Abstract
Objective:
To evaluate the rate of seropositivity to hepatitis B and C and Human Immunodeficiency Virus (HIV) infections among children with β-thalassemia major receiving multiple transfusions in Ahmedabad, India, compared with healthy controls.
Materials and Methods:
The study was performed during January 2007 to January 2009 on multi-transfused children suffering with β-thalassemia major registered in the Prathama Blood Centre, Ahmedabad; Jeevandeep hospital, Ahmedabad; and Red Cross Blood Centre, Ahmedabad, and investigated for the prevalence and development of transfusion-transmitted infections. Hepatitis B surface Antigen (HBsAg), anti-Hepatitis C Virus (HCV) Antibodies (Ab), and HIV Ab were checked using a fourth-generation Enzyme-Linked Immunosorbent Assay (ELISA). Positive tests were confirmed by western blots. Healthy blood donors were used for the control group.
Results:
Hepatitis B surface antigen, anti-HCV Ab, and HIV Ab were positive in one of 96 (1.04%; 95% Confidence Interval (CI) = 0.17–1.3), 24 of 96 (25%; 95% CI = 11.4–14.2), and one of 96 (1.04%; 95% CI = 0.12–1.3), respectively. The rate of anti-HCV Ab was significantly higher in multi-transfused children suffering with β-thalassemia major. In thalassemia patients, the rate of positive anti-HCV Ab was significantly higher than that for positive HBsAg (P<0.001) and HIV Ab (P<0.001).
Conclusion:
It is concluded that HCV is the current major problem in multi-transfused children with thalassemia major and more careful pretransfusion screening of blood for anti-HCV must be introduced in blood centers.
Keywords: Hepatitis B, hepatitis C, Human immunodeficiency virus, β-thalassemia major, seroprevalence
Introduction
Thalassemia also known as “Cooley's anemia” is an inherited disease of the red blood cells classified as a hemoglobinopathy. The genetic defect results in synthesis of an abnormal hemoglobin molecule. The thalassemias are a group of congenital anemia that is characterized by deficient synthesis of one or more globin subunits of the hemoglobin. According to the chain whose synthesis is impaired, the thalassemia are designated as α, β, γ, δ, δβ, or εγδβ thalassemia. The β thalassemia is probably the most common inherited hemoglobin disorder in the Indian subcontinent, with an uneven distribution among the different endogenous populations. The basic defect in β thalassemia is a reduced or absent production of β globin chains with relative excess of α chains. The designations commonly used to describe the β thalassemia syndrome are based on clinical severity. Beta (β)-thalassemia major is the most severe form. This is also called “Cooley's anemia” or Mediterranean anemia. It manifests within the first year of life in 95% of the patients.
Conventional treatment of patients suffering from β thalassemia is regular blood transfusion support from early childhood. The current management of thalassemia includes regular transfusion program and chelation therapy. The rationale for this treatment started in 1960s and was modified in the following years to achieve progressively higher levels of hemoglobin, which corrects the anemia and prevents the ineffective erythropoiesis, increases oxygen delivery to tissues, promotes growth, and improves the general well being.[1] Current guidelines recommend a pretransfusion threshold not exceeding 9.5% g/dl, which seems to be associated with adequate marrow inhibition and a relatively low iron burden.[2,3] Piomelli et al. have recommended a hypertransfusion regimen, with pretransfusion hemoglobin level of 10 g/dl.[4] Thus, they contribute to a group of patients called multi-transfused patients. They are subjected to various adverse effects of chronic transfusion that are uncommon in rare recipients of blood transfusions.
