Abstract
STUDY DESIGN
Case control.
OBJECTIVES
To use modified NFL Combine testing methodology to test for functional deficits in athletes following anterior cruciate ligament (ACL) reconstruction following return to sport.
BACKGROUND
There is a need to develop objective, performance-based, on-field assessment methods designed to identify potential lower extremity performance deficits and related impairments in this population.
METHODS
Eighteen patients (mean ± SD age, 16.9 ± 2.1 years; height, 170.0 ± 8.7 cm; body mass, 71.9 ± 21.8 kg) who returned to their sport within a year following ACL reconstruction (95% CI: 7.8 to 11.9 months from surgery) participated (ACLR group). These individuals were asked to bring 1 or 2 teammates to serve as control participants, who were matched for sex, sport, and age (n = 20; mean ± SD age, 16.9 ± 1.1 years; height, 169.7 ± 8.4 cm; body mass, 70.1 ± 20.7 kg). Functional performance was tested using the broad jump, vertical jump, modified long shuttle, modified pro shuttle, modified agility T-test, timed hop, triple hop, single hop, and crossover hop tests. A 1-way multivariate analysis of variance (MANOVA) was used to evaluate group differences for dependent performance variables.
RESULTS
The functional performance measurements of skills requiring bilateral involvement of both lower extremities showed no group differences between the ACLR and control groups (P>.05). An overall group difference (P = .006) was observed for the combined limb symmetry index (LSI) measures. However, the modified double-limb performance tasks (long shuttle, modified agility T-test, and pro shuttle) were not, independently, sufficiently sensitive to detect limb deficits in individuals with ACL reconstruction. Conversely, the LSI on the distance measures of the single-limb performance tasks all provided moderate to large effect sizes to differentiate between the ACLR and control groups, as the individuals who had ACL reconstruction demonstrated involved limb deficits on all measures (P<.05). Finally, the LSI for the timed hop test was not different between groups (P>.05).
CONCLUSIONS
These findings indicate that, while unilateral deficits are present in individuals following ACL reconstruction, they may not be evident during bipedal performance or during modified versions of double-limb performance activities. Isolation of the involved limb with unilateral hopping tasks should be used to identify deficits in performance.
Keywords: anterior cruciate ligament, hop tests, knee, prevention
In the past 25 years, study of the anterior cruciate ligament (ACL) has resulted in nearly 10 000 scientific articles indexed on Medline that focus on the investigation of injury incidence, mechanism of injury, surgical repair techniques, and rehabilitation of this important knee-stabilizing ligament. Due to the significant detrimental effects of ACL injury in young athletes, such as loss of entire seasons of sports participation and possible scholarship funding, significantly decreased academic performance,9 long-term disability, and up to 105 times greater risk of radiographically diagnosed osteoarthritis,3 research efforts have focused on optimization of interventions to improve outcomes following surgical reconstruction.
Reconstruction procedures consistently restore joint stability to the previous level, and advances in graft reconstruction and fixation techniques have led to the development of accelerated rehabilitation programs.46,47 These rehabilitation protocols include progression through the acute, subacute, functional, and return-to-activity51 phases of rehabilitation. Often, the focus is on the management of the acute and subacute phases, with relatively stringent guidelines regarding progression of weight-bearing and range of motion (ROM), and the selection of specific types of exercises. These guidelines and supervised therapy can significantly improve the early post-surgical outcomes.14 In contrast, guidelines in the final phases of rehabilitation are typically more general, with more global categorizations of appropriate exercises and progressions and the goal of transitioning the athlete following ACL reconstruction from the ability to perform activities of daily living (ADL) to proficiency with higher level sport-related activities.16,45,50,51 For instance, the typical ACL reconstruction protocols lack objective guidelines to systematically transition the athlete’s rehabilitation from activities focused on restoring techniques in uniplanar planned movements to those that develop proficiency with multiplanar movements and ultimately train mastery of dynamic neuromuscular control requiring power generation and absorption.29
A significant goal of the final return-to-sport phase of rehabilitation is to functionally progress and transition the athlete towards proficient performance of higher level sport-related activities.16,45,50,51 The “release for full activity” is a potentially sensitive landmark for the athlete who has a strong desire to return to immediate high-level sports participation. Rehabilitation guidelines for appropriate transition and integration into high-level activities are not well documented. For the treating clinician and recovering athlete, this phase of rehabilitation is often further complicated by pressure from coaches, parents, and teammates to accelerate the return-to-sport timeline. During this phase of rehabilitation, the treating clinician must be especially cognizant of the potential gap between the athlete’s perceived versus actual sports readiness, as subjective scores often do not correlate to quantified function and strength scores in athletes with ACL injuries and reconstructions.30,32,42 In the absence of objective measures that identify potential deficits,11 it may be difficult for clinicians to justify continued sport restriction and to identify and address persistent functional deficits related to the initial ACL injury or reconstruction.
The limiting of financial resources allocated to healthcare has increased the role of on-the-field individuals in the progression and transition of athletes’ return to sport following ACL reconstruction. As such, the reintegration of athletes into unrestricted sports participation is often characterized by participation in progressively challenging on-field activities with the team (eg, drills and technique training) under the guidance of the field clinician. These sport reintegration activities emphasize proper technique, as well as performance training, to prepare the athlete for unrestricted sport participation. However, the commonly used drills and performance-based training activities, such as those performed in the NFL Combine, are bilateral in their task demands, and the performance of bilateral drills and activities may mask deficits of the involved lower extremity that persist into this phase of rehabilitation.
Following ACL reconstruction, deficits in the involved lower extremity persist long after individuals return to full activity. Several studies document reduced functional scores, asymmetries in performance-based measures of function, and deficits in quadriceps femoris muscle strength after return to activity and up to 18 to 24 months following reconstruction.2,18,19,39,41,52,53 Single-limb hop tests are often used to identify persistent limb asymmetries in performance of higher level tasks, and deficits are quantified with a limb symmetry index (LSI) [(involved side performance/uninvolved side performance) × 100%].6,44 Deficits in performance on single-leg hop tests and quadriceps muscle strength are often present in athletes following ACL reconstruction when they are cleared for unrestricted sport participation.44 Impairments and performance limitations that persist in the end stages of rehabilitation and beyond may be masked during on-field participation of predominantly bilateral, performance-based tasks. As such, it is likely that athletes will participate in the on-field sport reintegration stage of rehabilitation with persisting unilateral deficits.
There is a need to develop objective, performance-based, on-field assessments designed to identify potential lower extremity deficits in the late stage of rehabilitation following ACL reconstruction. In an attempt to fill this need, we developed a series of tests based on the activities performed during the NFL Combine, which were modified to perform cutting and shuffling movements in a unilateral manner. Performance tests were taken and modified from the NFL Combine, as these activities are routinely used to assess and train performance across many different sports and athletic levels.
The purpose of this study was to determine if existing bilateral tests can be modified to expose unilateral lower limb deficits and to compare them to single-leg hop tests presently used for this purpose. We hypothesized that the modified NFL Combine testing (modified double-limb performance testing) and single-limb performance testing (single-leg hop tests) would identify deficits in the involved limb of athletes following ACL reconstruction who were cleared for unrestricted return to sport. We further hypothesized that athlete performance on NFL Combine activities (double-limb performance testing) would show performance equal to uninjured individuals.
