Abstract
Context:
Lateral ankle sprains can manifest into chronic mechanical joint laxity when not treated effectively. Joint laxity is often measured through the use of manual stress tests, stress radiography, and instrumented ankle arthrometers.
Purpose:
To systematically review the literature to establish the influence of chronic ankle instability (CAI) on sagittal and frontal plane mechanical joint laxity.
Data Sources:
Articles were searched with MEDLINE (1966 to October 2008), CINAHL (1982 to October 2008), and the Cochrane Database of Systematic Reviews (to October 2008) using the key words chronic ankle instability and joint laxity, functional ankle instability and joint laxity, and lateral ankle sprains and joint laxity.
Study Selection:
To be included, studies had to employ a case control design; mechanical joint laxity had to be measured via a stress roentogram, an instrumented ankle arthrometer, or ankle/foot stress-testing device; anteroposterior inversion or eversion ankle-subtalar joint complex laxity had to be measured; and means and standard deviations of CAI and control groups had to be provided.
Data Extraction:
One investigator assessed each study based on the criteria to ensure its suitability for analysis. The initial search yielded 1378 potentially relevant articles, from which 8 were used in the final analysis. Once the study was accepted for inclusion, its quality was assessed with the PEDro scale.
Data Synthesis:
Twenty-one standardized effect sizes and their 95% confidence intervals were computed for each group and dependent variable. CAI produced the largest effect on inversion joint laxity; 45% of the effects ranged from 0.84 to 2.61. Anterior joint laxity measures were influenced second most by CAI (effects, 0.32 to 1.82). CAI had similar but less influence on posterior joint laxity (effects, −0.06 to 0.68) and eversion joint laxity (effects, 0.03 to 0.69).
Conclusion:
CAI has the largest effect with the most variability on anterior and inversion joint laxity measurements, consistent with the primary mechanism of initial injury.
Keywords: ankle injury, joint laxity, chronic ankle instability, ankle sprain
In the United States, 23 000 physically active individuals incur lateral ankle sprains on a daily basis.8 The impact of this common injury is substantial, with pain, disability, and time lost from work and activity estimated to result in 1.2 million physician visits per year and an annual health care cost approximating $3.8 billion.8 In an assessment of the impact of lateral ankle sprains in National Collegiate Athletic Association athletes during a 16-year period, 14% of all injuries reported were lateral ankle sprains.14 The recurrence rates for these injuries are alarming as well, with estimates as high as 70%.39 Owing to the tendency for repeated lateral ankle sprains to occur with the continued lingering signs and symptoms associated with functional deficits, patients ultimately develop a condition termed chronic ankle instability (CAI).10
Although the exact cause of CAI remains unknown, substantial mechanical joint16 and sensorimotor elements11 are thought to be at play. Mechanical instability of the talocrural and talocalcaneal articulations accompanies acute lateral ankle sprains and occurs because of the disruption of the anterior talofibular, calcaneofibular, and posterior talofibular ligaments, which provide passive restraint for the lateral ankle complex.10 Acute lateral ankle sprains are frequently trivialized, and adequate rehabilitation does not follow. Patients can then develop pathological joint laxity that makes the lateral ankle-subtalar joint complex vulnerable to repetitive injury and, ultimately, the development of CAI. Early work investigating the influence of functional ankle instability (FAI) and CAI on joint displacement used a qualitative approach in which manual stress testing of the ankle-subtalar joint complex was performed.5,33 Although this initial research was important in trying to describe joint laxity changes in patients suffering from CAI, it was limited in that the specific degree of joint laxity was difficult to establish. Stress radiography, established thereafter, was important in allowing joint laxity to be measured more accurately.29,30,40 However, the reliability and validity of manual stress tests with or without stress radiography have been questioned,6,7 leading to the development of instrumented arthrometers and custom-made mechanical devices that can precisely quantify joint kinematics noninvasively.14,17,22,23
Previous investigations have established the relationships between linear and angular joint displacement and functional ability in CAI,20 as well as correctly classifying CAI patients.19 Although this work has been important in understanding the relationship of CAI and mechanical joint laxity, the overall effects that CAI may have on joint laxity have not been adequately summarized.37
Methods
Study Search Strategy
MEDLINE (1966 to October 2008), CINAHL (1982 to October 2008), and the Cochrane Database of Systematic Reviews (to October 2008) were searched using the keywords chronic ankle instability and joint laxity, functional ankle instability and joint laxity, and lateral ankle sprains and joint laxity. Articles were additionally obtained by cross-referencing published articles from the database searches. Collectively, the search produced 1378 potentially relevant articles, which were further screened for inclusion.
