Abstract
Background
Patients with diabetes often present with lower extremity (LE) edema; however, because of concomitant peripheral arterial disease, compression therapy is generally avoided by providers in fear of compromising arterial circulation. This pilot study sought to assess whether diabetic socks with mild compression (18–25 mm Hg) can reduce LE edema in patients with diabetes without negatively impacting vascularity.
Methods
Eighteen subjects (9 males, 9 females) aged 61 ± 11 years with diabetes, LE edema, and a mean ankle–brachial index (ABI) of 1.10 ± 0.21 successfully completed this uncontrolled study. At baseline, subjects were fitted and instructed to wear the socks during all waking hours. Follow-up visits occurred weekly for four consecutive weeks. Edema was quantified through midfoot, ankle, and calf circumferences and cutaneous fluid measurements. Vascular status was tracked via ABI.
Results
Repeated measures analysis of variance and least significant difference post hoc analyses were used for data analyses. Calf circumferences showed a statistically significant (p < .05) decrease of 1.3 ± 0.28 cm after just one week and remained significantly smaller than baseline throughout the study. Foot circumferences were significantly reduced at week 2 (−0.98 ± 0.35 cm) and remained significantly below baseline for the remainder of the study. The ankle also demonstrated a trend of circumference reduction but was not statistically significant. Cutaneous edema significantly reduced by week 3 (−3.1 ± 1.3 U) and remained so at week 4. Ankle–brachial index significantly increased (0.14 ± 0.049) at week 2 but was not significantly higher at weeks 3 or 4. No adverse events occurred during the study.
Conclusions
Mild compression therapy (18–25 mm Hg) decreased swelling in diabetes patients with LE edema without compromising vascularity.
Keywords: compression, diabetes, edema, lower extremity
Introduction
Diabetes mellitus has escalated to the status of a pandemic and is found in as many as 25.8 million people, or 8.3% of the United States population.1 Lower extremity (LE) or peripheral edema is a common clinical finding in patients with diabetes; however, the lack of reliable measures to objectively quantify edema2 makes it difficult to assess edema's true prevalence in this population. The cause of edema may be difficult to isolate and, in fact, may have multiple or combined etiologies.3,4 Prior to treating LE edema, a thorough history and physical must be performed to address the underlying edema pathology.5 Patients with diabetes also have a 2–5 times greater risk for developing peripheral arterial disease (PAD) as compared with the nondiabetic population.5 An estimated one out of every three people with diabetes over the age of 50 years has concomitant PAD,6 and this prevalence exceeds 70% in patients over 70 years of age.7
In patients with diabetes, foot elevation has generally been recommended to reduce edema and prevent other sequential problems.8,9 However, for ambulatory individuals, the best outcome from this would be cyclic periods of swelling and subsequent reduction. Further, foot elevation may decrease tissue oxygenation of the foot since the dependent position is known to increase blood flow within the arterial system.8,10,11
Once systemic pathology has been managed or ruled out, peripheral edema is most often treated with graduated compression therapy to reduce swelling via a wrap system that can enhance fibrinolysis and venous outflow.9 Standard compression sock therapy is defined as a graded compression of 35–45 mm Hg at the ankle, with gradually decreasing compression toward the knee.12,13 However, compression therapy has long been considered risky practice in patients with diabetes because of the fear of compromising arterial circulation in a population that has a PAD prevalence of at least 20%.14 Additionally, such high-pressure compression is not only uncomfortable, but presents difficulties to the patient during the donning and doffing process and could lead to skin trauma and abrasions. All these could potentially reduce patient compliance and, therefore, clinical effectiveness.9,15
In this study, we hypothesized that daily use of a mild compression stocking that provides 18–25 mm Hg of pressure may benefit diabetes patients with edema without vascular compromise. To our knowledge, there are no previous reports of the vascular effects of a mild compression socks on diabetes patients with LE edema. Therefore, the purpose of our study was to assess whether mild compression diabetic socks can offer benefits without compromising vascularity.
Methods
Subjects
This study received ethical approval from the local institutional review board. All participants received oral and written information and signed an informed consent before participating. Consecutive patients from the Rosalind Franklin Health System clinic aged ≥18 years with a history of type 1 or 2 diabetes and clinically identified mild-to-moderate LE edema were recruited for the study. Patients were excluded if they had an infected foot ulcer, untreated osteomyelitis, or severe PAD (ankle–brachial systolic pressure index < 0.6). All consented patients were found to meet the inclusion/exclusion criteria.
