Abstract
Previous observation has shown that the wild-type Kras2 allele is a suppressor of lung cancer in mice. Here we report that loss of heterozygosity (LOH) of chromosome 12p was detected in ~50% of human lung adenocarcinomas and large cell carcinomas, and Kras2 mutations were detected at codon 12 in ~40% of adenocarcinomas and large cell carcinomas. Interestingly, all of the lung adenocarcinomas and large cell carcinomas containing a Kras2 mutation exhibited allelic loss of the wild-type Kras2 allele when a correlation between LOH of the region on chromosome 12p and Kras2 mutation was made. These results from human lung cancer tissues provide a strong evidence in support of our previous observation in mouse models that the wild-type Kras2 is a tumor suppressor of lung cancer.
Keywords: wild-type Kras2, mutations: lung cancer, loss of heterozygosity, tumor suppressor
Introduction
Activating point mutations in the ras genes have been detected in more human tumor types and at a higher frequency (25–30% of all human tumors) than any other oncogenes (Bos, 1989; Anderson et al., 1992; Rodenhuis and Slebos, 1992; Beaupre et al., 1999). For example, ras mutations are detected in 40–50% of colon carcinomas (Perucho et al., 1981; Vogelstein et al., 1988; Burmer et al., 1991; Wang et al., 1993); 80% of pancreatic carcinomas (Mariyama et al., 1989; Shibata et al., 1990; Burmer et al., 1991; Pinto et al., 1997); and 30–50% of lung adenocarcinomas (Rodenhuis et al., 1988; Suzuki et al., 1990, Reynolds et al., 1991; Li et al., 1994; Mills et al., 1995). Kras2 mutations account for >90% of the activating ras mutations observed in these tumor types. Ras oncogenes are also seen in numerous other solid tumor types and in hematopoietic malignancies (Kiaris and Spandidos, 1995; Beaupre and Kurzrock, 1999). Some tumors exhibit activating mutations in each of the three ras genes (thyroid tumors and acute myelogenous leukemias). Some tumors have mutations in both Kras2 and Hras (chronic myelomocytic leukemia), whereas, other tumors contain activating mutations predominantly in Hras (squamous cell carcinomas of the skin and basal cell carcinomas) or in Nras (melanomas).
The oncogenic alleles of ras genes are generally perceived to be dominant since their transforming ability exists when normal alleles are also expressed (Barbacid, 1987; Marshall, 1991). However, recent evidence from both in vivo and in vitro studies suggest that the dominance of the ras oncogene might result from overexpression of the mutant ras allele or from deletion of the wild-type allele. Pervious studies in our laboratory showed that the wild-type Kras2 allele could suppress the oncogenic potential of the mutant Kras2 allele (Zhang et al., 2001). Heterozygous Kras2-deficient mice were highly susceptible to chemically induced lung tumors compared to wild-type littermates. All tumors displayed an activated Kras2 because of a chemically induced mutation. Wild-type Kras2 inhibited cell growth, colony formation and tumor development in a murine lung tumor cell line containing an activated Kras2 allele. In addition, the loss of wild-type Kras2 was found in 67–100% of chemically induced mouse lung adenocarcinomas harboring a mutant Kras2 allele (Zhang et al., 2001). Moreover, loss of the wild-type ras allele has been observed in mouse and human tumors indicating that the absence of the normal allele may facilitate transformation by one copy of the oncogenic ras allele. Hegi et al. (1994) reported that 14% of methylene chloride-induced mouse lung carcinomas exhibit allelic loss of the Kras2 wild-type while each retained the acivated Kras2 allele. Tumors that do not contain a mutated Kras2 allele did not exhibit loss of the normal Kras2 allele. Similar results have been reported for mouse skin tumors harboring activated Hras genes, where loss of the wild-type allele occurred only in tumors containing a mutant Hras allele (Bremner and Balmain, 1990; Buchmann et al., 1991). Thompson et al. (2002) showed in a transgenic rat model that over expression of wild-type Kras2 and Hras proteins significantly reduced MNU-induced rat mam-mary cancer when compared to their nontransgenic littermates. These findings suggest that wild-type Ras is a tumor suppressor and is frequently lost during tumor progression.