METHODS
Participants
Eighteen individuals (mean ± SD age, 16.9 ± 2.1 years; height, 170.0 ± 8.7 cm; body mass, 71.9 ± 21.8 kg) who had undergone a unilateral ACL reconstruction (ACLR group) and returned to their primary sport (football, soccer, basketball, or volleyball) within a year following reconstruction (95% CI: 7.8 to 11.9 months from surgery) were recruited to participate. Participants in the ACLR group were asked to bring 1 or 2 teammates with them to serve as control group participants matched for activity level, sex, sport, and age (n = 20; mean ± SD age, 16.9 ± 1.1 years; height, 169.7 ± 8.4 cm; body mass, 70.1 ± 20.7 kg). Informed written consent was obtained from all participants (legal guardian if under 18 years of age) and approved by The Institutional Review Board of Cincinnati Children’s Hospital Medical Center. After informed consent was obtained, height and weight were measured and recorded. Participants were given a questionnaire to report their prior history of knee injury, which was corroborated by a personal interview with the investigator.35 Concomitant injuries (eg, meniscal, other ligamentous, chondral) and specifics regarding surgical procedure (eg, graft type) were documented but were not further analyzed in this study.
Procedures
The current report provides an approach to applying objective field-testing methodology with functional tests designed to identify lower extremity asymmetry and to demonstrating the potential use of these tests as reliable measures. These data were collected in a large-scale 1-day field setting designed to replicate NFL Combine testing procedures, though with some additional modifications. Athletes were randomly assigned to 1 of the 9 testing stations and proceeded through testing in a systematic manner. At each testing station, the same researcher instructed participants in performing the appropriate test then demonstrated its performance. If a task was not performed according to instructions or data could not be recorded, the participant immediately stopped and rested. The participants in both groups were athletes involved in running and cutting sports, with previous experience performing activities similar to the demands of the tasks used for testing. Accordingly, proper test performance was most often obtained after only 1 practice trial by each participant. Limb testing order was counterbalance randomized. After each test station, participants were given a minimum of 2 minutes’ rest and were encouraged to wait until they achieved full recovery before testing the opposite limb or transferring to the next station.
Double-Limb Performance Testing
Broad Jump
The broad jump distance was measured on a testing mat and recorded to the nearest centimeter (FIGURE 1). Athletes were instructed to start with the toes of both feet on a line and to use arm swing to leap forward as far as possible. Distance was measured from the start line to where the closest body segment touched on the test mat. Athletes were allowed 2 trials to achieve maximum broad jump distance to be recorded for analysis.
FIGURE 1.
Broad jump test.
Vertical Jump
Vertical jump height was measured on an MX1 vertical jump trainer (MXP Sports, Reading, PA) (FIGURE 2). Prior to the test, each participant’s overhead reach was determined by having the participant reach directly overhead with both hands up towards the ball, with the midline of the basketball aligned with the distal interphalangeal joint of the right and left middle fingers. The participant was told to use a natural overhead reach (no exaggerated superior rotation of the shoulder girdle). The digital readout of the system was zeroed to subtract overhead reach from jump height and thus to provide actual vertical displacement during the vertical jump testing. Each participant stood 30.5 cm behind the midpoint of the MX1 ball attachment and performed a countermovement vertical jump off both feet and grabbed the ball with both hands. The height of the MX1 was adjusted to the maximum height from which the participant could grab the ball and maintain grip on the ball until landing. The ball height was raised incrementally (2–5 cm), until the athlete could not pull the ball down from a height after 3 successive trials. The highest successful attempt was recorded. Prior authors have demonstrated countermovement vertical jump testing to have a test-retest reliability of 0.993.48 We previously observed that adding a goal provides a valuable extrinsic motivator to encourage maximal effort during the task.8
FIGURE 2.

Standing vertical jump test and measurement.
Modified Double-Limb Performance Testing
The T-test, pro shuttle, and long shuttle activities are used in field and NFL Combine settings to determine timed performance on tasks related to sports that require quick starts, dynamic changes in direction, and efficient movement. However, the standard performance of each of these tests combines left and right directional changes. While this is functionally ideal for individuals who require cutting from both sides, it is not as useful for evaluation and comparison of potential unilateral deficits. Therefore, the tests were modified to isolate cutting and shuffles in a unilateral manner.29
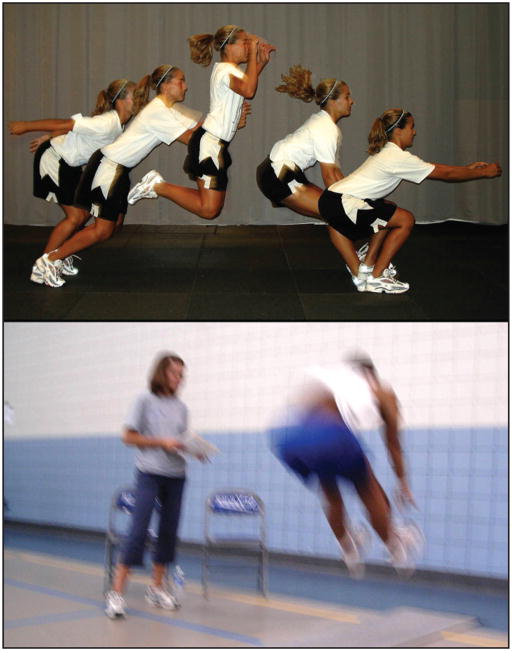
Modified Agility T-Test
The modified agility T-test (FIGURE 3) was developed from the standard T-test to evaluate lower extremity side-to-side differences in cutting and running maneuvers. The start limb for the modified agility T-test was counterbalance randomized. The participant was initially guided through the course by the test administrator, who emphasized the importance of performing a shuffling movement and not running or using crossover steps during the lateral movement portions of the test. The participants informed the investigators when they were ready to begin the test, and timing gates were zeroed. Each athlete initiated movement at a self-selected time of readiness, and timing began when any portion of the athlete’s body bisected the timing gate. All trials were electronically timed with SPARQ XLR8 digital timing system (Nike Inc, Beaverton, OR). After the participants felt they had an adequate rest (at least 2 minutes), the contralateral direction was tested. The total time was recorded for each limb. One successful trial was performed per limb, and the test run with shuffle push-off limb (the involved limb driving push-off during the lateral shuffle) was categorized as the involved trial. We have previously demonstrated that the modified T-test has good reliability in NFL Combine testing methods.13
FIGURE 3.
Modified agility T-test.