The natural course of the disease is dramatically altered by transfusion side effects, which need to be monitored and treated throughout life. Iron overload resulting in end-organ damage and blood-borne infectious agents still represent the principal causes of morbidity and mortality. Blood transfusion exposes the patient to a number of risks, adverse events associated with transfusion, such as nonhemolytic febrile reactions, allergic reactions, delayed transfusion reactions, transfusion-related lung injury, graft-versus-host disease, red cell alloimmunization and transfusion of infectious agents including viruses, bacteria and parasites.[5,7]
Thalassemia is one of the common genetic conditions prevalent in India. With an estimated incidence of 2 per 1,000 births and a carrier frequency of 3-4%, it constitutes a significant health burden. Blood transfusion is the mainstay of therapy in view of the constraints in bone marrow transplantation. Recent developments in the transfusion services have improved the quality of blood products, and availability of good supportive therapy has increased the survival and enhanced the quality of life in the survivors.
Appropriate and regular red cell transfusion remains the main treatment of choice for a large number of patients with thalassemia major. These patients who are maintained on hyper-transfusion regimen can develop various complications due to multiple transfusions, one of them being transfusion-associated infections. The transfusion-associated diseases are overcome by safe donor selection and, further, by application of better screening methods. This study was designed to determine the prevalence and incidence of Transfusion-Transmitted Infections (TTI) in multiply transfused thalassemia patients during the study period.
Materials and Methods
A prospective study was conducted from January 2007 to January 2009. In this study, a cohort of 115 patients was selected from regular transfusion group and the patients were followed up for one and half year. They were followed up for the effect of transfusion during the study period. There was a decline in the number of patients from 115 to 96 due to mortality and transfer of patients. A total of 96 multiply transfused thalassemia patients were prospectively included in this study; further, 3 consecutive samples were collected after every 6 month and investigated for the TTI. Five to seven milliliter of blood was collected in plain tube and serum was separated. The serum was taken in two aliquots, labeled appropriately and stored in two different boxes at -30°C in deep freezer, till the tests for TTI were performed. The tests for TTI were performed on the preserved sample to investigate prevalence and development of TTI by standardized laboratory techniques by the same individual at Prathama Blood Centre. For detection of Hepatitis C Virus (anti-HCV), Human Immunodeficiency Virus (anti-HIV) antibody, and Hepatitis B surface Antigen (HBsAg), the Enzyme Linked Immunosorbant Assays (ELISA) tests were done on the patients’ serum. The assays were done in batches at the end of the study period, with strict adherence to the kit manufacturer's instructions. The thalassemia patients were receiving regular transfusions from Prathama Blood Centre, Ahmedabad; Jeevandeep hospital, Ahmedabad; and Red Cross Blood Centre, Ahmedabad, all of which were included in this study and investigated for the prevalence and development of TTI.
Results
The prevalence of TTI was studied. There were a total of 96 patients; of them one patient (1.04%) was positive for HBsAg, 24 (25%) were positive for anti-HCV, and one (1.04%) was positive for anti-HIV [Table 1].
Table 1.
Prevalence of transfusion-transmitted infections in the first set of samples
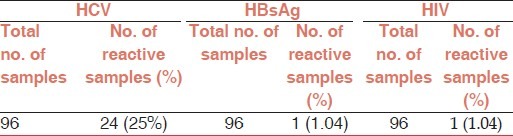
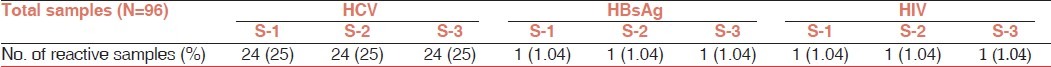
Table 2 shows the prevalence of TTI in three consecutive sets of samples, which was the same throughout the study. The prevalence of transfusion-transmitted infections with anti-HCV, HBsAg, and anti-HIV in the first set of samples (S-1) was 25%, 1.04%, and 1.04%, respectively. This prevalence of TTI in the second (S-2) and third sets of samples (S-3) were the same as in the first set of samples (S-1). Prevalence of TTI remained same during the study period. No patient was observed to have acquired transfusion-transmitted infections such as HBV, HCV, and HIV during the study period [Table 2].
Table 2.
