Abstract
Despite its narrow therapeutic index, lithium remains widely used as a mood stabilizer for the treatment of bipolar disease. The cardiac side-effects of lithium have been well documented, and may induce non-specific T-wave flattening, prolonged QT interval, sinus node dysfunction and also ventricular tachycardia and ventricular fibrillation. We report the case of a 61-year-old male patient diagnosed with bipolar disorder who developed life-threatening cardiac manifestations secondary to severe lithium poisoning. Although hemodialysis was performed and the arrhythmias were adequately treated, the patient died on the sixth day after hospital admission due hemorrhagic complications after tracheostomy.
Keywords: Bipolar disorder, intensive care unit, life-threatening cardiac manifestations, lithium poisoning
Introduction
Lithium salts are widely employed as mood stabilizers in psychiatry. Their action mechanism remains unknown, although their effects on biological membranes have already been demonstrated.[1] A serum level lying in the range of 0.8 and 1.2 mEq/L is considered therapeutic.[2] The cardiovascular effects resulting from the use of lithium have been well documented for a broad range of plasma concentrations.[3] Lithium salts may induce T-wave flattening, sinus node dysfunction,[4–6] atrioventricular conduction abnormalities, ventricular extrasystole[7] and prolonged QT interval.[8] On rare occasions, ventricular tachycardia and fatal ventricular fibrillation have also been reported.
Case Report
A 61-year-old male patient with a 5-year history of bipolar disorder was admitted to the Emergency Unit with progressively decreased consciousness level, which had started 5 days previously. The patient has been taking lithium carbonate medication (600 mg/day) for the past 5 years and, due to his psychiatric condition, has been considered to have accidently ingested an overdose of lithium. Unfortunately, in the present investigation, we did not have the opportunity to accurately measure the serum level of lithium to precisely quantify the lithium overdose status. However, the patient's general clinical condition and the increasing reports of lithium intoxication in psychiatric patients have supported the putative diagnosis of lithium intoxication. He presented with sleepiness and prostration, along with mental confusion and rigidity of the lower extremities, which had worsened progressively over the 2 days prior to admission. He was also receiving insulin therapy, metformin 850 mg 3xday, thyroxine (T4) 50 mcg/day, enalapril 40 mg/day, atenolol 100 mg/day and lithium carbonate 600 mg/day.
Physical examination on admission revealed a non-pale, anicteric and acyanotic patient. Pulmonary auscultation revealed the presence of rales in pulmonary base. The respiratory rate was 29 bpm. Cardiac auscultation revealed irregular cardiac rhythm, heart rate of 130 bpm and blood pressure of 80 × 40 mmHg. Abdomen examination was normal.
Blood analysis showed hemoglobin = 12.5 g/dL, hematocrit = 36%, white blood cells (WBC) = 9500/mm³ (82% neutrophils and 18% lymphocytes), platelets 207,000/mm3 and multiple blood cultures negative for any pathogenic organisms. Chest X-radiography was normal.
Therefore, the proposal of lithium poisoning was then strongly suggested as a diagnostic hypothesis. The patient was transferred to the intensive care unit (ICU) and submitted to hemodialysis after hemodynamic stabilization. The initial lithium serum level was 2.9 mmol/L (reference values: 0.6–1.2 mmol/L), thereby confirming the initial diagnosis. Other biochemical tests revealed creatinine: 2.3 mg/dL, urea: 114 mg/dL, potassium: 3.1 mEq/L and sodium: 145mEq/L.
On the following day, mechanical ventilation and administration of dopamine were initiated because of hypotension and bradycardia. Brain tomography was normal and the electroencephalogram showed metabolic encephalopathy, ascribed to lithium poisoning. Echocardiogram was performed and revealed mildly dilated left atrium and hypertrophy of the left ventricle, and left ventricular systolic function was normal. The creatine kinase-MB fraction CKMB level was 132 U/L (normal range: 25 U/L) and cardiac troponin I was 20.92 μg/L (normal range: 0.16 μg/L); therefore, cardiac catheterization was performed to rule out an ischemic cause for recurrent severe arrhythmias in a patient who had past history of chest pain. The exam demonstrated that the coronary circulation was free of obstructive lesions.