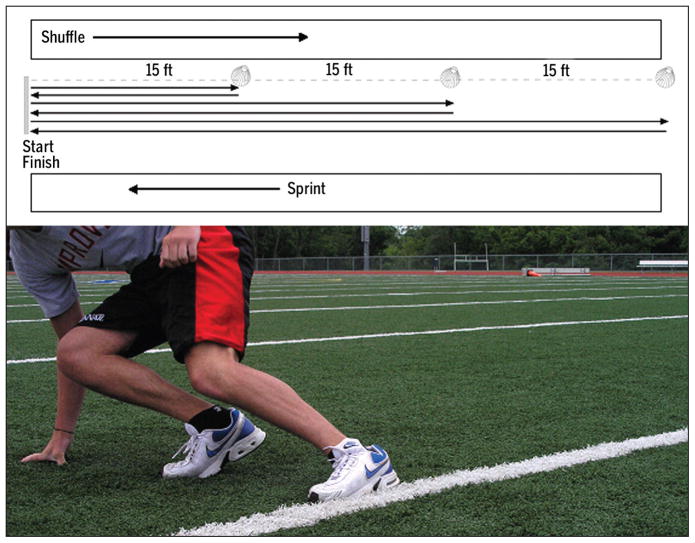
Modified Pro Shuttle
The pro shuttle was modified from the standard NFL Combine testing to force the athlete to complete the task in each direction instead of self-selected preference only (FIGURE 4). The participant was initially guided through the task by the test administrator, who emphasized the importance of performing a shuffling movement and not running or using crossover steps during the lateral movement portions of the test. Each athlete was instructed to begin in a 3-point stance, with either the right or left hand touching the ground directly in front of, and in line with, the middle cone and the feet straddling the line. The participant was instructed to initiate the movement with a self-selected starting point. Timing began when hand pressure was no longer sensed by the timing pad. The athlete’s movement was initiated in the left-hand direction if the left hand was touching the ground, or in the right-hand direction if the right hand was touching the ground. Once movement was initiated, the athlete was instructed to sprint to, and touch with the outside hand, the cone 15 ft (4.57 m) from the middle, then to reverse direction, run to the opposite cone 30 ft (9.14 m) away, and touch that line with the outside hand. To finish, the athletes were instructed to reverse direction again and sprint through the electronic timing gate (SPARQ XLR8 digital timing system) extending from the middle cone. After the participants felt that they had an adequate rest (at least 2 minutes), they performed the modified pro shuttle facing the opposite (180° from previous test) direction. The total time was recorded to complete the task for each limb. One successful trial was performed per limb, and the test run with initial shuffle push-off limb (the limb with ACL reconstruction driving initial push-off) was categorized as the involved trial. The start limb for the modified pro shuttle was counterbalance assigned.
FIGURE 4.
Modified pro shuttle.
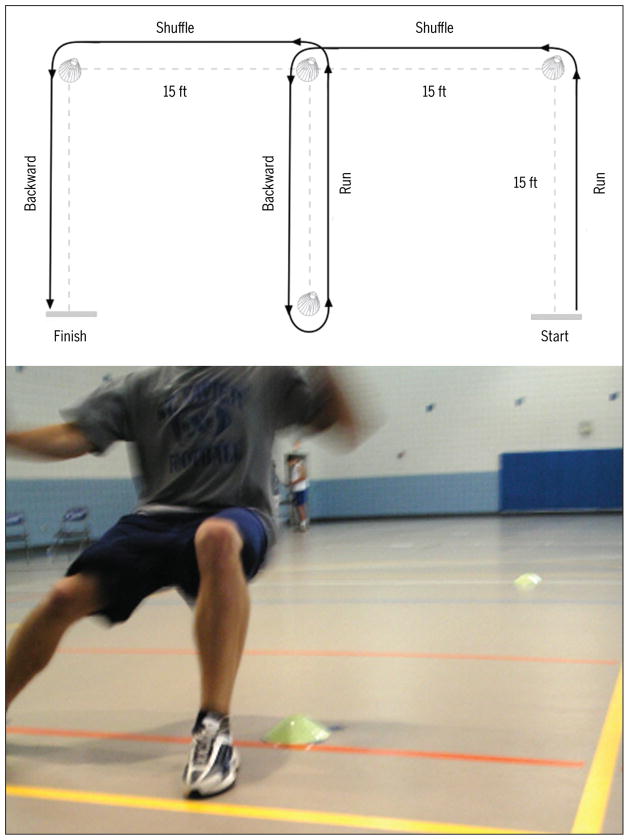
Modified Long Shuttle
The long shuttle was modified from the NFL Combine long shuttle to isolate the push-off limb during the activity (FIGURE 5). The start limb for the modified long shuttle was counterbalance assigned. The participant was initially guided through the course by the test administrator, who emphasized the importance of performing a shuffling movement and not running or using crossover steps during the lateral movement portions of the test. From a starting line, the participants were instructed to shuffle (without crossover steps) 15 ft (4.57 m), to touch the line or over the line with their fingers, to sprint back to the starting line touch point, then to shuffle (without crossover steps) to the 30-ft (9.14 m) touch point and sprint back to start touch point, and finally to shuffle (without crossover steps) to the 45-ft (13.72 m) touch point and sprint back, breaking through the electronic timing gate. Athletes were required to bend down and touch the line at each 15-, 30- and 45-ft interval, for a total of 5 line touches. After the participants felt they had an adequate rest (at least 2 minutes), they performed the modified long shuttle facing the opposite direction (180° from previous test). The total time was recorded to complete the task for each limb. The limb that was isolated during the shuffle push-offs was categorized as the testing side during the trials. One successful trial was performed per limb.
FIGURE 5.
Modified long shuttle.
Single-Limb Performance Testing
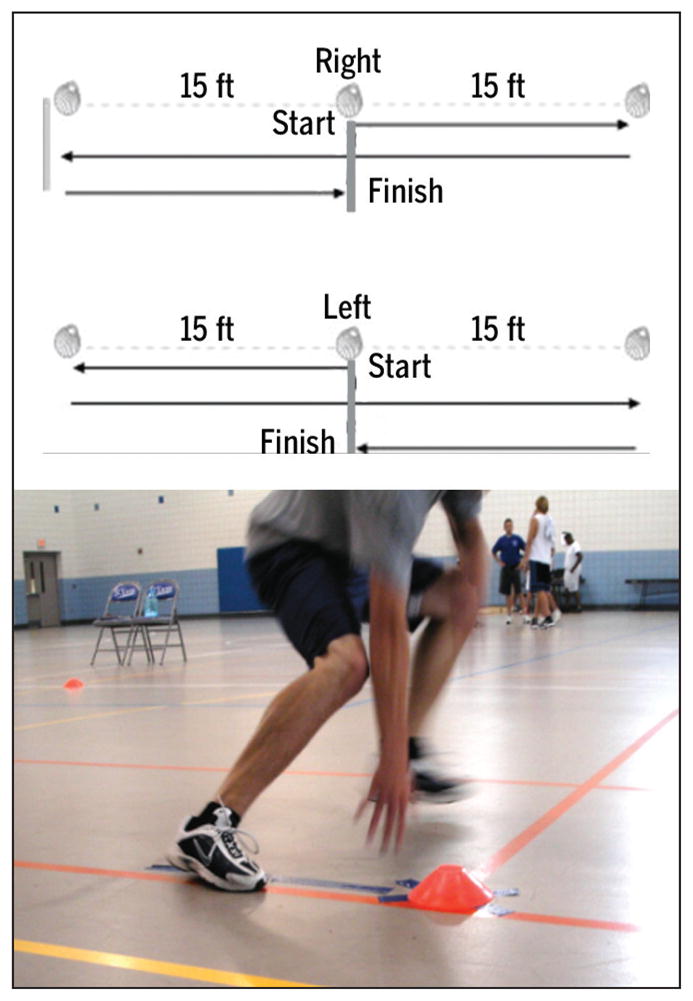
Single Hop for Distance
The athlete’s starting position for this maneuver was a semi-crouched position on the single limb being tested. The athlete was instructed to initiate the hop by swinging the arms forward, simultaneously extending at the hip and knee, and hopping forward as far as possible while being able to land safely on the same limb. A stabilized, 1-second landing on the hop limb was required for a successful trial (FIGURE 6A). Of the 2 trials, that with the greatest distance was used for further analysis. Testing was performed for both limbs, and the first limb tested was determined with counterbalance randomization. Distance was measured to the nearest centimeter on a standard measuring tape affixed to the floor.
