Abstract
Objectives
Randomized trials found physical activity (PA) effective in decreasing depressive symptoms. Few studies included Black participants. The purpose of this systematic literature review was to determine the effects of PA on depressive symptoms in Black adults.
Methods
Articles were abstracted by conducting a computer and hand search of eligible studies.
Results
Eight of 13 studies found a significant inverse relationship between PA and depressive symptoms in Black adults. Sources for the heterogeneity were explored.
Conclusion
Future studies should include representative samples of Black adults, incorporate a theory which considers multiple levels of influence, account for genetic factors in the etiology of depressive symptoms, include individuals diagnosed with depression and with health conditions which may increase the risk of depressive symptoms, account for intra-group ethnic heterogeneity, measure and differentiate between social support and social network, consider aspects of the physical environment and use standardized measurements of PA.
Keywords: exercise, depression, African American, systematic review, Stokols' Social Ecology of Health Promotion
INTRODUCTION
Randomized trials which followed CONSORT reporting guidelines (Moher D. Schulz KF. Altman DG. CONSORT GROUP [Consolidated Standards of Reporting Trials], 2001) have found physical activity effective in decreasing depressive symptoms in individuals with clinical depression (Brenes et al., 2007; Dunn, Trivedi, Kampert, Clark, & Chambliss, 2005; Knubben et al., 2007; Mather et al., 2002; Singh, Clements, & Singh, 2001) and in healthy community samples (Baker et al., 2007; Penninx et al., 2002). Many of these studies did not report race (Baker et al., 2007; Knubben et al., 2007; Mather et al., 2002; Singh et al., 2001), possibly because they were not conducted in the U.S. When race was reported, there was no specification of groups classified as "non-White" (Brenes et al., 2007; Penninx et al., 2002) or the small numbers of ethnic minorities precluded analyses of race/ethnicity effects (Dunn et al., 2005). Thus, it is not surprising that a report of the U.S. Surgeon General concluded ethnic minorities are underrepresented in mental health research (U.S. Department of Health & Human Services [USDHHS], 1999).
Physical activity is hypothesized to decrease depressive symptoms through biological, psychological and social mechanisms (Brosse, Sheets, Lett, & Blumenthal, 2002; Craft & Perna, 2004; Dishman et al., 2006; Fox, 1999; North, McCullagh, & Tran, 1990; Paluska & Schwenk, 2000; Scully, 1998; N. A. Singh & Fiatarone Singh, 2000; Yeung, 1996). Since the mechanism of action is unknown, physical activity may not exert antidepressant effects in everyone. The purpose of this systematic literature review was to determine the effects of physical activity on depressive symptoms in Black adults.
METHODS
Research literature was abstracted by conducting an on-line computer search of MEDLINE using OVID software, ISI Web of Science, and PubMed. Inclusion criteria included race-specific results in quantitative studies of the relationship between physical activity and depressive symptoms. No time restriction was placed on publication date. Healthy adults and those with clinical depression were included, such as Major or Minor Depressive Disorder and dysthymia. Individuals with mood disorders in addition to clinical depression were excluded. Studies focused on non-diagnostic depressive symptoms were included. All types of physical activity were included regardless of dosage. Quantitative studies published in peer-reviewed journals through August 27, 2009 were located using the following key words in OVID (includes title, original title, abstract, name of substance word, and subject heading word), topics in ISI Web of Science (all citation databases, including Science, Social Sciences, and Arts & Humanities), and in PubMed (limiting search to humans); exercise or physical activity and depress*, dysthmi*, or seasonal affective disorder. In OVID, the subheading African Continental Ancestry Group was included in the search, while Black or African American was in ISI Web of Science and PubMed. Asterisks were used to include all words with a certain term. A further hand search of reference lists of eligible studies was conducted.
RESULTS
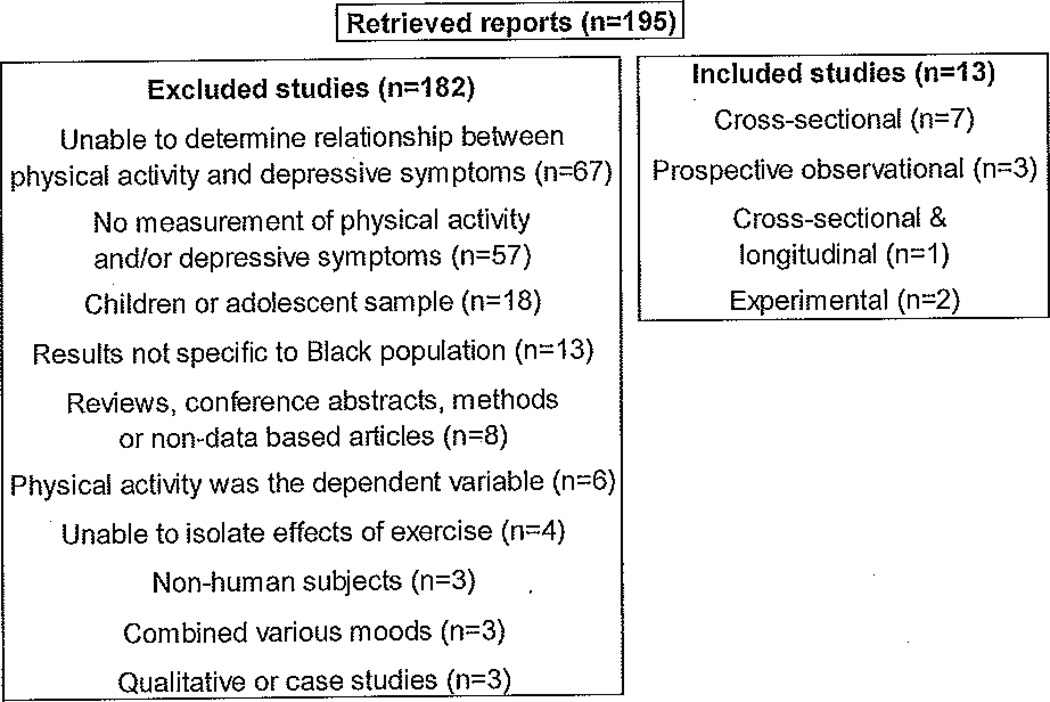
Figure 1 summarizes the process of inclusion of the studies identified for review and analysis. Of the 195 non-duplicating articles found, 182 were excluded for a variety of reasons. Several were not quantitative studies in peer-review journals. Many were excluded due to unrelated sample such as nonhuman subjects or children. Often studies were excluded due to methodological issues such as combining depression with other mood disorders, or measuring concepts similar to but not identical to physical activity, such as physical health or mobility. Since the purpose of this review was to determine the effects of physical activity on depressive symptoms, depressive symptoms had to be the dependent variable. Finally, studies were excluded if the relationship between physical activity and depressive symptoms was undeterminable, such as when physical activity and depressive symptoms were both covariates in a regression with a different outcome.
