Abstract
Background:
Lack of awareness and community motivation, compounded with fragmented blood transfusion services in our country, Often leads to shortage of blood. Donor recruitment and retention are essential for ensuring adequate blood supply. However, adverse events (AEs) in donors have a negative impact on donor return.
Aims and Objectives:
The present study was aimed to assess the frequency of AEs in whole blood donors and analyze the predisposing factors for AEs.
Material and Methods:
The study was conducted on allogeneic whole blood donors over a period of 14 months, i.e., from January 2002 to February 2003. A total of 37,896 donors were monitored for any AEs: 22587 (59.6%) were voluntary donors (VD) and 15,309 (40.4%) were replacement donors (RD).
Results:
Overall reaction rate was 2.5% with vasovagal reactions constituting 63.5% and hematomas 35.0% of all reactions. Vasovagal reactions showed a significant association with young age, lower weight, first time donation status, female gender, and nature of blood donation camps. Amongst male donors, RDs had more reactions (P=0.03) than VDs. Majority of donors (85%) with vasovagal reactions admitted to some fear or anxiety prior to donation. Hematoma formation occurred significantly more when less trained staff performed phlebotomy.
Conclusion:
Donor safety is an essential prerequisite to increase voluntary blood donation. AE analysis helps in identifying the blood donors at risk of donor reactions and adopting appropriate donor motivational strategies, pre-donation counseling, and care during and after donation.
Keywords: Adverse events, donors, vasovagal reactions
Introduction
Lack of awareness and motivation in the community, compounded with a fragmented blood transfusion service in our country, often leads to shortage of blood and blood components. Generally, two strategies are adopted to meet the public demand of blood and its components – recruitment of new donors and retention of already recruited donors. Replacement donors, who still form a high proportion of all whole blood donors in developing countries,[1] can be retained as future voluntary donors if found non-reactive for transfusion transmissible infection. Adverse events (AEs) in blood donors can adversely affect donor recruitment and retention.
While blood donation is a safe procedure, a small percentage of donors may experience an AE. The most frequent AE is usually a mild vasovagal reaction, but for the donor it is an unpleasant experience, and acts as a deterrent for repeat donation. It has been documented in various studies that 2–6% of donors experience an AE, but only 0.08–0.3% have a syncopal reaction where there is loss of consciousness.[2–4] Donor characteristics that have been observed to predispose to AEs include young age, low weight, first-time donation status, female gender, and Caucasian race.[4–8] These studies are primarily on voluntary donors from developed countries and may be applied to predict the reaction pattern in voluntary donors in India, but may not be applicable to replacement donors who donate blood for a variety of reasons. The only other study from India on donor reactions describes only vasovagal reactions and is a retrospective analysis of risk factors in replacement donors.[9] The present study is prospective and analyzes the entire spectrum of AEs in both voluntary and replacement donors and factors predisposing to these events.
Materials and Methods
The study was conducted on allogeneic whole blood donors over a period of 14 months, i.e., from January 2002 to February 2003. Criteria for the selection of whole blood donors were in accordance with the rules laid down in Drugs and Cosmetics Act, Ministry of Health and Family Welfare, Government of India.[10] Blood collection was performed in the blood donation area of the department within the hospital premises and in blood donation camps organized at various locations in and around the city of Chandigarh, North India. Donors were observed before, during, and after blood donation for any AEs. Post-phlebotomy observation was defined as the time until the donor left the donor site, which was usually 30 min after donation. A total of 37,896 donors were monitored for any AEs: 22587 (59.6%) were voluntary donors (VD) and 15,309 (40.4%) were replacement donors (RD).
