Abstract
Context:
High ankle sprains are common in athletes who play contact sports. Most high ankle sprains are treated nonsurgically with a rehabilitation program.
Evidence Acquisition:
All years of PUBMED, Cochrane Database of Systematic Reviews, CINAHL PLUS, SPORTDiscuss, Google Scholar, and Web of Science were searched to August 2010, cross-referencing existing publications. Keywords included syndesmosis ankle sprain or high ankle sprain and the following terms: rehabilitation, treatment, cryotherapy, braces, orthosis, therapeutic modalities, joint mobilization, massage, pain, pain medications, TENS (ie, transcutaneous electric nerve stimulation), acupuncture, aquatic therapy, strength, neuromuscular training, perturbation training, and outcomes.
Results:
Level of evidence, 5. A 3-phase rehabilitation program is described. The acute phase is directed at protecting the joint while minimizing pain, inflammation, muscle weakness, and loss of motion. Most patients are treated with some form of immobilization and have weightbearing restrictions. A range of therapeutic modalities are used to minimize pain and inflammation. Gentle mobilization and resistance exercises are used to gain mobility and maintain muscle size and strength. The subacute phase is directed at normalizing range of motion, strength, and function in activities of daily living. Progressive mobilization and strengthening are hallmarks of this phase. Neuromuscular training is begun and becomes the central component of rehabilitation. The advanced training phase focuses on preparing the patient for return to sports participation. Perturbation of support surfaces, agility drills, plyometrics, and sport-specific training are central components of this phase.
Conclusion:
The rehabilitation guidelines discussed may assist clinicians in managing syndesmotic ankle sprains.
Keywords: syndesmosis ankle sprain, distal tibiofibular sprain, syndesmosis instability, ankle rehabilitation
Syndesmotic ankle sprains (high ankle sprains) are a challenging lower extremity injury for athletes and sports health clinicians. Epidemiologic data suggest that syndesmotic ankle sprains account for 11% to 17% of the ankle sprains in athletic populations.15,24 Most of these injuries occur in collision sports such as American football, wrestling, ice hockey, rugby, and lacrosse. Fifty to seventy-five percent of the ankle sprains in some collision sports are classified as syndesmotic ankle injuries.13,28,46,59,64 The overall incidence of tibiofibular syndesmosis sprains in the general public is unclear. However, considering the epidemiologic data available on syndesmosis sprains and the fact that about 10 million ankle sprains occur in the United States each year, there is no doubt that the number is large.8,42 Interest in this injury and its treatment has grown due to several recent syndesmotic ankle sprains in high-profile collegiate and professional athletes. Although it may appear that high ankle sprains are becoming more prevalent, this perception is more likely a product of increased awareness than a true increase in the number of these injuries. The primary purpose of this article is to discuss current concepts in the rehabilitation of syndesmotic ankle sprains. We begin with a brief overview of tibiofibular syndesmosis anatomy, mechanisms of injury, assessment, and factors in determining surgical versus nonsurgical intervention because this information provides a framework for the discussion of rehabilitation. Detailed reviews of these background topics are available for a more comprehensive discussion of distal tibiofemoral syndesmosis injuries.4,18,40,54,63,66
Anatomy of the Distal Tibiofibular Syndesmosis
The distal tibiofibular syndesmosis is a complex of connective tissues that provide stability to the mortise of the talocrural (ankle) joint. The principal structures of this joint complex include the tibia, fibula, interosseous membrane, and 4 ligaments: the anterior inferior tibiofibular ligament, the posterior inferior tibiofibular ligament, the interosseous ligament, and the transverse tibiofibular ligament.4,16 The anterior and posterior inferior tibiofibular ligaments are strong ligaments that serve as primary stabilizers of the distal tibiofibular joint.45,49,65 The interosseous tibiofibular ligament is a thickening of the interosseous membrane about 10 to 15 mm proximal to the talocrural joint. Some have suggested that this ligament functions like a spring, allowing some medial-to-lateral splaying of the tibia and fibula during movement and loading.45 The transverse tibiofibular ligament is a deep portion of the posterior inferior tibiofibular ligament and posterior capsule that has a fibrocartilaginous appearance.4,16,45 The deltoid ligament serves as a secondary stabilizer to the distal ankle syndesmosis and may therefore be injured along with the syndesmotic connective tissues.4,16,55 Together, the connective tissue complex of the distal tibiofibular syndesmosis provides a strong and stable ankle mortise. It is then no surprise that significant injuries to this complex generally require high loads, such as those experienced in collision sports or high-velocity trauma. It is also not surprising that a large number of syndesmotic injuries involve fractures of the fibula or tibia.2
Mechanisms of Injury
Forceful external rotation of the foot and ankle is the most universally accepted mechanism of injury for syndesmotic ankle sprains.12,19,20,26 In this mechanism, the talus is positioned in the mortise when a high-magnitude external rotation moment causes the talus to separate the distal tibia and fibula. This is most commonly experienced (1) when an athlete rapidly pivots internally off a foot planted in external rotation, (2) when contact with another player applies a valgus load to the leg while the foot is planted, or (3) when a direct blow to the lateral aspect of the heel forces the foot and ankle of a kneeling or fallen athlete into external rotation (toward the ground).12,20,57 A less common mechanism of injury is hyperdorsiflexion.20,28,45 In this mechanism, the widest portion of the talus forcefully rotates into the ankle mortise. The superiorly directed load forces the distal tibia and fibula apart in much the same way a splitting mall or wedge forces firewood to split apart. A number of other less common mechanisms of injury have been reported, including straight eversion,36,45 inversion of the ankle with a plantar flexed foot,28,31,58 and internal rotation of the foot and ankle complex.58 Risk factors associated with syndesmotic ankle sprains include participation in collision sports24,46; wearing rigid boots, as in skiing and ice hockey22,64; and a planovalgus (flat) foot alignment,63 which increases the likelihood of an externally rotated foot alignment when the foot is planted.