Intervention
Subjects were sized for their mild compression diabetic socks according to the manufacturer's guidelines. Each subject was dispensed 4–7 pairs at the first visit and instructed to wear them during all waking hours. They were also provided with washing solution and laundering instructions. The sock (Sigvaris Diabetic Sock, Sigvaris Inc., Peachtree, GA) provided 18–25 mm Hg of pressure (Figure 1) and incorporated the needs of a typical diabetes patient with no toe seam and extra padded foot.
Figure 1.

Sigvaris compression diabetic sock.
Procedures
The duration of this uncontrolled study was 4 weeks, and recruited subjects were requested to visit the clinic every week for clinical assessment. Midfoot, ankle, and calf circumferences were considered primary outcomes of this study. Ankle–brachial systolic pressure index and cutaneous water content were considered secondary outcomes.
At the initial visit (week 0), all subjects disclosed a full medical history and a standardized physical exam was performed. The history and physical exam included duration and type of diabetes, type of diabetes medication (insulin, oral, combination therapy, diet), previous history of foot ulcers, amputation (toe, foot), LE bypass, LE angioplasty, coronary artery bypass surgery, cardiac angioplasty, arthritis, liver disease, osteoporosis, malignancy, and bone tumors. Diabetic peripheral neuropathy was defined as lack of sensation on 1 of the 10 tested sites by 10 g Semmes-Weinstein monofilament or vibration perception threshold (VPT) at hallux >25 V.16 Subject height and weight were measured to determine body mass index (BMI).
Lower extremity edema was quantified through manual circumference measurements of the midfoot (taken at the widest midfoot area), ankle (taken at the narrowest position immediately above the medial and lateral malleoli), and calf (taken at the widest portion of the calf). Circumference measurements were verified by taking the widest of three measurements of the widest portion of the calf and midfoot, and by taking the narrowest of three measurements of the ankle. A spring-loaded Gulick tape measure was used for circumference measurements. It is a compact, self-locking tape measure with flexible vinyl tape that will not stretch and a push-button release. The tape measure is spring-loaded to offer a high level of accuracy with consistent tension that prevents excessive compression of body tissue. The largest eligible leg was designated the study leg for the remainder of the study. Cutaneous water content measurements in the calf were quantified via MoistureMeterD (Delfin Technologies Ltd., Kuopio, Finland), a handheld device that measures water content of biological tissues.17–19 The device measures the dielectric constant of the skin and subcutaneous fat, which is directly proportional to the water content in the tissue. Increasing values in the dielectric constant are indicative of increased water content. Measurements were taken with the 55 mm MoistureMeter probe centralized on the skin at the point 2 cm distal and 2 cm posterior to the fibula head. Five measurements were taken, and the mean value was used for analysis.19–21 Additionally, vascular assessment was performed using ankle–brachial index (ABI). Ankle–brachial index measurements were performed according to recommendations by the American Diabetes Association after allowing the patient to rest for at least 5 min in the supine position.22 The Koven Doppler system was used to assist in the measurement of the ABI. The brachial systolic pressure for both arms was first obtained, and the higher of the two values was used to calculate ABI. The blood pressure cuff was then placed on the patient's leg approximately 2 in. above the medial malleolus. The posterior tibial and dorsalis pedis systolic pressures were then obtained, and the higher of the ankle systolic pressures was used in the ABI calculation. Ankle–brachial indexes have been reported to be reliable measurements for diagnosing peripheral vascular disease16 and have a 95% sensitivity in detecting angiographically positive disease in an ABI of less than 0.9.23All subjects returned to the clinic within 1 week ± 1 day from the week 0 visit for four consecutive weeks. An attempt was made to schedule all follow-up appointments at the same time of day as the screening visit, and switching between morning and afternoon visit times was not allowed. At each follow-up visit (weeks 1–4), subjects were reclined to a supine position and midfoot, ankle, and calf circumference measurements were made immediately after removal of their stockings. The dielectric constant values were obtained following circumference measurements. The ABI was measured last and was always captured after the subject had been in the supine position for a minimum of 5 min.
Statistical Analysis
Statistical analyses were performed using SPSS® version 19. Results were expressed as means ± standard deviation. Repeated measures analysis of variance (ANOVA) test was used to examine significant change in the circumference measurements, cutaneous water content, and ABI in the course of intervention. If the data were found to not be spherical, a Huyhn–Feldt adjustment was used to determine significance. When a significant difference (p < .05) was found, the least significance difference test was used as the post hoc to assess pairwise comparisons. Comparison between genders was performed using Wilcoxon rank-sum test. The effect of gender and neuro-pathy severity (quantified by VPT) on outcomes of study was examined using multivariable ANOVA test.