An AE was defined as the symptoms or signs of donor discomfort of sufficient severity such that either the donor called for attention of the staff or they were noticed by the staff. Pain at the time of venepuncture was excluded.[11]
Adverse events
Donor reactions were categorized as immediate and delayed depending upon whether a reaction was noted at the site of donation or was reported by the donor after leaving the site of donation. They were further classified according to nature and severity of the reaction. The donors were observed for any evidence of vasovagal reaction, and if it occurred, it was graded as mild, moderate, or severe as per standard criteria.[11] Other adverse events observed were hematoma/bruise at the phlebotomy site, accidental arterial puncture, neurological injury, local allergy, and thrombophlebitis. In case of any reaction at the donation site, immediate management was initiated, and if necessary, the donor was shifted to hospital emergency service. Once the donor recovered from the AE, a detailed report form was filled by the phlebotomist, which included all demographic details, reaction details, and questionnaire to assess pre-donation apprehensions. For delayed reactions, the donor was advised to get in touch with the designated department staff. Telephone numbers were provided to the donors along with a delayed reaction form with a stamped addressed envelope. Trained doctors and postgraduate students of the department perform donor phlebotomy at our institute; hence, doctor donor rapport could be established satisfactorily.
This study was cleared by the institutional review board.
Statistical analysis
Mean±SD/range was determined wherever required. Different variables and reaction rates were compared using Chi-square test and binominal multiple logistic regression test, determining significance at P<0.05.
Results
Donor demographics
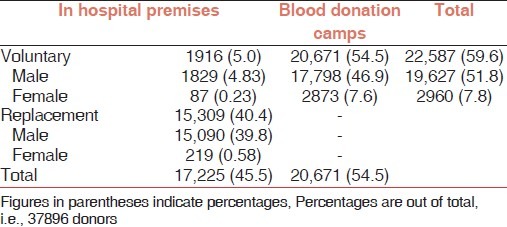
A total of 37,896 units of whole blood were collected from 22,587 (59.6%) voluntary and 15,309 (40.4%) replacement donors. As compared to RDs, all of whom donated in the department, majority of VDs, 20,671 out of 22,587 (92%), donated in the blood donation camps (BDC) outside hospital premises, as per convenience of donors. Proportion of female donors was significantly higher in VDs (13.1%) as compared to RDs; 219 out of 15,309 (1.4%) (P<0.001) [Table 1].
Table 1.
Blood donation in and outside hospital premises
Mean age of the donors was 31±9 years, with a range of 18–60 years. Mean age of male VDs was 31.4±10.2 (range 18–60) years and female VDs 30.7±10.3 (range 18–59) years. Mean age of male RDs was 30.6±8.2 (range 18–60) and female RDs 33.2±9.1 (range 18–55) years [Figure 1]. However, 54.7% donors (20,744) were in the 18–30 years group, 36.5% (13,841) in the 31–45 years group, and only 8.7% (3311) were in the 46–60 years of age group. Mean weight of the donors was 69.5±11.6 kg, with donors weighing in the range of 45 to 130 kg. Mean weight of male VDs was 70±11.3 (range 45–130) kg and female VDs 60.0±9.8 (range 45–110) kg. Mean weight for male RDs was 69.9±11.8 (range 45–120) kg and female RDs 65.2±10.2 (range 48–92) kg [Figure 2].
Figure 1.
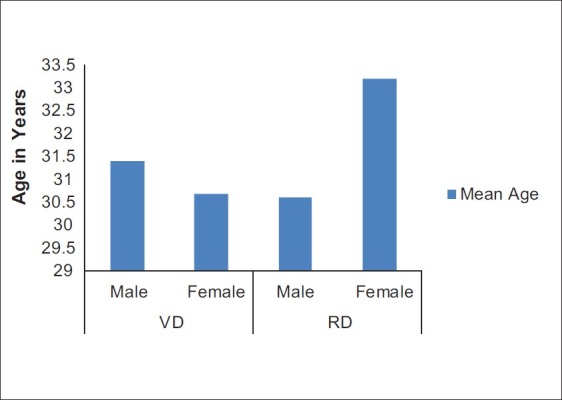
Mean age of blood donors in voluntary and replacement group
Figure 2.