Study Selection Criteria
The following criteria were used for study evaluation and inclusion: a case control or quasiexperimental design investigating the effects of CAI or FAI on mechanical joint laxity; mechanical joint laxity measured via stress roentogram, instrumented ankle arthrometer, or ankle/foot stress testing device; anterior, posterior, inversion, or eversion ankle-subtalar joint laxity measured with the techniques just cited; and the means and standard deviations or standard errors provided for each quantitative mechanical joint laxity measurement for the CAI or FAI group and the matched healthy (control) group.
A single examiner identified and screened the 1378 studies for potential inclusion in the analysis, of which 1329 were excluded because they did not assess ankle-subtalar joint laxity; 49 potential articles were retrieved and analyzed further. Fourteen studies were identified that measured either mechanical joint laxity in the anterior or posterior direction or joint laxity during inversion or eversion movement. Of these 14 articles, 6 were excluded because they examined joint laxity with subjective/qualitative methods. Therefore, the systematic review included 8 studies that objectively measured joint laxity, from which multiple effects were used to systematically investigate CAI/FAI effects (Figure 1).
Figure 1.
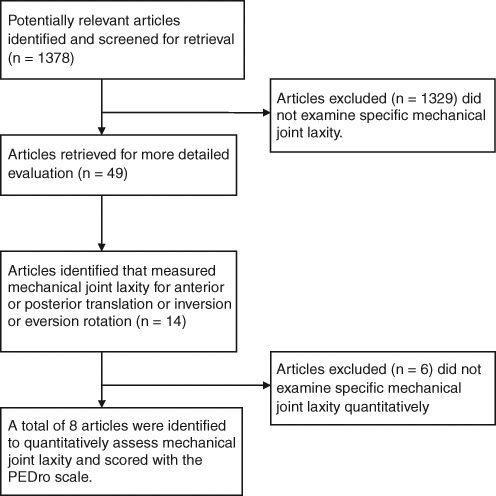
Schema for selected studies for the systematic review.
Assessment of Study Quality
All studies selected for inclusion in the analysis were evaluated with the PEDro scale (ie, methodological quality of randomized controlled trials [RCTs] and non-RCTs).27 The 11-item checklist yields a PEDro score based on a 10-point scale in which large values indicate a higher-quality study design.27 A maximum score of 10 can occur for an RCT if all of the established criteria in the checklist are met, whereas a maximum score of 8 can be achieved for non-RCTs. Two authors assessed the 8 studies that met the criteria so that agreement regarding the PEDro score could be established for each study used in the analysis.27
Data Analysis/Extraction
Standardized effect sizes were calculated to establish the effect of CAI/FAI, compared to healthy control groups, on mechanical joint laxity measurements taken for anterior and posterior translations as well as inversion and eversion rotations. The effect sizes were computed by subtracting the healthy group mean from the CAI/FAI mechanical joint laxity mean for each movement and dividing that sum by the standard deviation of the healthy condition.2,4,31 Thus, a positive effect represents greater mechanical joint laxity, whereas a negative effect represents decreased joint laxity. The 95% confidence interval (CI) provides information concerning the variability of the observed effect size, its precision, as well as the accuracy with which the interval contains the population parameter (ie, the true value). The standardized effect sizes were interpreted according to the guidelines established by Cohen4 in which values < 0.20 are trivial or not substantial, 0.20 and 0.49 are small but substantial, 0.50 and 0.79 are moderate, and ≥ 0.80 are large.
Results
A total of 21 effects from 8 studies15,17,19,24-26,36,38 were used in the analysis to investigate the effects of CAI/FAI on mechanical joint laxity in the sagittal and frontal planes (Table 1). The PEDro scores for these studies ranged from 4 to 6, with an average rating of 5. Studies across this analysis did not investigate the same effects. As such, some studies investigated only the effects of CAI on anterior joint laxity, whereas others investigated the influence of CAI on anterior and inversion joint laxity. Specifically, 4 studies investigated the effects of CAI/FAI on anterior joint laxity17,19,24,36; 3 investigated posterior joint laxity17,19,24; 8 investigated inversion joint laxity15,17,19,24-26,36,38; and 3 investigated eversion joint laxity.17,19,24
Table 1.