Several investigations have suggested allelic loss of chromosome 12p in human lung tumors, particularly adenocarcinomas and large cell carcinomas. The smallest common deleted region on 12p12–13 is flanked by D12S269 and D12S308 adjacent to the Kras2 gene. (Takeuchi et al., 1996a,b; De Gregorio et al., 1998). However, these studies did not analyse the correlation between allelic loss on 12p12–13 and Kras2 mutations. Since the percentage of lung adenocarcinomas that contain allelic loss on 12p12–13 is similar to the percentage of tumors that exhibit Kras2 mutations, it is possible that allelic loss may accompany each case of mutant Kras2 allele. To test the hypothesis that the wild-type Kras2 allele is a tumor suppressor gene in human lung tumors, we determined the extent of correlation between loss of heterozygosity (LOH) of chromosome 12p and Kras2 mutations in adenocarcinomas and large cell carcinomas.
A total of 22 adenocarcinomas and 8 large cell carcinomas were genotyped for LOH on chromosome 12. These tumors and their paired normal tissues were obtained from the Cooperative Human Tissue Network of The Ohio State University Department of Pathology (Columbus, OH, USA) and the University of Cincinnati (Cincinnati, OH, USA). A pathologist classified all tumors histopathologically. High-molecular weight DNA was isolated from both tumor and normal tissues of each case according to published protocols (Blin and Stafford, 1976). Allelic losses were assayed by PCR using eight polymorphic microsatellite markers on chromosome 12p: D12S89, D12S358, D12S310, D12S1606, D12S1596, G60541, D12S1617 and D12S1592 (Research Genetics, Inc.). All markers were scored on an 8% denaturing polyacrylamide gel. The gel was dried and exposed to X-ray film overnight, and LOH was scored visually. Only those samples in which a 40% or more difference were scored as an allelic loss. Using PCR-direct sequencing analysis, Kras2 gene codon 12 mutations were determined in all lung adenocarcinoma and large cell carcinoma DNAs. PCR amplification of Kras2 exon 1 from lung tumors was carried out as described (You et al., 1992). The sequences of PCR primers for Kras2 exon 1 were Kras2-1F: 5′-TTTTTATTATAAGGCCTGCT-3′ and Kras2—1R: 5′-GTCCACAAAATGATTCTGAA-3′. The 114 bp PCR products were eluted using QIAquick gel extraction kit (Qiagen, Valencia, CA, USA). Codon 12 mutations were detected using an ABI PRISM 3700 DNA analyzer (Perkin-Elmer/Applied Biosystems).
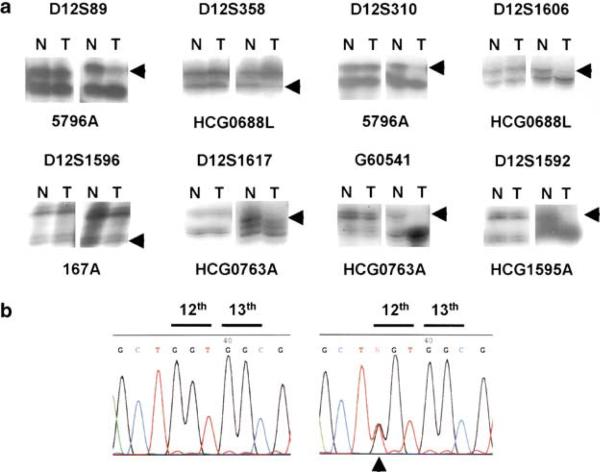
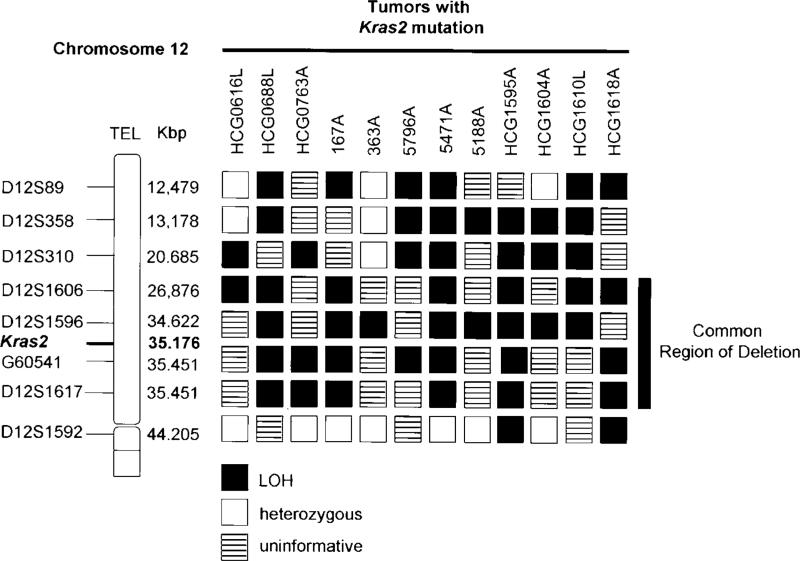