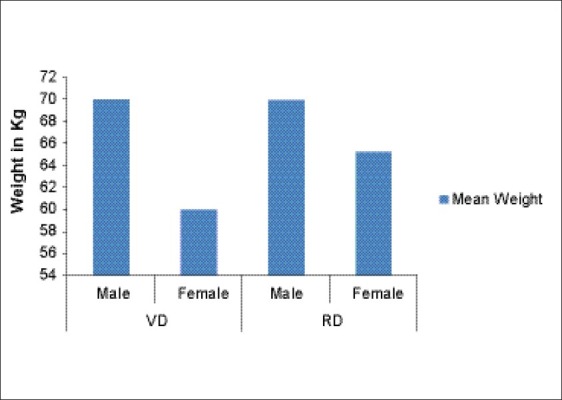
Mean weight of blood donors in voluntary and replacement group
Significantly higher numbers of VDs were repeat donors, i.e., 11,286 (49.97%) as compared to only 5028 (32.84%) repeat RDs (P<0.0001).
Adverse events
Out of 37,896 donors, AEs were observed in 948 donors, giving an overall incidence of 2.5%. Overall AE frequency in RDs and VDs was not significantly different; 562 out of 22,587 for VDs (2.49%) and 386 out of 15,309 for RDs (2.52%) (2.52% vs 2.49%; P=0.87). Out of these 948 AEs, 425 (44.8%) were observed in the department, and 523 (55.2%) in the blood donation camps (BDC), the difference was not found to be statistically significant. (P=0.72). The AEs in female donors were significantly higher as compared to male donors (4.8% vs 2.3%) (P<0.001) [Table 2]. There was no significant difference in the frequency of AEs between voluntary and replacement female donors (4.9% vs 4.6%) (P=0.97); however, voluntary male donors had significantly less AEs rate (2.1%) as compared to replacement male donors (2.5%) (P=0.03).
Table 2.
Comparison of adverse events between voluntary and replacement donors
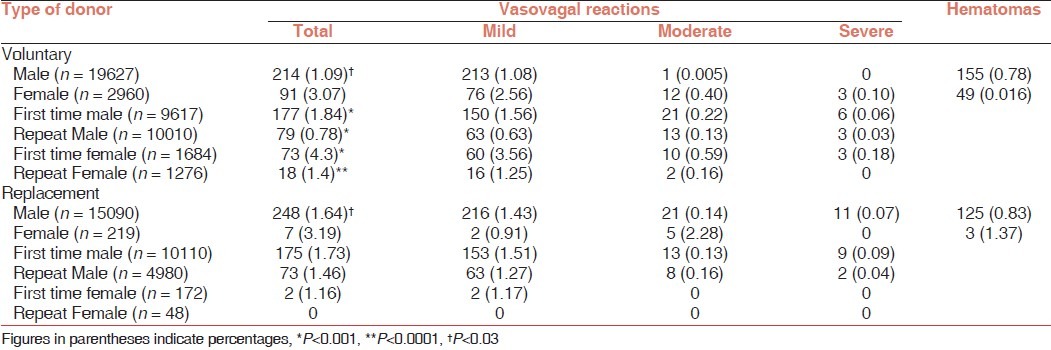
Out of 948 adverse events observed, majority, i.e., 602 (63.5%) were vasovagal in nature. Next common type of reaction was hematoma formation, 332 (35.0%). Other reactions formed a minority of total reaction. These were: nerve injury 2 (0.2%), thrombophlebitis 1 (0.1%), local allergy 1 (0.1%), and delayed vasovagal reactions, 10 (1.1%) [Table 2].