Figure 1.
Process of Inclusion for Review.
Studies reviewed (n=13) were assessed and listed in Table 1, which summarizes the samples, designs, methods and key findings. Eight of the studies found a significant inverse relationship between physical activity and depressive symptoms (Farmer et al., 1988; Knox et al., 2006; Malebo, van Eeden, & Wissing, 2007; Orr, James, Garry, & Newton, 2006; Patil, Johnson, & Lichtenberg, 2008; Siegel, Yancey, & McCarthy, 2000; Wilbur et al., 2009; Wise, Adams-Campbell, Palmer, & Rosenberg, 2006). The studies reviewed comprised 7 cross-sectional (Artinian, Washington, Flack, Hockman, & Jen, 2006; Bopp, Wilcox, Oberrecht, Kammermann, & McElmurray, 2004; Farmer et al., 1988; Malebo et al., 2007; Orr et al., 2006; Patil et al., 2008; Siegel et al., 2000;), 3 prospective observational (Knox et al., 2006; Nelson et al., 2008; Walker et al., 2004), 1 combination cross-sectional and longitudinal (Wise et al., 2006), and 2 experimental (Izquierdo-Porrera, Powell, Reiner, & Fontaine, 2002; Wilbur et al., 2009). Ten of the 13 studies used convenience sampling. Most of the studies had majority female samples; 10 were more than 70% female and 8 were 100% female. Only 1 study from 1988 used a nationally representative sample (Farmer et al., 1988). About half of the studies specified exclusion criteria based on health and/or capacity to participate in physical activity, such as the presence of disabilities (Farmer et al., 1988; Izquierdo-Porrera et al., 2002; Knox et al., 2006; Nelson et al., 2008; Walker et al., 2004; Wilbur et al., 2009). One study excluded those with mental illness (Artinian et al., 2006) while another excluded those who reported physician-diagnosed depression (Wise et al., 2006). All of the studies used an established measure of depressive symptoms. Ten studies measured depressive symptoms with the Center for Epidemiologic Studies Depression Scale (CESD), a self-report scale developed for epidemiologic studies at the National Institute of Mental Health (Radloff, 1977). Each study measured physical activity differently.
Table 1.
Summary of Studies of Physical Activity and Depressive Symptoms in Black Adults.
| Authors | n | Subject Selection |
Gender | Age | Design | Physical Activity Measurement |
Psychological Instrument |
Key Findings on PA & depressive symptoms variables |
|---|---|---|---|---|---|---|---|---|
| Artinian et al. (2006) | 245 | Convenience | female | 61 years (SD, 12.7 years) |
Cross- sectional |
Assessment of PA was determined by two one-item measures |
20 item CESD, scored differently than original |
Non-significant relationship between depressive symptoms and # of days within last 30 of moderate- intensity activity: F1,241=3.13 (p>.05) |
| Bopp et al. (2004) | 42 | Convenience | female | 70.59 ±9.21 years |
Cross- sectional |
PA Scale for the Elderly, only asked about strength training participation (yes/no and hours/week) |
5 item version of the Geriatric Depression Scale, with one of the items removed to improve internal consistency |
Non-significant correlation between strength training participation and depression |
| Farmer et al. (1988) | 155 | Stratified random sampling |
57% female |
25–77 | Cross- sectional |
Current recreational & nonrecreational PA |
20 item CESD | Adjusted odds ratio for depressive symptoms was 16.5 in men with little or no PA in recreation, and 19.2 in women with little or no activity apart from recreation |
| Izquierdo-Porrera et al. (2002) | 46 out of 48 (96%) |
Convenience | 83% female |
29–83 | Experimental | Attendance in PA church program |
20 item CESD | Attendance in PA intervention was not correlated with depressive symptoms (r=.16, p>.05) |
| Knox et al. (2006) | 2,637 | Random & convenience |
56% female |
33–45 | Prospective observational |
METS from strenuous PA to daily activities such as cleaning & gardening over previous year |
20 item CESD | The adjusted predictor of # of depressive episodes was B=− 28.40, SE=7.61, p=.0002 for PA. |
| Malebo, et al. (2007) | 293 | Convenience | 52% male | 20–35 | Cross- sectional |
PA Index measured 5 categories of activity: intensity, duration, frequency, summer participation, and winter participation |
General Health Questionnaire depression subscale |
Fewer depressive symptoms in sports participants compared to non- sport participants (t=−1.84, p=.07, small effect size) |
| Nelson et al. (2008) | 186 | Random | female | 35–47 at baseline, followed for 8 years |
Prospective observational |
Kilocalories of leisure-time PA per week were calculated from the Paffenbarger PA Questionnaire and categorized into the top third (≥ 1450 kcal/wk), middle third (< 1450 to 644 kcal/wk), and bottom third (< 644 kcal/wk) of reported current activity |
20 item CESD | PA at any level was not related to depressive symptoms among African American women (top third OR = 0.04, CI = − 1.87, 1.94; middle- third OR = 0.05, CI = −1.53, 1.63. The lowest PA tertile was used as the reference group.) |
| Orr et al. (2006) | 922 | Convenience | pregnant women |
18–20+ | Cross- sectional |
PA for fun & fitness before and during pregnancy |
20 item CESD | Proportionately more women with lower levels of depressive symptoms engaged in PA during pregnancy (65.9%) than those with higher levels of depressive symptoms (51.8%) |
| Patil et al. (2008) | 74 | Convenience | 81.1% female |
60–95 | Cross- sectional |
Estimated number of times weekly of PA (intentional cardiovascular workout) for at least 20 consecutive minutes |
15 item Geriatric Depression Scale |
Correlation between PA and depressive symptoms was −.29, p<01 (two-tailed) |
| Siegel et al. (2000) | 378 | Convenience | female | adults | Cross- sectional |
Leisure-time PA operationalized as “no PA”, “only light PA/weekly,” “vigorous PA at least 20 min once or twice weekly,” and “vigorous PA at least 20 min three or more times weekly” |
20 item CESD | PA predicted depressive symptoms (B = − 0.15, p<.01), holding education, income, marital status, and pounds overweight constant |
| Walker et al. (2004) | 100 | Convenience | post- partum |
22.40 ±3.75 |
Prospective observational |
7-day PA recall, kcal/kg/d |
20 item CESD |
Non-significant correlation between depressive symptoms and PA (r = −.078) |
| Wilbur et al. (2009) | 278 | Convenience | female | 48.5 (SD 6.0) |
Quasi- experimental |
Adherence to walking frequency calculated as the percentage of the prescribed minimum of 68 walks completed during the adoption phase of the intervention |
20 item CESD | Higher walking adherence was predictive of lower depressive symptoms at 24 weeks (B = −.023, p = .036) |
| Wise et al. (2006) | 35,224 | Convenience | female | 21–69 | Cross- sectional and prospective observational |
Vigorous PA during high school; average # of hours spent each week during the past year in walking for PA & vigorous PA |
