Abstract
Objective:
Identify the types and prevalence of intestinal parasites among food handlers, and test the effectiveness of the current pre-employment screening policy.
Methods:
A cross sectional survey was carried out in the catchment areas of seven primary health care centres (PHCCs) to represent various sections of Riyadh city. A total of 700 food handlers working in restaurants were randomly selected from the study area. All study subjects were asked to complete a data collection form and to bring a fresh stool specimen on the specified day to the designated PHCC.
Results:
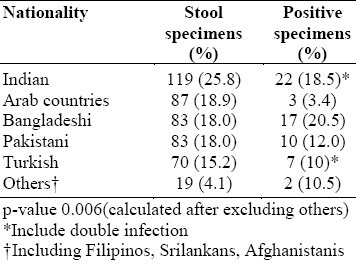
About 66% of the selected subjects complied in bringing fresh stool specimens. Fifty nine (12.8%) of the specimens were positive for parasites. There was a significant association between the food handler's nationality and the likelihood of a positive specimen result, being highest among the Bangladeshis (20.2%) and Indians (18.5%) and the lowest among the Arabs (3.4%) and the Turks (10%). The commonest intestinal parasites isolated were Giardia lamblia (33.8%), followed by Enterobius vermicularis (27.4%). The current screening policy does not seem effective, as there was an absence of significant association between holding a valid PEHC and the test result, with 81% of the positive results from persons holding valid pre-employment health certificates (PEHCs).
Conclusions:
Though it is obligatory for food handlers to hold a PEHC in Saudi Arabia, the prevalence of intestinal parasites remains high. Possible solutions include health education on hygiene, more frequent stool tests, and assessment of the current annual screening procedure.
Keywords: Intestinal parasites, health education, foodhandlers, Saudi Arabia
INTRODUCTION
Intestinal parasitic infection is considered as one of the most common tropical diseases in developing countries, where the prevalence rate ranges between 30 and 60%.1–3 The prevalence of almost all parasites depends on climatic and socio-environmental conditions.4 In a Bangladesh slum, over 80% of the population have one or more parasites.5 In some parts of India (Madras), Trichuris Trichiura was found among 62.3% of the children.6 In Pakistan, the prevalence of parasites in diarrhoeal patients was found to be 71%, with a high rate of Giardia Lamblia.7 Asymptomatic carriers of intestinal parasities are a particular public health hazard, especially if they work in catering facilities, where they may become a source of infection for others.8
Expatriates account for more than one fourth of the total population in Saudi Arabia. Most catering staff come from South-East Asia and the Indian subcontinent. Pre-employment stool examinations are mandatory for food handlers in Saudi Arabia before they can get their pre-employment health certificates (PEHCs). One stool specimen annually is needed.
Several studies have been conducted on the prevalence of intestinal parasites in patients,4,9,10 food handlers in a military hospital,11 and food handlers in communities other than Riyadh city.8,12 To the best of our knowledge no community-based study was carried out on the prevalence of food handlers in Riyadh, the Capital of Saudi Arabia.
The objective of the current study is to identify the type and prevalence of intestinal parasites among food handlers in Riyadh city, and to test the effectiveness of the current pre-employment screening policy.
MATERIALS AND METHOD
Seven primary health care centres (PHCCs) were randomly selected to represent the geographical parts of Riyadh city. Their catchment areas were taken as the study area, which included 669 different kitchens and public restaurants employing 2245 food handlers. A total of 700 food handlers were randomly selected as the study sample. The study was conducted during the period between April 1st and June 28th, 1995.
Specimen Collection
All study subjects were given a tight-lid plastic container and instructed to bring a stool specimen fresh within half an hour on the specified day, to allow an even workload for the laboratory of the designated PHCC. They were also asked to complete a data collection form with the help of trained health inspectors; it included the demographic characteristics of the worker, any related symptoms, e.g. diarrhoea, date of last PEHC (if present). Those who failed to bring the bottle were reminded with phone calls from the designated research assistant.
Stool Analysis Technique
All specimens were examined grossly by qualified laboratory technicians for consistency and presence of blood or mucus. Direct faecal smears were prepared for microscopic assessment for the presence of trophozoites and cysts within 15 minutes of receipt under magnifications of 10 and 40x.
Data Analysis
The data were entered into a PC microcomputer and were analysed using Stat Pac Gold statistical analysis package. The association between two categories was tested for significance using chi-square test, and p value less than 0.05 was considered significant.