Vasovagal reactions
Out of 602 vasovagal reactions majority, i.e., 507 (84.2%) were mild in degree; 72 (12%) were moderate, and 23 (3.8%) were severe in degree. Donors experiencing a vasovagal reaction complained of different symptoms. In order of frequency, these were: perspiration 393 (65.3%), dizziness 336 (55.8%), pallor 333 (55.3%), anxiety 312 (51.8%), loss of consciousness 87 (14.5), nausea 61 (10%), vomiting 37 (6.1%), tonic–clonic convulsions 19 (3.2%), palpitations 13 (2.2%), weakness 10 (1.7%), feeling of warmth 9 (1.5%), feeling of cold 5 (0.8%), thirst 4 (0.7%), chest tightness 4 (0.7%), tetany 3 (0.5%), headache 3 (0.5%), twitching 3 (0.5%), dimness of vision with strain on eyes 2 (0.3%), incontinence 2 (0.3%), voice fadeout 2 (0.3%), tremors of hand 1 (0.2%), and cramps 1 (0.2%). In addition, one donor informed that she had started her menstruation after she got a reaction. Those having generalized convulsions had it for a mean duration of 5.3 seconds, ranging from 3 to 10 seconds. Systolic blood pressure ranged from un-recordable to 160 mmHg. Most of the donors had a reaction during or immediately after donation, while the donor was still lying on the donor couch, 389/602 (63.7%). No incidence of donor injury as a result of reaction occurred during the study period.
Factors affecting frequency of vasovagal reactions
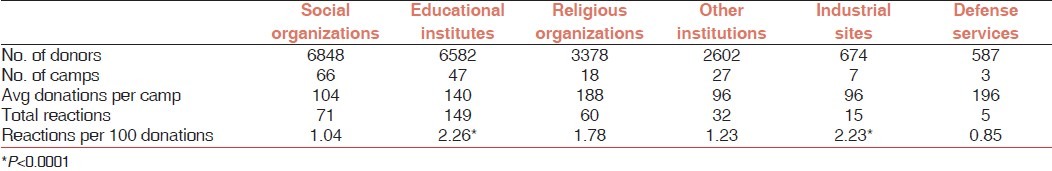
Site of donation: There was no significant difference in the overall vasovagal reaction rate amongst donors donating in hospital premises or BDC (1.58% vs. 1.59%). However, male VDs donating in BDC had significantly more reactions 1.59% vs. 0.94% (P=0.03) as compared with those donating in the department. On analyzing the frequency of reactions at voluntary BDCs, donors at educational institutions and industrial sites had higher number of reactions; least number were observed in camps organized by the defense services (P<0.0001) [Table 3].
Table 3.
Nature of camp and vasovagal reactions
Donation status: First-time male VDs had a reaction rate of 1.84%, which decreased to 0.79% with repeat donations (P<0.001). Similarly, first-time female VDs had a reaction rate of 4.33%, which declined to 1.41% (P<0.0001) on subsequent donations. Although similar trend was seen in RDs male and female, but the difference was not statistically significant.
Donor demographic factors: Overall reaction rate in female donors was significantly higher than males (4.8% vs. 2.3%) (P<0.001). Between female VDs and RDs, the reaction rates were similar (4.9% and 4.6% respectively). Male VDs had significantly lesser reactions (2.1%) as compared to RDs (2.5%) (P=0.03). A continuous decrease in the rate of vasovagal reaction was seen with increasing age of the donor (P<0.0001). Mean age of the donors who had a vasovagal reaction was 26±7 years, with a range of 18–54 years. Highest rate of reaction was seen in the donors within the age group 18–24 years (2.71%), which was significantly higher than the overall reaction rate (1.59%) (P<0.0001), and lowest rate of reaction was 0.33% in the age group 46–60 years, which was significantly lower than the overall reaction rate (P<0.0001).
Reaction rate in donors decreased as weight of the donor increased. Reaction rate in donors weighing less than 60 kg was significantly higher as compared with those weighing more than 60 kg (2.52% Vs. 1.25%; P<0.0001).
First time versus repeat donors: 21,584 (56.95%) of total 37,896 blood donors were first-time blood donors; 50.03% VDs and 67.15% RDs were first-time donors. Of the total 602 vasovagal reactions, most, i.e., 250 were seen in first-time VDs with a reaction rate of 2.21%. In case of repeat voluntary donors, this number was 97 with a reaction rate of 0.85%. Rate of reaction in VDs dropped significantly after first donation (2.21% to 0.85%; P<0.0001), but this decrease was not significant in case of RDs (1.76% to 1.47%; P=0.21) [Figure 3].