20 item CESD | Compared with women who were never active, the adjusted OR of depressive symptoms for women who were active in high school but inactive in adulthood, inactive in high school but active and adulthood, and always active was 0.90, 0.83, and 0.76 respectively. Compared with women who reported no vigorous PA, the adjusted OR of depressive symptoms for women reporting <1, 1, 2, 3–4, and 7 hr or more/week was .89, .85, .74, .72, and .75 respectively (p<.001). |
PA=physical activity
Although a broad range of ages were sampled, 18–90 years, no clear determination can be made regarding age and the relationship between physical activity and depressive symptoms in Black adults. Studies which included adults of all ages usually found a significant relationship between physical activity and depressive symptoms (Farmer et al., 1988; Siegel et al., 2000; Wise et al., 2006). However, in studies including specific age groups, physical activity was sometimes related to depressive symptoms in young adults (Malebo et al., 2007; Orr et al., 2006), but not always (Walker et al., 2004), often related in middle age (Knox et al., 2006; Wilbur et al., 2009) and middle to old age (Nelson et al., 2008), and occasionally related in older adults (Patil et al., 2008), but usually not (Artinian et al., 2006; Bopp et al., 2004).
The relationship between body mass index (BMI), physical activity and depressive symptoms is not clear. Wise et al. (2006) stratified analyses by BMI (<30 vs. 30+) and found the odds of depressive symptoms in Black women who engaged in vigorous physical activity five hours or more per week versus none were slightly stronger in nonobese than obese women, but the associations were not statistically different. Wise et al. also found walking for exercise had a weak inverse relationship with depressive symptoms among obese women, but no association was found among nonobese women.
DISCUSSION
No firm conclusion can be drawn concerning the effects of physical activity on depressive symptoms in Black adults. There are many possible sources for heterogeneity demonstrated in this literature. Convenience sampling often resulted in mostly female samples. Only three studies specifically addressed the effects of physical activity on depressive symptoms. Future studies designed to examine the effects of physical activity on depressive symptoms in Black adults should be based on representative samples, with a particular focus on adequate numbers of men.
Most of the reviewed studies measured depressive symptoms with the CESD, a widely recognized tool with established reliability and validity. A majority of the studies used the original 20 item questionnaire (Artinian et al., 2006; Farmer et al., 1988; Knox et al., 2006; Nelson et al., 2008; Orr et al., 2006; Siegel et al., 2000; Walker et al., 2004; Wilbur et al., 2009; Wise et al., 2006) with Cronbach alphas ranging from .71 to .93 (Artinian et al., 2006; Nelson et al., 2008; Siegel et al., 2000; Walker et al., 2004; Wilbur et al., 2009). Another measurement of depressive symptoms in the reviewed articles was the Geriatric Depression Scale (Bopp et al., 2004; Patil et al., 2008). Although both reported good psychometrics for the Geriatric Depression Scale in previous studies, neither study used the original version (Bopp et al., 2004; Patil et al., 2008), Only one study reported the Cronbach alpha for their study, which was quite low (.41 to .49) (Bopp et al., 2004). Future studies should continue to use an established measure of depressive symptoms and continue to report psychometrics with subsequent studies.
In contrast to the established measurement of depressive symptoms, each of the reviewed studies measured physical activity differently, which may account for the conflicting results. Intensity refers to how much work is being performed or the magnitude of the effort required to engage in physical activity (Centers for Disease Control and Prevention [CDC], 2009). Reviewed articles measured intensity as moderate (Artinian et al., 2006), vigorous (Siegel et al., 2000; Wise et al., 2006) and through energy expenditure such as metabolic equivalents (Knox et al., 2006) and kilocalories (Nelson et al., 2008; Walker et al., 2004). Frequency is typically measured as the number of times an activity is performed (CDC, 2009). Reviewed articles measured frequency as number of times weekly (Patil et al., 2008; Siegel et al., 2000) and number of days in last 30 days (Artinian et al., 2006). One study measured the attendance rate at a structured program by dividing the number of sessions attended by the total possible number of sessions offered (Izquierdo-Porrera et al., 2002). Another study calculated adherence to walking frequency as the percentage of the prescribed minimum of 68 walks completed during the adoption phase of the intervention (Wilbur et al., 2009). Duration is commonly measured as the length of time in which an activity is performed (CDC, 2009). Reviewed articles measured duration by at least 20 minutes (Patil et al., 2008; Siegel et al., 2000), at least 30 minutes per day (Artinian et al., 2006), hours per week (Bopp et al., 2004) or average number of hours per week (Wise et al., 2006). Various types of physical activity were measured, such as leisure-time physical activity (Nelson et al., 2008; Siegel et al., 2000), fun and fitness (Orr et al., 2006), strength training (Bopp et al., 2004), intentional cardiovascular workout (Patil et al., 2008), recreational and nonrecreational (Farmer et al., 1988), walking (Wilbur et al., 2009; Wise et al., 2006) and daily activities such as cleaning and gardening (Knox et al., 2006). Recall varied from seven days (Walker et al., 2004), last 30 days (Artinian et al., 2006) or over previous year (Knox et al., 2006; Wise et al., 2006). Only three studies measured physical activity with a questionnaire which demonstrated reliability and validity in previous studies (Bopp et al., 2004; Malebo et al., 2007; Nelson et al., 2008). All three used a different questionnaire and only one reported reliability and validity of the physical activity measurement in their results section (Malebo et al., 2007). Only one study reported validating self-report data (Wilbur et al., 2009). Specifically, heart rate monitors and an automated telephone response system was reported (Wilbur et al., 2009). Finally, only one study accounted for seasonal physical activity, specifically summer and winter participation (Malebo et al., 2007). Future studies should use physical activity measurements which have demonstrated reliability and validity in previous studies, continue to report psychometrics in subsequent studies, and validate self-report measures. Established physical activity measurements which include intensity, frequency, duration and type should continue to be utilized. Although this review did not support a recommendation regarding period of recall, recommendations have been made for relatively short reporting intervals (no longer than three months), with the possible exception of advanced age where long term memory may be better preserved than recent recollections of activity patterns (Shepard, 2003).