In total, eight microsatellite markers were analysed with focus on the Kras2 region. Allelotype data for individual markers is summarized in Table 1. A total of 10 out of 22 (45.5%) adenocarcinomas and 4 of 8 (50.0%) large cell carcinomas were found to have allelic loss at least on one of the markers used. Figure 1a shows representative results of the allelotype analysis of chromosome 12p at eight microsatellite markers. For Kras2 mutation analysis, our data showed 9 of 22 (40.9%) of adenocarcinomas and three of eight (37.5%) of large cell carcinomas contained a Kras2 mutation at codon 12 (GGT→TGT, CGT, GAT, GCT and GTT transition; Figure 1b, Table 2). When LOH analysis and Kras2 mutation data were combined, the majority of the allelic loss on chromosome 12p observed in adenocarcinomas and large cell carcinomas corresponded with an activated Kras2 mutation. Approximately 90.0% (9 of 10) of adenocarcinomas and 75.0% (3 of 4) of large cell carcinomas exhibited allelic loss of chromosome 12p while each retained the activated Kras2 allele. A total of 12 tumors with Kras2 mutations and with LOH at one or more loci on 12p are shown in Figure 2. Of these, tumors HCG0688L, 5796A, HCG1595A, HCG1610L and HCG1618A displayed losses at all of the informative markers analysed, whereas tumor 363A lost only the D12S1596 marker while retaining heterozygosity at the nearest informative markers, D12S310 and D12S1592. Tumors 167A and 5471A also displayed terminal deletion for marker D12S1617/G60541, where Kras2 is located, with retention of heterozygosity at the nearest informative marker, D12S1592 (Figure 2). The LOH data localized a minimal region of LOH to markers D12S1606 and D12S1617/G60541. The physical genomic map has placed the Kras2 gene at a position that is flanked by these two markers in a ~800 kb region. Our results indicate that the wild-type Kras2 allele is lost in human lung adenocarcinomas and large cell carcinomas.
Table 1.
LOH on chromosome 12 in non-small cell lung cancer
| Frequency of LOH on chromosome 12 |
||
|---|---|---|
| Marker | Adenocarcinoma LOH/Ia (%) | Large cell carcinoma LOH/I (%) |
| D12S89 | 4/11 (36.4) | 2/5 (40.0) |
| D12S358 | 6/11 (54.5) | 3/6 (50.0) |
| D12S310 | 5/11 (45.5) | 3/6 (50.0) |
| D12S1606 | 4/8 (50.0) | 3/4 (75.0) |
| D12S1596 | 6/10 (60.0) | 2/3 (66.7) |
| G60541 | 7/16 (43.8) | 2/3 (66.7) |
| D12S1617 | 5/13 (38.5) | 2/4 (50.0) |
| D12S1592 | 2/12 (16.7) | 0/3 (0.0) |
| Combined | 10/22 (45.5) | 4/8 (50.0) |
Number of tumors that were informative for the marker tested.