Figure 3.
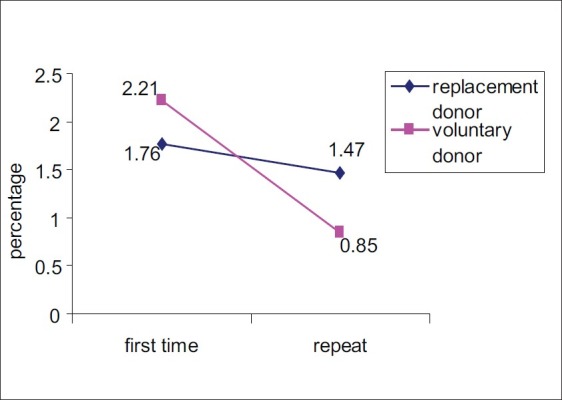
Trend in reaction rates in first time and repeat replacement and voluntary donors
Volume of blood collected: According to the donor weight either 350±3 mL (for donors weighing less than 55 kg) or 450±45 mL (donors weighing ≥55 kg) blood was collected. Accordingly, donors weighing less than 55 kg donated ≤7.78±0.78 mL/kg (11.11% of total blood volume), whereas donors weighing more than 55 kg donated ≤8.04±0.80 mL/kg (or 11.48% of total blood volume). Out of all the donors who had a vasovagal reaction, in 123 donors (20.4%) desired amount of blood could not be collected, resulting in under collection and wastage of the unit collected. Overall reaction frequency was significantly higher in donors (replacement as well as voluntary) donating 350±35 mL of blood (3.97%) as compared to those donating 450±45 mL blood (0.67%) (P<0.0001).
Since blood volume collected was adjusted as per weight of the donor, weight seemed to significantly affect the occurrence of reactions.
Psychological factors: After recovery from the reaction, the donors were interviewed regarding any predisposing psychological factors. 84.6% of the donors acknowledged one or more of the following conditions prior to or during donation: general apprehension about safety of blood donation (75.9%), painful phlebotomy (31.6%), knowledge of a friend's reaction to donation (19.9%), prolonged wait before donation (20.6%), and fear of needle and/or blood (15.6%). RDs in addition also expressed anxiety regarding the health status of their patients.
Other factors: There seemed to be no relationship with the time of last meal taken. 136 (22.3) donors had a vasovagal reaction during donation, 253 (41.4) immediately post donation, 124 (20.3) while taking refreshments, and 97 (15.8%) just before leaving the donation site. Only one donor (0.2%) had a reaction prior to phlebotomy.
Hematomas
A total of 332 hematoma formations occurred out of 37,896 donations (0.88%). These occurred at donation site and resulted into under collection; no hematoma formation was reported by the donor after leaving the donation site. Of all the phlebotomies performed during the study period, 24,879 (65.61%) were performed by phlebotomists having an experience of more than 5 years. Comparison of experience of phlebotomist vs. frequency of hematomas revealed that significantly higher number of hematomas were formed by less experienced phlebotomists, 4.7 per 1000 donations vs. 16.5 per 1000 donations (P<0.0001).
Discussion
AEs occurred in 2.5% of the donor population studied. These results are in agreement with some studies[4,6] but lower than others where prevalences varying from 8.9%[12] to 11–21%[3] have been reported. Variations may result due to differences in donor demographics, behavior of collection staff, use of donor chairs versus flat bed, and methodology used to obtain information regarding AEs from donors. Vasovagal reactions constituted 63.5% of all AEs and were mostly mild in nature. Majority occurred at donation site only. Young age, lower weight, female gender, and first-time donation status were associated with significantly higher reaction prevalence (P<0.001 to 0.0001). There was a significant drop in the reaction prevalence after the age of 36 years. Mean age of the donors who had a vasovagal reaction was 26 years, compared with the mean age of our total donor population, which was 31 years. Highest reaction prevalence (2.72%) was seen in donors 18–24 years of age and was significantly higher than the overall prevalence of 1.6% (P<0.0001). A study by France[13] postulated that baroreceptor sensitivity is decreased in healthy young individuals when they are physically or psychologically stressed. With increasing age, the body becomes more stable hemodynamically. Also, the young donors were more apprehensive to the pain of phlebotomy.