Selected studies for review.a
| Research Study | PEDro Score | Study Design | Participants, n | Inclusion Criteria | Measurement Technique | Joint Laxity Measures |
|---|---|---|---|---|---|---|
| Hubbard et al17 | 6 | Quasiexperimental (intact group), within subject | 51 unilateral FAI | Respond yes to select items on questionnaire | Instrumented ankle arthrometer and stress radiography with a Telos device | Total anteroposterior displacement, total internal-external rotation (abduction-adduction), anterior laxity, talar tilt laxity (stress radiography) |
| Hubbard et al19 | 6 | Case control, between subject | 30 unilateral CAI, 30 controls | Respond yes to select items on questionnaire | Instrumented arthrometer | Anterior, posterior, inversion, and eversion laxity |
| Hubbard15 | 6 | Case control, between subject | 16 unilateral CAI, 16 controls | Respond yes to select items on questionnaire; personal interview | Instrumented arthrometer | Anterior, posterior, inversion, and eversion laxity |
| Lentell et al24 | 5 | Quasiexperimental (intact group), within subject | 34 unilateral CAI | Screened for unilateral CAI that has plateaued | Stress radiography with manual stress test | Inversion laxity via talar tilt |
| Louwerens et al25 | 4 | Case control, between subject | 22 bilateral CAI, 11 unilateral CAI, 10 controls | Frequent inversion trauma and sensations of giving way | Stress radiography with custom mechanical device | Talocrural tilt and subtalar tilt |
| Lui et al26 | 5 | Quasiexperimental (intact group), within subject | 15 unilateral CAI | > 2 episodes of severe unilateral sprain within 10 yrs of study | Instrumented ankle arthrometer | Anterior and inversion laxity |
| van Hellemondt et al36 | 4 | Quasiexperimental (intact group), within subject | 15 unilateral CAI | Frequent inversion trauma and sensations of giving way | Stress radiography with a Telos device | Talocrural tilt and subtalar tilt |
| Yamamoto et al38 | 4 | Case control, between subject | 23 unilateral CAI, 80 controls | None provided | Stress radiography with a Telos device | Talocrural tilt and subtalar tilt |
CAI, chronic ankle instability; FAI, functional ankle instability.
CAI and Anterior Joint Laxity
Four studies17,19,24,36 analyzed the effects that CAI/FAI had on anterior joint laxity (mean PEDro score, 5.8) (Table 2). The standardized effect sizes ranged from 0.32 to 1.82, indicating that CAI/FAI results in greater anterior joint laxity compared to a healthy condition. Two studies17,36 demonstrated nearly identical effects, 0.32 and 0.33, which are considered small but clinically relevant, whereas the other 2 investigations19,24 exhibited much larger effects, 1.82 and 1.16, with greater variability even though they used same methodology and instrumentation. In 3 of the 4 studies, the 95% CI for each effect did not cross zero, indicating that CAI/FAI patients do exhibit significant increases in anterior joint laxity when compared to healthy controls.
Table 2.
Anterior joint laxity and effect sizes by group.
| Study | Variable | Control | CAI/FAIa | Effect Sizeb |
|---|---|---|---|---|
| Hubbard15 | Anterior displacement, mm | 11.8 ± 0.9 | 13.4 ± 1.9 | 1.82 (1.41, 2.24) |
| Hubbard et al19 | Anterior laxity, mm | 11.9 ± 1.9 | 14.1 ± 2.3 | 1.16 (0.48, 1.83) |
| Hubbard et al17 | Anterior displacement, mm | 11.1 ± 3.2 | 12.1 ± 3.1 | 0.32 (−0.56, 1.20) |
| Lui et al26 | Anterior drawer flexibility, mm/N | 0.15 ± 0.06 | 0.17 ± 0.05 | 0.33 (0.30, 0.37) |
CAI, chronic ankle instability; FAI, functional ankle instability.
95% confidence intervals in parentheses.
CAI and Posterior Joint Laxity
Three studies analyzed CAI/FAI on posterior joint laxity measures15,17,19 (mean PEDro score, 6.0) (Table 3). For posterior joint laxity measures, the point estimates for the standardized effect sizes ranged from −0.06 to 0.68 and were not nearly as large as those observed for anterior joint laxity. Two of these studies15,17 demonstrated positive moderate effect sizes indicative of greater laxity in the CAI/FAI group compared to the healthy control group, whereas the other study19 revealed an insubstantial effect (−0.06) demonstrating that CAI/FAI patients have less posterior joint laxity compared to that of healthy patients. The 95% CIs17,19 of 2 studies confirmed no significant differences between CAI/FAI patients and healthy controls on posterior joint laxity, whereas the study that did produce the largest effect15 showed that CAI/FAI patients exhibit significant increases in posterior joint laxity in comparison to healthy controls.
Table 3.