FIGURE 6.
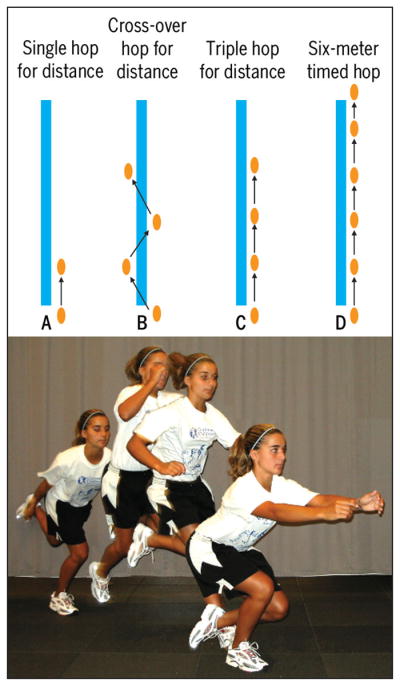
Hop tests.
Crossover Hop for Distance
The starting position for this maneuver was with the athlete in a semi-crouched position on the single limb being tested. The athlete was instructed to initiate the hop by swinging the arms forward and hopping forward as far as the athlete could and land safely on the same foot but on the opposite side of the line medial to the stance limb. Athletes were instructed to immediately redirect into 2 subsequent forward-directed hops, crossing over the midline with each hop. The final landing on the hop limb was required to be stabilized and held for 1 second to be recorded as a successful trial (FIGURE 6B). The trial with the greatest distance out of 2 trials was used for further analysis. Both limbs were tested, with the first limb to be tested determined by counterbalance randomization. Distance was measured to the nearest centimeter on a standard measuring tape affixed to the floor.
Triple Hop for Distance
The starting position for this maneuver was a semi-crouched position on the single limb being tested. The athlete was instructed to initiate the hop by swinging the arms forward, while hopping forward as far as possible and safely landing on the same limb, and to immediately redirect into 2 subsequent hops, holding the third landing. The final landing on the hop limb had to be stabilized and held for 1 second to be recorded as a successful trial (FIGURE 6C). The trial with the greatest distance out of 2 trials was used for further analysis. Testing was performed for both limbs, and the limb tested first was determined with counterbalance randomization. The distance was measured to the nearest centimeter on a standard measuring tape affixed to the floor.
Six-Meter Timed Hop
The starting position for this maneuver was with the athlete in a semi-crouched position on the single limb being tested. The athlete began with the toe on the start transmitter. Timing began when toe pressure was removed and ended when the athlete interrupted the infrared beam at the distance of 6 m from the starting line. The athlete was instructed to hop on the single limb as fast as possible to reach the finish line. The fastest time of 2 successful trials measured using the Speed Trap II timing system (Brower Timing Systems, Draper, UT) (FIGURE 6D) was used for data analysis. Testing was performed for both limbs, and the limb to be tested first was determined with counterbalance randomization.
Statistics
Two separate 1-way multivariate analyses of variance were employed to investigate the group differences (ACLR versus control) for the double-limb performance measures and LSI measures for the modified double-limb and single-limb performance tests. LSI for the distance performance measurements was calculated as the ratio of the value for the involved side, divided by the value for the uninvolved side, multiplied by 100; LSI for the timed performance measurements was calculated as the ratio of the value for the uninvolved side, divided by the value for the involved side, multiplied by 100. LSI values are, therefore, expressed in percentages, with a score lower than 100% indicating a deficit (less distance covered or more time used) of the involved side. The dominant limb was determined by asking the participants which leg they would use to “kick a ball as far as possible.” The involved limb of individuals in the ACLR group was matched to the nondominant limb of individuals in the control group. Preliminary assumption testing was performed to check for univariate and multivariate outliers, normality, and multicollinearity, with no serious violations noted. Statistical analyses were conducted in SPSS Version 18.0 (SPSS Inc, Chicago, IL). Statistical significance was established a priori at P<.05.
RESULTS
The participants in the ACLR group were not different from those in the control group for age, height, and mass (P>.05). TABLES 1 and 2 present the absolute performance scores, split by group for the male and female participants. The double-limb performance tests showed no group differences between ACLR and control groups (P>.05). The ACLR group demonstrated a mean ± SD countermovement vertical jump maximum height of 40.1 ± 11.3 cm, compared to 41.3 ± 7.2 cm for the control group (P>.05). The broad jump distance was also similar between the ACLR (176.3 ± 34.0 cm) and control (169.7 ± 28.3 cm) groups (P>.05).
TABLE 1.
Mean Absolute Scores on the Tests for Male Participants*
| Test/Participant Group | Control | ACLR |
|---|---|---|
| Vertical jump, cm | 49.3 (15.3, 23.5) | 49.9 (14.8, 24.5) |
| Broad jump, cm | 201.4 (66.4, 92.2) | 213.0 (63.6, 104.2) |
| Long shuttle, s† | ||
| Uninvolved/dominant† | 8.7 (8.0, 9.3) | 8.7 (7.0, 10.4) |
| Involved/nondominant‡ | 8.5 (7.6, 9.4) | 8.7 (6.9, 10.5) |
| MAT, s | ||
| Uninvolved/dominant† | 10.0 (8.7, 11.3) | 10.3 (8.0, 12.6) |
| Involved/nondominant‡ | 10.1 (8.5, 11.6) | 10.4 (7.2, 13.6) |
| Pro shuttle, s | ||
| Uninvolved/dominant† | 5.2 (5.0, 5.5) | 5.3 (4.4, 6.3) |
| Involved/nondominant‡ | 5.3 (5.2, 5.4) | 5.2 (4.0, 6.5) |
| Single hop, cm | ||
| Uninvolved/dominant† | 194.3 (158.0, 230.5) | 197.3 (142.0, 252.5) |
| Involved/nondominant‡ | 199.2 (166.8, 231.7) | 184.9 (108.4, 261.4) |
| Triple hop, cm | ||
| Uninvolved/dominant† | 539.0 (387.4, 690.5) | 541.8 (300.3, 783.2) |
| Involved/nondominant‡ | 546.8 (422.1, 671.5) | 513.3 (230.9, 795.6) |
| Crossover hop, cm | ||
| Uninvolved/dominant† | 504.4 (360.2, 648.6) | 499.0 (245.0, 753.0) |
| Involved/nondominant‡ | 496.8 (377.2, 616.4) | 468.5 (177.6, 759.4) |
| Timed hop, s | ||
| Uninvolved/dominant† | 2.5 (2.0, 3.0) | 2.4 (1.7, 3.0) |
| Involved/nondominant‡ | 2.4 (2.0, 2.9) | 2.6 (1.1, 4.1) |
Abbreviations: ACLR, individuals following unilateral anterior cruciate ligament reconstruction; MAT, modified agility T-test.
