Abstract
Background
Many studies have linked depression and obesity; few have more than two assessments of depressive symptoms and adiposity to address the potential bi-directional relation between adiposity and depressive symptoms from young adulthood through old age. We test whether baseline depressive symptoms are associated with changes in weight, whether baseline adiposity is associated with changes in depressive symptoms, and whether these associations vary by sex.
Methods
Participants (N=2,251; 47% female) were from the Baltimore Longitudinal Study of Aging. Using Hierarchical Linear Modeling on 30 years of data, the trajectory of adiposity and depressive symptoms over adulthood was estimated from >10,000 observations (M=4.5 assessments per participant) of body mass index (BMI; kg/m2), waist circumference, and hip circumference and >10,000 observations (M=4.5 assessments per participant) of the Center for Epidemiological Studies Depression scale. Baseline depressive symptoms and adiposity were then tested as predictors of the trajectory of adiposity and depressive symptoms, respectively. Additional analyses tested for sex-specific associations.
Results
Sex moderated the association between depressive symptoms and weight gain such that women who experienced depressed affect had greater increases in BMI (binteraction=.12, SE=.04), waist (binteraction=.22, SE=.10) and hip circumference (binteraction=.20, SE=.07) across adulthood, controlling for relevant demographic and behavioral covariates. Baseline adiposity was unrelated to the trajectory of depressive symptoms (Median b=.00) for both sexes.
Conclusions
Women who experience symptoms of depression tend to gain more weight across adulthood than men who experience such symptoms. Whether an individual was normal weight or overweight was unrelated to changes in depressive symptoms across adulthood.
In the United States, approximately 1 in 3 adults is obese (Flegal et al., 2010). The obesity epidemic is not limited to the US as the prevalence of overweight and obesity has increased worldwide in both affluent and less affluent nations (Haslam & James, 2005, WHO, 2000). Obesity is associated with a range of physical and psychological outcomes, including diabetes, hypertension, and heart disease (Malnick & Knobler, 2006), and may ultimately contribute to premature mortality (Adams et al., 2006, Flegal et al., 2005). Psychologically, obese individuals may be at greater risk for depression (Luppino et al., 2010) and may face discrimination in settings ranging from the work place to the doctor’s office (Puhl & Heuer, 2009). Although depression is often considered a result of obesity (Anderson et al., 2007, Bjerkeset et al., 2008), longitudinal research indicates that depression and symptoms of depression can increase risk of obesity and weight gain (Luppino et al., 2010, Richardson et al., 2003, Vogelzangs et al., 2008). The present research addresses the mutual relation between adiposity and depressive symptoms across the adult lifespan.
Most longitudinal research has addressed the question of whether depressive symptoms at baseline predict obesity at follow-up. Comparatively fewer longitudinal studies have assessed both depressive symptoms and adiposity at multiple points in time to test how baseline depression is associated with the trajectory of adiposity and none have addressed this relation with multiple assessments past age 50. One study of younger adults found that baseline depressive symptoms were associated with small increases in waist circumference, but not body mass index (BMI) (Needham et al., 2010). This study only included younger adults (mean age about 30 at baseline), and since the effect of depression on obesity may be cumulative (Kivimäki et al., 2009), this effect may be stronger in middle and older ages. Thus, multiple assessments over a broad age range are needed to test for potential non-linear changes over time.
In addition to the effect of depressive symptoms on the trajectory of adiposity, weight may also be associated with the trajectory of depressive symptoms. Symptoms of depression tend to follow a U-shaped curve across adulthood, with younger and older adults reporting more symptoms of depression than more middle-aged adults (Sutin et al., 2012). Similar to the effect of depression on weight, longitudinal research has focused primarily on predicting incident depression (Anderson et al., 2007, Kasen et al., 2008) and depressive symptoms (Bjerkeset et al., 2008, Herva et al., 2006) from baseline weight. Although there is support for obesity as a predictor of subsequent major depression (Anderson et al., 2007, Kasen et al., 2008), among younger adults, baseline adiposity tends to be unrelated to the trajectory of depressive symptoms (Needham et al., 2010). The first aim of this research is to test whether depressive symptoms are associated with the trajectory of adiposity and whether adiposity is associated with the trajectory of depressive symptoms across the adult lifespan.
A second aim is to test whether the association between depressive symptoms and changes in weight is stronger for women than men. Obese women are more likely than obese men to have suffered major depression (Onyike et al., 2003, Beydoun & Wang, 2010) and depressive symptoms (Gaysina et al., in press, Zaninotto et al., 2010, Heo et al., 2006, Dragan & Akhtar-Danesh, 2007). The association may even be reversed for men (Beydoun & Wang, 2010, Carpenter et al., 2000). Carpenter and colleagues (Carpenter et al., 2000), for example, found that obese men had a lower risk of past year major depressive disorder (MDD), whereas obese women were at greater risk. A systematic review of the literature (Atlantis & Baker, 2008) and a meta-analysis (de Wit et al., 2010) indicated that the association between symptoms of depression and obesity is stronger among women than men. Not all studies, however, find this sex difference (e.g., Luppino et al., 2010, Simon et al., 2006).
With more than 10,000 observations of both BMI and depressive symptoms, we use hierarchical linear modeling (HLM) and cross-lagged models to test whether baseline depressive symptoms are associated with the trajectory of BMI and vice versa. We take a comprehensive approach by also including two additional measures of adiposity (waist and hip circumference) and four symptom subscales (depressed affect, well-being, somatic complaints, and interpersonal problems). Finally, we test sex as a moderator of the longitudinal relation between depressive symptoms and adiposity.
Method
Participants
Participants (N = 2,251) were drawn from the Baltimore Longitudinal Study of Aging (BLSA), an ongoing multidisciplinary study of normal aging performed by the National Institute on Aging. Participants in the BLSA are generally healthy and educated (M = 16.47 years of education, SD=2.42); the present sample is 74% White, 20% Black, and 6% other ethnicity and 47% women. Basic anthropometric measures (see below) were available on all participants since the BLSA’s inception; administration of the current depressive symptoms measure (see below) started in 1979. The mean age at the first assessment of the CES-D was 57.85 (SD = 17.06; range = 19 to 95) and the mean age at the most recent assessment was 65.54 years (SD = 16.08; range 19 to 99). The local Institutional Review Board approved the study and all participants provided written informed consent before each assessment.