Posterior joint laxity and effect sizes by group.a
| Study | Control | CAI/FAIb | Effect Sizec |
|---|---|---|---|
| Hubbard15 | 4.1 ± 1.2 | 4.9 ± 1.1 | 0.68 (0.10, 1.24) |
| Hubbard et al19 | 5.2 ± 1.6 | 5.1 ± 1.2 | −0.06 (−0.64, 0.50) |
| Hubbard et al17 | 7.2 ± 1.6 | 7.7 ± 1.7 | 0.32 (−0.11, 0.75) |
Variable for each study: posterior displacement, mm.
CAI, chronic ankle instability; FAI, functional ankle instability.
95% confidence intervals in parentheses.
CAI and Inversion Joint Laxity
Eight studies15,17,19,24-26,36,38 provided 11 effects in which the influence of CAI/FAI on inversion joint laxity measures could be analyzed (PEDro score, 5.0) (Table 4). The point estimates calculated for this effect were positive, indicating that, collectively, CAI/FAI patients demonstrate larger amounts of inversion joint laxity compared to healthy patients. Three studies25,36,38 characterized frontal plane inversion joint laxity with 2 separate measures—talar tilt and subtalar tilt rotation. These studies were published within 3-year time span and used nearly identical methodology in quantifying inversion joint laxity measurements. There was a considerable amount of variability in the range of standardized effect sizes calculated (0.06 to 2.61). Forty-five percent of the total effects calculated within these studies demonstrated large values, ranging from 0.84 to 2.6115,25,36,38; of these 5 large effects, 3 were very large, ranging between 1.80 and 2.61.15,38 Of the 11 effects computed, 4 (36%) were trivial or not substantial, with the range being 0.06 to 0.21,17,19,25,26 whereas 2 (18%) were small but substantial, 0.31 and 0.37; finally, 2 (18%) effects were deemed moderate, 0.84 and 0.92. Regarding the 95% CI, 3 of 11 effects (27%) did not cross zero, indicating that CAI/FAI patients do exhibit significant increases in inversion joint laxity compared to healthy controls.
Table 4.
Inversion joint laxity and effect sizes by group.
| Study | Variable | Control | CAI/FAIa | Effect Sizeb |
|---|---|---|---|---|
| Hubbard15 | Inversion rotation° | 32.3 ± 1.8 | 35.6 ± 2.9 | 1.80 (0.9, 2.7) |
| Hubbard et al19 | Inversion laxity° | 34.1 ± 3.9 | 34.9 ± 4.9 | 0.21 (−1.2, 1.6) |
| Hubbard et al17 | Inversion rotation° | 32.3 ± 1.8 | 35.6 ± 2.9 | 0.14 (−1.53, 1.82) |
| Lui et al26 | Inversion flexibility, deg/N·m | 9.01 ± 2.4 | 9.19 ± 2.4 | 0.07 (−1.3, 1.4) |
| Lentell et al24 | Talar tilt° | 4.0 ± 2.7 | 5.0 ± 2.9 | 0.37 (−0.5, 1.2) |
| Louwerens et al25 | Talar tilt° | 2.6 ± 3.9 | 6.2 ± 4.8 | 0.92 (−1.5, 3.3) |
| Subtalar tilt° | 10.1 ± 3.4 | 10.3 ± 3.8 | 0.06 (−2.0, 2.1) | |
| Yamamoto et al38 | Talar tilt° | 4.6 ± 3.1 | 12.7 ± 8.2 | 2.61 (1.93, 3.29) |
| Subtalar tilt° | 5.2 ± 2.6 | 10.3 ± 2.9 | 1.96 (1.39, 2.53) | |
| van Hellemondt et al36 | Talar tilt° | 6.3 ± 4.3 | 7.6 ± 5.4 | 0.31 (−1.86, 2.48) |
| Subtalar tilt° | 7.7 ± 2.6 | 9.8 ± 3.2 | 0.84 (−0.46, 2.13) |
CAI, chronic ankle instability; FAI, functional ankle instability.
95% confidence intervals in parentheses.
CAI and Eversion Joint Laxity
Three studies analyzed eversion joint laxity (mean PEDro score, 6.0) (Table 5).15,17,19 All of the effect sizes were positive, indicating greater eversion joint laxity in patients with CAI/FAI compared to healthy controls. For the eversion joint laxity measures, the standardized effect sizes ranged from 0.03 to 0.69. The low range of the effect sizes for eversion laxity was similar to that observed for inversion joint laxity; however, the high end of the eversion range (0.69) was not nearly as close to that observed for inversion (2.61). The 3 effects represented magnitudes that were trivial (0.03),17 small (0.22),19 and moderate (0.69).15 The 95% CIs indicate that none of the effects demonstrated significant differences between CAI/FAI patients and healthy controls on eversion joint laxity.
Table 5.
