Abstract
The safety and consistency of the care given to hospital inpatients has recently become a particular political and public concern. The traditional ‘ward round’ presents an obvious opportunity for systematically and collectively ensuring that proper standards of care are being achieved for individual patients. This paper describes the design and implementation of a ‘ward safety checklist’ that defines a set of potential risk factors that should be checked on a daily basis, and offers multidisciplinary teams a number of prompts for sharing and clarifying information between themselves, and with the patient, during a round. The concept of the checklist and the desire to improve ward rounds were well received in many teams, but the barriers to adoption were informative about the current culture on many inpatient wards. Although the ‘multidisciplinary ward round’ is widely accepted as good practice, the medical and nursing staff in many teams are failing to coordinate their workloads well enough to make multidisciplinary rounds a working reality. ‘Nursing’ and ‘medical’ care on the ward have become ‘de-coupled’ and the potential consequences for patient safety and good communication are largely self-evident. This problem is further complicated by a medical culture which values the primacy of clinical autonomy and as a result can be resistant to perceived attempts to ‘systematize’ medical care through instruments such as checklists.
Introduction
Predictably, the latest moves to reconfigure the National Health Service (NHS) have excited intense public and political debate.1 The service holds a uniquely sensitive position in the public sentiment, widely regarded as a source of national pride2 and apparently able to sustain high levels of patient satisfaction.3,4 Nonetheless, there are signs of a growing public, professional and regulatory unease about the ability of NHS Hospital Trusts to consistently deliver the most basic elements of inpatient care.5–7 While the service is demonstrably capable of delivering remarkable medical treatments to the very highest standards, it is simultaneously capable of allowing vulnerable people to come to harm through poor management of entirely avoidable risks – infection, dehydration, poor nutrition, pressure injury and deep vein thrombosis being obvious examples. Such failures usually have little to do with shortcomings in information and medical knowledge and, distressingly, are more often a function of poor communication, failure of teamwork and a silo mentality that complicates issues of ownership and accountability.
At University College London Hospitals (UCLH), our experience of supporting the implementation of the World Health Organization safe surgery checklist has prompted us to look at expanding the ‘checklist’ approach8 to the wider clinical context of inpatient care. While we agree that there is a need for more research about the effectiveness of clinical checklists,9 the experience of checklists in other safety-critical, ‘high reliability’ sectors such as aerospace, the military, transport and so on, and of consistent use in specific medical environments,10,11 continues to provide a persuasive argument for their potential. Thomassen,12 for instance, reports that even in a routine, well-established preanaesthetic induction pathway, one or more items from a 26-point checklist was missing in 17% of cases (range 4–46%). We also believe that, in the current economic climate, the avoidable costs associated with routine, ‘low level’ failure will come under increasing scrutiny. Semel et al.13 estimate that the costs of implementing and sustaining the WHO safe surgery checklist were recovered once the checklist had prevented just five serious clinical incidents. Similarly, the Keystone ICU programme, which incorporates the routine use of checklists, clearly demonstrated that improving patient care, by reducing number of catheter-related bloodstream infections, thereby generated a substantial healthcare cost-saving.14
Purpose and design
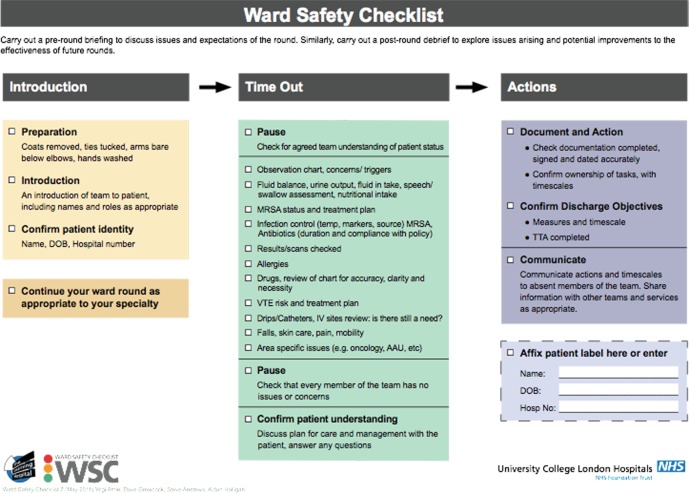
In designing the UCLH ward safety checklist (WSC) (Figure 1), we reviewed a number of proposed and existing experimental designs to create a design that broadly followed the format of the ‘safe surgery checklist.’ It comprises:
An ‘introduction’ dealing with preparation, patient identity, and staff and patient introductions;
A ‘time out’ stage: the basic ‘safety checklist’ element but giving staff a prompt to pause, check for a common understanding, review a list of common risk factors and then check the patient's own understanding of their care;
An ‘actions’ section equivalent to the surgery ‘sign out’ and dealing with issues of documentation, objective setting and ongoing actions and communication.