Prevalence of transfusion-transmitted infections in three consecutive sets of samples
Discussion
Management of patients suffering with β-thalassemia is based on adequate and safe blood transfusions and receiving regular iron-chelation therapy, all of which improve the quality of life and survival of patients.[3]
This study was designed to determine the prevalence and incidence of transfusion transmitted infections in multiply transfused thalassemia patients during the study period. This study carried out at Prathama Blood Centre, Ahmedabad over a period of 2 years from Jan 2007 to Jan 2009. Cohort of 115 patients was selected from regular transfusion group and they were followed for one and half year and evaluated for the prevalence and development of transfusion transmitted infections. A total of 96 multiply transfused thalassemia patients were prospectively included in the study and investigated for the prevalence and development of transfusion transmitted infections.
Patients with thalassemia major require repeated transfusions of blood exposing them to the risk of Transfusion-Transmitted Diseases (TTDs). The probability of acquiring TTDs is related to the probability of being exposed to the infected units of blood. This probability depends on the prevalence of carriers among the blood donors in the population and the number of units transfused. Thus, the infection rate of TTDs increase with age in subsequent years. The incidence of hepatitis and HIV infections in Indian pediatric patients with thalassemia is high due to high prevalence of hepatitis and HIV in the general population.[8,9]
Transfusion-transmitted infections such as Hepatitis B Virus (HBV), Hepatitis C Virus (HCV), and HIV are dreaded consequences of transfusions, as these can result in long-term morbidity and mortality. In India, it is mandatory to screen donated blood for anti-HIV 1 and 2 (since 1991), anti-HCV (since 2000), HBsAg, syphilis, and malaria. TTI can still occur from blood donations negative for markers for these infections as reported by various Indian investigators[6,10] and international studies.[11–13] This residual risk of TTI transmission from screened blood depends on the safety of donor population, sensitivity of the screening tests used, window-period donations, and other reasons such as mutant strains.[14]
Hepatitis C virus, which was discovered in 1989, is an enveloped virus of size 30-60 nm, and it gets transmitted through the parenteral route. The clinical course seems to be more serious in hepatitis C infection. Studies available from India give prevalence of markers for TTI in donors and recipients.[6,10–15] The prevalence of anti-HCV in multiple-transfused patients is confirmed to be high.[15,16] A three-years prospective study from India by Choudhury et al,[15] observed that anti-HCV prevalence in the same number of thalassemia major patients was 23%, 30.7%, and 35.9% each year, respectively. The present study showed similar result as described by Choudhury et al.[15]
Prevalence studies have found that common infections occurring in thalassemic patients are Hepatitis C (2.2%-44%), followed by Hepatitis B (1.2%-7.4%) and HIV (0%-9%).[6,10–12,15] Karimi et al,[12] found the prevalence of HCV to be 15.7%, Prati et al[13] found it to be 14.8%, and Singh et al[10] found a high prevalence of HCV (20%) in multiply transfused thalassemia major patients. Results of these observations were in accordance to the present study in which a high prevalence of HCV (25%) was reported.