RESULTS
Of the 700 food handlers selected for the study, 461 (65.8%) responded. All food handlers working in kitchens and public restaurants in the study area were non-Saudi men, ranging in age from 21 to 48 years. They represented 11 different countries, the majority of them (65.9%) from South East Asian countries and the Indian subcontinent (Table 1). There was a significant association between the nationality of the food handler and the likelihood of his having a positive stool specimen for parasites (P = 0.006). The highest prevalence was among the Bangladeshis (20.5%), followed by the Indians (18.5%); the least was among the Arabs (3.4%) and the Turks (10%) (Table 1).
Table 1.
Prevalence of intestinal parasitic infections in various nationalities in Riyadh, Saudi Arabia(N=461)
Of the 461 stool specimens examined, 59 (12.8%) were found to be positive for parasites. Giardia lamblia constituted 33.8% of total positive specimens; 42.9% of which were found among Indians, followed by Bangladeshis (33.3%), Pakistanis (14.3%), and Turks (9.5%). No parasites were found among Arabs and the other nationalities (Table 2). Enterobius vermicularis was the second most common parasite (27.4%) of the total positive specimens; 43.8% of which were found among Indians, followed by Bangladeshis, Turks and Pakistanis (18.8, 18.8, and 12.3% respectively) Table 2. Entamblia histolytica constituted 19.4% and was equally prevalent among Arabs, Pakistanis, Turks and others 16.8% (Table 2). Only 8.4% of the Arab food handlers had positive results, compared to 14.97% of the non-Arab ones (Table 3).
Table 2.
Distribution of the most common intestinal parasites according to nationality in Riyadh

Table 3.
Prevalence of the most common intestinal parasites in food handlers according to nationality

Of 59 positive subjects, 81.4% had a valid PEHC. Furthermore, there was no significant difference between the subjects who had or did not have a valid PEHC, and the likelihood of having a positive test for parasites (p=0.13). Two specimens (3.4%). (3.4%) were found to have double infection. The majority of infected persons were asymptomatic 45 (76.3%); whereas (23.7%) complained of diarrhoea at the time of the study (Figure 1). Sixty-six percent of the infected persons with Giardiases were found to be asymptomatic. The prevalence of each type of intestinal parasite is shown in Figure 2.
Figure 1.
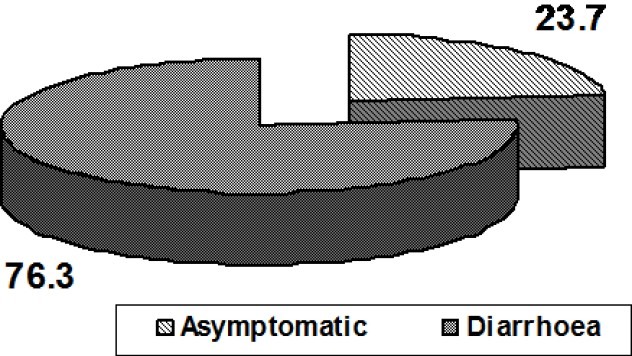
Symptoms of intestinal parasitic infection among food handlers in Riyadh, Saudi Arabia
Figure 2.
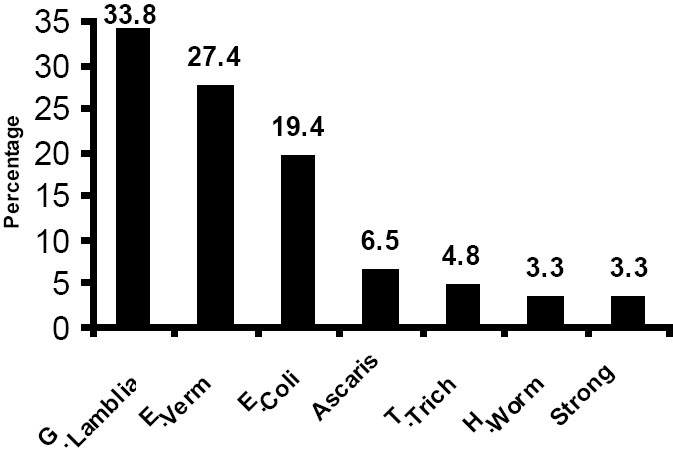
Prevalence of each type of intestinal parasites among food handlers in Riyadh, Saudi Arabia
DISCUSSION
Although the study subjects were reassured that the test would not influence their ability to continue their jobs and defaulters were reminded and rescheduled, only 65.8% of the subjects complied. Two fresh stool samples two days apart per patient were reported to increase the yield of isolation.13–15
The technique used in this study, microscopy of a single fresh faecal smear, is recognised as having low sensitivity in detecting most intestinal parasites and will only have detected those that were abundant in the particular faecal sample supplied. However, our one-sample-per-subject policy was employed due to scheduling difficulties and concern over col-lection of additional samples being unacceptable by the study subjects. This policy may lead to under-estimation of the problem size. Use of a magnification of 10x and 40x means that cryptosporldium SPP will have missed. Moreover, Microsporldia SPP, in particular, need special stain which is not available in the labs. We also realise that for adequate sensitivity strongloides SPP require concentration or culture which is not available in the basic laboratory of PHCCs. The prevalence of intestinal parasites in this study (13%), is similar to the figure (14.2%) of a similar study in Al-Madina (in the West of Saudi Arabia).12 A lower prevalence rate (7.6%)8 was reported among food handlers in the Eastern Province, although food handlers attending a pre-employment examination were studied.