Figure 1.
(a) Representative autoradiograph showing LOH in non-small cell lung cancer. Above each autoradiograph, microsatellite marker; under each autoradiograph, patient's identification number; arrowheads, the allele losses; N, normal DNA;T, Tumor DNA. For each sample, the left panel, lung tumor without LOH; the right panel, lung tumor with LOH. (b) Representative example for Kras2 gene codon 12 mutation. On the left, lung tumor without Kras2 mutation; on the right, lung tumor with Kras2 gene 12th codon mutation (GGT→TGT transition)
Table 2.
Correlation between LOH on chromosome 12p and Kras2 activation in nonsmall cell lung cancer
| Tumor type | Patient number | Kras2 mutation | Frequency of LOH on chromosome 12p | Tumors with Kras2 mutations and LOH |
|---|---|---|---|---|
| Adenocarcinoma | 22 | 9/22 (40.9%) | 10/22 (45.5%) | 9/10 (90.0%) |
| Large cell carcinoma | 8 | 3/8 (37.5%) | 4/8 (50.0%) | 3/4 (75.0%) |
Figure 2.
LOH map of chromosome 12 in non-small cell lung cancers. A total of 12 samples containing a Kras2 mutation exhibited LOH at one or more loci on chromosome 12 Kras2 region. The genetic map of chromosome 12 was derived from NCBI Human Genome Resources. L, large cell carcinoma; A, adenocarcinoma
To our knowledge, this is the first report on the correlation between the presence of a mutant Kras2 allele and allelic loss on human chromosome 12p. Several prior studies have implicated the involvement of a tumor suppressor gene on chromosome 12p in the development of acute lymphoblastic leukemia (Takeuchi et al., 1996a; Baccichet and Sinnett, 1997). Baccichet and Sinnett (1997) suggested that the smallest commonly deleted region was between the markers D12S89 (distal) and D12S358 (proximal), which is similar to the region identified in prostate adenocarcinomas (Kibel et al., 1998). However, Takeuchi et al. (1996a) analysed acute lymphoblastic leukemias for allelic loss on chromosome 12p and identified two regions of deletion, one being the region closer to the Kras2 locus and the second being a more distal common deleted region delimited by the markers, D12S89 and D12S358 (Takeuchi et al., 1996a).
Owing to the important role in lung tumor development, Kras2 has been considered a major candidate gene for pulmonary adenoma susceptibility gene 1 (Pas 1) locus that was mapped to the distal region of chromosome 6, and accounts for approximately 50% of the phenotypic variance in mouse (Gariboldi et al., 1993). Three recent reports have demonstrated that human PAS1 locus located in the human 12p12 chromosome region and tightly linked to the Kras2 gene are involved in susceptibility to human lung adenocarcinoma (Manenti et al., 1997; Dragani et al., 2000; Yanagitani et al., 2002). Recently, by using congenic mice, we have identified that the Kras2 gene is a strong candidate for the Pas 1 locus on mouse chromosome 6 that predominately affects lung tumor progression (data not shown). Our results, those of Takeuchi et al., and similar results of LOH in human lung tumors produced by De Gregorio and his colleagues (Takeuchi et al., 1996a,b; De Gregorio et al., 1998) raise the possibility that the wild-type Kras2 allele is a tumor suppressor gene and can inhibit the progression of human lung tumors that contain a mutant Kras2. These findings also suggest that other tumors, especially pancreatic and colon carcinomas, are more likely to show positive correlation between allelic loss on chromosome 12p and activating Kras2 mutations since they contain a relatively high percentage of oncogenic Kras2 alleles.