Results
Recruitment
Twenty consecutive patients (age 61 ± 11 years, BMI 36.4 ± 9.3 kg/m2, 45% male) were recruited; however, two were lost to follow-up prior to completing the trial. Seventy-five percent of participants were diagnosed with diabetic peripheral neuropathy. Table 1 summarized the demography of recruited subjects as well as baseline clinical assessment. No significant difference was found between male and female subjects for age, BMI, history of diabetes, ABI, or ankle and calf size (p > .05). However, neuropathy severity quantified by VPT and Semmes-Weinstein monofilament at baseline was significantly higher in men (p < .05). Additionally, edema and foot size were significantly higher in men.
Table 1.
Subject Demographics
| Male N = 9 | Female N = 11 | p value | |
|---|---|---|---|
| Age (years) | 60 ± 11 | 61 ± 11 | 0.8 |
| BMI (kg/m2) | 35.3 ± 9.1 | 38.8 ± 9.1 | 0.2 |
| History of diabetes (years) | 21 ± 7 | 14 ± 10 | 0.1 |
| History of diabetic foot ulcers (% of participants) | 60% | 30% | - |
| History of venous leg ulcer (% of participants) | 10% | 20% | - |
| Diabetic peripheral neuropathy (% of participants)a | 100% | 50% | - |
| VPT (V) | 60 ± 29 | 25 ± 15 | 0.001 |
| Semmes–Weinstein monofilament (# of sensation out of ten) | 1.9 ± 2.6 | 8.1 ± 3.8 | 0.001 |
| ABI | 1.13 ± 0.20 | 1.08 ± 0.19 | 0.6 |
| Foot circumference (cm) | 30.1 ± 3.0 | 26.1 ± 2.7 | <0.01 |
| Ankle circumference (cm) | 26.3 ± 2.5 | 24.4 ± 4.4 | 0.3 |
| Calf circumference (cm) | 41.6 ± 5.0 | 41.6 ± 6.2 | 0.98 |
| Skin tissue dielectric constant value | 34.8 ± 5.9 | 27.8 ± 4.3 | <0.01 |
Defined as <10/10 Semmes–Weinstein monofilament score or VPT at hallux >25 V.
Change in Lower Extremities Circumferences
Table 2 summarizes the results across the different points of measurements. Results suggested a reduction for all three points of circumference measurements (Figure 2). Foot circumference was reduced on average by 1.9% and 4.2%, respectively, in week 1 and week 4 compared with baseline (Figure 2B). The reduction was significant at week 1 [p = .01, 95% confidence interval (CI) = (0.27,1.69) cm] and remained significant to week 4 [p = .001, 95% CI = (0.58,1.8) cm]. The circumference reduction was independent of gender (p = .56) and age (p = .99) of participants.
Table 2.
Change in Outcomes of Study Post-Intervention
| Baseline | Week 1 | Week 2 | Week 3 | Week 4 | |
|---|---|---|---|---|---|
| Foot circumference (cm) | 28.17 ± 3.43 | 27.63 ± 3.12 | 27.19 ± 3.02 | 26.88 ± 3.27 | 26.97 ± 2.87 |
| Ankle circumference (cm) | 25.25 ± 3.74 | 24.31 ± 3.53 | 24.16 ± 3.36 | 24.49 ± 4.48 | 23.64 ± 2.92 |
| Calf circumference (cm) | 41.43 ± 5.63 | 40.12 ± 5.41 | 40.26 ± 5.54 | 40.16 ± 5.21 | 40.27 ± 4.83 |
| Skin tissue dielectric constant value | 31.37 ± 5.30 | 29.66 ± 4.14 | 29.71 ± 4.35 | 28.28 ± 4.06 | 29.38 ± 4.41 |
| ABI | 1.10 ± 0.21 | 1.04 ± 0.18 | 1.24 ± 0.26 | 1.15 ± 0.22 | 1.15 ± 0.17 |
Figure 2.