Giardiasis is endemic in many parts of the world, including Europe and the USA.9,16) Consumption of faecally contaminated water is the main mode of transmission, followed by direct person-to-person contact. On a few occasions food has been implicated as a source of infection.13,17 Giardia lamblia was the most common parasite (33.8%) isolated in this study. The prevalence rate of Giardia lamblia has had a wide range in different Saudi studies, namely 3.1-30%.4,8,12 The finding that three quarters of the positive-testing workers were asymptomatic could not be explained totally by the high proportion of Giardiasis (only 66% were asymptomatic), as it was suggested by a few studies.18
This study was consistent with the findings of previous studies7–12,20–25 which recognized that intestinal parasitic infection among food handlers is still an important public health problem in the Kingdom of Saudi Arabia.
CONCLUSIONS AND RECOMMENDATIONS
The finding of a higher prevalence among the Bangladeshis and Indians who have a high prevalence rate in their own countries5–7,19 indicates that more rigorous strategies should be directed to these high risk groups. The Indians represent a high proportion of the total sample size (26%) and 18.5% of positive specimens. They need health education regarding certain hygienic measures to avoid spreading of the infection and more frequent stool tests, especially upon arrival from travel to their countries.
The finding of 81% positive results among the subjects who had a valid PEHC and the absence of significant association between a valid PEHC and test result call into question the effectiveness of the annual screening procedure. Reinfection is another possible cause of these results because some of the subjects might have had a holiday in an endemic area and come back carrying the infection or been in contact with some one who had the infection.
Re-evaluation of the process of pre-employment examinations, especially those in the catering trade is highly recommended. Biannual screening of two stool samples two days apart per food handler is also recommended, as is a re-examination checkup upon arrival after holiday, particularly for those coming from high prevalence countries.
ACKNOWLEDGMENT
The authors are grateful to Drs. Jamal Jarallah, Sulaiman Al-Shammari, and Fayek S. El Khwsky from the Department of Family and Community Medicine, College of Medicine, King Saud University for their constructive comments, and Mr. Mohamed Eijaz for secretarial assistance.
REFERENCES
- 1.Musaiger AO, Gregory WB. Change in parasitic infections among school children in Bahrain, 1980-1986: A preliminary study 1990. Saudi Med J. 1990;11(2):113–5. [Google Scholar]
- 2.World Health Organization. Prevention and control of intestinal parasitic infections. 1987;749:7–18. [PubMed] [Google Scholar]
- 3.Al-Shammari S, Khoja T, Al-Khwasky F, Gad A. Intestinal Parasitic diseases in Riyadh, Saudi Arabia: Prevalence, Sociodemographic and environmental associates. Tropical Medicine and International Health. 2001;6(3):184–9. doi: 10.1046/j.1365-3156.2001.00698.x. [DOI] [PubMed] [Google Scholar]
- 4.Khan MU, Amir SE, Eid OM, Aggrewal S. Parasitic infestation in expatriates in Riyadh, Saudi Arabia. Ann Saudi Med. 1989;9(5):471–4. [Google Scholar]
- 5.Khan MU, Shahidullah M, Barua DK, Begum T. Efficacy of periodic deworming in an urban Slum population for parasite control. Ind J Med Res. 1984;83:82–8. [PubMed] [Google Scholar]
- 6.ElKins DB. A survey of intestinal helminthes among children of different social communities in Madras, India. Transa Roya Soci Trop Med Hyg. 1984;78:132–3. doi: 10.1016/0035-9203(84)90195-0. [DOI] [PubMed] [Google Scholar]
