Gallagher SM, Castorino JJ, Wang D, Philp NJ. Monocarboxylate transporter 4 regulates maturation and trafficking of CD147 to the plasma membrane in the metastatic breast cancer cell line MDA-MB-231. Cancer Res. 2007;67:4182–4189. doi: 10.1158/0008-5472.CAN-06-3184. [DOI] [PubMed] [Google Scholar]
- 20.Betapudi V, Licata LS, Egelhoff TT. Distinct roles of nonmuscle myosin II isoforms in the regulation of MDA-MB-231 breast cancer cell spreading and migration. Cancer Res. 2006;66:4725–4733. doi: 10.1158/0008-5472.CAN-05-4236. [DOI] [PubMed] [Google Scholar]
- 21.Stock C, Gassner B, Hauck CR, Arnold H, Mally S, Eble JA, Dieterich P, Schwab A. Migration of human melanoma cells depends on extracellular pH and Na−/H+ exchange. J Physiol. 2005;567:225–238. doi: 10.1113/jphysiol.2005.088344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kennedy KM, Dewhirst MW. Tumor metabolism of lactate: the influence and therapeutic potential for MCT and CD147 regulation. Future Oncol. 2010;6:127–148. doi: 10.2217/fon.09.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Walenta S, Wetterling M, Lehrke M, Schwickert G, Sundfor K, Rofstad EK, Mueller-Klieser W. High lactate levels predict likelihood of metastasis, tumor recurrence, and restricted patient survival in human cervical cancers. Cancer Res. 2000;60:916–921. [PubMed] [Google Scholar]
- 24.Semenza GL. Hypoxia-inducible factor 1: oxygen homeostasis and disease pathophysiology. Trend Mol Med. 2001;7:345–350. doi: 10.1016/s1471-4914(01)02090-1. [DOI] [PubMed] [Google Scholar]
- 25.Ullah MS, Devies AJ, Halestrap AP. The plasma membrane lactate transporter MCT4, but not MCT1, is upregulated by hypoxia through a HIF-1α-dependent mechanism. J Biol Chem. 2006;281:9030–9037. doi: 10.1074/jbc.M511397200. [DOI] [PubMed] [Google Scholar]
- 26.Py G, Eydoux N, Lambert K, Chapot R, Koulmann N, Sanches H, Bahi L, Peinnequin A, Mercier J, Bigard AX. Role of hypoxia-induced anorexia and right ventricular hypertrophy on lactate transporter and MCT expression in rat muscle. Metabolism. 2005;54:634–644. doi: 10.1016/j.metabol.2004.12.007. [DOI] [PubMed] [Google Scholar]
- 27.Van der Meer DL, van den Thillart GE, Witter F, de Bakker MA, Besser J, Richardson MK, Spaink HP, Leito JT, Bagowski CP. Gene expression profiling of the long-term adaptive response to hypoxia in the gills of adult zebrafish. Am J Physiol Regul Integr Comp Physiol. 2005;289:R1512–R1519. doi: 10.1152/ajpregu.00089.2005. [DOI] [PubMed] [Google Scholar]
- 28.Ord JJ, Streeter EH, Roberts ISD, Cranston D, Harris AL. Comparison of hypoxia transcriptome in vitro with in vivo gene expression in human bladder cancer. Br J Cancer. 2005;93:346–354. doi: 10.1038/sj.bjc.6602666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hao J, Chen H, Madigan MC, Cozzi PJ, Beretov J, Delprado WJ, Russell PJ. Co-expression of CD147 (EMMPRIN), CD44v3-10, MDR1 and monocarboxylate transporters is associated with prostate cancer drug resistance and progression. Br J Cancer. 2010;103:1008–1018. doi: 10.1038/sj.bjc.6605839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chen H, Wang L, Beretov J, Hao J, Xiao W, Li Y. Co-expression of CD147/EMMPRIN with monocarboxylate transporters and multiple drug resistance proteins is associated with epithelial ovarian cancer progression. Clin Exp Metastasis. 2010;27:557–569. doi: 10.1007/s10585-010-9345-9. [DOI] [PubMed] [Google Scholar]
- 31.Morris ME, Felmlee MA. Overview of the proton-coupled MCT (SLC16A) family of transporters: characterization, function and role in the transport of the drug of abuse γ-hydroxybutyric acid. AAPS J. 2008;10:311–321. doi: 10.1208/s12248-008-9035-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cho SJ, Kim JS, Kim JM, Lee JY, Jung HC, Song IS. Simvastatin induces apoptosis in human colon cancer cells and in tumor xenografts, and attenuates colitis-associated colon cancer in mice. Int J Cancer. 2008;123:951–957. doi: 10.1002/ijc.23593. [DOI] [PubMed] [Google Scholar]
- 33.Lee J, Jung KH, Park YS, Ahn JB, Shin SJ, Om SA, Ohdo Y, Shin DB, Kim TW, Lee N, Byun JH, Hong YS, Park JO, Park SH, Lim HY, Kang WK. Simvastatin plus irinotecan, 5-fluorouracil, and leucovorin (FOLFIEI) as first-line chemotherapy in metastatic colorectal patients: a multicenter phase II study. Cancer Chemother Pharmacol. 2009;64:657–663. doi: 10.1007/s00280-008-0913-5. [DOI] [PubMed] [Google Scholar]
- 34.Kochuparambil ST, Al-Husein B, Goc A, Soliman S, Somanath PR. Anticancer efficacy of simvastatin on prostate cancer cells and tumor xenografts is associated with inhibition of Akt and reduced prostate-specific antigen expression. J Pharmacol Exp Ther. 2010;336:496–505. doi: 10.1124/jpet.110.174870. [DOI] [PubMed] [Google Scholar]
- 35.Podhorecka M, Halicka D, Klimek P, Kowal M, Chocholska S, Dmoszynska A. Simvastatin and purine analogs have a synergic effect on apoptosis of chronic lymphocytic leukemia cells. Ann Hematol. 2010;89:1115–1124. doi: 10.1007/s00277-010-0988-z. [DOI] [PMC free article] [PubMed] [Google Scholar]