The electrocardiogram (ECG) performed at admission evidenced atrial fibrillation, ST segment elevation of 1 mm diffusely, T-wave inversion and left ventricular overload [Figure 1a]. On the next day, the patient presented new event of atrial fibrillation with low-ventricular response, alternating with periods of bradycardia (HR: 45 bpm) and tachycardia (HR: 174b pm), thereby demanding electrical cardioversion, performed successfully. Three days after admission, the patient presented with ventricular tachycardia [Figure 1b] and bradyarrhythmia, which required implantation of temporary intravenous pacemaker for safe administration of antiarrhythmic agents. Two days later, the pacemaker for the clinical control of arrhythmias was turned off and the serum lithium levels had decreased to 0.6 mmol/L. The control ECG showed sinus rhythm and absence of arrhythmias.
Figure 1a.

Electrocardiogram carried out at admission showing atrial fibrillation with diffuse ST segment depression of 1 mm, T-wave inversion and left ventricular overload
Figure 1b.
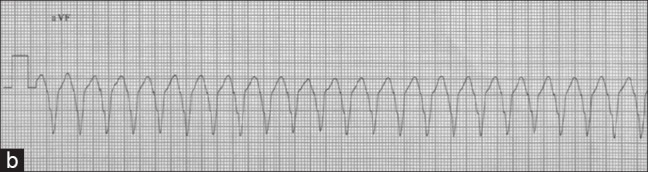
Electrocardiogram at 3 days after admission revealing ventricular tachycardia
The patient underwent tracheostomy, but presented hemorrhagic complications due to this procedure 4 days later. The patient progressed with cardiorespiratory arrest by pulseless electrical activity. Resuscitation manoeuvres were unsuccessful, and the patient died.
Discussion
Lithium was introduced for the treatment of bipolar disorder in 1949, and has since then been considered the main therapeutic approach for this condition.[9]
The lithium has a small therapeutic index and, therefore, lithium intoxication still remains an important issue during lithium-based therapy. Lithium intoxication may be avoided by an attentive administration, especially during combined multidrug therapies. Moreover, the periodical monitoring of lithium plasmatic concentrations besides the clinical observation and correct and continuous education process of patients and health supporting professional team to promptly identify the first signs of lithium intoxication.[10] The patients under lithium therapy are usually submitted to continuous therapeutic protocols usually associated with multidrug interventions. The drug interactions can even enhance the risks of lithium intoxication. The concomitant use of drugs that interfere in the renal function, decreasing the lithium excretion, can even worsen the risks of lithium intoxication even when correct lithium doses are used. Diuretics and neuroleptic drugs, anticonvulsants, angiotensin-converting enzyme inhibitors (ACE inhibitors) and several non-steroidal anti-inflammatory drugs may interact and lead to toxic effect when administered in association with lithium. The chronic renal failure associated with arterial hypotension caused by lithium overdose may have further reduced the lithium excretion. Moreover, the enalapril, a potentially nephrotoxic drug, may have contributed to worsening the intoxication illness observed in this case report.
According to Waring, hemodialysis is more efficient for lithium clearance than other techniques, such as hemodiafiltration.[11] In order to re-establish the therapeutic lithium levels, our patient was submitted to three conventional hemodialysis sessions, even though data on his renal function were only slightly altered. It is noteworthy that in the present case there were severe clinical manifestations such as complex and persistent arrhythmias, whereas lithium concentrations were only moderately increased. It must be highlighted that there were no other apparent explanations for the presence of these complex arrhythmias, once invasive investigation did not reveal any anatomical substrate that could account for such a finding. Moreover, the patient did not present any previous symptoms that could suggest the presence of cardiac arrhythmias. The normal left ventricular systolic function excludes the putative diagnosis of Takotsubo cardiomyopathy that could be considered due to the increased levels of troponin in the absence of obstructive coronary lesion. In this case, the increased levels of troponin could be explained by the sepsis and renal failure conditions. Increased levels of troponin have been observed in septic patients, and the troponin levels in these patients also appears to be a predictor of short- and possibly also long-term outcome in septic patients.[12] The causes of troponin increase in critically ill patients are not well understood, but it may be related to the massive release of pro-inflammatory cytokines with miotoxic properties and also by the direct action of bacterial endotoxin or even by the ischemia related to the microvascular dysfunction. The prevalence and clinical significance of elevated troponin levels in patients with renal failure have been recently reviewed elsewhere. Although the exact causes of troponin elevation in these patients remain to be elucidated, increasing levels of troponin generally have been associated with worse clinical outcome.[13]
In conclusion, the present case report is important for intensivist professionals to reflect on the cardiac risks and ECG changes associated with lithium toxicity, including supraventricular (atrial fibrilation) and ventricular (non-sustained ventricular tachycardia) rhythm disturbances that can occur abruptly or during the therapeutics. This report also demonstrates the need to include lithium intoxication in the differential diagnosis of drug overdose with prominent ECG changes.