Figure 1.
The UCLH ward safety checklist
As with the Safe Surgery checklist (SSC), the WSC initiative did not seek to introduce any new medical or nursing knowledge or practice. All of the elements on the checklist are entirely familiar to the clinical professions, and many clinicians would assert that these checks are ‘done already’ and that a checklist is therefore superfluous. Nonetheless, the checklist items selected represent well known sources of risk if they are overlooked or not routinely checked and are often demonstrably involved in clinical incidents. The purpose of the checklist is to ensure that these risk items are checked consistently, and that there is good intra- and interprofessional communication about a patient's care, free from any negative impact of status or hierarchy.
However, in some important respects the WSC differs from the SSC. The SSC is integrated into a relatively well-structured, safety critical operating-theatre process, dealing principally with an unconscious patient. In contrast, basic inpatient care processes are generally less well defined. They deal principally with conscious and often anxious patients and carers, and in a context which is superficially not safety critical.
Implementation
Because of these differences and the particular sensitivities of inpatient care, we shaped the design and implementation of the WSC according to a number of key principles:
Ward round focused
The checklist can be used in a variety of contexts, as a personal aide memoire for clinicians, as a tool to guide handover between teams, or as a briefing template. But we describe and promote it principally as a tool for use by the multidisciplinary team in the context of a ward round.
Multidisciplinary
We resisted any move to have the checklist ‘assigned’ to one particular professional group, either in terms of a responsibility to implement it or as a specific operational role when it was in use. The ‘basic care’ and ‘checklist’ concepts led some to presuppose that the WSC represented a new ‘nursing task’. WSC implementation assumes a collective responsibility to adopt and use the checklist across all professions and disciplines, and does not specify particular roles.
‘No ticks, no signatures’
Similarly, we resisted expectations that the checklist would be rendered as a physical checklist to be ‘ticked’ and signed by a named clinician to form part of the patient's clinical record, as is the case with the SSC. Our concern was not to add to the workload of already saturated clinicians, and to avoid the suggestion that the checklist represents a mistrust of clinical competence. We do however suggest that the patients’ notes are documented to indicate that the WSC has been used at least once for each 24 period of inpatient stay, as a minimal addition to the daily notes. A paper based WSC is available with ‘tick boxes’ should teams choose to use it as a formal checklist, but the checklist is more commonly understood as a laminated folder insert or ‘credit card size’ prompt card worn behind ID badges.
Include the patient
Although designed principally with their safety in mind, there is always a risk that a checklist distracts clinicians’ personal attention away from properly interacting with the patient. It was for this reason that the WSC has specific prompts for proper patient introductions and ‘time outs’ during which the patient's understanding of their care is checked. WSC training sessions also deliberately included ward-based simulations using role-played patients, and we were reassured that almost all training groups maintained their principal focus on interacting appropriately with the patient.
Outcome focused
The WSC is not designed as a prescription for how ward rounds are carried out. The checklist specifically includes a prompt to clinicians to ‘continue your round’ in order to accommodate those teams who already have an established and effective structure to their rounds, providing they adequately cover the safety checks listed. For those that have no explicit structure, we offer the chronology represented on the checklist as a sensible template, but there is no attempt to impose a particular style or structure on rounding teams. How teams choose to use the checklist is seen as their decision.