Depressive Symptoms
Depressive symptoms were measured with the Center for Epidemiologic Studies Depression Scale (CES-D; Radloff, 1977). This 20-item scale assesses the frequency of depressive symptoms within the previous week. Items are rated on a four-point scale from 0 (rarely) to 3 (most or all of the time). In addition to the total scale score, four subscales tap into different aspects of depressive symptoms (Hertzog et al., 1990, Radloff, 1977): Depressed Affect (e.g., “I felt sad.”), Well-Being (e.g., “I enjoyed life.”), Somatic Complaints (e.g., “My sleep was restless.”), and Interpersonal Problems (e.g., “I felt that people disliked me.”). The CES-D is a reliable, valid, and widely-used measure of depressive symptoms (Gatz & Hurwicz, 1990, Lewinsohn et al., 1997). The CES-D correlates with other measures of depressive symptoms and interviews assessing clinical depression (Roberts & Vernon, 1983, Weissman et al., 1977) and has an internal consistency typically between .80 and .90 (Naughton & Wiklund, 1993). Previous investigations of the factor structure have found the four-factor solution a good fit to the data, indicating that the CES-D measures four aspects of depressive symptoms (Knight et al., 1997). Participants had up to 19 assessments of depressive symptoms (M assessments per participant = 4.49, SD = 3.49, range = 1 to 19) approximately 2.5 years apart (M interval = 2.46, SD = 1.78) for a total of 10,075 assessments. At baseline, the CES-D had a mean of 7.05 (SD=6.92), Depressed Affect had a mean of 1.21 (SD=2.11), Well-Being had a mean of 9.88 (SD=3.06), Somatic Complaints had a mean of 2.64 (SD=2.58) and Interpersonal Problems had a mean of .24 (SD=.67).
Participants who had only one CES-D assessment (21%) were more likely to be of an ethnicity other than white or African American (χ2 = 33.08, p < .01), but there were no differences in age (F(1,2250) = .14, ns), education (F(1,2250) = 2.70, ns), or sex (χ2 = 2.19, ns). Controlling for age, sex, education, and ethnicity, those who had only one assessment of the CES-D scored higher on depressive symptoms than those who had repeated CES-D assessments (M = 8.29 [SE = .32] versus M = 6.60 [SE = .16], p < 01).
Anthropometric assessments
Participants’ weight and height were measured and recorded by trained staff clinicians and BMI was derived as kg/m2. Weight and hip circumferences were obtained with a flexible tape measure, manipulated to maintain close contact with the skin without compression of underlying tissues. Waist circumference was defined as the minimal abdominal perimeter located halfway between the rib cage and the pelvic crest. Hip circumference was defined as the point of maximal protrusion of the gluteal muscles and, in the anterior plane, the symphysis of the pubis. For participants who had at least one assessment of depressive symptoms, there were 10,049 assessments of height and weight concurrent and subsequent to the initial CES-D assessment (M assessments per participant = 4.46, SD=2.96, range = 1 to 16; M interval between assessments = 2.51 years, SD=1.47, range 0 to 20), 9,542 assessments of waist circumference (M assessments per participant = 4.29, SD=2.83, range = 1 to 16; M interval between assessments = 2.00 years, SD=1.77, range 0 to 20), and 9, 494 assessments of hip circumference (M assessments per participant = 4.29, SD=2.82, range = 1 to 16; M interval between assessments = 1.99 years, SD=1.71, range 0 to 18). At baseline, BMI had a mean of 25.94 (SD=4.42), waist circumference had a mean of 86.92 cm (SD=12.96), and hip circumference had a mean of 100.85 cm (SD=8.72).
Statistical overview
We used two approaches, hierarchical linear modeling (HLM) and cross-lagged models, to test whether depressive symptoms were associated with change in adiposity, and vice versa across adulthood. First, we used HLM (Raudenbush & Bryk, 2002, Singer & Willett, 2003) to model change in adiposity and depressive symptoms over time. HLM is a flexible approach that can be applied to evaluate within-individual change or growth trajectories. In HLM analyses, the number and spacing of measurement observations may vary among persons, given that the time-series observations in each individual are used to estimate each individual’s trajectory (Level 1), and those individual parameters are the basis of the population estimates (Level 2). Even data from individuals who were tested on only a single occasion can be used to stabilize estimates of the mean and variance. In this way, all available data can be included in the analyses. This is a major advantage of conducting analyses within the HLM framework; by contrast, missing data and varying timing pose major problems in conventional repeated measures analyses of variance (ANOVA). Furthermore, longitudinal HLM can estimate age trajectories over a broad age span with data collected in a relatively shorter time interval.
We conducted the analyses using HLM Version 6 (Raudenbush et al., 2004). To evaluate the longitudinal trajectories, we first defined the Level 1 model and then tested possible Level 2 predictors. At Level 1, we fit a quadratic model for each of the adiposity measures because of the established non-linear changes in weight across the lifespan (Drøyvold et al., 2006, Rissanen et al., 1988). We also included antidepressant medication use (5% on antidepressants at any time during the study) and smoking status (2.2% current smokers at any time during the study) as time-varying covariates at Level 1. At Level 2, we entered characteristics of the individual as independent variables to explain between-subjects variation in the intercept and the linear slope. Specifically, we tested sex, ethnicity, education, and the first assessment of depressive symptoms as Level 2 predictors of both the intercept and linear slope. Supplementary analyses controlled for women who reported ever being on hormone therapy (58% of women with data available on hormone therapy). We centered age in decades on the grand mean ([age - 65.54 years]/10) to minimize the correlation between the linear and quadratic terms. The equations for the models were:
Where γ0 is the estimated intercept, γ1 is the estimated linear slope, and γ2 is the estimated quadratic slope. We fit a similar set of models to test for the association between baseline adiposity and the trajectory of depressive symptoms. At Level 1, we again fit a quadratic model for the CES-D because of non-linear changes in depressive symptoms across the lifespan (Sutin et al., 2012), and we included antidepressant medication use and smoking as time-varying covariates. At Level 2, we tested sex, ethnicity, education, and each of the adiposity measures (BMI, waist circumference, and hip circumference) as predictors of the intercept and linear slope of the total CES-D and for each of the subscales. Due to the large number of statistical tests, we set p to < .01.