Acknowledgments
The authors are grateful to Fundação de Amparo ao Ensino, Pesquisa e Assistência (FAEPA) do Hospital das Clínicas and Faculdade de Medicina de Ribeirão Preto-USP for financial support. MGM and MAM also thank Helena Rodrigues Villela Machado, Lucilaine de Oliveira and Zilda Maria da Silva for their assistance during the data collection. OAMF also thanks the CNPq research fellowship program for the financial support.
Footnotes
Source of Support: OAMF also thanks the CNPq research fellowship program for the financial support.
Conflict of Interest: None declared.
References
- 1.Baldessarini RJ, Tarazi FI. Drugs and the treatment of psychiatric disorders. Psychosis and mania. In: Hardman JG, Limbird LE, editors. Goodman & Gilman's. The pharmacological basis of therapeutics. 10th ed. New York: McGrawHill; 2001. pp. 507–11. [Google Scholar]
- 2.Griswold KS, Pessar LF. Management of bipolar disorder. (1357-8).Am Fam Physician. 2000;62:1343–53. [PubMed] [Google Scholar]
- 3.Waring WS. Delayed cardiotoxicity in chronic lithium poisoning: discrepancy between serum lithium concentrations and clinical status. Basic Clin Pharmacol Toxicol. 2007;100:353–5. doi: 10.1111/j.1742-7843.2007.00054.x. [DOI] [PubMed] [Google Scholar]
- 4.Wellens HJ, Cats VM, Duren DR. Symptomatic sinus node abnormalities following lithium carbonate therapy. Am J Med. 1975;59:285–7. doi: 10.1016/0002-9343(75)90365-4. [DOI] [PubMed] [Google Scholar]
- 5.Wilson JR, Kraus ES, Bailas MM, Rakita L. Reversible sinus-node abnormalities due to lithium carbonate therapy. N Engl J Med. 1976;294:1223–4. doi: 10.1056/NEJM197605272942209. [DOI] [PubMed] [Google Scholar]
- 6.Rosenqvist M, Bergfeldt L, Aili H, Mathé AA. Sinus node dysfunction during long-term lithium treatment. Br Heart J. 1993;70:371–5. doi: 10.1136/hrt.70.4.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bucht G, Smigan L, Wahlin A, Eriksson P. ECG changes during lithium therapy.A prospective study. Acta Med Scand. 1984;216:101–4. doi: 10.1111/j.0954-6820.1984.tb03777.x. [DOI] [PubMed] [Google Scholar]
- 8.Mamiya K, Sadanaga T, Sekita A, Nabeyama Y, Yao H, Yukawa E. Lithium concentration correlates with QTc in patients with psychosis. J Electrocardiol. 2005;38:148–51. doi: 10.1016/j.jelectrocard.2004.10.004. [DOI] [PubMed] [Google Scholar]
- 9.Jefferson JW. Current and potential uses of lithium. J Clin Psychiatry. 1990;51:392–9. [PubMed] [Google Scholar]
- 10.Delva NJ, Hawken ER. Preventing lithium intoxication. Guide for physicians. Can Fam Physician. 2001;47:1595–600. [PMC free article] [PubMed] [Google Scholar]
- 11.Waring WS. Management of lithium toxicity. Toxicol Rev. 2006;25:221–30. doi: 10.2165/00139709-200625040-00003. [DOI] [PubMed] [Google Scholar]
- 12.Markou N, Gregorakos L, Myrianthefs P. Increased blood troponin levels in ICU patients. Curr Opin Crit Care. 2011;17:454–63. doi: 10.1097/MCC.0b013e3283491f0d. [DOI] [PubMed] [Google Scholar]
- 13.Roongsritong C, Warraich I, Bradley C. Common causes of troponin elevations in the absence of acute myocardial infarction: Incidence and clinical significance. Chest. 2004;125:1877–84. doi: 10.1378/chest.125.5.1877. [DOI] [PubMed] [Google Scholar]