Eversion joint laxity and effect sizes by group.
| Study | Variable | Control | CAI/FAIa | Effect Sizeb |
|---|---|---|---|---|
| Hubbard15 | Eversion rotation° | 22.3 ± 2.8 | 24.2 ± 4.7 | 0.69 (−0.66, 2.03) |
| Hubbard et al19 | Eversion laxity° | 20.6 ± 4.5 | 21.6 ± 4.7 | 0.22 (−1.39, 1.83) |
| Hubbard et al17 | Eversion rotation° | 24.8 ± 3.1 | 24.9 ± 3.2 | 0.03 (−0.82, 0.88) |
CAI, chronic ankle instability; FAI, functional ankle instability.
95% confidence intervals in parentheses.
Discussion
The physical examination remains the primary means to diagnose the musculoskeletal pathology of ankle injuries. Manual stress testing of the passive joint structures is essential. The anterior drawer and inversion talar tilt tests are essential for determining the sagittal and frontal plane mechanical joint stability.32 Although the physical examination is performed to assess a patient’s level of mechanical joint laxity, it relies extensively on the practitioner’s level of experience and on the sensitivity of the test itself. The literature has shown that the sensitivity of the anterior drawer test varies between 32% to 80%,3,35 with the talar tilt test at 52%.3
Due to the inherent limitations of quantifying ankle-subtalar joint complex stability with manual stress testing during a physical examination, the use of stress radiography has been advocated.6,28,32 Mechanical positioning tools may provide more reliable assessments of joint laxity.12,25,28,32,38 Instrumented ankle arthrometers may provide a more reliable and valid method for quantifying sagittal plane translation and frontal plane rotation of the ankle-subtalar joint complex in healthy and CAI patients.13,15,17-19,22,23
Research investigating CAI and the tendency toward accelerated joint surface degradation leading to posttraumatic ankle osteoarthritis1,21 will continue to be a substantial challenge faced by those in the orthopaedic community.9,34
CAI and Anterior Joint Laxity
The 4 studies that assessed the influence of CAI on joint laxity displayed disparate results, with 2 revealing small effects17,26 and with 2 demonstrating large effects.15,19 Data from Hubbard et al15,19 demonstrate good precision because the boundaries for the CIs are narrow, whereas the effect observed from Lui et al26 is 3 to 6 times smaller than those observed in the other investigations,15,19 but their point estimate also contains a narrow CI, indicative of precise and significant effect. Hubbard et al15 measured anterior joint laxity with an instrumented ankle arthrometer and defined it as a function of joint deformation according to a fixed load (125 N). Lui and colleagues28 also used an instrumented arthrometer but defined anterior joint laxity as the slope of the linear portion of the load deformation curve, which may account for the difference in the calculated effects sizes between the 2 investigations.
It is not surprising that small to very large effects of anterior joint laxity were identified in patients with CAI compared to healthy controls, because talocrural joint laxity is often the debilitating outcome of recurrent lateral ankle injuries.5,12,21,24,25 Both the anterior talofibular and the calcaneofibular ligaments play a primary role in providing passive restraint to the talocrural complex. Sequential sectioning of the anterior talofibular and calcaneofibular in a cadaveric model does increase anterior talar translation.23 Compared to uninjured controls, patients with CAI demonstrated significant anterior drawer laxity and greater talar tilt with supination stress.12 Clinicians sometimes assume that the lateral ankle ligaments heal following injury, but talocrural joint laxity may persist if these ankles are not adequately treated.12,24,25 Rehabilitation programs need to emphasize sufficient time for anterior ligament healing and provide a graded therapeutic exercise regime that restores joint range of motion, muscles strength, and sensorimotor control.
CAI and Posterior Joint Laxity
The magnitude of effects derived from the 3 studies examining the influence of CAI on posterior joint laxity ranged from trivial (−0.06) to moderate (0.68).15,17,19 The largest effect observed (0.68) was from the Hubbard study15 that investigated ligament laxity in 16 patients with unilateral CAI. Average posterior displacement in the injured ankle was 7.7 mm, compared to 7.2 mm in the control ankle. Although the magnitude of the point estimate can be viewed as being moderate, interpretation of the upper limit of the interval estimate (ie, the 95% CI) indicates that the true effect could be as high as 1.24 and as low as 0.10. This suggests that CAI patients who sustain more than 1 unilateral ankle sprain and frequent episodes of ankle giving way (at least once a month) may present with significantly greater posterior laxity compared to that of matched controls. A smaller effect (0.32) was observed in 51 patients with self-reported unilateral FAI.17 Differences in patient inclusion criteria may account for larger differences in the posterior joint laxity measurements and a different magnitude of effect.17 Surprisingly, in a similar investigation based on the same inclusion criteria and ankle ligament laxity measurement device,19 CAI had a much smaller and negative effect (−0.06) compared to healthy controls. CAI patients did not demonstrate any difference in posterior joint laxity compared to healthy controls.