Frequency of reactions decreased as the weight of the donor increased from 45 kg to more than 80 kg (P<0.0001). Also, the mean weight of the donors who had a vasovagal reaction was less than the mean weight of the total donor population, an observation similar to that reported by Kasprisin et al.[14] Newman[7,15] showed that reaction rate was inversely proportional to the weight of the donor while Boynton and Taylor reported that reactions were twice that expected in donors weighing less than 120 lbs.[12] In contrast, in a study on Indian donors by Tondon et al.,[9] the weight of the donor had no significant effect on the occurrence of vasovagal reactions. The authors mention that at their centre, blood is drawn considering the weight and gender of the donor. At our centre also, the volume of blood collected depends upon the weight and gender (350 mL from female donors and those weighing less than 55 kg). Yet, we observed that weight had a significant association with occurrence of reactions. One possible reason could be the differences in age distribution of the donors. In our study 11,657 (30.8%) donors were in the 18–24 years age group and 20,744 (54.7%) in the 18–30 years age group, whereas in the study by Tondon et al.,[9] majority of the donors (38%) belonged to the age group of 31–40 years.
Female donors, both voluntary and replacement, had significantly higher reaction rate; twofold as compared to male donors. Most studies[4,16,17] have reported higher prevalence in female donors, although there is contradictory data too.[15,18] Repeat donation status lowered the chances of a vasovagal reaction significantly in VDs. This different behavior of voluntary and replacement donor can be partially explained by the “opponent-affective theory” of Solomon. When an aversive stimulus eliciting an emotional state (A) like blood donation is encountered and terminated, the individual experiences a qualitatively and hedonically opposite new state (B), which then gradually subsides and returns to neutrality. With repeated exposure to the event, state A becomes weaker and B stronger. The latter strengthens with repeated exposure, e.g., regular blood donation.[19] This may explain the motivational drive and decreased reaction prevalence in regular VDs. RDs on the contrary donate at irregular intervals and only when demanded by their patient's condition.
Another factor, which influenced the frequency of vasovagal reactions, was the site of BDC. This assumes importance in our scenario since BDCs are organized at sites convenient to the VDs. The prevalence of reaction was significantly higher in educational institutions and in industrial sites. In the former situation, younger and first-time donors constitute majority of the donor population, while in the latter sites, the staff may be under pressure to donate, hence more anxious. The least number of reactions were observed in BDCs organized by defense staff. This is in keeping with their spirit of courage and service. In contrast, in an earlier study from our institute, Agnihotri et al.[20] had reported least number of reactions from camps organized by religious organizations. Our findings did not substantiate this; probable reasons could be increased number of young donors and female donors in our study. We had earlier analyzed prevalence in trends of transfusion-transmissible infections over a period of 5 years and documented that student donors had the least prevalence and are the safest source of blood supply.[21] Hence, special care needs to be taken to reduce donation AEs in this category of VDs so that they can be motivated to become regular donors. Donors who experience a reaction are usually reluctant to return for repeat donation.[22] Majority of the donors with reactions admitted to anxiety of donation, fear of needle/pain/blood, and having witnessed a previous donor reaction. Hence, allocation of apprehension in donors, both through motivational strategies and pre-donation counseling, cannot be overemphasized.
Overall reaction rate between RDs and VDs did not seem to be significant on simple statistical analysis. However, further analysis showed the RDs who reacted had higher mean age and weight than VDs, and male RDs had significantly more AEs than male VDs. The reaction rate declined significantly in repeat VDs; in RDs, there was a downward trend but not significant. Hence it appears that there are probably psychological and attitudinal differences between the two categories of donors. Despite RDs donating in more comfortable premises designed as per regulatory requirements, stress on account of their patients’ health status appeared to be a predisposing factor in some of the RDs. VDs, on the other hand, donate in varying premises, which are very often not physically comfortable in our country, both due to infrastructure and weather problems. Studies comparing AEs in RDs and VDs are not available in literature; the only other study from India is on RDs, while studies from the developed countries are primarily on VDs.