Values are mean (95% confidence interval).
Uninvolved side for those in the ACLR group and dominant side for those in the control group.
Involved side for those in the ACLR group and nondominant side for those in the control group.
TABLE 2.
Mean Absolute Scores on the Tests for Female Participants*
| Test | Control | ACLR |
|---|---|---|
| Vertical jump, cm | 38.6 (14.3, 16.2) | 35.9 (12.1, 16.1) |
| Broad jump, cm | 159.1 (58.2, 67.1) | 160.7 (58.3, 68.2) |
| Long shuttle, s | ||
| Uninvolved/dominant† | 9.1 (8.6, 9.6) | 9.4 (8.9, 9.8) |
| Involved/nondominant‡ | 9.1 (8.7, 9.5) | 9.3 (8.9, 9.7) |
| MAT, s | ||
| Uninvolved/dominant† | 10.5 (10.0, 11.0) | 10.8 (10.1, 11.5) |
| Involved/nondominant‡ | 10.4 (9.9, 10.9) | 10.8 (10.2, 11.5) |
| Pro shuttle, s | ||
| Uninvolved/dominant† | 5.8 (5.5, 6.0) | 5.7 (5.5, 5.9) |
| Involved/nondominant‡ | 5.6 (5.4, 5.8) | 5.7 (5.5, 5.9) |
| Single hop, cm | ||
| Uninvolved/dominant† | 169.7 (160.6, 178.8) | 172.6 (162.3, 182.8) |
| Involved/nondominant‡ | 168.1 (159.3, 176.9) | 157.6 (143.3, 171.9) |
| Triple hop, cm | ||
| Uninvolved/dominant† | 469.2 (444.0, 494.3) | 485.8 (444.9, 526.6) |
| Involved/nondominant‡ | 464.1 (440.8, 487.5) | 434.1 (387.2, 481.0) |
| Crossover hop, cm | ||
| Uninvolved/dominant† | 438.8 (418.5, 459.2) | 434.0 (399.5, 468.6) |
| Involved/nondominant‡ | 424.6 (400.1, 449.2) | 397.5 (354.0, 441.1) |
| Timed hop, s | ||
| Uninvolved/dominant† | 2.5 (2.4, 2.6) | 2.5 (2.3, 2.7) |
| Involved/nondominant‡ | 2.5 (2.3, 2.7) | 2.6 (2.4, 2.8) |
Abbreviations: ACLR, individuals following unilateral anterior cruciate ligament reconstruction; MAT, modified agility T-test.
Values are mean (95% confidence interval).
Uninvolved side for those in the ACLR group and dominant side for those in the control group.
Involved side for those in the ACLR group and nondominant side for those in the control group.
A separate 1-way multivariate analysis of variance was employed to investigate the group (ACLR versus control) differences in LSI measures for the 7 tests categorized as either modified double-limb performance tasks or single-limb performance tasks. There was a statistically significant main effect for group for the combined dependent variables (P = .006), with a large effect size observed (partial eta-squared, 0.458). Upon evaluation of the results for each of the LSI measures, a distinct group difference was noted for the single-limb performance tests, while the modified double-limb performance tasks were not sufficiently sensitive to detect limb deficits in individuals after ACL reconstruction. Specifically, the LSI for the long shuttle, modified agility T-test, and pro shuttle were not different between ACLR and control groups (P>.05), with very small effect sizes to differenti-ate between groups (partial eta-squared values lower than 0.05).
The LSI for single-limb tests indicated significant deficits in the ACLR group. The LSI for the single hop test was 92% in the ACLR group, compared to 100% in the control (P<.001) group, with a large effect size (partial eta-squared, 0.36). The triple hop LSI was significantly lower (P<.001) in the ACLR group (91%) compared to the control group (100%), with a large effect size (partial eta-squared, 0.31). Similar results were found for the crossover hop LSI (ACLR, 92%; control, 97%; P = .03), with a moderate effect size (partial eta-squared, 0.13). Finally, the LSI for the timed hop test was not different between groups (ACLR, 96%; control, 100%; P>.05), with a small to moderate effect to determine group differences (partial eta-squared, 0.06).
DISCUSSION
Asymmetries in limb performance during athletic tasks may be potential risk factors for lower extremity injury, particularly second ACL injury, and should be minimized prior to return to sport following ACL reconstruction.38 All stages of rehabilitation following ACL reconstruction should attempt to identify and minimize these limb asymmetries, not only with strength but with performance of athletic maneuvers. Side-to-side asymmetries are evident during drop landing4 and drop vertical jump34 in patients following ACL reconstruction for up to 2 years. Athletes who demonstrate side-to-side differences in biomechanical measures during a drop vertical jump are at increased risk of ACL injury, when compared to those with more symmetrical lower extremity biomechanics.12 A 5-year follow-up for a cohort with asymmetrical limb-to-limb biomechanics related to their initial injury also demonstrated a very high rate of secondary injury (44%).12
Following ACL reconstruction, patients frequently demonstrate asymmetrical force distribution in the lower extremities when performing high-level tasks such as landing5 and less dynamic tasks such as squatting.31 Neitzel et al27 demonstrated that, during squatting, individuals with ACL reconstruction were unable to balance side-to-side loading equal to that of controls until 12 to 15 months following surgery. The individuals with ACL reconstruction demonstrated side-to-side deficits between 33% and 48% at 1.5 to 4 months postsurgery and deficits between 21% and 28% at 6 to 7 months postsurgery. Asymmetrical limb loading is likely influenced by side-to-side imbalances in muscular strength, flexibility, and coordination, all of which may be important predictors of increased injury risk.1,12,15 Knapik et al13 demonstrated that side-to-side balance in strength and flexibility is important for the prevention of injuries, and that athletes are more injury prone when asymmetries are present. Baumhauer et al1 also found that individuals with muscle strength imbalances exhibited higher incidence of injury. Paterno and colleagues33 reported that, after an athlete is released to return to sport post ACL reconstruction, altered neuromuscular control of the hip and side-to-side asymmetry in knee joint recruitment during a dynamic landing task are predictors of a second ACL injury.37 Side-to-side asymmetries may increase injury risk for both limbs. Overreliance on the uninvolved limb can put greater stress and torques on that knee, while the involved limb may be at risk due to an inability of the musculature to effectively absorb the high forces associated with sporting activities. Considering the potential for side-to-side biomechanical differences to increase risk for subsequent ACL injury, identification of limb asymmetries and appropriate intervention are necessary prior to reintegration into sport competition.
While the standard T-test, pro shuttle, and long shuttle are basic criteria for the assessment of sports-related agility,10,38,49 they may not adequately measure side-to-side differences, due to the equalization of cutting directions in performance of the test. For this reason, we modified these agility measures to increase reliance on a single limb during the task. We hypothesized that this modification would identify the differences between an athlete’s involved and noninvolved sides better than the standard tests used to assess sports-related agility. Despite the modifications, we did not find asymmetries during these tasks. It may be that despite the modifications, the repeated bilateral nature of the tasks may allow the uninvolved limb to mask deficits of the involved lower extremity that were evident from the single-limb task testing. These data indicate that these types of modifications to bilateral agility tasks may not be adequate to identify involved limb deficits of the magnitude seen in this group of athletes.