Assessment
The patient’s report of the injury, description of symptoms, and presentation usually provide a high suspicion of syndesmotic ankle sprain. Most are unable to ambulate after injury without the use of crutches. Increased pain and instability are typically experienced if the patient attempts to push off the toes or pivot inward with the foot planted. The amount of edema is variable. Sprains that are isolated to the distal tibiofibular ligaments often have a relatively small pocket of swelling over the syndesmotic ligaments, whereas more extensive injuries involving tears of the interosseous membrane and/or deltoid ligament often have substantial swelling of the ankle and/or distal leg (Figure 1).
Figure 1.

An acute ankle injury including a tibiofibular syndesmosis sprain. Note the edema and ecchymosis in the region of the distal tibiofibular syndesmosis and extending up the leg. Acute tenderness to palpation was present over the syndesmosis, and it extended approximately 6 in. (15 cm) superiorly over the interosseous membrane.
Most patients exhibit point tenderness over the anterior or posterior inferior tibiofibular ligaments. This tenderness may extend up the leg when the interosseous membrane is involved. Nussbaum and coworkers46 reported that there is a significant association between how far tenderness extends up the leg and how much time is lost from competition in sports. Tenderness may also be observed over the deltoid ligament or the lateral ankle ligaments because these structures are frequently injured at the same time as the syndesmosis. It is also important to assess the integrity of the fibula and tibia given that fractures of one or both of these bones can accompany syndesmosis injuries.2,20,36
Several clinical tests for syndesmotic instability have been described (Table 1). Each test is designed to apply stress to the connective tissues of the distal tibiofibular syndesmosis through manual loading or by having the patient perform a task that results in similar loading patterns. Beumer and coworkers7 performed a biomechanical analysis of a subset of these manual stress tests and determined that, with the exception of the external rotation stress test, the small displacements associated with these tests makes it unlikely that they can distinguish widening of the mortise with a syndesmotic injury from that of a normal syndesmosis. The authors recommended that examiners consider the amount of pain during these tests as an indication of syndesmosis involvement rather than attempt to assess the extent of widening or injury.7 A biomechanical study of the squeeze test by Teitz and Harrington60 provides further support for this approach. Alonso and coworkers1 assessed the reliability of manual stress tests for syndesmotic ankle sprains and the ability of these tests to predict return to function, and they found that only the external rotation stress test had good reliability and was predictive of the time that it took to return to function. Williams et al63 recently described the stabilization test in which the patient is asked to perform a series of functional tasks (heel raise, walk, run, and/or vertical hop) before and after athletic tape is applied circumferentially around the distal tibiofibular joint (Figure 2). This test is unique in that it attempts to stabilize the distal syndesmosis and thereby reduce symptoms associated with instability rather than reproduce the symptoms by applying stress to the joint. The test result is positive if the patient’s symptoms are significantly reduced when performing the tasks while taped. Besides being used diagnostically after injury, clinical tests are important to rehabilitation specialists when assessing healing and patients’ readiness for progression during the rehabilitation.
Table 1.
Stress tests for distal tibiofibular syndesmosis sprains.
| Stress Test | Description |
|---|---|
| Cotton17 | The talus is translated from medial to lateral in the ankle mortise. The test result is positive if there is excessive motion (compared to that of the opposite side) or pain. |
| Crossed leg35 | The patient sits with the middle of the injured leg across the top of the opposite knee. Pressure is applied to the medial aspect of the proximal tibia and fibula at or near the knee to apply shear strain to the distal syndesmosis ligaments. The test result is positive if there is pain at the distal tibiofibular joint. This is essentially a functional squeeze test performed by the patient. |
| External rotation12 | The patient sits over the side of a examination table with the knee in approximately 90° of flexion. The examiner stabilizes the leg midway of the tibial shaft and applies an external rotation moment at the ankle. The test result is positive if there is pain in the region of the distal syndesmosis ligaments or interosseous membrane. |
| Fibular translation48 | The fibula is translated in an anteroposterior direction. The test result is positive with pain in the region of the distal tibiofibular syndesmosis. |
| Squeeze28 | The tibia and fibula are compressed midway up the leg to apply shear strain to the distal syndesmosis ligaments. The test result is positive if there is pain at the distal tibiofibular joint. |
Figure 2.

Taping used in the syndesmosis stabilization test.64 Patients perform heel raises, walking, running, and vertical hopping (if possible) before and after 1.5-in. (3.8-cm) athletic tape is circumferentially applied over the tibiofibular syndesmosis to provide joint stability. The test result is positive if the patient’s complaints of pain and/or instability in the region of the distal syndesmosis are relieved with the taping.
Imaging
Imaging is important when assessing syndesmotic ankle sprains because there is a range of pathology that can present with these injuries. Imaging results are also important to the rehabilitation specialist because they provide important information regarding the severity of the injury, issues that can affect recovery and rehabilitation progression, and insight on the health status of the joint (long-term prognosis). This knowledge helps the rehabilitation specialist when planning treatment and discussing the injury and expectations with a patient.
Radiographs are used to assess bony integrity and the stability of the ankle mortise. Typical views used to assess the joint include a weightbearing anteroposterior view, a mortise view, and a lateral view. Although stress radiographs have classically been defined as a method of assessing syndesmotic stability, work by Beumer and colleagues,5 using radiostereometry and serial cutting of the syndesmotic ligaments, suggests that stress radiographs probably offer little advantage over plain views in assessing syndesmotic stability.
Magnetic resonance imaging (MRI) has been shown to be highly sensitive and specific to injuries of the distal tibiofibular ligaments, and it has demonstrated excellent agreement among raters.47,61 Moreover, MRI provides insight into the extent of ankle injury and helps to identify concomitant injuries to other structures in the region. In a retrospective review that included 59 patients with acute or chronic syndesmotic ankle sprains, Brown and coworkers14 found a high prevalence of other lesions, including anterior talofibular ligament sprains, bone bruises, and osteochondral lesions. To date, there are no reports that have assessed the association between the extent of lesions on imaging and clinical presentation or long-term outcomes. Hence, it is unclear if MRI findings are prognostic of recovery time and outcomes. Research defining the clinical significance of imaging results is required before conclusions can be drawn on whether routine MRI is cost-beneficial in the management of syndesmotic ankle sprains.