In the present study, out of 96 multiply transfused thalassemic patients, 24 (25%) were reactive for anti-HCV. An important finding in the present study, all anti-HCV–reactive patients were above the age of 8 years, which may be because of the HCV untested blood transfusion before June 2001. In the present study, a high prevalence of anti-HCV (25%) was reported probably because of HCV untested blood transfusion before 2001. Anti-HCV test has been made mandatory by the Government of India from June 2001.[15]
Transfusion-associated hepatitis is a major problem in South-East Asian countries, including India, due to endemic hepatitis infections in this region. The prevalence of HBV is low in the US and Western Europe (0.1%-0.5%), while in South-East Asia and China, which are endemic areas, this is in the range of 5%-15%. Prevalence of HBV and HCV in blood donors in India is about 1%-5% and 1%, respectively. According to the Drugs and Cosmetic Act (1992), every blood unit has to be tested for HBsAg, anti-HIV I and II, VDRL, and malaria. HBsAg testing is mandatory according to the Act, but it can either be carried out by ELISA or Reverse Passive Hemagglutination Assay (RPHA).[15]
Hepatitis B is a special problem in India since it is a medium endemic area. This problem is acutely reflected in blood transfusion services due to dependence on first-degree relative or paid blood donors and lack of non-remunerated repeat voluntary blood donors. Routine HBsAg screening in blood units does not eliminate the risk of HBV transmission. HBsAg test may be negative in the window phase of HBV infection, in the convalescence phase and also in HBV chronic infection, with very low level of viremia. Prevention of post-transfusion hepatitis starts with selection of non-remunerated voluntary blood donors. It has been observed that polyclonal antibody-based ELISA gives better sensitivity and provides better detection of mutants.[15]
Hepatitis B Virus may occasionally be transmitted through transfusion of blood units that are HBsAg-negative but HBV DNA-positive. Children with -thalassemia are particularly susceptible to HBV because they receive multiple blood transfusions. Singh et al.[10] found 5.7% prevalence of HBV in multiply transfused β-thalassemia major patients. Many prevalence studies have found that the HBV infection occurring in multiply transfused thalassemic patients range from 0.53% to 7.4%.[6,10–12] Results of these observations were in accordance of the present study, where prevalence of HBV was 1.04% reported.
The prevalence of HIV infection in thalassemia varies greatly worldwide, from less than 1% to more than 20%. With the use of standard procedures for prevention, it is possible to keep the risk of HIV transmission very low, with the use of the most sensitive screening measures. In the absence of treatment, the median time from HIV seroconversion to the onset of AIDS in transfused patients is about 7-11 years. Factors affecting progression include symptomatic primary infection, age at infection, and viral load. Patients with thalassemia identified with HIV infection should be managed in collaboration with an infectious diseases unit with expertise in HIV.[6,10,12,17,18] Results of these observers were in accordance of the present study where prevalence of HIV was reported to be 1.04%.
Cases of AIDS have been reported from India since 1986. The voluntary donors screening for HIV in donated blood was introduced in India in March 1989. The Indian study on multi-transfused thalassemia patients indicate the seropositivity for HIV varying from 0.5% to 3.8%.[8] The present study showed similar result as described by Choudhury et al.[8] The preventive measures include careful donor selection, laboratory testing, safe transfusion practice, and blood product sterilization. In India, National AIDS Control Organization (NACO) was established under the Ministry of Health and Family Welfare for the control of HIV infection in India. NACO supplied various equipment for HIV screening and component preparation to blood banks and HIV (ELISA and RAPID) kits are also supplied free of cost. HIV antibody tests are to be carried out according to the prevalence of HIV infection in a particular population.[15]
Conclusion