In addition to HLM, we also used cross-lagged models (Ferrer & McArdle, 2003, Jöreskog & Sörbom, 1979) to examine the potential bi-directional relation between depressive symptoms and weight. For all participants with two or more assessments of both weight and depressive symptoms measured concurrently (N = 1,759), we used the first (Time 1) and the last (Time 2) assessments. Each variable at Time 2 was specified as a function of three components: (1) an autoregression (β), representing the effect of the same variable at baseline; (2) a cross-lagged regression (γ), representing the effect of the other variable at baseline; and (3) a residual (d), which is allowed to correlate with the residual of the other variable. All cross-lagged models controlled for age, sex, ethnicity, education, antidepressant use, and smoking. We used Mplus (Muthén & Muthén, 2008) to test the cross-lagged models.
Results
Baseline Depressive Symptoms and the Trajectory of Adiposity
Consistent with previous analyses on this sample (Sutin et al., 2011) and others (Clarke et al., 2009), both the linear and quadratic terms were significant for each adiposity measure (Table 1). These terms indicated that, on average, participants tended to gain weight across adulthood, with a slight plateau in old age.
Table 1.
HLM Coefficients and Variance Estimates of Intercept, Linear, and Quadratic Equations Predicting Adiposity from Age in Decades
| Component | BMI | Waist | Hip |
|---|---|---|---|
| σ2: Residual within-subject variance | 1.52** | 22.87** | 14.88** |
| Intercept | |||
| γ00: Mean | 27.43 (.11)** | 92.21 (.29)** | 103.32 (.23)** |
| u0: Variance | 21.89** | 144.67** | 85.58** |
| Linear Slope | |||
| γ10: Mean | .36 (.04)** | 2.48 (.76)** | 1.03 (.10**) |
| u1: Variance | 1.87** | 5.44** | 5.83** |
| Quadratic Slope | |||
| γ20: Mean | −.29 (.02)** | −.66 (.04)** | −.24 (.03)** |
Note. N = 2,251 for BMI, N = 2225 for Waist, and N = 2212 for Hip. Standard errors are shown in parenthesis. HLM = hierarchical linear modeling; BMI = Body Mass Index.
p < .01.
Contrary to expectation, the total scale score for the CES-D was unrelated to change in BMI and waist circumference (Table 2). The CES-D had a small negative relation with the slope of hip circumference: Participants who experienced depressive symptoms gained less weight on their hips across adulthood. This association was likely due to the reverse-scored items related to positive affect included in the total CES-D scale score. That is, the Well-Being subscale was associated with hip circumference: Participants who reported experiencing positive emotions increased more in hip circumference across adulthood. There were no other significant associations between the subscales of the CES-D and the trajectory of any of the three measures of adiposity. We also tested whether depressive symptoms were associated with the trajectory of waist-hip ratio (WHR) because of its association with disease phenotypes. The total CES-D scale score and all of the subscales were unrelated to the slope of WHR (all bs = .00).
Table 2.
CES-D Predictors of the Slope of Three Measures of Adiposity
| CES-D | BMI | Waist | Hip |
|---|---|---|---|
| Total Scale Score | .00 (.01)a | −.03 (.01) | −.04 (.01)** |
| Depressive Affect | .03 (.02)a | .00 (.05) a | .01 (.04)a |
| Well-Being | .01 (.01) | .06 (.03) | .11 (.03)** |
| Somatic | .00 (.02) | −.06 (.04) | −.06 (.04) |
| Interpersonal | −.01 (.06) | −.08 (.15) | .06 (.14) |
Note. N = 2251 for BMI; N = 2225 for waist, and N = 2212 for hip. Standard errors are shown in parenthesis. Coefficients are applied to (age - mean age) in decades. BMI = Body Mass Index.
Significant interaction with sex.
p < .01.
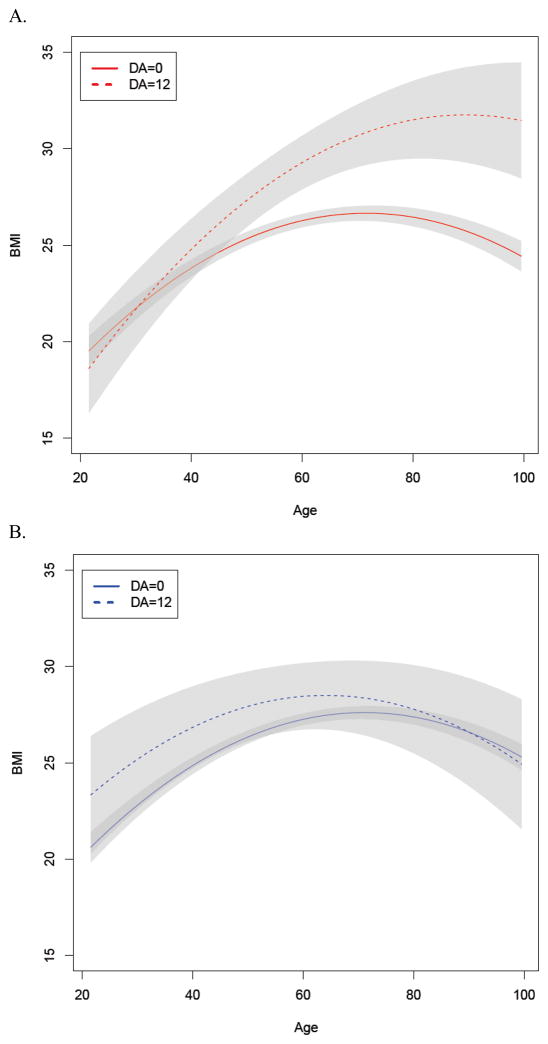
The association between depressive symptoms and the trajectory of adiposity was, however, moderated by sex. Interestingly, depressive symptoms had the opposite effect on the trajectory of BMI for men and women (bCES-DxSex=.03 [SE=.01], p<.01). Among women, increasing depressive symptoms was associated with more weight gain across the lifespan. In contrast, men who experienced depressive symptoms, although initially heavier in younger adulthood, gained less weight over time than men who did not experience such symptoms. The analyses of the subscales of the CES-D revealed that the association at the full-scale level was due to Depressed Affect (see Figure): Women who experienced depressive affect gained more weight, whereas men who experienced depressive affect gained less (bDAxSex = .12 [SE=.04], p<.01). A similar pattern emerged for waist (bDAxSex = .22 [SE=.10]) and hip (bDAxSex = .20 [SE=.08]) circumference. These findings were virtually identical when controlling for hormone therapy use among women. Sex did not moderate the association between the other aspects of depressive symptoms and adiposity. In addition, neither ethnicity nor education moderated the effect of depressive symptoms on the trajectory of any of the adiposity measures.