Differential Diagnosis
The differential diagnosis of acute syndesmotic ankle sprains includes Maisonneuve fracture, Weber fractures (type B and C), deltoid ligament sprain, and lateral ankle sprain.2,20,36,47 A number of other injuries can accompany syndesmosis sprains, including bone bruises and osteochondral lesions of the distal tibiofibular joint or talus.14 In patients presenting with chronic pain after syndesmotic ankle sprain, the differential diagnosis includes latent syndesmotic instability, scarring within the syndesmosis, impingement of the distal fascicle of the anterior inferior tibiofibular ligament, heterotopic ossification in the region of the syndesmosis, osteoarthritis, and osteochondral lesions of the distal tibia, fibula, or talar dome (S. Mosier-LaClair, H. Pike, G. Pomeroy, unpublished data, 2000).3,4,12,14,48,53,58 Knowledge of these differential diagnoses, comorbidities, and common sequelae are important to the rehabilitation specialist because they are frequently encountered when treating patients with syndesmosis injuries.
Nonsurgical Versus Surgical Management
Surgery is indicated when there is frank instability based on a disruption of normal tibiofibular relationships on radiographs. Radiographic measurements of the lower extremities of fresh cadavers have established the following “normal” tibiofibular relationships (95% confidence intervals): (1) a tibiofibular clear space of ≤ 6 mm on anteroposterior and mortise views and (2) tibiofibular overlap of at least 6 mm or 42% of the fibular width on the anteroposterior view and 1 mm on the mortise view.27 Although these tibiofibular relationships are widely accepted in the orthopaedic community, there is evidence challenging the clinical importance of these relationships.6,44 In addition to radiographic evidence of syndesmosis instability, indications for surgical treatment include the presence of fracture requiring fixation in the absence of instability or evidence of other surgically treatable lesions, such as a repairable syndesmotic ligament tear, latent instability, scarring within the syndesmosis, and calcification in the syndesmosis, which are common causes of chronic pain after syndesmosis sprains.2,12,20,58,63 Frank tibiofibular instability is rare in syndesmosis sprains without an accompanying fracture.59 Nonsurgical management is usually prescribed for most other clinical presentations. It is unclear if a larger percentage of people who sustain syndesmotic sprains would benefit from surgical treatment. The high incidence of chronic pain, instability, and functional limitations after high ankle sprain and the excellent surgical success rates suggest that this may be the case.24,59,63 Arthroscopy directed at assessing and treating undiagnosed instability or other syndesmotic pathology is often helpful in patients who are making especially slow progress in rehabilitation. Rehabilitation after surgery is similar to that used in nonsurgical management but generally progresses more slowly and includes a longer period of reduced weightbearing with immobilization in either a weightbearing cast or walking boot. Taylor and coworkers,59 however, recently reported excellent results using a rehabilitation program involving early weightbearing and mobilization in a small sample of patients who underwent surgical fixation.
Rehabilitation
We are unaware of any randomized clinical trials or case control studies that specifically investigate conservative management of syndesmotic ankle sprains. Current rehabilitation guidelines for syndesmosis ankle sprains are largely based on clinical experience; hence, our current approach (as discussed in this article) is largely based on clinical experience and a few case series (ie, Level 4 and 5 evidence).13,24,40,46,63 Most of the treatment principles employed are similar to those used in treating patients with lateral ankle sprains but with adaptations that take into account the unique anatomy, physiology, and pathomechanics associated with syndesmosis injuries. A recent survey of professionals who frequently treat high-level athletes with syndesmotic ankle sprains suggests that current management of high ankle sprains includes a range of rehabilitation approaches that extends from treating people with this injury exactly the same as those with lateral ankle sprains to treating all patients diagnosed with distal tibiofibular syndesmosis sprains with 4 to 6 weeks of nonweightbearing ambulation with the joint immobilized in a cast or boot (Foster and Williams, unpublished data, 2005). Each rehabilitation program for acute syndesmotic ankle sprains currently described in the peer-reviewed literature is either a 3- or 4-phase program with time- or criterion-based progression.13,24,40,46,63
Our Preferred Approach
The 3-phase approach described in Table 2 provides a general framework for treatment progression; however, treatment is tailored to the individual patient’s presentation, goals, and circumstances because these factors are highly variable. Patients are carefully monitored with frequent discussion of symptoms and concerns, observation of task performance during rehabilitation, and regular assessment using palpation, the external rotation test, and the stabilization test. The information gained from this monitoring assists the rehabilitation specialist in tailoring the approach to the patient.
Table 2.
Three-phase rehabilitation program.
| Rehabilitation Phase | Goals, Sample Treatments, and Criteria for Progression |
|---|---|
| Acute | Goal: Joint protection while minimizing pain, inflammation, weakness, and loss of motion. |
| Joint protection: Immobilization in a walking cast, boot, custom orthosis, lace-up ankle brace, or ankle stirrup. External rotation and end-range dorsiflexion are avoided. | |
| Weightbearing: Based on assessment and patient symptoms—varies from nonweightbearing to full weightbearing. | |
| Pain and inflammation control: Compression, elevation, cryotherapy, electrical stimulation, manual therapy, other modalities, and/or alternative therapies such as acupuncture. | |
| Maintenance of strength and mobility: Gentle motion, cycle ergometer, progressive resistance exercise with bands, cords, ankle weights, and/or electrical stimulation. | |
| Progressed when: Able to ambulate in full weightbearing on various surfaces and traverse stairs with minimal discomfort. | |
| Subacute | Goal: Normalize joint mobility, strength, neuromuscular control, and return to basic function in activities of daily living. |
| Mobility: Low-load, long-duration stretching with cords, bands, or towels; repetitive motion through the range of motion; cycle ergometer; joint mobilization; and/or aquatic therapy. | |
| Strengthening: Cords, bands, ankle weights, heel raises, step up/down, calf press with isotonic equipment, and/or neuromuscular training exercises. | |
| Neuromuscular training: Progressive use of air cushions, rocker boards, wobble boards, air-filled domes, trampolines, or other perturbation of support surfaces. | |
| Progressed when: Can jog and hop with minimal discomfort. | |
| Advanced training | Goal: Prepare for return to sports participation. |
| Neuromuscular training: Perturbation of support surfaces. | |
| Functional/agility drills: Running, jumping rope, hopping, shuffling, carioca, and/or figure-8 running with or without use of props such as cones, hurdles, and ladders. | |
| Strength/power: Advanced strengthening, plyometrics. | |
| Sports-specific drills: Dribbling drills, running reception patterns, shooting balls, skating/rollerblading. | |
| Return to sports when: Performs sport tasks at game speed with minimal discomfort and quality movement. |
Acute Phase
The primary goal of the acute phase of rehabilitation is to protect the healing joint while minimizing pain, inflammation, muscle weakness, and loss of joint motion. Protection is provided by restricting joint movement in directions that may strain healing ligaments and by modulating weightbearing. An orthosis that provides stability to the syndesmosis joint is usually prescribed to help achieve this goal.11,32,38 The directions of motion restriction and degree of immobilization depend on the physical exam and presentation. Limiting external rotation is usually the primary concern. Most orthoses provide some restraint to external rotation moments. Casts, walking boots, and custom orthoses designed to limit external rotation provide the greatest protection, whereas ankle stirrups, athletic tape, and lace-up ankle braces provide less syndesmosis stabilization. The decision on which orthosis to use is usually made by the attending physician. This tailored approach is preferred over a standardized protocol involving complete immobilization and restricted weightbearing. Some clinicians recommend limiting dorsiflexion with a posterior splint or heel lift, but this is typically unnecessary in our experience. In theory, the syndesmosis must be able to accept the anterior portion of the talus in dorsiflexion for normal range of motion to return. Hence, strictly restricting dorsiflexion can be counterproductive. Allowing dorsiflexion through the full range of motion is usually helpful, providing that forceful and ballistic dorsiflexion are avoided.