Isolated single-limb performance tasks, such as the single-leg hop tests used in this study, may provide a critical component to field-based functional performance testing to identify persistent deficits in lower limb performance, including deficits in functional power, force attenuation, and postural stability. Specifically, single-leg hop tests, such as the single hop for distance, triple hop for distance, and crossover hop for distance, demonstrated potentially significant functional deficits in athletes released to full sport reintegration. The ability to generate and maintain isolated single-limb power is important during single-limb cutting maneuvers in sport. Also, improved ability to attenuate force on a single limb and the regeneration and redirection of motion may be relevant to reducing in injury risk in various single-limb actions in sports.17,22,32 Specifically, athletes who use a landing strategy characterized by decreased knee flexion may increase out-of-plane loads, increase ground reaction forces, and subject their limb to abrupt bone-to-bone stress at the knee.20,25 This may be evident in increased landing forces and could be a result of decreased thigh muscle strength.17 If tasks that isolate single-limb performance are sensitive to involved limb deficits, then these athletes may be targeted with neuromuscular training that increases hip and thigh muscle strength,21,26 improves postural stability,35 and increases single-limb force generation and attenuation.22,26 In addition, neuromuscular training can also reduce side-to-side deficits in single-limb force attenuation,22 which may provide the ultimate benefit to athletes who have had ACL reconstruction and desire return to sport.27
Following ACL reconstruction, the athletes who participated in this study demonstrated greater limb asymmetry on the performance of single-limb tasks compared to control participants. These findings are similar to those of our previous research in athletes following ACL reconstruction at the time of return to sport. We identified significant limb asymmetries in performance during single-limb hop tests and in knee joint mechanics during a bilateral landing-jump task.43,44 Munro and colleagues reported that the current hop tests provided reliable scores for use with subjects in a clinical or team sport environment. In addition, based on their normal subjects’ scores of greater than 90% LSI on all 4 hop tests, they recommend that a minimum limb symmetry value of greater than 90% be utilized during rehabilitation and conditioning rather than previously recommended 85%.21 The current results support the possibility that the 85% LSI criterion may not be sufficiently sensitive to capture residual deficits in athletes following ACLR.
Residual biomechanical and neuromuscular deficits may increase reinjury risk during early sports reintegration. However, we do not know the criterion performance values that would lead to increased risk of injury following ACL reconstruction. Although limb asymmetries were identified, 1 of the limitations of these types of tasks (single hop, triple hop, etc) is the inability to account for overall quality of movement (dynamic valgus, decreased knee flexion, altered trunk mechanics, etc) while performing these tasks. Clinic-based assessments that also evaluate quality of movement may be beneficial to include in assessment of athletes who wish to return to sport and should be further investigated to validate their utility for use in criterion-based return-to-sport guidelines.7,24,25,29,40
CONCLUSION
Single-limb tasks identified significant residual deficits in individuals who had been allowed full unrestricted return to sport following ACL reconstruction. Modification of bilateral limb tasks with tests focused to isolate single-limb performance did not provide enough sensitivity to identify these deficits. The development of sensitive test protocols that can be incorporated into bilateral, field-based movement patterns should be further investigated.
TABLE 3.
Mean Limb Symmetry Index Scores on the Tests for All Participants*
| Test | Control | ACLR |
|---|---|---|
| Long shuttle | 101 (98, 103) | 101 (99, 103) |
| MAT | 101 (98, 103) | 100 (97, 102) |
| Pro shuttle | 102 (99, 105) | 99 (96, 103) |
| Single leg hop | 100 (98, 103) | 92 (89, 95) |
| Triple hop | 100 (97, 103) | 91 (88, 94) |
| Crossover hop | 97 (94, 101) | 92 (89, 95) |
| Timed hop | 100 (96, 104) | 96 (91, 100) |
Abbreviations: ACLR, individuals following unilateral anterior cruciate ligament reconstruction; MAT, modified agility T-test.
Values are mean (95% confidence interval).
KEY POINTS.
FINDINGS
Single-limb tasks identified significant residual deficits in individuals allowed full unrestricted return to sport following ACL reconstruction. Modification of bilateral limb tasks with tests focused to isolate single-limb performance did not provide sufficient sensitivity to identify these deficits.
IMPLICATIONS
The unilateral functional deficits identified in patients following ACL reconstruction in the current study may place them at greater risk of reinjury.
CAUTION
There may be other combinations of single- and double-limb tasks that will help to further quantify functional deficits following ACL reconstruction. These measurements may not measure the quality of movement (eg, lower limb alignment) during these challenging tasks, which may also be predictive determinants of second injury following ACL reconstruction.
Acknowledgments
This study was approved by the Cincinnati Children’s Hospital Institutional Review Board.
The authors would like to acknowledge funding support from NFL Charities. The authors would also like to acknowledge funding support from National Institutes of Health/NIAMS grants R01-AR049735, R01-AR05563, and R01-AR056259. The authors acknowledge the Sports Medicine Biodynamics Team, especially Dr Mark Paterno, who worked together to make large data collection session possible. The authors would like to thank St Xavier High School, including Wellington Orthopaedics (Richelle Gwin, John Brehm, and Michael Gordon), for their invaluable support to complete this project.