The effects of CAI on posterior joint laxity have been studied less than anterior joint laxity. The passive tissues that provide restraint against posterior translation of the talocrural complex are not injured nearly as often.1 The evidence from this analysis suggests that patients with CAI do not have a large amount of posterior joint laxity. Clinically, posterior joint laxity does not generally pose a challenge to the practitioner when treating patients with CAI. However, clinicians do need to be cognizant of its existence and the limitations that it can impose to the successful rehabilitation of the chronically unstable ankle.
CAI and Inversion Joint Laxity
Inversion joint laxity is widely investigated in patients with CAI because it is the primary mechanism of injury (combined plantar flexion and inversion). In this review, 11 effects from 8 investigations focused on inversion: 3 investigations measured inversion rotation or laxity17,19,15; 4, talar and subtalar tilt24,25,36,38; and 1, inversion flexibility.26 Four used an instrumented ankle arthrometer17,19,15,26 to measure inversion joint laxity. Instrumented ankle arthrometry was developed so that ligament laxity of the ankle-subtalar joint complex could be assessed in a more reliable and valid way. The other 4 investigations grouped in the inversion joint laxity analysis measured talar tilt and subtalar tilt angles.24,25,36,38 Three25,36,38 used a mechanical hinge device to stabilize the patient while a stress radiograph was taken. The other investigation used a manual stress radiography test.24 Because of the differences in the variables measured and the methodologies, the calculation of effect sizes allows for direct meaningful comparison among these studies.
The effects for inversion joint laxity were the largest; 5 of the 11 ranged from 0.84 to 2.61.15,25,38 The magnitude of these effects suggests that CAI demonstrated the greatest influence on inversion joint laxity. The largest effect size, 2.61(95% CI [1.9 to 3.3]), was from data in the Yamamoto et al38 investigation for talar tilt. When this effect size and its interval estimate are evaluated closely, the magnitude of the effect suggests that CAI increased inversion joint laxity 2.61 standard deviation units beyond the control mean. Perhaps even more important is the interpretation of the interval estimate. The width of the interval indicates excellent precision, with the likelihood that the effect of CAI on laxity is even higher (3.3). The CIs for the large effects did not cross zero, suggesting that CAI ankles demonstrated significantly greater inversion joint laxity when compared to that of matched controls.
Although 45% of the total effects were large, a surprisingly proportion (36%) were trivial. These effects were derived from inversion flexibility,26 inversion rotation,17 inversion laxity,19 and subtalar tilt.25 The CIs for the point estimates were relatively wide and did cross zero. These characteristics suggest an overall lack of precision of the sample statistic to the population parameter, as well as the lack of statistic significance between CAI and control groups. Of the 11 effects, 2 (18%) were moderate.25,36 Neither were significant, and each interval estimate demonstrated a lack of precision, principally because of the relatively small samples employed in the studies relative to the amount of random error generated in the measurement. It is not surprising that the largest and most significant effects observed in patients with CAI were reflected in the inversion joint laxity measures owing to the high incidence and recurrence of the lateral inversion ankle sprain. Clinicians should direct rehabilitation programs toward firmly restoring joint stability either through improved immobilization techniques or through exercises that better focus on enhancing dynamic joint stability.
CAI and Eversion Joint Laxity
Medial ankle sprains and eversion ankle injuries are not nearly as common as the lateral ankle injury. In the current analysis, 3 studies provided 3 effects that were grouped to provide an assessment of CAI/FAI influences on eversion joint laxity.15,17,19 The point estimates from the studies represent a trivial effect (0.03), a small effect (0.22), and a moderate effect (0.69). The medial ankle ligaments are rarely involved in the common lateral ankle sprain, only 2 of the 3 studies yielded very small effects.17,19 Their 95% CIs, the true population effect for eversion laxity could yield a value as high as 1.83. For the eversion rotation variable,24 a moderate effect (0.69) produced a 95% CI of −0.66 to 2.03. The data show that small to moderate eversion joint laxity persists in patients who suffer from CAI.
Summary
This systematic review suggests that CAI has the greatest influence on inversion joint laxity, followed by anterior joint laxity. The magnitude of these effects, along with their 95% CIs, suggests that these effects are very large. Posterior and eversion joint laxity is present in those with CAI, but the effects are not nearly as profound.
Footnotes
No potential conflict of interest declared.