Training
We designed a training and information programme that acknowledged these principles and which placed a particular emphasis on the ‘human factors’ that influence safety, quality and consistency in healthcare. UCLH is a complex Trust with a working population of some 6600 staff operating across several geographical sites, and we initially used workforce data to map out a target training population. Some 1700 staff were identified as least potential participants in ward rounds on the basis of their department or position, and further manual segmentation reduced this to approximately 1300 staff who were potentially involved in adult inpatient round and should be familiar with the WSC. Beyond this, there was no further segmentation – all grades of staff from medicine, nursing, pharmacy and therapy were given access to the training programmes. Participants were asked to attend, as far as possible, as functioning clinical teams so that they could discuss their own particular practice and decide on their adoption of the checklist. The four-hour training session covered issues of rounding practice and behaviour, culture and human factors in medical error, teamwork and communication; where possible it involved one or two simulated patient encounters using role-played patients and a mock ward environment. To date, some 660 of the target population have been trained. Figure 2 represents the breakdown of the training population according to readily acknowledged profession-grade categories (‘junior doctor’, ‘registrar’, ‘nurse’, etc.).
Figure 2.
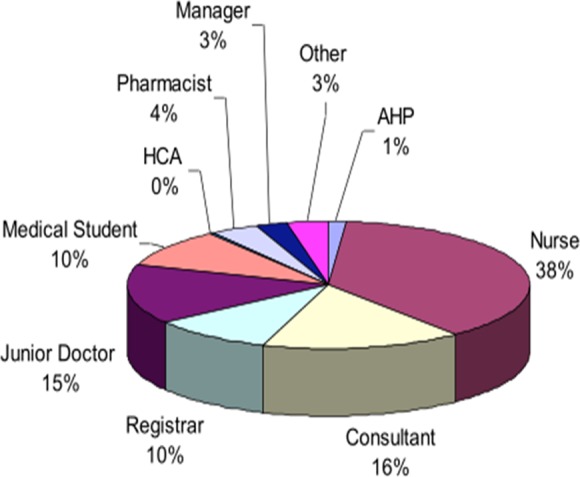
Ward safety checklist training programme attendance broken down by professional group
An estimated further 300 staff have been briefed during departmental audit and safety days, preparatory to their participation in individual training.
Issues in training
The preference for training as functional teams was based on our experience of team-based training of theatre staff in the context of the WHO safe surgery checklist training. For many individuals SSC training was valued as the first or only multidisciplinary training session they had attended, despite several years of service; many scrub nurses, for instance, had had no previous opportunity for training alongside their surgeon colleagues. In the context of the WSC, gaining similar access to functional teams was more problematic, there being no obvious equivalent of re-rostering operating lists to ‘free up’ operational teams. As a result, although there was a generally proportionate representation of professions across the programme, individual training groups could become skewed by an over representation of, for instance, junior doctors, pharmacists or nurses. In these cases the training session and simulation exercises were less an opportunity to discuss how a particular team might adopt the checklist in their practice – which was the original intention – and more an opportunity to experience the checklist and discuss the issues arising. Training groups responded well to the message that the checklist was positioned principally as an aid to good practice rather than a new process or record keeping exercise. During simulations, almost all groups remained admirably focused on the quality of their interaction with the simulated patient and not on the content or chronology of the checklist. The checklist was used principally to retrospectively ‘trap’ any issues that had been missed or under explored during the ‘usual practice’ of the clinician ‘leading’ the round. In some cases, teams adopted distributed responsibility for ensuring this retrospective use of the checklist, but the majority of teams chose to nominate a ‘monitor’ role who would prompt the round leader if issues on the checklist had not been addressed.
Further follow-up is required to map how the checklist has been adopted in the live environment, but the anecdotal evidence suggests a variety of modes of use. In some cases, nurses have adopted it as a handover tool so that patient-specific issues are identified in advance of consultant rounds. The checklist concept was also generally well received among medical students and the more junior doctors, since it evidently gave them guidance about structure and expectations of a round, a template for self-briefing and an opportunity to ask ‘naive’ questions of more experienced counterparts. The more senior medical adopters were split between those who personally used the checklist and those who designated a member of their team into an informal ‘monitor’ role. At the time of writing, our experience is that most rounding teams who use the checklist do so in a ‘background, backup’ mode to retrospectively quality assure their round.