References
- 1.Baumhauer JF, Alosa DM, Renstrom AF, Trevino S, Beynnon B. A prospective study of ankle injury risk factors. Am J Sports Med. 1995;23:564–570. doi: 10.1177/036354659502300508. [DOI] [PubMed] [Google Scholar]
- 2.Bush-Joseph CA, Hurwitz DE, Patel RR, et al. Dynamic function after anterior cruciate ligament reconstruction with autologous patellar tendon. Am J Sports Med. 2001;29:36–41. doi: 10.1177/03635465010290011101. [DOI] [PubMed] [Google Scholar]
- 3.Deacon A, Bennell K, Kiss ZS, Crossley K, Brukner P. Osteoarthritis of the knee in retired, elite Australian Rules footballers. Med J Aust. 1997;166:187–190. doi: 10.5694/j.1326-5377.1997.tb140072.x. [DOI] [PubMed] [Google Scholar]
- 4.Decker MJ, Torry MR, Noonan TJ, Riviere A, Sterett WI. Landing adaptations after ACL reconstruction. Med Sci Sports Exerc. 2002;34:1408–1413. doi: 10.1097/00005768-200209000-00002. http://dx.doi.org/10.1249/01.MSS.0000027627.82650.1F. [DOI] [PubMed] [Google Scholar]
- 5.Decker MJ, Torry MR, Noonan TJ, Sterett WI, Steadman JR. Gait retraining after anterior cruciate ligament reconstruction. Arch Phys Med Rehabil. 2004;85:848–856. doi: 10.1016/j.apmr.2003.07.014. [DOI] [PubMed] [Google Scholar]
- 6.Eitzen I, Moksnes H, Snyder-Mackler L, Risberg MA. A progressive 5-week exercise therapy program leads to significant improvement in knee function early after anterior cruciate ligament injury. J Orthop Sports Phys Ther. 2010;40:705–721. doi: 10.2519/jospt.2010.3345. http://dx.doi.org/10.2519/jospt.2010.3345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ekegren CL, Miller WC, Celebrini RG, Eng JJ, Macintyre DL. Reliability and validity of observational risk screening in evaluating dynamic knee valgus. J Orthop Sports Phys Ther. 2009;39:665–674. doi: 10.2519/jospt.2009.3004. http://dx.doi.org/10.2519/jospt.2009.3004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ford KR, Myer GD, Smith RL, Byrnes RN, Dopirak SE, Hewett TE. Use of an overhead goal alters vertical jump performance and biomechanics. J Strength Cond Res. 2005;19:394–399. doi: 10.1519/15834.1. http://dx.doi.org/10.1519/15834.1. [DOI] [PubMed] [Google Scholar]
- 9.Freedman KB, Glasgow MT, Glasgow SG, Bernstein J. Anterior cruciate ligament injury and reconstruction among university students. Clin Orthop Relat Res. 1998:208–212. doi: 10.1097/00003086-199811000-00028. [DOI] [PubMed] [Google Scholar]
- 10.Grobler LA, Schwellnus MP, Trichard C, Calder S, Noakes TD, Derman WE. Comparative effects of zopiclone and loprazolam on psychomotor and physical performance in active individuals. Clin J Sport Med. 2000;10:123–128. doi: 10.1097/00042752-200004000-00007. [DOI] [PubMed] [Google Scholar]
- 11.Hartigan EH, Axe MJ, Snyder-Mackler L. Time line for noncopers to pass return-to-sports criteria after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2010;40:141–154. doi: 10.2519/jospt.2010.3168. http://dx.doi.org/10.2519/jospt.2010.3168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005;33:492–501. doi: 10.1177/0363546504269591. http://dx.doi.org/10.1177/0363546504269591. [DOI] [PubMed] [Google Scholar]
- 13.Hickey KC, Quatman CE, Myer GD, Ford KR, Brosky JA, Hewett TE. Methodological report: dynamic field tests used in an NFL combine setting to identify lower-extremity functional asymmetries. J Strength Cond Res. 2009;23:2500–2506. doi: 10.1519/JSC.0b013e3181b1f77b. http://dx.doi.org/10.1519/JSC.0b013e3181b1f77b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Howe JG, Johnson RJ, Kaplan MJ, Fleming B, Jarvinen M. Anterior cruciate ligament reconstruction using quadriceps patellar tendon graft. Part I. Long-term followup. Am J Sports Med. 1991;19:447–457. doi: 10.1177/036354659101900505. [DOI] [PubMed] [Google Scholar]
- 15.Knapik JJ, Bauman CL, Jones BH, Harris JM, Vaughan L. Preseason strength and flexibility imbalances associated with athletic injuries in female collegiate athletes. Am J Sports Med. 1991;19:76–81. doi: 10.1177/036354659101900113. [DOI] [PubMed] [Google Scholar]
- 16.Kvist J. Rehabilitation following anterior cruciate ligament injury: current recommendations for sports participation. Sports Med. 2004;34:269–280. doi: 10.2165/00007256-200434040-00006. [DOI] [PubMed] [Google Scholar]
- 17.Lephart SM, Ferris CM, Riemann BL, Myers JB, Fu FH. Gender differences in strength and lower extremity kinematics during landing. Clin Orthop Relat Res. 2002:162–169. doi: 10.1097/00003086-200208000-00019. [DOI] [PubMed] [Google Scholar]
- 18.Mattacola CG, Perrin DH, Gansneder BM, Gieck JH, Saliba EN, McCue FC., 3rd Strength, functional outcome, and postural stability after anterior cruciate ligament reconstruction. J Athl Train. 2002;37:262–268. [PMC free article] [PubMed] [Google Scholar]
- 19.McHugh MP, Tyler TF, Browne MG, Gleim GW, Nicholas SJ. Electromyographic predictors of residual quadriceps muscle weakness after anterior cruciate ligament reconstruction. Am J Sports Med. 2002;30:334–339. doi: 10.1177/03635465020300030601. [DOI] [PubMed] [Google Scholar]
- 20.Meyer EG, Villwock MR, Haut RC. Osteochondral microdamage from valgus bending of the human knee. Clin Biomech (Bristol, Avon) 2009;24:577–582. doi: 10.1016/j.clinbiomech.2009.05.006. http://dx.doi.org/10.1016/j.clinbiomech.2009.05.006. [DOI] [PubMed] [Google Scholar]
- 21.Munro AG, Herrington LC. Between-session reliability of four hop tests and the agility T-test. J Strength Cond Res. doi: 10.1519/JSC.0b013e3181d83335. http://dx.doi.org/10.1519/JSC.0b013e3181d83335. [DOI] [PubMed]
- 22.Myer GD, Brent JL, Ford KR, Hewett TE. A pilot study to determine the effect of trunk and hip focused neuromuscular training on hip and knee isokinetic strength. Br J Sports Med. 2008;42:614–619. doi: 10.1136/bjsm.2007.046086. http://dx.doi.org/10.1136/bjsm.2007.046086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Myer GD, Ford KR, Brent JL, Hewett TE. The effects of plyometric vs. dynamic stabilization and balance training on power, balance, and landing force in female athletes. J Strength Cond Res. 2006;20:345–353. doi: 10.1519/R-17955.1. http://dx.doi.org/10.1519/R-17955.1. [DOI] [PubMed] [Google Scholar]
- 24.Myer GD, Ford KR, Hewett TE. Rationale and clinical techniques for anterior cruciate ligament injury prevention among female athletes. J Athl Train. 2004;39:352–364. [PMC free article] [PubMed] [Google Scholar]
- 25.Myer GD, Ford KR, Hewett TE. Tuck jump assessment for reducing anterior cruciate ligament injury risk. Athl Ther Today. 2008;13:39–44. doi: 10.1123/att.13.5.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Myer GD, Ford KR, Khoury J, Succop P, Hewett TE. Biomechanics laboratory-based prediction algorithm to identify female athletes with high knee loads that increase risk of ACL injury. Br J Sports Med. 45:245–252. doi: 10.1136/bjsm.2009.069351. http://dx.doi.org/10.1136/bjsm.2009.069351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Myer GD, Ford KR, Palumbo JP, Hewett TE. Neuromuscular training improves performance and lower-extremity biomechanics in female athletes. J Strength Cond Res. 2005;19:51–60. doi: 10.1519/13643.1. http://dx.doi.org/10.1519/13643.1. [DOI] [PubMed] [Google Scholar]