Figure.
Estimated trajectories of BMI plotted separately for a baseline Depressed Affect score of 0 and a baseline Depressed Affect score of 12 for women (A) and men (B).
We next tested whether having ever experienced severe depressive symptoms (CES-D ≥16, Beekman et al., 1997) at any point during the study period was associated with the trajectory of adiposity. Participants who had experienced at least one such episode increased more in BMI across adulthood than participants who had not experienced such symptoms (b = .24 [SE = .09], p<.01). Similar to the above analyses, there was an interaction with sex, such that this association was only apparent among female participants (b = .37 [SE = .14], p = .01). Severe depressive symptoms were unrelated to the trajectory of waist and hip circumference.
Finally, we used cross-lagged models as a second way of testing the association between depressive symptoms and weight over time. Similar to the HLM analyses, the total CES-D was unrelated to changes in BMI over time (γ = .01, ns). Also consistent with the HLM analyses, Depressed Affect was associated with greater increases in BMI (γ = .03) and this effect was moderated by sex: Depressed Affect was associated with weight gain among women (γ = .06, p < .01) but not among men (γ = −.01, ns). In contrast to the HLM analyses, the Well-Being subscale was associated with increases in waist circumference (γ = .04, p < .01), but neither the total CES-D (γ = −.01, ns) nor Well-Being (γ = .00, ns) was associated with increases in hip circumference. There were no other effects of depressive symptoms on change in weight.
Adiposity and the Trajectory of Depressive Symptoms
Consistent with previous research on this sample (Sutin et al., 2012) and others (Needham et al., 2010), the estimated trajectory of depressive symptoms was curvilinear (Table 3). That is, both the linear and the quadratic terms were significant: Depressive symptoms decreased from early to middle adulthood, but then gradually increased again in older adulthood. BMI, waist circumference, and hip circumference were unrelated to the trajectory of depressive symptoms, measured both as the total CES-D score and the four subscales (Median estimate = .00; range .00 to .01). Sex, ethnicity, and education did not moderate the effect of adiposity on the trajectory of depressive symptoms. The cross-lagged models also indicated no relation between any of the measures of adiposity and changes in depressive symptoms over time (Median estimate = .01; range −.01 to .03).
Table 3.
HLM Coefficients and Variance Estimates of Intercept, Linear, and Quadratic Equations Predicting Depressive Symptoms from Age in Decades
| Component | Total CES-D | Depressed Affect | Well-Being | Somatic | Interpersonal |
|---|---|---|---|---|---|
| σ2: Residual within-subject variance | 20.92** | 2.39** | 3.49** | 3.74** | .29** |
| Intercept | |||||
| γ00: Mean | 5.86 (.12)** | .88 (.03)** | 10.34 (.05)** | 2.44 (.05)** | .17 (01)** |
| u0: Variance | 14.09** | .72** | 2.19** | 2.22** | .05** |
| Linear Slope | |||||
| γ10: Mean | .49 (.07)** | .03 (.02) | −.08 (.02)** | .29 (.03)** | −.01 (.01) |
| u1: Variance | 2.92** | .31** | .18** | .32** | .02** |
| Quadratic Slope | |||||
| γ20: Mean | .41 (.03)** | .11 (.01)** | −.04 (.01)** | .17 (.01)** | .02 (.00)** |
Note. N = 2,251. Standard errors are shown in parenthesis. HLM = hierarchical linear modeling.
p < .01.
Discussion
We used data from a long-running longitudinal study of community-dwelling volunteers to address several questions about the nature of the relation between depressive symptoms and adiposity across adulthood. We found that women who experienced depressive symptoms, specifically depressed affect, gained more weight across adulthood than women who did not experience such symptoms, whereas the opposite pattern emerged for men. Adiposity was unrelated to the trajectory of depressive symptoms across adulthood.
Across the lifespan, women are at greater risk for experiencing depressive symptoms and disorders (Angst et al., 2009, Piccinelli & Wilkinson, 2000). Women also tend to gain more weight on average across adulthood than men (Williamson, 1993). Interestingly, the effect of depressive symptoms on weight gain for women was more pronounced in middle age. That is, the estimated trajectory of BMI was similar for women experiencing depressive symptoms and symptom-free women until around midlife, at which point women who experienced depressive symptoms gained weight more rapidly than women without such symptoms. Of note, controlling for hormone therapy did not change the results. Thus, among women, depressive symptoms may exacerbate the weight gain associated with normal aging, particularly the effects of menopause. This finding also suggests that the effect of depression on adiposity and potential sex differences may not become apparent until middle and older ages. Indeed, the effect of depression on obesity may be cumulative (Kivimäki et al., 2009), and multiple assessments over a long period of time may be necessary to uncover such effects (Luppino et al., 2010). Of note, Needham and colleagues (Needham et al., 2010) did not find sex-specific effects of depressive symptoms on increases in adiposity among younger adults. The age of participants at their last assessment, however, was about the same time that sex differences started to emerge in the present study.