- 7.Baqai R, Zuberi SJ. Prevalence of intestinal parasites in Diarrhoeal patients. J Pak Med Assoc. 1986;36:7–11. [PubMed] [Google Scholar]
- 8.Khan ZA, Al-Jama AA, Madan I. Parasitic infections among food handlers in Dammam and Al-Khobar, Saudi Arabia. Ann Saudi Med. 1987;7(1):47–50. [Google Scholar]
- 9.Hussain Qadri SM, Khalil SH. Intestinal parasites: Incidence and etiology in over 1,000 patients at King Faisal specialist hospital in Riyadh. Ann Saudi Med. 1987;7(3):207–11. [Google Scholar]
- 10.Al-Fayez SF, Khogheer YA. A follow up study on prevalence of parasitic infections among patients attending King Abdulaziz University Hospital, Jeddah. Saudi Med J. 1989;10(3):193–7. [Google Scholar]
- 11.Abu Al-Saud AS. Faecal parasites in non-Saudi catering and domestic staff at the Riyadh Military hospital. Saudi Med J. 1983;4(3):259–62. [Google Scholar]
- 12.Ali SI, Jamal K, Hussain Qadri SM. Prevalence of intestinal parasites among food handlers in Al-Madinah. Ann Saudi Med. 1992;12(1):63–6. doi: 10.5144/0256-4947.1992.63. [DOI] [PubMed] [Google Scholar]
- 13.Al-Ballaa SR, Al-Sekeit M, Al-Ballaa SR, et al. Prevalence of pathogenic intestinal parasites among preschool children in Al-Madina District, Saudi Arabia. Ann Saudi Med. 1993;13(3):259–63. doi: 10.5144/0256-4947.1993.259. [DOI] [PubMed] [Google Scholar]
- 14.Healy GR. Diagnostic techniques for stool samples. In: Ravin JI, editor; Ravin JI, editor. Amebiasis: Human Infection by Entameba histolytica. New York: Churchill Livingstone; 1988. pp. 495–510. [Google Scholar]
- 15.Mathur TN, Kaur J. The frequency of excretion of cysts of E. histolytica in known cases of non-diagnostic amebic colitis based on 21 stool examinations. Ind J Med Res. 1993;61:330–4. [PubMed] [Google Scholar]
- 16.Knight R. Epidemiology and transmission of giardiasis. Transa Roya Soci Trop Med Hyg. 1980;74(4):433–5. doi: 10.1016/0035-9203(80)90044-9. [DOI] [PubMed] [Google Scholar]
- 17.Petersen LR, Cartter ML, Hadler J. A food-Borue outbreak of Giardia Lamblia. J Infect Dis. 1988;157(4):846–8. doi: 10.1093/infdis/157.4.846. [DOI] [PubMed] [Google Scholar]
- 18.Meyer EA, Jarroll EL. Reviews and Commentary – Giardiasis. Am J Epidemiol. 1980;111(1):1–12. doi: 10.1093/oxfordjournals.aje.a112860. [DOI] [PubMed] [Google Scholar]
- 19.Ibrahim OMG, Bener A, Shalabi A. Prevalence of Intestinal Parasites among expatriate Woncers in Al-Ain, United Arab Emirates. Ann Saudi Med. 1993;13(2):126–9. doi: 10.5144/0256-4947.1993.126. [DOI] [PubMed] [Google Scholar]
- 20.Abdel-Hafez MA, El-Kady N, Noah MS, Bolbol AS, Baknina MH. Parasitic infestation in expatriates in Riyadh Saudi Arabia. Ann Saudi Med. 1987;7(3):202–6. [Google Scholar]
- 21.Bolbol AS, Mohmoud AA. Laboratory and clinical study of intesdtinal pathogenic parasites among the Riyadh population. Saudi Med J. 1984;5:159–66. [Google Scholar]
- 22.Abu Al-Saud AS. A survey of the pattern of parasitic infestation in Saudi Arabia. Saudi Med J. 1983;4(2):117–22. [Google Scholar]
- 23.Al-Madani AA, Omar MS, Abu-Zeid HA, Abdulla SA. Intestinal parasites in urban and rural communities of Abha, Saudi Arabia. Ann Saudi Med. 1989;9(2):182–5. [Google Scholar]
- 24.Abu-Zeid HA, Khan MU, Omar MS, Al-Madani AA. Relationship of intestinal parasites in urban communities in Abha to socio-economic mental factors. Saudi Med J. 1989;10(6):477–80. [Google Scholar]
- 25.Siddiqui MA. The prevalence of human intestinal parasites in Al-Baha, Saudi Arabia: a preliminary survey. Annals of Tropical Medicine and Parasitology. 1981;75(5):565–6. doi: 10.1080/00034983.1981.11687483. [DOI] [PubMed] [Google Scholar]