Only one of the studies in this review reported guidance by a theory or conceptual model (Wilbur et al., 2009). Since physical activity is hypothesized to decrease depressive symptoms through biological, psychological and social mechanisms (Brosse et al., 2002; Craft & Perna, 2004; Dishman et al., 2006; Fox, 1999; North et al., 1990; Paluska & Schwenk, 2000; Scully, 1998; Singh & Fiatarone Singh, 2000; Yeung, 1996), theories or models that take into consideration multiple levels of influence are recommended to guide the investigation of physical activity and depressive symptoms in Black adults. Ecological models such as Stokols' (1992) Social Ecology of Health Promotion can address factors within the individual as well as environmental factors and guides the subsequent recommendations.
Social Ecology of Health Promotion
The Social Ecology of Health Promotion Model focuses on personal and environmental factors that play either an etiologic or moderating role in human health (Stokols, 1992).
Personal factors
Personal factors were further defined as biogenetic, psychological, and behavioral (Stokols, 1992). Examples of biogenetic factors include genetics, sex, age and disabling injuries. Although Stokols did not include BMI, such a variable would fit in this category as well.
A typical factor within individuals which may influence the impact of physical activity on depressive symptoms is genetics. For example, rodent studies have found physical activity enhances the expression of protein brain derived neurotrophic factor (BDNF) (Russo-Neustadt & Chen, 2005; Zheng et al., 2006), which is capable of producing an antidepressant response itself and may enhance the function of monoamine systems disordered in clinical depression (Russo-Neustadt & Chen, 2005). In humans, physical activity has been shown to increase serum BDNF in healthy young adults (Ferris, Williams, & Shen, 2007; Tang, Chu, Hui, Helmeste, & Law, 2008; Winter et al., 2007) and middle-age adults with multiple sclerosis (Castellano & White, 2008; Gold et al., 2003; Schulz et al., 2004). However, none of these studies reported depressive symptoms. It is unclear if an increase in serum BDNF resulting from physical activity leads to a decrease in depressive symptoms. Just as physical activity changes the expression of BDNF, physical activity could theoretically change the expression of certain genes associated with depressive symptoms, such as dopaminergic candidate genes and serotonin transporter genes, which could potentially result in a decrease in depressive symptoms. None of the reviewed studies accounted for genetic factors. Future studies should account for genetic factors in the relationship between physical activity and depressive symptoms by including genetic tests such as family history, assaying the biochemistry, chromosomal analysis and/or measuring mutations at the DNA level (CDC, 2007).
The association between physical activity and depressive symptoms may be confounded by type of physical activity, sex, age, BMI and disability. For Black women, the inverse relationship with depressive symptoms was larger for physical activity apart from recreation, while for Black men the relationship with depressive symptoms was larger for physical activity in recreation after adjustment for several confounders (Farmer et al., 1988). In addition, although adults aged 18–90 years were sampled, no clear determination can be made regarding age and the relationship between physical activity and depressive symptoms in Black adults. Although walking for exercise had a weak inverse association with depressive symptoms among obese but not obese women in one study (Wise et al., 2006), the relationship between BMI, physical activity and depressive symptoms remains unclear in Black women and not known in Black men. Finally, the effectiveness of physical activity in decreasing depressive symptoms in Black adults with other illnesses or disability which results from those illnesses has not been well studied. This suggests the need to investigate the effects of different types of physical activity, stratify results by sex, age (perhaps by young, middle and older adults) and BMI, and include Black adults with disabilities that may increase the risk of depressive symptoms.
Psychological factors have been hypothesized as part of the mechanism by which physical activity decreases depressive symptoms (Brosse et al., 2002; Craft & Perna, 2004; Fox, 1999; North et al., 1990; Paluska & Schwenk, 2000; Scully, 1998; Singh & Fiatarone Singh, 2000; Yeung, 1996). However, of the three studies which specifically addressed the possible effects of physical activity on depressive symptoms in Black adults (Farmer et al., 1988; Wilbur et al., 2009; Wise et al., 2006), none included psychological factors. Future studies should include psychological variables such as self-efficacy.
Environmental factors
Environmental factors were delineated as sociocultural and geographic (Stokols, 1992). Examples of sociocultural factors that may confound the relationship between physical activity and depressive symptoms include socioeconomic status of individuals and groups, social support and culture (Stokols, 1992). Physical activity remained predictive of depressive symptoms in Black U.S. adults, even after controlling for education, employment status, occupation and income (Farmer et al., 1988; Wilbur et al., 2009; Wise et al., 2006).
Most reviewed studies have focused solely on factors within individuals with little consideration for the social context. Mental illness and less severe mental health problems should be understood in a social context since social environments can increase or decrease the likelihood of exposure to certain types of stressors (USDHHS, 1999). For example, the positive effects of social support on mental health have been established (Blazer, 2005; Bruce, 2002; Harris, 2001; Jorm, 1995; Kawachi & Berkman, 2001; Lin & Peek, 1999; Lépine & Bouchez, 1998; Paykel, 1994; Vilhjalmsson, 1993). Future studies examining the effects of physical activity on depressive symptoms in Black U.S. adults should control for social support and examine the possible interaction between physical activity and social support on depressive symptoms. Whenever possible, general measures of support that have meaning across a variety of situations should be combined with measures that capture the unique dynamic of support related to physical activity, depressive symptoms, and the combination of physical activity and depressive symptoms (Depner, Wethington, & Ingersoll-Dayton, 1984; O'Reilly, 1988). In addition, it is essential to distinguish between social network and social support (Bowling, 1997; Cohen, 1988; House & Kahn, 1985; Hutchinson, 1999; Israel, 1982; Israel & Rounds, 1987; O'Reilly, 1988; Tardy, 1985). Social network is the existence or quantity and structure of social relationships, while social support is the functional content of relationships (House & Kahn, 1985).