Sex differences in the behavioral correlates of depression may contribute to greater weight gain for women than men. Among individuals suffering from atypical depression, for example, women are more likely to report overeating and extreme fatigue than men (Angst et al., 2002b). Among individuals suffering from MDD, compared to men, women are more likely to experience increased appetite and a loss of interest in pleasurable activities (Romans et al., 2007). Among individuals suffering from depressive symptoms, women are more likely to report changes in appetite, feelings of fatigue, and difficulty sleeping than are men (Angst et al., 2002a). Finally, to cope with symptoms of depression, men are more likely to engage in sports and other hobbies, whereas women are more likely to be prescribed antidepressant medication (Angst et al., 2002a). Depressed women may be more vulnerable to weight gain than depressed men because their most common behavioral expressions of depression are the two most common risk factors for weight gain: overeating and physical inactivity. In addition, poor sleep quality (Gangwisch et al., 2005, Spiegel et al., 2005) and antidepressant medication (Fava, 2000) have both been associated with weight gain.
Biological mechanisms may also contribute to the association between depressive symptoms and weight gain among women. Activity of the hypothalamic-pituitary-adrenal (HPA) axis has been implicated in both depression and obesity. When faced with a stressor, the cortisol response increases with age, and this increase is three times stronger for women than men (Otte et al., 2005). Resting cortisol among women suffering from MDD increases with age, starting in about middle adulthood (Akil et al., 1993). Such hyperactivity of the HPA axis has been implicated in weight gain over time (Vicennati et al., 2009). This weight gain may also contribute to the link between depressive symptoms and chronic diseases, such as cardiovascular disease and diabetes.
At the sample-level, the total CES-D scale score was primarily unrelated to the trajectory of the three measures of adiposity. The subscale analyses, however, revealed that both negative and positive affect were associated with weight gain. Among women, weight gain was particularly tied to feelings of sadness and loneliness. Somewhat surprisingly, the Well-Being subscale was also associated with increases in hip circumference (HLM analysis) and waist circumference (cross-lagged analysis) over time. The Depressed Affect and Well-Being subscales have higher internal consistencies than either the Somatic Complaints or Interpersonal Problems subscales; thus, the associations between adiposity and the affective dimensions may be more robust than the more heterogeneous subscales. Of note, the Somatic Complaints subscale of the CES-D was unrelated to weight gain, which is surprising given that these items tap into the physical manifestations of depression, including changes in appetite.
Sadness and happiness are often assumed to lie on opposite sides of the same continuum, but evidence suggests that negative and positive affect are two independent dimensions (Watson et al., 1988). Their correlates, therefore, may not necessarily go in opposite directions; they may be similar. In the current study, Depressed Affect and Well-Being did share similar associations with weight gain, which obscured the association between weight gain and the total CES-D scale score because the items that measured well-being were reverse scored into the total score. These findings suggest that emotionality, rather than the valence of the emotion per se, is associated with weight gain.
The relation between emotions and weight is certainly complex and both negative and positive emotions can lead to increases in food consumption (Macht, 2008). For example, depressed mood may lead to greater food intake in an attempt to regulate emotions (Chua et al., 2004), whereas positive emotions increase the pleasantness of food (Macht et al., 2002). Although some have found that experiencing positive mood can lead to increases in food consumption (Macht, 1999, Patel & Schlundt, 2001), others find positive affect to be unrelated to eating behavior and weight gain (Cyders & Smith, 2008). Thus, the association between Well-Being and weight gain in the present study should be interpreted with caution, particularly given that this association did not extend to overall increases in BMI and the relations differed across analytical techniques.
Obesity increases risk of both clinical depression and severe depressive symptoms (Luppino et al., 2010). Obesity is a stigmatized condition, which, if internalized, could lead to feelings of low self-worth and depression (Ashmore et al., 2008, Hatzenbuehler et al., 2009). Body shape influences how individuals feel about themselves (Schwartz & Brownell, 2004), how they are perceived (Crandall, 1994, Roehling et al., 2008), and their interactions with others (Hebl & Mannix, 2003). In addition to the social pressures associated with weight, obese individuals may engage in fewer activities due to their weight, which reduces quality of life (Hassan et al., 2003). In the present research, however, we found no evidence that BMI or other measures of weight were associated with the trajectory of depressive symptoms; higher BMI was unrelated to greater increases in depressive symptoms across the adult lifespan. This finding complements previous research that found adiposity to be unrelated to changes in depressive symptoms across early adulthood (Needham et al., 2010).
This study had several strengths, including multiple assessments of depressive symptoms and adiposity across 30 years in individuals ranging from young adulthood through old age. This study also had limitations. Participants in the BLSA tend to be healthy and educated; our findings, however, are broadly consistent with previous research on young adults (Needham et al., 2010) and thus are unlikely to be sample specific. In addition, we considered the potential bidirectional association between adiposity and depressive symptoms, but similar relations may or may not be found for clinical disorders, such as major depression. Given that major depression follows a different trajectory across adulthood than depressive symptoms, the association with weight may also vary. Future research would benefit from assessments of clinical depression, other psychiatric conditions, as well as medical conditions that are commonly comorbid with depression and also associated with weight. Finally, we did not address the mechanisms through which depressive symptoms are associated with weight gain. Future research could test behavioral and/or physiological factors that may mediate the relation between depressive symptoms and increases in adiposity across adulthood.
With over 10,000 assessments of both BMI and depressive symptoms, we tested the nature of the relation between depressive symptoms and adiposity across the adult lifespan. Women who experienced depressed affect gained more weight over time, but there was no evidence that obesity increased depressive symptoms for either women or men. The present research suggests that, compared to men, women may suffer greater physiological costs of depressive symptoms with aging.
Acknowledgments
Funding/Support: This research was supported entirely by the Intramural Research Program of the NIH, National Institute on Aging.
Role of the funder: The funder had no role in the design and conduct of the study; in the collection, analysis, and interpretation of the data; or in the preparation, review, or the decision to submit.