Acknowledgements
We are grateful to G Otterson and P Ross for their assistance in human tissue collection, G Stoner and W Lemon for their critical reading of this manuscript, and E Wiley for secretarial assistance. This work was supported by Public Health Service Grants R01CA58554 (MY), R41CA093204 (MY) R01CA78797 (YW) and P30CA16058.
References
- Anderson MW, Reynolds SH, You M, Maronpot RM. Environ. Health Perspect. 1992;98:13–24. doi: 10.1289/ehp.929813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baccichet A, Sinnett D. Br. J. Haematol. 1997;99:107–114. doi: 10.1046/j.1365-2141.1997.3663180.x. [DOI] [PubMed] [Google Scholar]
- Barbacid M. Annu. Rev. Biochem. 1987;56:779–827. doi: 10.1146/annurev.bi.56.070187.004023. [DOI] [PubMed] [Google Scholar]
- Beaupre DM, Kurzrock R. J. Clin. Oncol. 1999;17:1071–1079. doi: 10.1200/JCO.1999.17.3.1071. [DOI] [PubMed] [Google Scholar]
- Beaupre DM, Talpaz M, Marini FC, III, Cristiano RJ, Roth JA, Estrov Z, Albitar M, Freedman MH, Kurzrock R. Cancer Res. 1999;59:2971–2980. [PubMed] [Google Scholar]
- Blin N, Stafford DW. Nucleic Acids Res. 1976;3:2303–2308. doi: 10.1093/nar/3.9.2303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bos JL. Cancer Res. 1989;49:4682–4689. [PubMed] [Google Scholar]
- Bremner R, Balmain A. Cell. 1990;61:407–417. doi: 10.1016/0092-8674(90)90523-h. [DOI] [PubMed] [Google Scholar]
- Buchmann A, Ruggeri B, Klein-Szanto AJ, Balmain A. Cancer Res. 1991;51:4097–4101. [PubMed] [Google Scholar]
- Burmer GC, Rabinovitch PS, Loeb LA. Environ. Health Perspect. 1991;93:27–31. doi: 10.1289/ehp.919327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Gregorio L, Manenti G, Incarbone M, Pilotti S, Pastorino U, Pierotti MA, Dragani TA. Int. J. Cancer. 1998;79:269–272. doi: 10.1002/(sici)1097-0215(19980619)79:3<269::aid-ijc10>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- Dragani TA, Hirohashi S, Juji T, Kawajiri K, Kihara M, Ono-Kihara M, Manenti G, Nomoto T, Sugimura H, Genka K, Yokota J, Takahashi T, Mitsudomi T, Nagao M. Cancer Res. 2000;15:5017–5020. [PubMed] [Google Scholar]
- Gariboldi M, Manenti G, Canzian F, Falvella FS, Radice M, Pierotti MA, Della Porta G, Binelli G, Dragani TA. Nat. Genet. 1993;3:132–136. doi: 10.1038/ng0293-132. [DOI] [PubMed] [Google Scholar]
- Hegi ME, Devereux TR, Dietrich WF, Cochran CJ, Lander ES, Foley JF, Maronpot RR, Anderson MW, Wiseman RW. Cancer Res. 1994;54:6257–6264. [PubMed] [Google Scholar]
- Kiaris H, Spandidos DA. Int. J. Oncol. 1995;7:413–421. [PubMed] [Google Scholar]
- Kibel AS, Schutte M, Kern SE, Isaacs WB, Bova GS. Cancer Res. 1998;58:5652–5565. [PubMed] [Google Scholar]
- Li S, Rosell R, Urban A, Font A, Ariza A, Armengol P, Abad A, Navas JJ, Monzo M. Lung Cancer. 1994;11:19–27. doi: 10.1016/0169-5002(94)90279-8. [DOI] [PubMed] [Google Scholar]