References
- 1. Anderson MK, Hall SJ, Martin M. Sports Injury Management. 2nd ed. Baltimore, MD: Lippincott Williams & Wilkins; 2000 [Google Scholar]
- 2. Becker BJ. Synthesizing standardized mean-change measures. Br J Math Stat Psychol. 1988;41:257-278 [Google Scholar]
- 3. Blanshard KS, Finlay DB, Scott DJ, Ley CC, Siggins D, Allen MJ. A radiological analysis of lateral ligament injuries of the ankle. Clin Radiol. 1986;37(3):247-251 [DOI] [PubMed] [Google Scholar]
- 4. Cohen J. Statistical Analysis for the Behavioral Sciences. New York, NY: Academic Press; 1977 [Google Scholar]
- 5. Freeman MA. Instability of the foot after injuries to the lateral ligament of the ankle. J Bone Joint Surg Br. 1965;47(4):669-677 [PubMed] [Google Scholar]
- 6. Frost SC, Amendola A. Is stress radiography necessary in the diagnosis of acute or chronic ankle instability? Clin J Sport Med. 1999;9(1):40-45 [DOI] [PubMed] [Google Scholar]
- 7. Fujii T, Luo ZP, Kitaoka HB, An KN. The manual stress test may not be sufficient to differentiate ankle ligament injuries. Clin Biomech (Bristol, Avon). 2000;15(8):619-623 [DOI] [PubMed] [Google Scholar]
- 8. Gerber JP, Williams GN, Scoville CR, Arciero RA, Taylor DC. Persistent disability associated with ankle sprains: a prospective examination of an athletic population. Foot Ankle Int. 1998;19(10):653-660 [DOI] [PubMed] [Google Scholar]
- 9. Harrington KD. Degenerative arthritis of the ankle secondary to long-standing lateral ligament instability. J Bone Joint Surg Am. 1979;61(3):354-361 [PubMed] [Google Scholar]
- 10. Hertel J. Functional anatomy, pathomechanics, and pathophysiology of lateral ankle instability. J Athl Train. 2002;37(4):364-375 [PMC free article] [PubMed] [Google Scholar]
- 11. Hertel J. Sensorimotor deficits with ankle sprains and chronic ankle instability. Clin Sports Med. 2008;27(3):353-370 [DOI] [PubMed] [Google Scholar]
- 12. Hertel J, Denegar CR, Monroe MM, Stokes WL. Talocrural and subtalar joint instability after lateral ankle sprain. Med Sci Sports Exerc. 1999;31(11):1501-1508 [DOI] [PubMed] [Google Scholar]
- 13. Hollis JM. A six-degree-of-freedom test system for the study of joint mechanics and ligament forces. J Biomech Eng. 1995;117(4):383-389 [DOI] [PubMed] [Google Scholar]
- 14. Hootman JM, Dick R, Agel J. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train. 2007;42(2):311-319 [PMC free article] [PubMed] [Google Scholar]
- 15. Hubbard TJ. Ligament laxity following inversion injury with and without chronic ankle instability. Foot Ankle Int. 2008;29(3):305-311 [DOI] [PubMed] [Google Scholar]
- 16. Hubbard TJ, Hertel J. Mechanical contributions to chronic lateral ankle instability. Sports Med. 2006;36(3):263-277 [DOI] [PubMed] [Google Scholar]
- 17. Hubbard TJ, Kaminski TW, Vander Griend RA, Kovaleski JE. Quantitative assessment of mechanical laxity in the functionally unstable ankle. Med Sci Sports Exerc. 2004;36(5):760-766 [DOI] [PubMed] [Google Scholar]
- 18. Hubbard TJ, Kovaleski JE, Kaminski TW. Reliability of intratester and intertester measurements derived from an instrumented ankle arthrometer. J Sport Rehabil. 2003;12(3):208-220 [Google Scholar]
- 19. Hubbard TJ, Kramer LC, Denegar CR, Hertel J. Contributing factors to chronic ankle instability. Foot Ankle Int. 2007;28(3):343-354 [DOI] [PubMed] [Google Scholar]
- 20. Hubbard TJ, Kramer LC, Denegar CR, Hertel J. Correlations among multiple measures of functional and mechanical instability in subjects with chronic ankle instability. J Athl Train. 2007;42(3):361-366 [PMC free article] [PubMed] [Google Scholar]
- 21. Karlsson J, Bergsten T, Peterson L, Zachrisson BE. Radiographic evaluation of ankle joint stability. Clin J Sport Med. 1991;1(1):166-175 [Google Scholar]