Footnotes
Author contributions: Dr. Sutin had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Conflict of interest: The authors have no conflict of interest to report.
References
- Adams KF, Schatzkin A, Harris TB, Kipnis V, Mouw T, Ballard-Barbash R, Hollenbeck A, Leitzmann MF. Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old. New England Journal of Medicine. 2006;355:763–778. doi: 10.1056/NEJMoa055643. [DOI] [PubMed] [Google Scholar]
- Akil H, Haskett RF, Young EA, Grunhaus L, Kotun J, Weinberg V, Greden J, Watson SJ. Multiple HPA profiles in endogenous depression: Effect of age and sex on cortisol and beta-endorphin. Biological Psychiatry. 1993;33:73–85. doi: 10.1016/0006-3223(93)90305-w. [DOI] [PubMed] [Google Scholar]
- Anderson SE, Cohen P, Naumova EN, Jacques PF, Must A. Adolescent obesity and risk for subsequent major depressive disorder and anxiety disorder: Prospective evidence. Psychosomatic Medicine. 2007;69:740–747. doi: 10.1097/PSY.0b013e31815580b4. [DOI] [PubMed] [Google Scholar]
- Angst J, Gamma A, Gastpar M, Lépine JP, Mendlewicz J, Tylee A. Gender differences in depression: Epidemiological findings from the European DEPRES I and II studies. European Archives of Psychiatry and Clinical Neuroscience. 2002a;252:201–209. doi: 10.1007/s00406-002-0381-6. [DOI] [PubMed] [Google Scholar]
- Angst J, Gamma A, Rössler W, Ajdacic V, Klein DN. Long-term depression versus episodic major depression: Results from the prospective Zurich study of a community sample. Journal of Affective Disorders. 2009;115:112–121. doi: 10.1016/j.jad.2008.09.023. [DOI] [PubMed] [Google Scholar]
- Angst J, Gamma A, Sellaro R, Zhang H, Merikangas K. Toward validation of atypical depression in the community: Results of the Zurich cohort study. Journal of Affective Disorders. 2002b;72:125–138. doi: 10.1016/s0165-0327(02)00169-6. [DOI] [PubMed] [Google Scholar]
- Ashmore JA, Friedman KE, Reichmann SK, Musante GJ. Weight-based stigmatization, psychological distress, & binge eating behavior among obese treatment-seeking adults. Eating Behaviors. 2008;9:203–209. doi: 10.1016/j.eatbeh.2007.09.006. [DOI] [PubMed] [Google Scholar]
- Atlantis E, Baker M. Obesity effects on depression: Systematic review of epidemiological studies. International Journal of Obesity. 2008;32:881–891. doi: 10.1038/ijo.2008.54. [DOI] [PubMed] [Google Scholar]
- Beekman ATF, Deeg DJH, Van Limbeek J, Braam AW, De Vries MZ, Van Tilburg W. Criterion validity of the Center for Epidemiologic Studies Depression scale (CES-D): Results from a community-based sample of older subjects in the Netherlands. Psychological Medicine. 1997;27:231–235. doi: 10.1017/s0033291796003510. [DOI] [PubMed] [Google Scholar]
- Beydoun MA, Wang Y. Pathways linking socioeconomic status to obesity through depression and lifestyle factors among young US adults. Journal of Affective Disorders. 2010;123:52–63. doi: 10.1016/j.jad.2009.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjerkeset O, Romundstad P, Evans J, Gunnell D. Association of adult body mass index and height with anxiety, depression, and suicide in the general population: The HUNT study. American Journal of Epidemiology. 2008;167:193–202. doi: 10.1093/aje/kwm280. [DOI] [PubMed] [Google Scholar]
- Carpenter KM, Hasin DS, Allison DB, Faith MS. Relationships between obesity and DSM-IV major depressive disorder, suicide ideation, and suicide attempts: Results from a general population study. American Journal of Public Health. 2000;90:251–257. doi: 10.2105/ajph.90.2.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chua JL, Touyz S, Hill AJ. Negative mood-induced overeating in obese binge eaters: An experimental study. International Journal of Obesity. 2004;28:606–610. doi: 10.1038/sj.ijo.0802595. [DOI] [PubMed] [Google Scholar]
- Clarke P, O’malley PM, Johnston LD, Schulenberg JE. Social disparities in BMI trajectories across adulthood by gender, race/ethnicity and lifetime socio-economic position: 1986–2004. International Journal of Epidemiology. 2009;38:499–509. doi: 10.1093/ije/dyn214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crandall CS. Prejudice against fat people: Ideology and self-interest. Journal of Personality and Social Psychology. 1994;66:882–894. doi: 10.1037//0022-3514.66.5.882. [DOI] [PubMed] [Google Scholar]
- Cyders MA, Smith GT. Emotion-based dispositions to rash action: Positive and negative urgency. Psychological Bulletin. 2008;134:807–828. doi: 10.1037/a0013341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Wit L, Luppino F, Van Straten A, Penninx B, Zitman F, Cuijpers P. Depression and obesity: A meta-analysis of community-based studies. Psychiatry Research. 2010;178:230–235. doi: 10.1016/j.psychres.2009.04.015. [DOI] [PubMed] [Google Scholar]
- Dragan A, Akhtar-Danesh N. Relation between body mass index and depression: A structural equation modeling approach. BMC Medical Research Methodology. 2007:7. doi: 10.1186/1471-2288-7-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drøyvold WB, Nilsen TIL, Krüger Ø, Holmen TL, Krokstad S, Midthjell K, Holmen J. Change in height, weight and body mass index: Longitudinal data from the HUNT Study in Norway. International Journal of Obesity. 2006;30:935–939. doi: 10.1038/sj.ijo.0803178. [DOI] [PubMed] [Google Scholar]
- Fava M. Weight gain and antidepressants. Journal of Clinical Psychiatry. 2000;61:37–41. [PubMed] [Google Scholar]