Most people who experience syndesmotic ankle sprains are unable to bear their full weight during gait and therefore require the use of an assistive device such as crutches. Weightbearing guidelines are based on a patient’s symptoms and the overall picture provided by the injury event, physical examination, and imaging. Some people with relatively minor complaints are able to ambulate with full weightbearing, but most use crutches with weightbearing as tolerated. People with more severe injuries are often treated with a short period of more restricted weightbearing (1 to 2 weeks). Weightbearing is progressed toward full weightbearing based on the patient’s symptoms and exam. Full weightbearing is encouraged when patients are able to ambulate on various surfaces and ascend/descend stairs with minimal discomfort.
The methods of protecting the joint described above aid in limiting pain and inflammation. Several other therapies can be prescribed to address pain and inflammation. Tissue compression, cryotherapy, and elevation are usually applied together. Cryotherapy is used to reduce pain, whereas compression and elevation are used to limit edema and effusion, which may further assist with pain control.9,10,43 Pain and anti-inflammatory medications are often prescribed.21,52,56 Other treatments used more selectively include transcutaneous electric nerve stimulation,30,39 soft tissue massage directed at “milking” edema from the foot and ankle,25 and manual therapy (joint mobilization).23 Some athletes find alternative therapies such as acupressure and acupuncture to be helpful in relieving pain as well.34,37
Resistance exercise is prescribed early in the recovery period to minimize muscle atrophy and weakness. Although muscles demonstrating weakness62 or activation failure50,51 are the primary focus (usually, the triceps surae or peroneal musculature), each major group about the ankle joint is addressed to maintain muscle strength. Strengthening may be performed using a variety of exercise approaches, including elastic resistance bands or cords, ankle weights, or heel raise exercises. Elastic resistance bands are especially well suited for home use. When strict immobilization or nonweightbearing ambulation is prescribed, isometric strengthening and neuromuscular electrical stimulation are recommended to help minimize muscle atrophy and weakness. Exercise is performed in accordance with the previously described joint protection guidelines given that promotion of healing is the primary goal of this phase of treatment. Movement into external rotation and endrange dorsiflexion is usually avoided during rehabilitation in this phase. Exercise doses are prescribed in a manner that is specific to each patient. Patients are progressed to the subacute phase of treatment when they discontinue use of assistive devices in ambulation.
Subacute Phase
The goal of the subacute phase is to normalize range of motion, strength, gait, and function in the patient’s activities of daily living. Progressive mobilization and strengthening in the pain-free range of motion are the hallmarks of this phase. Forceful external rotation and dorsiflexion continue to be avoided; however, patients should be moving through the full range of motion by the end of this phase. Joint mobility is facilitated with the use of elastic resistance bands or cords, towels, and the controlled use of body weight. A cycle ergometer is an effective means of providing mobilization while increasing tissue perfusion and activating the musculature of the region. Low-load, long-duration stretching that gently promotes tissue creep and joint mobilization is effective when stiffness is present. Manual joint mobilization should be performed in a manner that applies little strain to the healing syndesmotic connective tissues.23 If aquatic therapy or a whirlpool is available, aquatic exercise can be used to mobilize the ankle joint in a safe environment that most patients find beneficial and pleasant.33
The use of elastic resistance or ankle weights continues to be the primary form of strengthening early in this phase. Later in the subacute phase, strengthening is accomplished using heel raises, forward and lateral stepping exercises, and calf presses using isotonic weight machines or isokinetic devices. Exercise is dosed with lower weight and higher repetitions early in the phase and so progresses to higher-intensity, low-repetition sets directed at increasing strength and muscle size. Neuromuscular training is performed through balance exercises on unstable surfaces, such as air cushions, wobble boards, rocker boards, and air-filled domes (Figure 3).67,68 Early in the phase, these exercises are performed in double-leg stance. The patient transitions to single-leg stance when control is demonstrated. These balance training exercises are performed with the knee extended or nearly extended so that the dominant balance strategy is centered about the ankle. Support surfaces advance from highly stable to less stable as the patient’s strength, endurance, and control increases. Having the patient perform exercise with the eyes closed and requiring the patient to place attention on other tasks such as counting backwards or catching/dribbling a ball further challenges the neuromuscular system. Neuromuscular training exercises such as those described above are used instead of traditional strengthening exercises in patients who have little evidence of muscle atrophy or weakness. However, in those with clear evidence of atrophy and weakness, a combined approach is recommended, including high-intensity strengthening and progressive neuromuscular training. The external rotation stress test12 and the stabilization test63 can be used to assess healing and the patient’s readiness for more advanced exercise, such as jogging and hopping. Careful monitoring and clear communication regarding the presence of pain, postexercise edema, or perception of instability are important in exercise prescription and determining readiness for progression. Patients are progressed to the advanced training phase when they are able to jog and perform a series of hops without pain.