- 22. Kovaleski JE, Gurchiek LR, Heitman RJ, Hollis JM, Pearsall AW. Instrumented measurement of anteroposterior and inversion-eversion laxity of the normal ankle joint complex. Foot Ankle Int. 1999;20(12):808-814 [DOI] [PubMed] [Google Scholar]
- 23. Kovaleski JE, Hollis J, Heitman RJ, Gurchiek LR, Pearsall AW. Assessment of ankle-subtalar-joint-complex laxity using an instrumented ankle arthrometer: an experimental cadaveric investigation. J Athl Train. 2002;37(4):467-474 [PMC free article] [PubMed] [Google Scholar]
- 24. Lentell G, Baas B, Lopez D, McGuire L, Sarrels M, Snyder P. The contributions of proprioceptive deficits, muscle function, and anatomic laxity to functional instability of the ankle. J Orthop Sports Phys Ther. 1995;21(4):206-215 [DOI] [PubMed] [Google Scholar]
- 25. Louwerens JW, Ginai AZ, van Linge B, Snijders CJ. Stress radiography of the talocrural and subtalar joints. Foot Ankle Int. 1995;16(3):148-155 [DOI] [PubMed] [Google Scholar]
- 26. Lui W, Siegler S, Techner L. Quantitative measurement of ankle passive flexibility using an arthrometer on sprained ankles. Clin Biomech (Bristol, Avon). 2001;16:237-244 [DOI] [PubMed] [Google Scholar]
- 27. Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003;83(8):713-721 [PubMed] [Google Scholar]
- 28. Martin D, Kaplan P, Kahler D, Dussault R, Randolph B. Retrospective evaluation of graded stress examination of the ankle. Clin Orthop. 1996;328:165-170 [DOI] [PubMed] [Google Scholar]
- 29. Meyer J, Lagier R. Post-traumatic sinus tarsi syndrome: an anatomical and radiological study. Acta Orthop Scand. 1977;48:121-128 [DOI] [PubMed] [Google Scholar]
- 30. Meyer JM, Garcia J, Hoffmeyer P, Fritschy D. The subtalar sprain: a roentgenographic study. Clin Orthop. 1986;226:169-173 [PubMed] [Google Scholar]
- 31. Morris SB. Distribution of the standardized mean change effect size for meta-analysis on repeated measures. Br J Math Stat Psychol. 2000;53:17-29 [DOI] [PubMed] [Google Scholar]
- 32. Tohyama H, Beynnon BD, Renstrom PA, Theis MJ, Fleming BC, Pope MH. Biomechanical analysis of the ankle anterior drawer test for anterior talofibular ligament injuries. J Orthop Res. 1995;13(4):609-614 [DOI] [PubMed] [Google Scholar]
- 33. Tropp H. Stabilometry recordings in functional and mechanical instability of the ankle joint. Int J Sports Med. 1985;6:180-182 [DOI] [PubMed] [Google Scholar]
- 34. Valderrabano V, Hintermann B, Horisberger M, Fung TS. Ligamentous posttraumatic ankle osteoarthritis. Am J Sports Med. 2006;34(4):612-620 [DOI] [PubMed] [Google Scholar]
- 35. van Dijk CN, Lim LS, Bossuyt PM, Marti RK. Physical examination is sufficient for the diagnosis of sprained ankles. J Bone Joint Surg Br. 1996;78(6):958-962 [DOI] [PubMed] [Google Scholar]
- 36. van Hellemondt FJ, Louwerens JW, Sijbrandij ES, van Gils AP. Stress radiography and stress examination of the talocrural and subtalar joint on helical computed tomography. Foot Ankle Int. 1997;18(8):482-488 [DOI] [PubMed] [Google Scholar]
- 37. Verhagen AP, de Vet HC, de Bie RA, et al. The Delphi list: a criteria list for quality assessment of randomized clinical trials for conducting systematic reviews developed by Delphi consensus. J Clin Epidemiol. 1998;51(12):1235-1241 [DOI] [PubMed] [Google Scholar]
- 38. Yamamoto H, Yagishita K, Ogiuchi T, Sakai H, Shinomiya K, Muneta T. Subtalar instability following lateral ligament injuries of the ankle. Injury. 1998;29(4):265-268 [DOI] [PubMed] [Google Scholar]
- 39. Yeung MS, Chan KM, So CH, Yuan WY. An epidemiological survey on ankle sprain. Br J Sports Med. 1994;28(2):112-116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Zell BK, Shereff MJ, Greenspan A, Liebowitz S. Combined ankle and subtalar instability. Bull Hosp Jt Dis Orthop Inst. 1986;46(1):37-46 [PubMed] [Google Scholar]