Reaction
The single most common issue to emerge from training sessions was the depth of the disconnect between medical and nursing staff. Many doctors, of all ranks, reported that they had no routine nursing support on their round. Some had lost the expectation of such support, and others accepted that nursing input to their round had become largely a matter of chance. Conversely, nursing staff would describe senior medical rounds as being irregular and unpredictable, making it impossible to guarantee that an experienced and well briefed nurse was available to participate. A busy postsurgical ward hosting a number of outliers might, it was reported, see seven or eight consultant-led teams during the day, with many more subsidiary junior doctor rounds engaged in follow-up. Some ward sisters had identified predefined slots to medical staff during which properly briefed and experienced nursing could be fully available, but medical uptake of these slots was inconsistent and rounding arrangements remained a common source of tension on the wards. Consistent multidisciplinary team rounds are not a working reality on UK hospital wards, and if simple devices such as a ward checklist succeed only in helping to highlight and resolve the disconnect between professions, they will have made a significant contribution to ward safety.
Widespread adoption of the WSC is dependent to some extent on gaining endorsement from senior medical staff. Medical directors were persuaded of the principle of the checklist early on in the implementation, not least because they are well positioned to see the consequences of persistent ‘low level’ failures in healthcare provision. Senior interest in the WSC was also prompted by a wider programme of methicillin-resistant staphylococcus aureus land infection control measures and may have had a role in raising awareness of issues such as good preparation and hand washing prior to patient encounters. The core of the consultant body has, expectedly, proved harder to convince. For some, the logic of collectively ensuring that routine basic checks have been carried out is self-evident and the checklist has been relatively easily incorporated into their practice. Among those that are more resistant, the common responses are that the checks named on the list are already consistently done. This is an assertion that is often not supported by first-hand observation of ward rounds or the histories of some reported incidents: anecdotally, in the two months prior to checklist implementation, one ward reported three serious incidents that could have been avoided had basic checks been made at the appropriate time. It had reported none in the first three months following checklist implementation.
Other medical staff reject the checklist as a challenge to their competence and autonomy, or a misunderstanding of the medical role. There is often an almost reflexive assumption that medical staff have a minor role in assuring ‘basic care’ (seen often as a nursing task) and good ‘medical input’ is predominantly about decision-making and exercising good clinical judgement. In some respects this is understandable for historical reasons, but it is an attitude that fails to fully acknowledge the role of the medical profession in building and endorsing clinical systems that reduce unwarranted and unproductive variation in the delivery of healthcare.15
Evaluation
The programme of evaluation is ongoing. Our approach to checklists has deliberately focused on the ‘human factors’ issues of teamwork, leadership, communication and consistency. We have developed an observational framework that allows us to feedback to teams about their rounding styles. The early indications from these data are that teams using the checklist have more ‘stable’ rounds with a more clearly repeating structure, higher levels of attention and less team ‘turnover’ in the course of a round, but these findings need further validation and possible corroboration against surveys of staff experience of rounds.
Conclusion
In many safety critical industries, failure to consistently adhere to basic safety checklists is now regarded as ‘unprofessional’ and an obvious dereliction of duty; still too often in the medical profession such measures are seen as a challenge to long held professional values and individual autonomy. To that extent, the antipathy of some towards ‘a checklist approach’ to patient safety on the ward is indicative of the cultural progress that still needs to be made in many areas of clinical practice. Achieving that progress must represent a priority for current and future generations of clinical leaders: it is a task that gives shape to the longstanding but often ill-defined calls for ‘better leadership’ in the NHS. Those leaders must of course preserve the high technical standards of care that have been achieved, and ensure that such care is delivered sensitively and compassionately. But as public expectations rise and medical care becomes ever more complex, clinical leaders must recognize themselves not just as elements of effective healthcare systems, but as prime movers in the development and maintenance of processes that assure safety and quality, however unglamorous and mundane a task that might appear.