In the present study, of the 96 multi-transfused thalassemic patients, 24 (25%) were reactive for anti-HCV, 1 (1.04%) patient was reactive for HBV, and 1 (1.04%) patient was reactive for HIV. It was observed that no patient acquired transfusion-transmitted infection such as HBV, HCV, and HIV during the study period. Therefore, it is concluded that HCV is the current major problem in multi-transfused children with thalassemia major and more careful pretransfusion screening of blood for anti-HCV must be introduced in our blood banks.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Modell B, Berdoukas V. New York and London: Grune and Stratton; 1984. The clinical approach to thalassemia. [Google Scholar]
- 2.Olivieri NF, Nathan DG, MacMillan JH, Wayne AS, Liu PP, McGee A, et al. Survival in medically treated patients with homozygous beta thalassaemia. N Engl J Med. 1994;331:574–8. doi: 10.1056/NEJM199409013310903. [DOI] [PubMed] [Google Scholar]
- 3.Olivieri NF, Brittenham GM. Iron-chelating therapy and the treatment of thalassemia. Blood. 1997;89:739–61. [PubMed] [Google Scholar]
- 4.Piomelli S, Loew T. Management of thalassemia major (Cooley's anemia) Hematol Oncol Clin North Am. 1991;5:557–69. [PubMed] [Google Scholar]
- 5.Brecher ME, Butch SH, Calhoun AR, Fiebig EW, Goodnough LT, Hahn L, et al., editors. 15th ed. 2005. Technical manual of the American Association of Blood Banks; pp. 283–336. [Google Scholar]
- 6.Choudhury N, Naik S, Ramesh V. High frequency of transfusion transmitted viral infection markers in thalassemia major patients. Indian J Hematol Blood Transfus. 1995;13:115–8. [Google Scholar]
- 7.Fongsatitkul L, Bannawat U, Sanguansermsri T, Kulapongs P. Unexpected red cell antibodies in thalassemic children. Birth Defects Orig Artic Ser. 1988;23:291–3. [PubMed] [Google Scholar]
- 8.Choudhury N, Saraswat S, Naveed M. Serological monitoring of thalassemia major patients for transfusion associated viral infections. Indian J Med Res. 1998;107:263–8. [PubMed] [Google Scholar]
- 9.Lee WS, Chan LL. Risk of seroconversion of hepatitis B, hepatitis C and HIV in children with multitransfused thalassemia major. J Paediatr Child Health. 2005;41:265–8. doi: 10.1111/j.1440-1754.2005.00608.x. [DOI] [PubMed] [Google Scholar]
- 10.Singh H, Pradhan M, Singh RL, Phadke S, Naik SR, Aggarwal R, et al. High frequency of hepatitis B virus infection in patients with β-thalassemia receiving multiple transfusions. Vox Sang. 2003;84:292. doi: 10.1046/j.1423-0410.2003.00300.x. [DOI] [PubMed] [Google Scholar]
- 11.Al-Sheyyab M, Batieha A, El-Khateeb M. The prevalence of hepatitis B, hepatitis C and human immune deficiency virus markers in multi-transfused patients. J Trop Pediatr. 2001;47:239–42. doi: 10.1093/tropej/47.4.239. [DOI] [PubMed] [Google Scholar]
- 12.Karimi M, Ghavanini AA. Seroprevalence of hepatitis B, hepatitis C and human immunodeficiency virus antibodies among multitransfused thalassaemic children in Shiraz, Iran. J Paediatr Child Health. 2001;37:564–6. doi: 10.1046/j.1440-1754.2001.00709.x. [DOI] [PubMed] [Google Scholar]
- 13.Prati D. Benefits and Complications of Regular Blood Transfusion in Patients with Beta-Thalassemia major.Centro Trasfusionale e di Immunologia dei Trapianti, IRCCS Ospedale Maggiore di Milano, Italia. Vox Sang. 2000;79:129–37. doi: 10.1159/000031230. [DOI] [PubMed] [Google Scholar]
- 14.Mine H, Emura H, Miyamoto M. High throughtout screening of 16 million serologically negative blood donors for hepatitis B virus, hepatitis C virus and HIV type-1 by NAT with specific and sensitive multiplex reagent in Japan. J Virol Methods. 2003;112:145–51. doi: 10.1016/s0166-0934(03)00215-5. [DOI] [PubMed] [Google Scholar]
- 15.Choudhury N, Phadke S. Transfusion transmitted diseases. Indian J Pediatr. 2001;68:951–8. doi: 10.1007/BF02722595. [DOI] [PubMed] [Google Scholar]
- 16.Saberi-Firoozi M, Khan Y, Karbasi HT. Anti-HCV seropositivity among multiply transfused patients with thalassemia major in southern Iran. Iran J Med Sci. 1996;21:59–61. [Google Scholar]
- 17.Kumar RM, Uduman S, Hamo IM, Morrison J, Khaurana AK. Incidence and clinical manifestations of HIV-1 infection in multitransfused thalassaemic Indian children. Trop Geogr Med. 1994;46(Suppl 3):S163–6. [PubMed] [Google Scholar]
- 18.Guidelines for the clinical management of thalassemia. Cyprus: Nicosia; 2005. Thalassemia international Federation; pp. 25–37. and 62-75. [Google Scholar]