Figure 3.
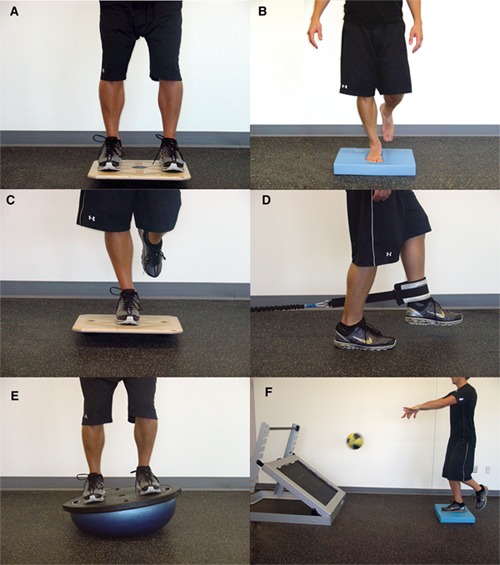
A sample progression of neuromuscular training exercises in the subacute phase of rehabilitation: A, double-leg balance on a balance board; B, single-leg balance on an air cushion; C, single-leg balance on a balance board; D, single-leg resistive cord exercises in which perturbation is applied via resisted movement of the opposite leg; E, double-leg weight shifts on a balance dome; F, throwing a weighted ball against a rebounder while balancing on one leg on an air cushion.
Advanced Training Phase
The goal of the advanced training phase is to prepare the patient for return to full activity in sports or activities of choice. More advanced neuromuscular training, agility drills, and sport-specific tasks are the central components of this phase.41,67,68 Exercises commonly used during this phase of rehabilitation include perturbation of support surfaces, jumping rope, hopping (forward, backward, and laterally), running, shuffling, and agility drills, such as carioca or running figure-8 patterns (Figure 4). Exercises begin slow, with movement in a single direction, and progressively become more quick, intense, and dynamic. Athletic tape or a lace-up ankle brace is usually used to support the joint. Props such as cones, hurdles, ladders, and other devices can be used to advance the difficulty of the exercises. Power is trained through bounding, box jumping, and other plyometric training with athletes whose sports participation involves explosive movement.29 As the patient approaches return to sport, sport-specific drills such as dribbling a basketball or a soccer ball, running football reception patterns, or sprinting with quick changes in direction are performed in a progressive fashion. Athletes are monitored for quality of movement and symptoms of pain or instability throughout this process. The patient is ready for return to sport when he or she can perform sport-specific tasks at game speed with good movement quality and little to no pain or instability.
Figure 4.
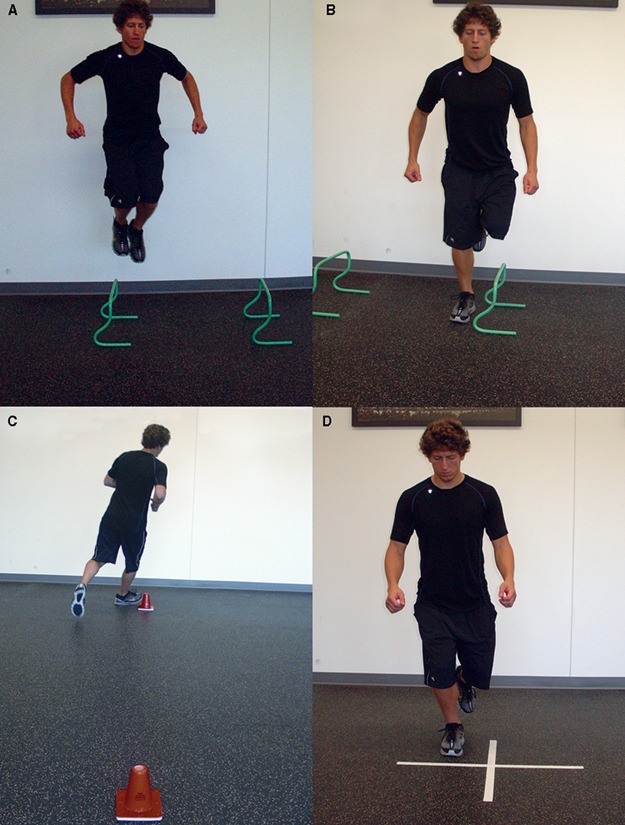
An example progression of functional/agility training exercises in the advanced training phase of rehabilitation: A, jumping over hurdles; B, hopping over hurdles; C, timed figure-8 running; and D, timed 4-square hop test.
Outcomes
The recovery period after syndesmotic ankle sprains is highly variable. One of the perplexing things about this injury is that some people who initially appear to have relatively minor injuries have protracted recovery periods, whereas others that appear to have more severe injuries progress quite rapidly. This suggests that current assessment methods are limited in their sensitivity with respect to injury severity. Overall, people who sustain syndesmotic ankle sprains typically experience much longer recovery periods than do those who sustain lateral ankle sprains.12,24,28,64 This fact and the variability in recovery periods are important issues to discuss with individuals who sustain syndesmosis injuries. Hopkinson and coworkers28 reported that individuals with syndesmotic ankle sprains required an average of 55 days to return to full activity, which was twice as long as those with grade III lateral ankle sprains. Wright and colleagues’ report64 of syndesmotic ankle sprains in National Hockey League players supports this length of recovery; players in their study averaged 45 days to return to game play (range, 6 to 137 days). Boytim and coworker’s report12 of syndesmotic ankle sprains in National Football League players provides a somewhat more optimistic picture, given that players in their study missed only 6.3 practices (range, 2 to 21) in comparison to an average of 1.1 (range, 0 to 12) for those with lateral ankle sprains. However, players with high ankle sprains required about 3 times as many treatments as those with lateral sprains. Chronic ankle dysfunction (pain, instability, and functional limitations) is common after this injury. Gerber et al24 reported that regardless of initial grade of injury severity, people who sustained syndesmosis sprains had a high incidence (more than 60%) of chronic ankle pain, instability, and limitations in hopping when evaluated 6 months after injury. However, all returned to sports participation despite their reports of chronic ankle disability.