DECLARATIONS
Competing interests
None declared
Funding
Development and initial roll out of the ward safety checklist was jointly funded by the four Trust Medical Boards. NHS London and the London Deanery, through the Simulation and Technology-enhanced Learning Initiative (STeLI) has supported the development of an in-situ training package for use in London Trusts wishing to implement the checklist
Ethical approval
Written informed consent to publish the article was obtained by the patient or next of kin
Guarantor
YA
Contributorship
All named authors are joint contributors
Acknowledgements
The UCH Education Centre would like to acknowledge the support of Sir Robert Naylor, Richard Murley, Tony Mundy, Paul Glynne, Gill Gaskin, Geoff Bellingan and all the clinical teams who have supported checklist implementation
References
- 1.House of Commons Health Committee. 2012. Public Expenditure. Thirteenth Report of Session 2010–2012. London: The Stationery Office, 24 January. See http://www.publications.parliament.uk/pa/cm201012/cmselect/cmhealth/1499/149902.htm .
- 2.Wind-Cowie M, Gregory T A Place for Pride. London: Demos, 2011. See http://www.demos.co.uk/publications/aplaceforpride [Google Scholar]
- 3.Department of Health Statistical Bulletin: Overall Patient Experience Scores: Updated with results from the 2010 Adult Inpatient Survey. London: Department of Health, 2011. See http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/documents/digitalasset/dh_127188.pdf [Google Scholar]
- 4.Ipsos MORI Public Perceptions of the NHS and Social Care. London: Ipsos MORI – Social Research Institute, 2011. See http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_126705.pdf [Google Scholar]
- 5.Colin-Thome D Mid-Staffordshire NHS Foundation Trust: A Review of Lessons Learnt for Commissioners and Performance Managers following the Healthcare Commission Investigation. London: Mid Staffordshire Public Inquiry, 2009. See http://www.midstaffspublicinquiry.com/sites/default/files/David_Colin-Thome_report_on_Mid_Staffs.pdf [Google Scholar]
- 6.Patients Association We've been Listening, Have you been Learning? Harrow: The Patients Association, 2011. See http://www.patients-association.com/Default.aspx?tabid=210 [Google Scholar]
- 7.Commission on Dignity in Care for Older People Delivering Dignity: Securing Dignity in Care for Older People in Hospitals and Care Homes. A Report for Consultation. London: The Commission on Improving Dignity in Care (Local Government Association, NHS Confederation, Age UK), 2012. See http://www.nhsconfed.org/Documents/dignity.pdf [Google Scholar]
- 8.Gawande A The Checklist Manifesto: How to Get Things Right. London: Profile Books, 2011 [Google Scholar]
- 9.Ko HC, Turner TJ, Finnigan MA Systematic review of safety checklists for use by medical care teams in acute hospital settings-limited evidence of effectiveness. BMC Health Serv Res 2011;11:211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lipitz-Snyderman A, Steinwachs D, Needham DM, Colantuoni E, Morlock LL, Pronovost PJ Impact of a statewide intensive care unit quality improvement initiative on hospital mortality and length of stay: retrospective comparative analysis. BMJ 2011;342:d219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Herring R, Caldwell G, Jackson S Implementation of a considerative checklist to improve productivity and team working on medical ward rounds. Clin Govern Int J 2011;16:129–36 [Google Scholar]
- 12.Thomassen Ø Implementation of safety checklists in medicine. Not as simple as it sounds. PhD thesis. Bergen: University of Bergen, 2012. See abstract: http://hdl.handle.net/1956/5532
- 13.Semel ME, Resch S, Haynes AB, et al. Adopting a surgical safety checklist could save money and improve the quality of care in U.S. hospitals. Health Aff 2010;29:1593–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Waters HR, Korn R Jr, Colantuoni E, et al. The business case for quality economic analysis of the Michigan Keystone Patient Safety Program in ICUs. Am J Med Qual 2011;26:333–9 [DOI] [PubMed] [Google Scholar]
- 15.James BC, Savitz LA How Intermountain trimmed health care costs through robust quality improvement efforts. Health Aff (Millwood) 2011;30:1185–91 [DOI] [PubMed] [Google Scholar]