A Surgeon General's expert panel concluded that the cultures that patients come from shape their mental health and affect the types of mental health services they use (USDHHS, 2001). Reviewed studies have not addressed cultural characteristics or intra-group ethnic heterogeneity (House & Williams, 2000; D. R. Williams, Yu, Jackson, & Anderson, 1997; D. R. Williams & Jackson, 2000). For example, approximately 2.4 million or 8% of U.S. Blacks are foreign born (U.S. Census Bureau, 2005). Sixty percent of foreign born Blacks living in the U.S. are from the Caribbean (McKinnon & Bennett, 2005, August). The 12-month rate of Major Depressive Disorder was 10.9% for Black U.S. adults of Caribbean ancestry born in the U.S., compared to 2% for Black U.S. adults born in the Caribbean (Williams et al., 2007). Future studies should account for intra-group ethnic heterogeneity, partly by taking into account different cultures within the same ethnic group and levels of acculturation for immigrants.
Examples of geographic factors which may confound the relationship between physical activity and depressive symptoms include regional differences and neighborhood characteristics. In the only reviewed study which addressed region of country, vigorous physical activity was most common in the West and least common in the South in the United States (Wise et al., 2006). Region of country is also an important component of seasonal affective disorder. Seasonal affective disorder is a type of depression which may be caused by latitude, climate, social and cultural influences and genetic factors (Mersch, Middendorp, Bouhuys, Beersma, & van den Hoofdakker, 1999). Latitude values indicate the angular distance between the Equator and points north or south of it on the surface of the Earth (Nationalatlas.gov, 2007). For example, significantly high correlations have been found between prevalence and latitude of seasonal affective disorder in North America; the higher the latitude, the higher the prevalence (Mersch et al., 1999). In addition, the climate, such as winter months, may predispose individuals to depressive symptoms (Mersch et al., 1999). None of the reviewed studies addressed seasonal affective disorder, but it is reasonable to design future studies to include such risk factors.
Another example of the impact of geographic factors is neighborhood characteristics. In the only reviewed study which addressed neighborhood characteristics, adherence to walking remained predictive of depressive symptoms while controlling for neighborhood deterioration and crime (Wilbur et al., 2009). Additional neighborhood characteristics which affect physical activity and depressive symptoms include animals, traffic, noise, trash and litter, night lighting, sidewalk conditions, public walking tracks and trails, and availability of public transportation (Gallagher et al., 2010; Strawbridge, Deleger, Roberts, & Kaplan, 2002). Future studies should include aspects of the physical environment, such as the neighborhood characteristics.
There are limitations of this systematic review. While physical activity and other forms of antidepressant treatments may offer some protection against stress, in some cases alleviating the cause of the stress may be a more effective and ethical solution than offering different treatment or coping methods. Another limitation is that theses, proceedings and textbooks were not reviewed. Nor were researchers and sponsoring organizations contacted for unpublished results. Thus, this systematic review is at risk of overestimating the effect of physical activity on depressive symptoms (Jadad, Moher, & Klassen, 1998). However, the results of this review found only about half of the eligible studies resulted in a significant inverse relationship between physical activity and depressive symptoms in Black adults, suggesting that publication bias, or the favoring of positive results, was not an issue. There is little empirical evidence to recommend blinding reviewers to the study authors, institutions, sponsorship, publication year and journal or study results (Jadad et al., 1998). Hence, the reviewer was not blinded. Data combination for meta-analysis was inappropriate (Moher, Jadad, & Kiassen, 1998) due to differences in how physical activity and depressive symptoms were measured, as well as varied statistical measures, including t-tests, one way analysis of variance, correlation, odds ratio, regression and percentages.
Strengths of this review include a focused clinical question developed a priori, clear and concise selection criteria, and assessment of quality (Klassen, Jadad, & Moher, 1998). The quality of the studies (Jadad et al., 1998) was assessed by focusing on methodological aspects including design, generalizability, various measurements of physical activity and depressive symptoms, and theoretical guidance, as well as the inclusion of potential confounders such as depression diagnosis and treatment, genetic factors, intra-group ethnic heterogeneity, the social context and region of the country and neighborhood characteristics.
CONCLUSION
Although randomized trials have found physical activity effective in decreasing depressive symptoms, few studies included sufficient numbers of Black participants to extrapolate this conclusion to Black adults. This systematic literature review has shown varying results on the effects of physical activity on depressive symptoms in Black adults. Heterogeneity may account for the divergent results. Future studies should include representative samples of Black women and men, use established measures of depressive symptoms and physical activity, report psychometrics and validate self-report measures. Physical activity measures should include intensity, frequency, duration and type. Studies should incorporate a theory which considers multiple levels of influence, such as Stokols' Social Ecology of Health Promotion which considers personal and environmental factors. Relevant personal factors include genetics, sex, age, disability, BMI and psychological factors. Appropriate environmental factors include socioeconomic status of individuals and groups, social support and network, intra-group ethnic heterogeneity, region of country, latitude, climate and neighborhood characteristics.
ACKNOWLEDGEMENT
The work of this study was supported by an Individual National Research Service Award, Grant # 1F31NR010669-01; the Michigan Institute for Clinical and Health Research, Clinical and Translational Service Award, Grant # UL1RR024986, and the Women's Health Disparities Interdisciplinary Training Grant, Grant # 5T32NR007965-05.