- 28.Myer GD, Paterno MV, Ford KR, Hewett TE. Neuromuscular training techniques to target deficits before return to sport after anterior cruciate ligament reconstruction. J Strength Cond Res. 2008;22:987–1014. doi: 10.1519/JSC.0b013e31816a86cd. http://dx.doi.org/10.1519/JSC.0b013e31816a86cd. [DOI] [PubMed] [Google Scholar]
- 29.Myer GD, Paterno MV, Ford KR, Quatman CE, Hewett TE. Rehabilitation after anterior cruciate ligament reconstruction: criteria-based progression through the return-to-sport phase. J Orthop Sports Phys Ther. 2006;36:385–402. doi: 10.2519/jospt.2006.2222. http://dx.doi.org/10.2519/jospt.2006.2222. [DOI] [PubMed] [Google Scholar]
- 30.Neeb TB, Aufdemkampe G, Wagener JH, Mastenbroek L. Assessing anterior cruciate ligament injuries: the association and differential value of questionnaires, clinical tests, and functional tests. J Orthop Sports Phys Ther. 1997;26:324–331. doi: 10.2519/jospt.1997.26.6.324. [DOI] [PubMed] [Google Scholar]
- 31.Neitzel JA, Kernozek TW, Davies GJ. Loading response following anterior cruciate ligament reconstruction during the parallel squat exercise. Clin Biomech (Bristol, Avon) 2002;17:551–554. doi: 10.1016/s0268-0033(02)00063-3. [DOI] [PubMed] [Google Scholar]
- 32.Noyes FR, McGinniss GH. Controversy about treatment of the knee with anterior cruciate laxity. Clin Orthop Relat Res. 1985:61–76. [PubMed] [Google Scholar]
- 33.Olsen OE, Myklebust G, Engebretsen L, Bahr R. Injury mechanisms for anterior cruciate ligament injuries in team handball: a systematic video analysis. Am J Sports Med. 2004;32:1002–1012. doi: 10.1177/0363546503261724. [DOI] [PubMed] [Google Scholar]
- 34.Paterno MV, Ford KR, Myer GD, Heyl R, Hewett TE. Biomechanical limb asymmetries in female athletes 2 years following ACL reconstruction. J Orthop Sports Phys Ther. 2005;35:A75. [Google Scholar]
- 35.Paterno MV, Ford KR, Myer GD, Heyl R, Hewett TE. Limb asymmetries in landing and jumping 2 years following anterior cruciate ligament reconstruction. Clin J Sport Med. 2007;17:258–262. doi: 10.1097/JSM.0b013e31804c77ea. http://dx.doi.org/10.1097/JSM.0b013e31804c77ea. [DOI] [PubMed] [Google Scholar]
- 36.Paterno MV, Myer GD, Ford KR, Hewett TE. Neuromuscular training improves single-limb stability in young female athletes. J Orthop Sports Phys Ther. 2004;34:305–316. doi: 10.2519/jospt.2004.34.6.305. [DOI] [PubMed] [Google Scholar]
- 37.Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 38:1968–1978. doi: 10.1177/0363546510376053. http://dx.doi.org/10.1177/0363546510376053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pauole KK. The Physical Performance T-Test as a Measure of Speed, Power, and Agility in Females. Long Beach, CA: California State University; 1996. [Google Scholar]
- 39.Petschnig R, Baron R, Albrecht M. The relationship between isokinetic quadriceps strength test and hop tests for distance and one-legged vertical jump test following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 1998;28:23–31. doi: 10.2519/jospt.1998.28.1.23. [DOI] [PubMed] [Google Scholar]
- 40.Powers CM. The influence of abnormal hip mechanics on knee injury: a biomechanical perspective. J Orthop Sports Phys Ther. 2010;40:42–51. doi: 10.2519/jospt.2010.3337. http://dx.doi.org/10.2519/jospt.2010.3337. [DOI] [PubMed] [Google Scholar]
- 41.Risberg MA, Holm I, Tjomsland O, Ljunggren E, Ekeland A. Prospective study of changes in impairments and disabilities after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 1999;29:400–412. doi: 10.2519/jospt.1999.29.7.400. [DOI] [PubMed] [Google Scholar]
- 42.Ross MD, Irrgang JJ, Denegar CR, McCloy CM, Unangst ET. The relationship between participation restrictions and selected clinical measures following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2002;10:10–19. doi: 10.1007/s001670100238. http://dx.doi.org/10.1007/s001670100238. [DOI] [PubMed] [Google Scholar]
- 43.Schmitt LC, Paterno MV, Ford KR, Myer GD, Hewett TE. Altered knee mechanics during ladning at the time of return to sport following ACL reconstruction: effects of quadriceps strength asymmetry [abstract] J Orthop Sports Phys Ther. 2010;2010:A42. [Google Scholar]
- 44.Schmitt LC, Paterno MV, Hewett TE. Functional performance at the time of return to sport following ACL reconstruction: the impact of quadriceps strength asymmetry [abstract] J Orthop Sports Phys Ther. 2009;39:A103. doi: 10.2519/jospt.2012.4194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Shelbourne KD, Nitz P. Accelerated rehabilitation after anterior cruciate ligament reconstruction. Am J Sports Med. 1990;18:292–299. doi: 10.1177/036354659001800313. [DOI] [PubMed] [Google Scholar]
- 46.Shelbourne KD, Nitz P. Accelerated rehabilitation after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 1992;15:256–264. doi: 10.2519/jospt.1992.15.6.256. [DOI] [PubMed] [Google Scholar]
- 47.Shen C, Jiang SD, Jiang LS, Dai LY. Bioabsorbable versus metallic interference screw fixation in anterior cruciate ligament reconstruction: a meta-analysis of randomized controlled trials. Arthroscopy. 26:705–713. doi: 10.1016/j.arthro.2009.12.011. http://dx.doi.org/10.1016/j.arthro.2009.12.011. [DOI] [PubMed] [Google Scholar]
- 48.Stockbrugger BA, Haennel RG. Validity and reliability of a medicine ball explosive power test. J Strength Cond Res. 2001;15:431–438. [PubMed] [Google Scholar]
- 49.Vanderford ML, Meyers MC, Skelly WA, Stewart CC, Hamilton KL. Physiological and sport-specific skill response of olympic youth soccer athletes. J Strength Cond Res. 2004;18:334–342. doi: 10.1519/R-11922.1. http://dx.doi.org/10.1519/R-11922.1. [DOI] [PubMed] [Google Scholar]
- 50.Wilk KE, Andrews JR. Current concepts in the treatment of anterior cruciate ligament disruption. J Orthop Sports Phys Ther. 1992;15:279–293. doi: 10.2519/jospt.1992.15.6.279. [DOI] [PubMed] [Google Scholar]
- 51.Wilk KE, Reinold MM, Hooks TR. Recent advances in the rehabilitation of isolated and combined anterior cruciate ligament injuries. Orthop Clin North Am. 2003;34:107–137. doi: 10.1016/s0030-5898(02)00064-0. [DOI] [PubMed] [Google Scholar]
- 52.Wilk KE, Romaniello WT, Soscia SM, Arrigo CA, Andrews JR. The relationship between subjective knee scores, isokinetic testing, and functional testing in the ACL-reconstructed knee. J Orthop Sports Phys Ther. 1994;20:60–73. doi: 10.2519/jospt.1994.20.2.60. [DOI] [PubMed] [Google Scholar]
- 53.Wojtys EM, Huston LJ. Longitudinal effects of anterior cruciate ligament injury and patellar tendon autograft reconstruction on neuromuscular performance. Am J Sports Med. 2000;28:336–344. doi: 10.1177/03635465000280030901. [DOI] [PubMed] [Google Scholar]