- Ferrer E, Mcardle JJ. Alternative structural models for multivariate longitudinal data analysis. Structural Equation Modeling. 2003;10:493–524. [Google Scholar]
- Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA - Journal of the American Medical Association. 2010;303:235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity. Journal of the American Medical Association. 2005;293:1861–1867. doi: 10.1001/jama.293.15.1861. [DOI] [PubMed] [Google Scholar]
- Gangwisch JE, Malaspina D, Boden-Albala B, Heymsfield SB. Inadequate sleep as a risk factor for obesity: Analyses of the NHANES I. Sleep. 2005;28:1289–1296. doi: 10.1093/sleep/28.10.1289. [DOI] [PubMed] [Google Scholar]
- Gatz M, Hurwicz ML. Are old people more depressed? Cross-sectional data on Center for Epidemiological Studies Depression Scale factors. Psychology and Aging. 1990;5:284–290. doi: 10.1037//0882-7974.5.2.284. [DOI] [PubMed] [Google Scholar]
- Gaysina D, Hotopf M, Richards M, Colman I, Kuh D, Hardy R. Symptoms of depression and anxiety, and change in body mass index from adolescence to adulthood: results from a British birth cohort. Psychological Medicine. :1–10. doi: 10.1017/S0033291710000346. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haslam DW, James WPT. Obesity. Lancet. 2005;366:1197–1209. doi: 10.1016/S0140-6736(05)67483-1. [DOI] [PubMed] [Google Scholar]
- Hassan MK, Joshi AV, Madhavan SS, Amonkar MM. Obesity and health-related quality of life: A cross-sectional analysis of the US population. International Journal of Obesity. 2003;27:1227–1232. doi: 10.1038/sj.ijo.0802396. [DOI] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Keyes KM, Hasin DS. Associations between perceived weight discrimination and the prevalence of psychiatric disorders in the general population. Obesity. 2009;17:2033–2039. doi: 10.1038/oby.2009.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hebl MR, Mannix LM. The weight of obesity in evaluating others: A mere proximity effect. Personality and Social Psychology Bulletin. 2003;29:28–38. doi: 10.1177/0146167202238369. [DOI] [PubMed] [Google Scholar]
- Heo M, Pietrobelli A, Fontaine KR, Sirey JA, Faith MS. Depressive mood and obesity in US adults: Comparison and moderation by sex, age, and race. International Journal of Obesity. 2006;30:513–519. doi: 10.1038/sj.ijo.0803122. [DOI] [PubMed] [Google Scholar]
- Hertzog C, Van Alstine J, Usala PD, Hultsch DF, Dixon R. Measurement properties of the Center for Epidemiological Studies Depression Scale (CES-D) in older populations. Psychological Assessment. 1990;2:64–72. [Google Scholar]
- Herva A, Laitinen J, Miettunen J, Veijola J, Karvonen JT, Läksy K, Joukamaa M. Obesity and depression: Results from the longitudinal Northern Finland 1966 Birth Cohort Study. International Journal of Obesity. 2006;30:520–527. doi: 10.1038/sj.ijo.0803174. [DOI] [PubMed] [Google Scholar]
- Jöreskog KG, Sörbom D. Advances in factor analysis and structural equation models. Cambridge, MA: Abt Books; 1979. [Google Scholar]
- Kasen S, Cohen P, Chen H, Must A. Obesity and psychopathology in women: A three decade prospective study. International Journal of Obesity. 2008;32:558–566. doi: 10.1038/sj.ijo.0803736. [DOI] [PubMed] [Google Scholar]
- Kivimäki M, Lawlor DA, Singh-Manoux A, Batty GD, Ferrie JE, Shipley MJ, Nabi H, Sabia S, Marmot MG, Jokela M. Common mental disorder and obesity: insight from four repeat measures over 19 years: prospective Whitehall II cohort study. BMJ (Clinical research ed) 2009:339. doi: 10.1136/bmj.b3765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knight RG, Williams S, Mcgee R, Olaman S. Psychometric properties of the Centre for Epidemiologic Studies Depression Scale (CES-D) in a sample of women in middle life. Behaviour Research and Therapy. 1997;35:373–380. doi: 10.1016/s0005-7967(96)00107-6. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Seeley JR, Roberts RE, Allen NB. Center for epidemiologic studies depression scale (CES-D) as a screening instrument for depression among community-residing older adults. Psychology and Aging. 1997;12:277–287. doi: 10.1037//0882-7974.12.2.277. [DOI] [PubMed] [Google Scholar]
- Luppino FS, De Wit LM, Bouvy PF, Stijnen T, Cuijpers P, Penninx BWJH, Zitman FG. Overweight, obesity, and depression: A systematic review and meta-analysis of longitudinal studies. Archives of General Psychiatry. 2010;67:220–229. doi: 10.1001/archgenpsychiatry.2010.2. [DOI] [PubMed] [Google Scholar]
- Macht M. Characteristics of eating in anger, fear, sadness and joy. Appetite. 1999;33:129–139. doi: 10.1006/appe.1999.0236. [DOI] [PubMed] [Google Scholar]
- Macht M. How emotions affect eating: A five-way model. Appetite. 2008;50:1–11. doi: 10.1016/j.appet.2007.07.002. [DOI] [PubMed] [Google Scholar]
- Macht M, Roth S, Ellgring H. Chocolate eating in healthy men during experimentally induced sadness and joy. Appetite. 2002;39:147–158. doi: 10.1006/appe.2002.0499. [DOI] [PubMed] [Google Scholar]
- Malnick SDH, Knobler H. The medical complications of obesity. QJM. 2006;99:565–579. doi: 10.1093/qjmed/hcl085. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén B. Mplus user’s guide. Los Angeles CA: Muthén & Muthén; 2008. [Google Scholar]
- Naughton MJ, Wiklund I. A critical review of dimension-specific measures of health-related quality of life in cross-cultural research. Quality of Life Research. 1993;2:397–432. doi: 10.1007/BF00422216. [DOI] [PubMed] [Google Scholar]