Contributor Information
Elisa R. Torres, School of Nursing, University of Iowa
Carolyn M. Sampselle, School of Nursing, University of Michigan
Kimberlee A. Gretebeck, School of Nursing, University of Michigan
David L. Ronis, School of Nursing, University of Michigan, Ann Arbor, VA
Harold W. Neighbors, School of Public Health, University of Michigan
REFERENCES
- Artinian NT, Washington OG, Flack JM, Hockman EM, Jen KC. Depression, stress, and blood pressure in urban African-American women. Progress in Cardiovascular Nursing. 2006;21(2):68–75. doi: 10.1111/j.0889-7204.2006.04787.x. [DOI] [PubMed] [Google Scholar]
- Baker MK, Kennedy DJ, Bohle PL, Campbell DS, Knapman L, Grady J, et al. Efficacy and feasibility of a novel tri-modal robust exercise prescription in a retirement community: A randomized, controlled trial. Journal of the American Geriatrics Society. 2007;55(1):1–10. doi: 10.1111/j.1532-5415.2006.01031.x. [DOI] [PubMed] [Google Scholar]
- Blazer DG. Origins of depression in later life. Psychological Medicine. 2005;35(9):1241–1252. doi: 10.1017/S0033291705004411. [DOI] [PubMed] [Google Scholar]
- Bopp M, Wilcox S, Oberrecht L, Kammermann S, McElmurray CT. Correlates of strength training in older rural African American and Caucasian women. Women & Health. 2004;40(1):1–20. doi: 10.1300/J013v40n01_01. [DOI] [PubMed] [Google Scholar]
- Bowling A. Measuring social networks and social support. In: Bowling A, editor. Measuring health: A review of quality of life measurement scales. 2nd ed. Philadelphia, PA: Open University Press; 1997. pp. 91–110. [Google Scholar]
- Brenes GA, Williamson JD, Messier SR, Rejeski WJ, Pahor M, Ip E, et al. Treatment of minor depression in older adults: A pilot study comparing sertraline and exercise. Aging & Mental Health. 2007;11(1):61–68. doi: 10.1080/13607860600736372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brosse AL, Sheets ES, Lett HS, Blumenthal JA. Exercise and the treatment of clinical depression in adults: Recent findings and future directions. Sports Medicine. 2002;32(12):741–760. doi: 10.2165/00007256-200232120-00001. [DOI] [PubMed] [Google Scholar]
- Bruce ML. Psychosocial risk factors for depressive disorders in late life. Biological Psychiatry. 2002;52(3):175–184. doi: 10.1016/s0006-3223(02)01410-5. [DOI] [PubMed] [Google Scholar]
- Castellano V, White LJ. Serum Brain-Derived Neurotrophic Factor response to aerobic exercise in Multiple Sclerosis. Journal of the Neurological Sciences. 2008;269(1–2):85–91. doi: 10.1016/j.jns.2007.12.030. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention [CDC] Six weeks to genomic awareness. [Retrieved January 3, 2009];2007 from http://www.cdc.gov/genomics/training/sixwks.htm.
- Centers for Disease Control and Prevention [CDC] Physical activity for everyone: Glossary of terms. [Retrieved August 18, 2009];2009 from http://www.cdc.gov.proxy.lib.umich.edu/physicaiactivity/everyone/glossary/index.html.
- Cohen S. Psychosocial models of the role of social support in the etiology of physical disease. Health Psychology. 1988;7(3):269–297. doi: 10.1037//0278-6133.7.3.269. [DOI] [PubMed] [Google Scholar]
- Craft LL, Perna FM. The benefits of exercise for the clinically depressed. Primary Care Companion Journal of Clinical Psychiatry. 2004;6(3):104–111. doi: 10.4088/pcc.v06n0301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Depner CE, Wethington E, Ingersoll-Dayton B. Social support: Methodological issues in design and measurement. Journal of Social Issues. 1984;40(4):37–54. [Google Scholar]
- Dishman RK, Berthoud H, Booth FW, Cotman CW, Edgerton VR, Fleshner MR, et al. Neurobiology of exercise. Obesity. 2006;14(3):345–356. doi: 10.1038/oby.2006.46. [DOI] [PubMed] [Google Scholar]
- Dunn AL, Trivedi MH, Kampert JB, Clark CG, Chambliss HO. Exercise treatment for depression: Efficacy and dose response. American Journal of Preventive Medicine. 2005;28(1):1–8. doi: 10.1016/j.amepre.2004.09.003. [DOI] [PubMed] [Google Scholar]
- Farmer ME, Locke BZ, Moscicki EK, Dannenberg AL, Larson DB, Radloff LS. Physical activity and depressive symptoms: The NHANES I epidemiologic follow-up study. American Journal of Epidemiology. 1988;128(6):1340–1351. doi: 10.1093/oxfordjournals.aje.a115087. [DOI] [PubMed] [Google Scholar]
- Ferris LT, Williams JS, Shen CL. The effect of acute exercise on serum Brain-Derived Neurotrophic Factor levels and cognitive function. Medicine & Science in Sports & Exercise. 2007;39(4):728–734. doi: 10.1249/mss.0b013e31802f04c7. [DOI] [PubMed] [Google Scholar]
- Fox KR. The influence of physical activity on mental well-being. Public Health Nutrition. 1999;2(3A):411–418. doi: 10.1017/s1368980099000567. [DOI] [PubMed] [Google Scholar]
- Gallagher NA, Gretebeck KA, Robinson J, Torres ER, Murphy SL, Martyn K. Neighborhood factors relevant to walking in older urban African-Americans: Use of focus groups and photovoice. Journal of Aging and Physical Activity. 2010;18:99–115. doi: 10.1123/japa.18.1.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold SM, Schulz KH, Hartmann S, Mladek M, Lang UE, Hellweg R, et al. Basal serum levels and reactivity of nerve growth factor and Brain-Derived Neurotrophic Factor to standardized acute exercise in Multiple Sclerosis and controls. Journal of Neuroimmunology. 2003;138(1–2):99–105. doi: 10.1016/s0165-5728(03)00121-8. [DOI] [PubMed] [Google Scholar]