Summary
Syndesmotic ankle sprains account for 11% to 17% of all ankle sprains in athletic populations. Most of these injuries occur in collision sports such as American football, ice hockey, rugby, lacrosse, and wrestling. Few people who sustain syndesmosis sprains without fractures have radiographic evidence of tibiofibular syndesmosis instability. Consequently, most syndesmotic ankle sprains are treated nonsurgically with a rehabilitation program. There are currently no randomized clinical trials or case control studies to guide rehabilitation. Our preferred approach involves a 3-phase program. The first phase is directed at promoting healing by protecting the joint while minimizing pain, inflammation, muscle weakness, and loss of motion. Patients transition from this acute phase to the subacute phase of rehabilitation when they are able to ambulate in full weightbearing with minimal discomfort. The subacute phase of rehabilitation is directed at normalizing range of motion, strength, gait, and basic function in the patient’s activities of daily living. Patients progress to the advanced training phase when they are able to jog and hop without pain or instability. The advanced training phase focuses on preparing the patient to return to sports participation or his or her activities of choice. Athletes are allowed to return to sport when they can perform their sport-specific tasks at game speed with good movement quality and no significant complaints of pain or instability. Evidence suggests that syndesmosis sprains typically require 6 to 8 weeks for recovery, but this is variable. Chronic pain, instability, and functional limitations are common after syndesmosis sprains. Future research should focus on developing more sensitive and specific physical examination methods, assessing the predictive value of imaging after injury, and evaluating the most appropriate treatment approaches for the various presentations of syndesmotic ankle sprains.
Footnotes
No potential conflict of interest declared.
References
- 1. Alonso A, Khoury L, Adams R. Clinical tests for ankle syndesmosis injury: reliability and prediction of return to function. J Orthop Sports Phys Ther. 1998;27(4):276-284 [DOI] [PubMed] [Google Scholar]
- 2. Amendola A. Controversies in diagnosis and management of syndesmosis injuries of the ankle. Foot Ankle. 1992;13(1):44-50 [DOI] [PubMed] [Google Scholar]
- 3. Bassett FH, 3rd, Gates HS, 3rd, Billys JB, Morris HB, Nikolaou PK. Talar impingement by the anteroinferior tibiofibular ligament: a cause of chronic pain in the ankle after inversion sprain. J Bone Joint Surg Am. 1990;72(1):55-59 [PubMed] [Google Scholar]
- 4. Beumer A. Chronic instability of the anterior syndesmosis of the ankle. Acta Orthop Suppl. 2007;78(327):4-36 [PubMed] [Google Scholar]
- 5. Beumer A, Valstar ER, Garling EH, et al. External rotation stress imaging in syndesmotic injuries of the ankle: comparison of lateral radiography and radiostereometry in a cadaveric model. Acta Orthop Scand. 2003;74(2):201-205 [DOI] [PubMed] [Google Scholar]
- 6. Beumer A, van Hemert WL, Niesing R, et al. Radiographic measurement of the distal tibiofibular syndesmosis has limited use. Clin Orthop Relat Res. 2004;423:227-234 [DOI] [PubMed] [Google Scholar]
- 7. Beumer A, van Hemert WL, Swierstra BA, Jasper LE, Belkoff SM. A biomechanical evaluation of clinical stress tests for syndesmotic ankle instability. Foot Ankle Int. 2003;24(4):358-363 [DOI] [PubMed] [Google Scholar]
- 8. Birrer RB, Fani-Salek MH, Totten VY, Herman LM, Politi V. Managing ankle injuries in the emergency department. J Emerg Med. 1999;17(4):651-660 [DOI] [PubMed] [Google Scholar]
- 9. Bleakley C, McDonough S, MacAuley D. The use of ice in the treatment of acute soft-tissue injury: a systematic review of randomized controlled trials. Am J Sports Med. 2004;32(1):251-261 [DOI] [PubMed] [Google Scholar]
- 10. Bleakley CM, McDonough SM, MacAuley DC, Bjordal J. Cryotherapy for acute ankle sprains: a randomised controlled study of two different icing protocols. Br J Sports Med. 2006;40(8):700-705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Boyce SH, Quigley MA, Campbell S. Management of ankle sprains: a randomised controlled trial of the treatment of inversion injuries using an elastic support bandage or an Aircast ankle brace. Br J Sports Med. 2005;39(2):91-96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Boytim MJ, Fischer DA, Neumann L. Syndesmotic ankle sprains. Am J Sports Med. 1991;19(3):294-298 [DOI] [PubMed] [Google Scholar]
- 13. Brosky T, Nyland J, Nitz A, Caborn DN. The ankle ligaments: consideration of syndesmotic injury and implications for rehabilitation. J Orthop Sports Phys Ther. 1995;21(4):197-205 [DOI] [PubMed] [Google Scholar]
- 14. Brown KW, Morrison WB, Schweitzer ME, Parellada JA, Nothnagel H. MRI findings associated with distal tibiofibular syndesmosis injury. AJR Am J Roentgenol. 2004;182(1):131-136 [DOI] [PubMed] [Google Scholar]
- 15. Cedell CA. Ankle lesions. Acta Orthop Scand. 1975;46(3):425-445 [PubMed] [Google Scholar]
- 16. Close JR. Some applications of the functional anatomy of the ankle joint. J Bone Joint Surg Am. 1956;38(4):761-781 [PubMed] [Google Scholar]