- Manenti G, Gariboldi M, Fiorino A, Zedda AI, Pierotti MA, Dragani TA. Mamm. Genome. 1997;8:801–804. doi: 10.1007/s003359900582. [DOI] [PubMed] [Google Scholar]
- Mariyama M, Kishi K, Nakamura K, Obata H, Nishimura S. Jpn. J. Cancer Res. 1989;80:622–626. doi: 10.1111/j.1349-7006.1989.tb01687.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall CJ. Trends Genet. 1991;7:91–95. doi: 10.1016/0168-9525(91)90278-X. [DOI] [PubMed] [Google Scholar]
- Mills NE, Fishman CL, Rom WN, Dubin N, Jacobson DR. Cancer Res. 1995;55:1444–1447. [PubMed] [Google Scholar]
- Perucho M, Goldfarb M, Shimizu K, Lama C, Fogh J, Wigler M. Cell. 1981;27:467–476. doi: 10.1016/0092-8674(81)90388-3. [DOI] [PubMed] [Google Scholar]
- Pinto MM, Emanuel JR, Chaturvedi V, Costa J. Acta. Cytol. 1997;41:427–434. doi: 10.1159/000332535. [DOI] [PubMed] [Google Scholar]
- Reynolds SH, Anna CK, Brown KC, Wiest JS, Beattie EJ, Pero RW, Iglehart JD, Anderson MW. Proc. Natl. Acad. Sci. USA. 1991;88:1085–1089. doi: 10.1073/pnas.88.4.1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodenhuis S, Slebos RJ. Cancer Res. 1992;52:2665s–2669s. [PubMed] [Google Scholar]
- Rodenhuis S, Slebos RJ, Boot AJ, Evers SG, Mooi WJ, Wagenaar SS, van Bodegom PC, Bos JL. Cancer Res. 1988;48:5738–5741. [PubMed] [Google Scholar]
- Shibata D, Almoguera C, Forrester K, Dunitz J, Martin SE, Cosgrove MM, Perucho M, Arnheimn N. Cancer Res. 1990;50:1279–1283. [PubMed] [Google Scholar]
- Suzuki Y, Orita M, Shiraishi M, Hayashi K, Sekiya T. Oncogene. 1990;5:1037–1043. [PubMed] [Google Scholar]
- Takeuchi S, Bartram CR, Miller CW, Reiter A, Seriu T, Zimmerann M, Schrappe M, Mori N, Slater J, Miyoshi I, Koeffler HP. Blood. 1996a;87:3368–3374. [PubMed] [Google Scholar]
- Takeuchi S, Mori N, Koike M, Slater J, Park S, Miller CW, Miyoshi I, Koeffler HP. Cancer Res. 1996b;56:738–740. [PubMed] [Google Scholar]
- Thompson TA, Haag JD, Lindstrom MJ, Griep AE, Lohse JK, Gould MN. Oncogene. 2002;21:2797–2804. doi: 10.1038/sj.onc.1205391. [DOI] [PubMed] [Google Scholar]
- Vogelstein B, Fearon ER, Hamilton SR, Kern SE, Preisinger AC, Leppert M, Nakamura Y, White R, Smits AM, Bos JL. N. Engl. J. Med. 1988;319:525–532. doi: 10.1056/NEJM198809013190901. [DOI] [PubMed] [Google Scholar]
- Wang Y, Stoner G, You M. Cancer Res. 1993;53:1620–1624. [PubMed] [Google Scholar]
- Yanagitani N, Kohno T, Sunaga N, Kunitoh H, Tamura T, Tsuchiya S, Saito R, Yokota J. Carcinogenesis. 2002;23:1177–1183. doi: 10.1093/carcin/23.7.1177. [DOI] [PubMed] [Google Scholar]
- You M, Wang Y, Stoner G, You L, Maronpot R, Reynolds SH, Anderson M. Proc. Natl. Acad. Sci. USA. 1992;89:5804–5808. doi: 10.1073/pnas.89.13.5804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Z, Wang Y, Vikis HG, Johnson L, Liu G, Li J, Anderson MW, Sills RC, Hong HL, Devereux TR, Jacks T, Guan KL, You M. Nat. Genet. 2001;29:25–33. doi: 10.1038/ng721. [DOI] [PubMed] [Google Scholar]