- Needham BL, Epel ES, Adler NE, Kiefe C. Trajectories of change in obesity and symptoms of depression: The cardia study. American Journal of Public Health. 2010;100:1040–1046. doi: 10.2105/AJPH.2009.172809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onyike CU, Crum RM, Lee HB, Lyketsos CG, Eaton WW. Is obesity associated with major depression? Results from the Third National Health and Nutrition Examination Survey. American Journal of Epidemiology. 2003;158:1139–1147. doi: 10.1093/aje/kwg275. [DOI] [PubMed] [Google Scholar]
- Otte C, Hart S, Neylan TC, Marmar CR, Yaffe K, Mohr DC. A meta-analysis of cortisol response to challenge in human aging: Importance of gender. Psychoneuroendocrinology. 2005;30:80–91. doi: 10.1016/j.psyneuen.2004.06.002. [DOI] [PubMed] [Google Scholar]
- Patel KA, Schlundt DG. Impact of moods and social context on eating behavior. Appetite. 2001;36:111–118. doi: 10.1006/appe.2000.0385. [DOI] [PubMed] [Google Scholar]
- Piccinelli M, Wilkinson G. Gender differences in depression. Critical review. British Journal of Psychiatry. 2000;177:486–492. doi: 10.1192/bjp.177.6.486. [DOI] [PubMed] [Google Scholar]
- Puhl RM, Heuer CA. The stigma of obesity: A review and update. Obesity. 2009;17:941–964. doi: 10.1038/oby.2008.636. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measures. 1977;1:385–401. [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical linear models: Applications and data analysis methods. Thousand Oaks, CA: Sage; 2002. [Google Scholar]
- Raudenbush SW, Bryk AS, Congdon R. HLM. 6. Lincolnwood, IL: Scientific Software International; 2004. [Google Scholar]
- Richardson LP, Davis R, Poulton R, Mccauley E, Moffitt TE, Caspi A, Connell F. A longitudinal evaluation of adolescent depression and adult obesity. Archives of Pediatrics and Adolescent Medicine. 2003;157:739–745. doi: 10.1001/archpedi.157.8.739. [DOI] [PubMed] [Google Scholar]
- Rissanen A, Heliovaara M, Aromaa A. Overweight and anthropometric changes in adulthood: A prospective study of 17 000 Finns. International Journal of Obesity. 1988;12:391–401. [PubMed] [Google Scholar]
- Roberts RE, Vernon SW. The center for epidemiologic studies depression scale: Its use in a community sample. American Journal of Psychiatry. 1983;140:41–46. doi: 10.1176/ajp.140.1.41. [DOI] [PubMed] [Google Scholar]
- Roehling MV, Roehling PV, Odland LM. Investigating the validity of stereotypes about overweight employees: The relationship between body weight and normal personality traits. Group and Organization Management. 2008;33:392–424. [Google Scholar]
- Romans SE, Tyas J, Cohen MM, Silverstone T. Gender differences in the symptoms of major depressive disorder. Journal of Nervous and Mental Disease. 2007;195:905–911. doi: 10.1097/NMD.0b013e3181594cb7. [DOI] [PubMed] [Google Scholar]
- Schwartz MB, Brownell KD. Obesity and body image. Body Image. 2004;1:43–56. doi: 10.1016/S1740-1445(03)00007-X. [DOI] [PubMed] [Google Scholar]
- Simon GE, Von Korff M, Saunders K, Miglioretti DL, Crane PK, Van Belle G, Kessler RC. Association between obesity and psychiatric disorders in the US adult population. Archives of General Psychiatry. 2006;63:824–830. doi: 10.1001/archpsyc.63.7.824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer JD, Willett JB. Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence. New York: Oxford University Press; 2003. [Google Scholar]
- Spiegel K, Knutson K, Leproult R, Tasali E, Van Cauter E. Sleep loss: A novel risk factor for insulin resistance and Type 2 diabetes. Journal of Applied Physiology. 2005;99:2008–2019. doi: 10.1152/japplphysiol.00660.2005. [DOI] [PubMed] [Google Scholar]
- Sutin AR, Ferrucci L, Zonderman AB, Terracciano A. Personality and obesity across the adult lifespan. Journal of Personality and Social Psychology. 2011;101:579–592. doi: 10.1037/a0024286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutin AR, Terracciano A, Milaneschi Y, Ferrucci L, An Y, Zonderman AB. Longitudinal trajectory of depressive symptoms across the adult lifespan. 2012 doi: 10.1001/jamapsychiatry.2013.193. In preparation. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vicennati V, Pasqui F, Cavazza C, Pagotto U, Pasquali R. Stress-related development of obesity and cortisol in women. Obesity. 2009;17:1678–1683. doi: 10.1038/oby.2009.76. [DOI] [PubMed] [Google Scholar]
- Vogelzangs N, Kritchevsky SB, Beekman ATF, Newman AB, Satterfield S, Simonsick EM, Yaffe K, Harris TB, Penninx BWJH. Depressive symptoms and change in abdominal obesity in older persons. Archives of General Psychiatry. 2008;65:1386–1393. doi: 10.1001/archpsyc.65.12.1386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Sholomskas D, Pottenger M. Assessing depressive symptoms in five psychiatric populations: A validation study. American Journal of Epidemiology. 1977;106:203–214. doi: 10.1093/oxfordjournals.aje.a112455. [DOI] [PubMed] [Google Scholar]
- WHO. WHO Technical Report Series. Geneva: World Health Organization; 2000. Obesity: preventing and managing the global epidemic; p. 894. [PubMed] [Google Scholar]
- Williamson DF. Descriptive epidemiology of body weight and weight change in U.S. adults. Annals of Internal Medicine. 1993;119:646–649. doi: 10.7326/0003-4819-119-7_part_2-199310011-00004. [DOI] [PubMed] [Google Scholar]
- Zaninotto P, Pierce M, Breeze E, Oliveira CD, Kumari M. BMI and waist circumference as predictors of well-being in older adults: Findings from the English longitudinal study of ageing. Obesity. 2010;18:1981–1987. doi: 10.1038/oby.2009.497. [DOI] [PubMed] [Google Scholar]