- 17. Cotton FJ. Dislocations and Joint-Fractures. Philadelphia, PA: WB Saunders & Co; 1911:535-588 [Google Scholar]
- 18. Dattani R, Patnaik S, Kantak A, Srikanth B, Selvan TP. Injuries to the tibiofibular syndesmosis. J Bone Joint Surg Br. 2008;90(4):405-410 [DOI] [PubMed] [Google Scholar]
- 19. Doughtie M. Syndesmotic ankle sprains in football: A survey of National Football League athletic trainers. J Athl Train. 1999;34(1):15-18 [PMC free article] [PubMed] [Google Scholar]
- 20. Edwards GS, Jr, DeLee JC. Ankle diastasis without fracture. Foot Ankle. 1984;4(6):305-312 [DOI] [PubMed] [Google Scholar]
- 21. Ekman EF, Fiechtner JJ, Levy S, Fort JG. Efficacy of celecoxib versus ibuprofen in the treatment of acute pain: a multicenter, double-blind, randomized controlled trial in acute ankle sprain. Am J Orthop (Belle Mead NJ). 2002;31(8):445-451 [PubMed] [Google Scholar]
- 22. Fritschy D. An unusual ankle injury in top skiers. Am J Sports Med. 1989;17(2):282-285 [DOI] [PubMed] [Google Scholar]
- 23. Fujii M, Suzuki D, Uchiyama E, et al. Does distal tibiofibular joint mobilization decrease limitation of ankle dorsiflexion? Man Ther. 2010;15(1):117-121 [DOI] [PubMed] [Google Scholar]
- 24. Gerber JP, Williams GN, Scoville CR, Arciero RA, Taylor DC. Persistent disability associated with ankle sprains: a prospective examination of an athletic population. Foot Ankle Int. 1998;19(10):653-660 [DOI] [PubMed] [Google Scholar]
- 25. Goats GC. Massage: the scientific basis of an ancient art. Part 2: physiological and therapeutic effects. Br J Sports Med. 1994;28(3):153-156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Guise ER. Rotational ligamentous injuries to the ankle in football. Am J Sports Med. 1976;4(1):1-6 [DOI] [PubMed] [Google Scholar]
- 27. Harper MC, Keller TS. A radiographic evaluation of the tibiofibular syndesmosis. Foot Ankle. 1989;10(3):156-160 [DOI] [PubMed] [Google Scholar]
- 28. Hopkinson WJ, Pierre P, Ryan JB, Wheeler JH. Syndesmosis sprains of the ankle. Foot Ankle. 1990;10(6):325-330 [DOI] [PubMed] [Google Scholar]
- 29. Ismail MM, Ibrahim MM, Youssef EF, El Shorbagy KM. Plyometric training versus resistive exercises after acute lateral ankle sprain. Foot Ankle Int. 2010;31(6):523-530 [DOI] [PubMed] [Google Scholar]
- 30. Kara M, Ozcakar L, Gokcay D, et al. Quantification of the effects of transcutaneous electrical nerve stimulation with functional magnetic resonance imaging: a double-blind randomized placebo-controlled study. Arch Phys Med Rehabil. 2010;91(8):1160-1165 [DOI] [PubMed] [Google Scholar]
- 31. Katznelson A, Lin E, Militiano J. Ruptures of the ligaments about the tibio-fibular syndesmosis. Injury. 1983;15(3):170-172 [DOI] [PubMed] [Google Scholar]
- 32. Kerkhoffs GM, Struijs PA, Marti RK, Assendelft WJ, Blankevoort L, van Dijk CN. Different functional treatment strategies for acute lateral ankle ligament injuries in adults. Cochrane Database Syst Rev. 2002;3:CD002938 [DOI] [PubMed] [Google Scholar]
- 33. Kim E, Kim T, Kang H, Lee J, Childers MK. Aquatic versus land-based exercises as early functional rehabilitation for elite athletes with acute lower extremity ligament injury: a pilot study. PM R. 2010;2(8):703-712 [DOI] [PubMed] [Google Scholar]
- 34. Kim HY, Koo ST, Kim JH, An K, Chung K, Chung JM. Electroacupuncture analgesia in rat ankle sprain pain model: neural mechanisms. Neurol Res. 2010;32(suppl 1):10-17 [DOI] [PubMed] [Google Scholar]
- 35. Kiter E, Bozkurt M. The crossed-leg test for examination of ankle syndesmosis injuries. Foot Ankle Int. 2005;26(2):187-188 [DOI] [PubMed] [Google Scholar]
- 36. Kleiger B. The mechanism of ankle injuries. J Bone Joint Surg Am. 1956;38(1):59-70 [PubMed] [Google Scholar]
- 37. Koo ST, Park YI, Lim KS, Chung K, Chung JM. Acupuncture analgesia in a new rat model of ankle sprain pain. Pain. 2002;99(3):423-431 [DOI] [PubMed] [Google Scholar]
- 38. Lamb SE, Marsh JL, Hutton JL, Nakash R, Cooke MW. Mechanical supports for acute, severe ankle sprain: a pragmatic, multicentre, randomised controlled trial. Lancet. 2009;373(9663):575-581 [DOI] [PubMed] [Google Scholar]
- 39. Lanham RH, Jr, Powell S, Hendrix BE. Efficacy of hypothermia and transcutaneous electrical nerve stimulation in podiatric surgery. J Foot Surg. 1984;23(2):152-158 [PubMed] [Google Scholar]
- 40. Lin CF, Gross ML, Weinhold P. Ankle syndesmosis injuries: anatomy, biomechanics, mechanism of injury, and clinical guidelines for diagnosis and intervention. J Orthop Sports Phys Ther. 2006;36(6):372-384 [DOI] [PubMed] [Google Scholar]
- 41. Linford CW, Hopkins JT, Schulthies SS, Freland B, Draper DO, Hunter I. Effects of neuromuscular training on the reaction time and electromechanical delay of the peroneus longus muscle. Arch Phys Med Rehabil. 2006;87(3):395-401 [DOI] [PubMed] [Google Scholar]
- 42. Lynch SA, Renstrom PA. Treatment of acute lateral ankle ligament rupture in the athlete: conservative versus surgical treatment. Sports Med. 1999;27(1):61-71 [DOI] [PubMed] [Google Scholar]
- 43. Mac Auley DC. Ice therapy: how good is the evidence? Int J Sports Med. 2001;22(5):379-384 [DOI] [PubMed] [Google Scholar]