Hematomas were the second commonest AE in donors. Demographic factors other than females donating in BDCs did not influence this reaction. The VDs here were mostly young female donors from colleges. However, the underlying factor seems to be the training of the phlebotomist, since those with longer experience caused significantly less hematomas. This observation is in agreement with Newman's study where incidence of hematoma was more when phlebotomist was untrained, had poor technique, or failed to select the best vein.[3] In a recent study by the American Red Cross on donor hemovigilance program, syncopal reactions were seen more frequently after whole blood donation, while hematomas were more common in platelet pheresis donors.[23] We still need to create voluntary plateletpheresis donor panels for evaluation of AEs in different types of donations.
Donor safety is an essential prerequisite to increase voluntary blood donation. One of the key objectives of our National Blood Policy is to achieve 100% voluntary blood donation,[24] the present national average being 61%. AE analysis helps in identifying the blood donors at risk of donor reactions and adopting appropriate donor motivational strategies, pre-donation counseling, and care during and after donation. This assumes importance in strengthening the voluntary blood donation program in our country.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.World Health Organization. Blood safety and donation. 2008. [Last cited 2010 Dec 10]. Available from: http://www.who.int/mediacentre/factsheets/fs279/en .
- 2.Lin JT, Ziegler DK, Lai CW, Bayer W. Convulsive syncope in blood donors. Ann Neurol. 1982;11:525–8. doi: 10.1002/ana.410110513. [DOI] [PubMed] [Google Scholar]
- 3.Newman BH. Donor reactions and injuries from whole blood donations (review) Transfus Med Rev. 1997;11:64–75. doi: 10.1016/s0887-7963(97)80011-9. [DOI] [PubMed] [Google Scholar]
- 4.Trouern-Trend JJ, Cable RG, Badon SJ, Newman BH, Popovsky MA. A case-controlled multicenter study of vasovagal reactions in blood donors: Influence of sex, age, donation status, weight, blood pressure, and pulse. Transfusion. 1999;39:316–20. doi: 10.1046/j.1537-2995.1999.39399219291.x. [DOI] [PubMed] [Google Scholar]
- 5.Tomasulo PA, Anderson AJ, Paluso MB, Gutschenritter MA, Aster RH. A study of criteria for blood donor deferral. Transfusion. 1980;20:511–8. doi: 10.1046/j.1537-2995.1980.20581034503.x. [DOI] [PubMed] [Google Scholar]
- 6.Newman BH, Siegfried BA, Buchanan LA. Donor reactions among African-American and Caucasian first-time whole-blood donors. Transfusion. 2005;45:1398–9. doi: 10.1111/j.1537-2995.2005.00212.x. [DOI] [PubMed] [Google Scholar]
- 7.Newman BH, Satz SL, Janowicz NM, Siegfried BA. Donor reactions in high-school donors: The effects of sex, weight, and collection volume. Transfusion. 2006;46:284–8. doi: 10.1111/j.1537-2995.2006.00713.x. [DOI] [PubMed] [Google Scholar]
- 8.Eder AF, Hillyer CD, Dy BA, Notari EP, 4th, Benjamin RJ. Adverse reactions to allogeneic whole blood donation by 16- and 17-year-olds. JAMA. 2008;299:2279–86. doi: 10.1001/jama.299.19.2279. [DOI] [PubMed] [Google Scholar]
- 9.Tondon R, Pandey P, Chaudhary R. Vasovagal reactions in ‘at risk donors’.A univariate analysis of age and weight on the grade of donor reactions. Transfus Apher Sci. 2008;39:95–9. doi: 10.1016/j.transci.2008.07.010. [DOI] [PubMed] [Google Scholar]