- Harris T. Recent developments in understanding the psychosocial aspects of depression. British Medical Bulletin. 2001;57:17–32. doi: 10.1093/bmb/57.1.17. [DOI] [PubMed] [Google Scholar]
- House JS, Kahn RL. Measures and concepts of social support. In: Cohen S, Syme L, editors. Social support and health. Orlando, FL: Academic Press; 1985. pp. 83–103. [Google Scholar]
- House JS, Williams DR. Understanding and reducing socioeconomic and Racial/Ethnic disparities in health. In: Smedley BD, Syme SL, editors. Promoting health: Intervention strategies from social and behavioral research. Washington, D.C.: National Academy Press; 2000. pp. 81–124. [Google Scholar]
- Hutchinson C. Social support: Factors to consider when designing studies that measure social support. Journal of Advanced Nursing. 1999;26(6):1520–1526. doi: 10.1046/j.1365-2648.1999.01041.x. [DOI] [PubMed] [Google Scholar]
- Israel BA. Social networks and health status: Linking theory, research, and practice. Patient Counseling and Health Education. 1982;4(2):65–79. doi: 10.1016/s0190-2040(82)80002-5. [DOI] [PubMed] [Google Scholar]
- Israel BA, Rounds KA. Social networks and social support: A synthesis for health educators. Advances on Health Education and Promotion. 1987;2:311–347. [Google Scholar]
- Izquierdo-Porrera AM, Powell CC, Reiner J, Fontaine KR. Correlates of exercise adherence in an African American church community. Cultural Diversity & Ethnic Minority Psychology. 2002;8(4):389–394. doi: 10.1037/1099-9809.8.4.390. [DOI] [PubMed] [Google Scholar]
- Jadad AR, Moher D, Klassen TP. Guides for reading and interpreting systematic reviews: II. How did the authors find the studies and assess their quality? Archives of Pediatrics & Adolescent Medicine. 1998;152(8):812–817. doi: 10.1001/archpedi.152.8.812. [DOI] [PubMed] [Google Scholar]
- Jorm AF. The epidemiology of depressive states in the elderly: Implications for recognition, intervention and prevention. Social Psychiatry and Psychiatric Epidemiology. 1995;30(2):53–59. doi: 10.1007/BF00794942. [DOI] [PubMed] [Google Scholar]
- Kawachi I, Berkman LF. Social ties and mental health. Journal of Urban Health. 2001;78(3):458–467. doi: 10.1093/jurban/78.3.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klassen TP, Jadad AR, Moher D. Guides for reading and interpreting systematic reviews: I. getting started. Archives of Pediatrics & Adolescent Medicine. 1998;152(7):700–704. [PubMed] [Google Scholar]
- Knox S, Barnes A, Kiefe C, Lewis CE, Iribarren C, Matthews KA, et al. History of depression, race, and cardiovascular risk in CARDIA. International Journal of Behavioral Medicine. 2006;13(1):44–50. doi: 10.1207/s15327558ijbm1301_6. [DOI] [PubMed] [Google Scholar]
- Knubben K, Reischies FM, Adli M, Schlattmann P, Bauer M, Dimeo F. A randomised, controlled study on the effects of a short-term endurance training programme in patients with major depression. British Journal of Sports Medicine. 2007;47(1):29–33. doi: 10.1136/bjsm.2006.030130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lépine JP, Bouchez S. Epidemiology of depression in the elderly. International Clinical Psychopharmacology. 1998;13(Suppl. 5):7–12. doi: 10.1097/00004850-199809005-00003. [DOI] [PubMed] [Google Scholar]
- Lin N, Peek MK. Social networks and mental health. In: Horwitz AV, Scheid TL, editors. A handbook for the study of mental health: Social contexts, theories and systems. Cambridge, MA: Cambridge University Press; 1999. pp. 241–258. [Google Scholar]
- Malebo A, van Eeden C, Wissing MP. Sport participation, psychological well-being, and psychosocial development in a group of young black adults. South African Journal of Psychology. 2007;37(1):188–206. [Google Scholar]
- Mather AS, Rodriguez C, Guthrie MF, McHarg AM, Reid IC, McMurdo ME. Effects of exercise on depressive symptoms in older adults with poorly responsive depressive disorder: Randomised controlled trial. British Journal of Psychiatry. 2002;180:411–415. doi: 10.1192/bjp.180.5.411. [DOI] [PubMed] [Google Scholar]
- McKinnon JD, Bennett CE. We the people: Blacks in the United States. [Retrieved January 9, 2009];2005 Aug; from www.census.gov/prod/2005pubs/censr-25.pdf.
- Mersch PPA, Middendorp HM, Bouhuys AL, Beersma DGM, van den Hoofdakker RH. Seasonal affective disorder and latitude: A review of the literature. Journal of Affective Disorders. 1999;53(1):35–48. doi: 10.1016/s0165-0327(98)00097-4. [DOI] [PubMed] [Google Scholar]
- Moher D, Schulz KF, Altman DG CONSORT GROUP [Consolidated Standards of Reporting Trials] The CONSORT statement: Revised recommendations for improving the quality of reports of parallel-group randomized trials. Annals of Internal Medicine. 2001;134(8):657–662. doi: 10.7326/0003-4819-134-8-200104170-00011. [DOI] [PubMed] [Google Scholar]
- Moher D, Jadad AR, Klassen TP. Guides for reading and interpreting systematic reviews: III. How did the authors synthesize the data and make their conclusions? Archives of Pediatrics & Adolescent Medicine. 1998;152(9):915–920. doi: 10.1001/archpedi.152.9.915. [DOI] [PubMed] [Google Scholar]
- Nationalatlas.gov. Latitude and longitude. [Retrieved January 12, 2008];2007 from http://nationalatlas.gov/articles/mappinq/a_latlong.html.