- 44. Nielson JH, Gardner MJ, Peterson MG, et al. Radiographic measurements do not predict syndesmotic injury in ankle fractures: an MRI study. Clin Orthop Relat Res. 2005;436:216-221 [DOI] [PubMed] [Google Scholar]
- 45. Norkus SA, Floyd RT. The anatomy and mechanisms of syndesmotic ankle sprains. J Athl Train. 2001;36(1):68-73 [PMC free article] [PubMed] [Google Scholar]
- 46. Nussbaum ED, Hosea TM, Sieler SD, Incremona BR, Kessler DE. Prospective evaluation of syndesmotic ankle sprains without diastasis. Am J Sports Med. 2001;29(1):31-35 [DOI] [PubMed] [Google Scholar]
- 47. Oae K, Takao M, Naito K, et al. Injury of the tibiofibular syndesmosis: value of MR imaging for diagnosis. Radiology. 2003;227(1):155-161 [DOI] [PubMed] [Google Scholar]
- 48. Ogilvie-Harris DJ, Reed SC. Disruption of the ankle syndesmosis: diagnosis and treatment by arthroscopic surgery. Arthroscopy. 1994;10(5):561-568 [DOI] [PubMed] [Google Scholar]
- 49. Ogilvie-Harris DJ, Reed SC, Hedman TP. Disruption of the ankle syndesmosis: biomechanical study of the ligamentous restraints. Arthroscopy. 1994;10(5):558-560 [DOI] [PubMed] [Google Scholar]
- 50. Palmieri-Smith RM, Hopkins JT, Brown TN. Peroneal activation deficits in persons with functional ankle instability. Am J Sports Med. 2009;37(5):982-988 [DOI] [PubMed] [Google Scholar]
- 51. Palmieri RM, Ingersoll CD, Hoffman MA, et al. Arthrogenic muscle response to a simulated ankle joint effusion. Br J Sports Med. 2004;38(1):26-30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Petrella R, Ekman EF, Schuller R, Fort JG. Efficacy of celecoxib, a COX-2-specific inhibitor, and naproxen in the management of acute ankle sprain: results of a double-blind, randomized controlled trial. Clin J Sport Med. 2004;14(4):225-231 [DOI] [PubMed] [Google Scholar]
- 53. Pritsch M, Lokiec F, Sali M, Velkes S. Adhesions of distal tibiofibular syndesmosis: a cause of chronic ankle pain after fracture. Clin Orthop Relat Res. 1993;289:220-222 [PubMed] [Google Scholar]
- 54. Rammelt S, Zwipp H, Grass R. Injuries to the distal tibiofibular syndesmosis: an evidence-based approach to acute and chronic lesions. Foot Ankle Clin. 2008;13(4):611-633 [DOI] [PubMed] [Google Scholar]
- 55. Rasmussen O, Kromann-Andersen C, Boe S. Deltoid ligament: functional analysis of the medial collateral ligamentous apparatus of the ankle joint. Acta Orthop Scand. 1983;54(1):36-44 [DOI] [PubMed] [Google Scholar]
- 56. Slatyer MA, Hensley MJ, Lopert R. A randomized controlled trial of piroxicam in the management of acute ankle sprain in Australian Regular Army recruits: the Kapooka Ankle Sprain Study. Am J Sports Med. 1997;25(4):544-553 [DOI] [PubMed] [Google Scholar]
- 57. Slawski DP, West OC. Syndesmotic ankle injuries in rodeo bull riders. Am J Orthop. 1997;26(11):794-797 [PubMed] [Google Scholar]
- 58. Taylor DC, Englehardt DL, Bassett FH., 3rd Syndesmosis sprains of the ankle: the influence of heterotopic ossification. Am J Sports Med. 1992;20(2):146-150 [DOI] [PubMed] [Google Scholar]
- 59. Taylor DC, Tenuta JJ, Uhorchak JM, Arciero RA. Aggressive surgical treatment and early return to sports in athletes with grade III syndesmosis sprains. Am J Sports Med. 2007;35(11):1833-1838 [DOI] [PubMed] [Google Scholar]
- 60. Teitz CC, Harrington RM. A biochemical analysis of the squeeze test for sprains of the syndesmotic ligaments of the ankle. Foot Ankle Int. 1998;19(7):489-492 [DOI] [PubMed] [Google Scholar]
- 61. Vogl TJ, Hochmuth K, Diebold T, et al. Magnetic resonance imaging in the diagnosis of acute injured distal tibiofibular syndesmosis. Invest Radiol. 1997;32(7):401-409 [DOI] [PubMed] [Google Scholar]
- 62. Willems T, Witvrouw E, Verstuyft J, Vaes P, De Clercq D. Proprioception and muscle strength in subjects with a history of ankle sprains and chronic instability. J Athl Train. 2002;37(4):487-493 [PMC free article] [PubMed] [Google Scholar]
- 63. Williams GN, Jones MH, Amendola A. Syndesmotic ankle sprains in athletes. Am J Sports Med. 2007;35(7):1197-1207 [DOI] [PubMed] [Google Scholar]
- 64. Wright RW, Barile RJ, Surprenant DA, Matava MJ. Ankle syndesmosis sprains in national hockey league players. Am J Sports Med. 2004;32(8):1941-1945 [DOI] [PubMed] [Google Scholar]
- 65. Xenos JS, Hopkinson WJ, Mulligan ME, Olson EJ, Popovic NA. The tibiofibular syndesmosis: evaluation of the ligamentous structures, methods of fixation, and radiographic assessment. J Bone Joint Surg Am. 1995;77(6):847-856 [DOI] [PubMed] [Google Scholar]
- 66. Zalavras C, Thordarson D. Ankle syndesmotic injury. J Am Acad Orthop Surg. 2007;15(6):330-339 [DOI] [PubMed] [Google Scholar]
- 67. Zech A, Hubscher M, Vogt L, Banzer W, Hansel F, Pfeifer K. Neuromuscular training for rehabilitation of sports injuries: a systematic review [published online ahead of print September 2, 2009]. Med Sci Sports Exerc. [DOI] [PubMed] [Google Scholar]
- 68. Zech A, Hubscher M, Vogt L, Banzer W, Hansel F, Pfeifer K. Balance training for neuromuscular control and performance enhancement: a systematic review. J Athl Train. 2010;45(4):392-403 [DOI] [PMC free article] [PubMed] [Google Scholar]