- 10.16th ed. Lucknow: Eastern Book Company; 2003. Drugs and Cosmetics Act 1940; pp. 279–303. [Google Scholar]
- 11.Rutman RC, Dpasuale-Barrios S. Donor Room Policies and Procedures. In: Green TS, Steckler D, editors. Donor Room Policies and Procedures. Arlington: American Association of Blood Banks; 1985. pp. 81–90. [Google Scholar]
- 12.Boynton MH, Taylor ES. Complications arising in donors in a mass blood procurement project. Am J Med Sci. 1945;209:421–36. [Google Scholar]
- 13.France C. Baroreflex sensitivity during noxious stimulation in vasovagal reactors to blood donation. Int J Psychophysiol. 1995;19:13–22. doi: 10.1016/0167-8760(94)00058-m. [DOI] [PubMed] [Google Scholar]
- 14.Kasprisin DO, Glynn SH, Taylor F, Miller KA. Moderate and severe reactions in blood donors. Transfusion. 1992;32:23–6. doi: 10.1046/j.1537-2995.1992.32192116426.x. [DOI] [PubMed] [Google Scholar]
- 15.Newman BH. Vasovagal reaction rates and body weight: Findings in high- and low-risk populations. Transfusion. 2003;43:1084–8. doi: 10.1046/j.1537-2995.2003.00478.x. [DOI] [PubMed] [Google Scholar]
- 16.Tomasulo PA, Anderson AJ, Paluso MB, Gutschenritter MA, Aster RH. A study of criteria for blood donor deferral. Transfusion. 1980;20:511–8. doi: 10.1046/j.1537-2995.1980.20581034503.x. [DOI] [PubMed] [Google Scholar]
- 17.McVay PA, Andrews A, Kaplan EB, Black DB, Stehling LC, Strauss RG, et al. Donation reactions among autologous donors. Transfusion. 1990;30:249–52. doi: 10.1046/j.1537-2995.1990.30390194347.x. [DOI] [PubMed] [Google Scholar]
- 18.Graham DT. Prediction of fainting in blood donors. Circulation. 1961;23:901–6. doi: 10.1161/01.cir.23.6.901. [DOI] [PubMed] [Google Scholar]
- 19.McCullogh J. National Blood Programs in developed countries. Transfusion. 1996;36:1019–32. doi: 10.1046/j.1537-2995.1996.36111297091749.x. [DOI] [PubMed] [Google Scholar]
- 20.Agnihotri SK, Sharma SK, Kumar S. Untoward reactions in blood donors. J Int Med. 1996;7:5. [Google Scholar]
- 21.Sharma RR, Cheema R, Vajpayee M, Rao V, Kumar S, Marwaha N, et al. Prevalence of markers of transfusion transmissible diseases in voluntary and replacement donors. Natl Med J India. 2004;17:19–21. [PubMed] [Google Scholar]
- 22.France CR, Rader A, Carlson B. Donors who react may not come back: Analysis of repeat donation as a function of phlebotomist ratings of vasovagal reactions. Transfus Apher Sci. 2005;33:99–106. doi: 10.1016/j.transci.2005.02.005. [DOI] [PubMed] [Google Scholar]
- 23.Eder AF, Dy BA, Kennedy JM, Notari EP, Iv, Strupp A, Wissel ME, et al. The American Red Cross donor hemovigilance program: Complications of blood donation reported in 2006. Transfusion. 2008;48:1809–19. doi: 10.1111/j.1537-2995.2008.01811.x. [DOI] [PubMed] [Google Scholar]
- 24.National Blood Policy. Objective-1: To reiterate firmly the Govt. commitment to provide safe and adequate quantity of blood, blood components and blood products. National AIDS Control Organization. Ministry of Health and Family Welfare. Govt. of India. 2007. [Last accessed on 2010 Dec 12]. pp. 7–8. Available from: http://www.nacoonline.org/upload/Final%20Publications/Blood%20Safety/National%20Blood%20Policy.pdf .