- Nelson DB, Sammel MD, Freeman EW, Lin H, Gracia CR, Schmitz KH. Effect of physical activity on menopausal symptoms among urban women. Medicine & Science in Sports & Exercise. 2008;40(1):50–58. doi: 10.1249/mss.0b013e318159d1e4. [DOI] [PubMed] [Google Scholar]
- North TC, McCullagh P, Tran ZV. Effect of exercise on depression. Exercise & Sport Sciences Reviews. 1990;18:379–415. [PubMed] [Google Scholar]
- O'Reilly P. Methodological issues in social support and social network research. Social Science and Medicine. 1988;26(8):863–873. doi: 10.1016/0277-9536(88)90179-7. [DOI] [PubMed] [Google Scholar]
- Orr ST, James SA, Garry J, Newton E. Exercise participation before and during pregnancy among low-income, urban, black women: The Baltimore Preterm Birth Study. Ethnicity & Disease. 2006;16(4):909–913. [PubMed] [Google Scholar]
- Paluska SA, Schwenk TL. Physical activity and mental health: Current concepts. Sports Medicine. 2000;29(3):167–180. doi: 10.2165/00007256-200029030-00003. [DOI] [PubMed] [Google Scholar]
- Patil SK, Johnson AS, Lichtenberg PA. The relation of pain and depression with various health-promoting behaviors in African American elders. Rehabilitation Psychology. 2008;53(1):85–92. [Google Scholar]
- Paykel ES. Life events, social support and depression. Acta Psychiatrica Scandinavica Supplementum. 1994;377:50–58. doi: 10.1111/j.1600-0447.1994.tb05803.x. [DOI] [PubMed] [Google Scholar]
- Penninx BWJH, Rejeski WJ, Pandya J, Miller ME, Di Bari M, Applegate WB, et al. Exercise and depressive symptoms: A comparison of aerobic and resistance exercise effects on emotional and physical function in older persons with high and low depressive symptomatology. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2002;57(2):124–132. doi: 10.1093/geronb/57.2.p124. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Russo-Neustadt AA, Chen MJ. Brain-Derived Neurotrophic Factor and antidepressant activity. Current Pharmaceutical Design. 2005;11(12):1495–1510. doi: 10.2174/1381612053764788. [DOI] [PubMed] [Google Scholar]
- Schulz KH, Gold SM, Witte J, Bartsch K, Lang UE, Hellweg R, et al. Impact of aerobic training on immune-endocrine parameters, neurotrophic factors, quality of life and coordinative function in multiple sclerosis. Journal of the Neurological Sciences. 2004;225(1–2):11–18. doi: 10.1016/j.jns.2004.06.009. [DOI] [PubMed] [Google Scholar]
- Scully D. Physical exercise and psychological well being: A critical review. British Journal of Sports Medicine. 1998;32(2):111–120. doi: 10.1136/bjsm.32.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shephard RJ. Limits to the measurement of habitual physical activity by questionnaires. British Journal of Sports Medicine. 2003;37:197–206. doi: 10.1136/bjsm.37.3.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegel JM, Yancey AK, McCarthy WJ. Overweight and depressive symptoms among African-American women. Preventive Medicine. 2000;31(3):232–240. doi: 10.1006/pmed.2000.0712. [DOI] [PubMed] [Google Scholar]
- Singh NA, Clements KM, Singh MA. The efficacy of exercise as a long-term antidepressant in elderly subjects: A randomized, controlled trial. Journals of Gerontology Series A-Biological Sciences & Medical Sciences. 2001;56(8):M497–M504. doi: 10.1093/gerona/56.8.m497. [DOI] [PubMed] [Google Scholar]
- Singh NA, Fiatarone Singh MA. Exercise and depression in the older adult. Nutrition in Clinical Care. 2000;3(4):197–208. [Google Scholar]
- Stokols D. Establishing and maintaining healthy environments. Toward a social ecology of health promotion. American Psychologist. 1992;47(1):6–22. doi: 10.1037//0003-066x.47.1.6. [DOI] [PubMed] [Google Scholar]
- Strawbridge WJ, Deleger S, Roberts RE, Kaplan GA. Physical activity reduces the risk of subsequent depression for older adults. American Journal of Epidemiology. 2002;156(4):328–334. doi: 10.1093/aje/kwf047. [DOI] [PubMed] [Google Scholar]
- Tang SW, Chu E, Hui T, Helmeste D, Law C. Influence of exercise on serum Brain-Derived Neurotrophic Factor concentrations in healthy human subjects. Neuroscience Letters. 2008;431(1):62–65. doi: 10.1016/j.neulet.2007.11.019. [DOI] [PubMed] [Google Scholar]
- Tardy CH. Social support measurement. American Journal of Community Psychology. 1985;73(2):187–202. [Google Scholar]
- U.S. Census Bureau (USCB) 2005 American community survey. [Retrieved January 22, 2008];2005 from http://factfinder.census.gov/servlet/STTable?_bm=v&-geo_id=01000US&-qr_name=ACS_2005_EST_G00_S0602&-ds_name=ACS_2005_EST_G00.
- U.S. Department of Health & Human Services [USDHHS] Rockville, MD: Author; 1999. Mental health: A report of the Surgeon General. [Google Scholar]
- U.S. Department of Health & Human Services [USDHHS] Rockville, MD: U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services; 2001. Mental health: Culture, race, and ethnicity-A supplement to mental health: A report of the Surgeon General. [PubMed] [Google Scholar]
- Vilhjalmsson R. Life stress, social support and clinical depression: A reanalysis of the literature. Social Science Medicine. 1993;37(3):331–342. doi: 10.1016/0277-9536(93)90264-5. [DOI] [PubMed] [Google Scholar]
- Walker L, Freeland-Graves JH, Milani T, George G, Hanss-Nuss H, Kim M, et al. Weight and behavioral and psychosocial factors among ethnically diverse, low-income women after childbirth: II. Trends and correlates. Women & Health. 2004;40(2):19–34. doi: 10.1300/J013v40n02_02. [DOI] [PubMed] [Google Scholar]
- Wilbur J, Zenk S, Wang E, Oh A, McDevitt J, Block D, et al. Neighborhood characteristics, adherence to walking, and depressive symptoms in midlife African American women. Journal of Women's Health. 2009;18(8):1201–1210. doi: 10.1089/jwh.2008.1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Jackson JS. Race/ethnicity and the 2000 census: Recommendations for African American and other black populations in the United States. American Journal of Public Health. 2000;90(11):1728–1730. doi: 10.2105/ajph.90.11.1728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Yu Y, Jackson JS, Anderson NB. Racial differences in physical and mental health: Socioeconomic status, stress and discrimination. Journal of Health Psychology. 1997;2:335–351. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- Williams DR, Gonzalez HM, Neighbors H, Nesse R, Abelson JM, Sweetman J, et al. Prevalence and distribution of major depressive disorder in African Americans, Caribbean Blacks, and non-Hispanic Whites: Results from the National Survey of American Life. Archives of General Psychiatry. 2007;64(3):305–315. doi: 10.1001/archpsyc.64.3.305. [DOI] [PubMed] [Google Scholar]
- Winter B, Breitenstein C, Mooren FC, Voelker K, Fobker M, Lechtermann A, et al. High impact running improves learning. Neurobiology of Learning & Memory. 2007;87(4):597–609. doi: 10.1016/j.nlm.2006.11.003. [DOI] [PubMed] [Google Scholar]
- Wise LA, Adams-Campbell LL, Palmer JR, Rosenberg L. Leisure time physical activity in relation to depressive symptoms in the Black Women's Health Study. Annals of Behavioral Medicine. 2006;32(1):68–76. doi: 10.1207/s15324796abm3201_8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeung RR. The acute effects of exercise on mood state. Journal of Psychosomatic Research. 1996;40(2):123–141. doi: 10.1016/0022-3999(95)00554-4. [DOI] [PubMed] [Google Scholar]
- Zheng H, Liu Y, Li W, Yang B, Chen D, Wang X, et al. Beneficial effects of exercise and its molecular mechanisms on depression in rats. Behavioural Brain Research. 2006;168(1):47–55. doi: 10.1016/j.bbr.2005.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]