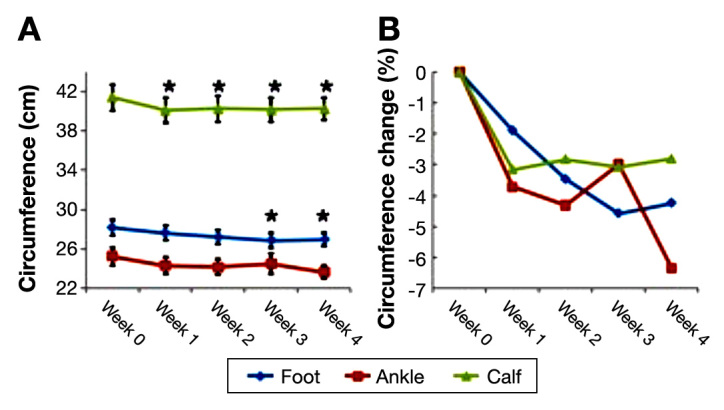
(A) Absolute change in circumference. (B) The percentage of change respect to baseline. The asterisk denotes value significantly different from baseline.
Similar results were observed for ankle circumference. The amount of reduction was significant compared with baseline measurement except for week 3. Ankle circum-ference was reduced on average by 3.7% and 6.5%, respectively, at week 1 [p = .001, 95% CI = (0.5,1.4) cm] and week 4 [p < 10-5, 95% CI = (0.94,2.3) cm]. Similar to the foot girth, the amount of reduction was independent of age and gender.
A significant reduction was also observed for calf circum-ference (p < .05). The rate of reduction was 3.2% (p < 10-4, 95 CI = [0.7,1.9] cm) at week 1 compared with baseline and remained almost the same for the remaining weeks of the study (Figure 2). Consistent with other measurements, the amount of impairment was independent of age (p = .2) and gender (p = .08).
Change in Secondary Outcomes
Cutaneous moisture, as quantified by measuring the dielectric constant value that is directly proportional to the amount of water in the tissue, also exhibited a significant decrease (Figure 3). At week 1, the dielectric constant value was reduced on average by 5.5% compared with baseline, but reduction was only significant after week 3, with an average reduction of 9.9% [p = .02, 95% CI = (0.38,5.81)]. The observed reduction was independent of age and gender (p = .16).
Figure 3.
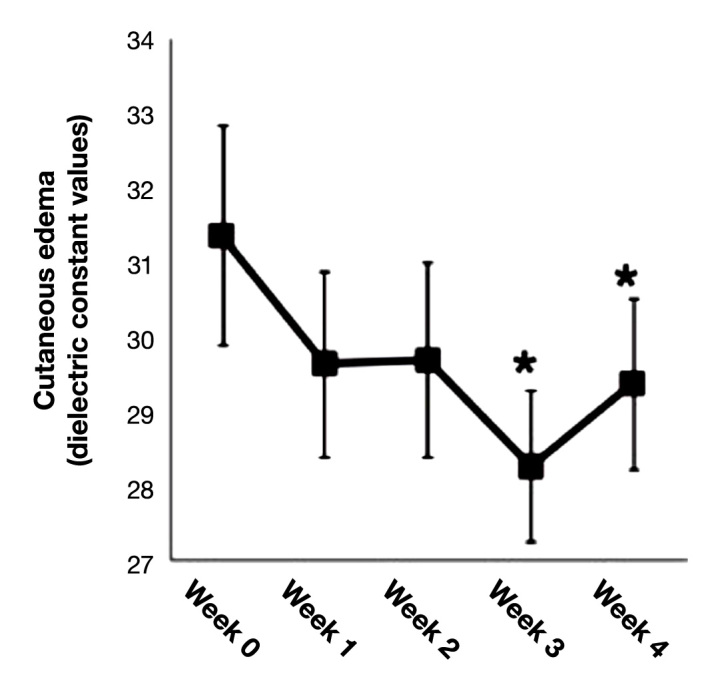
Change in cutaneous water content. The asterisk denotes a value significantly different from baseline.
Results also suggest moderate improvement in LE vascularity as quantified by ABI measurements (Figure 4). However, the improvement was only significant in week 2 [p = .01, 95% CI = (0.04,0.25)] with an average of 13.2% increase respective to baseline. Interestingly, the change in ABI was noted to be significantly dependent on age (p = .09) and gender (p = .013). Average improvement in ABI in subjects younger than 60 years old was 9% versus 19% improvement observed in individuals older than 60 years of age. On the same note, the rate of ABI improvement was 15.5% and 9.6%, respectively, in women and men at week 2 as compared with baseline, indicating a more positive impact on women than men.
Figure 4.
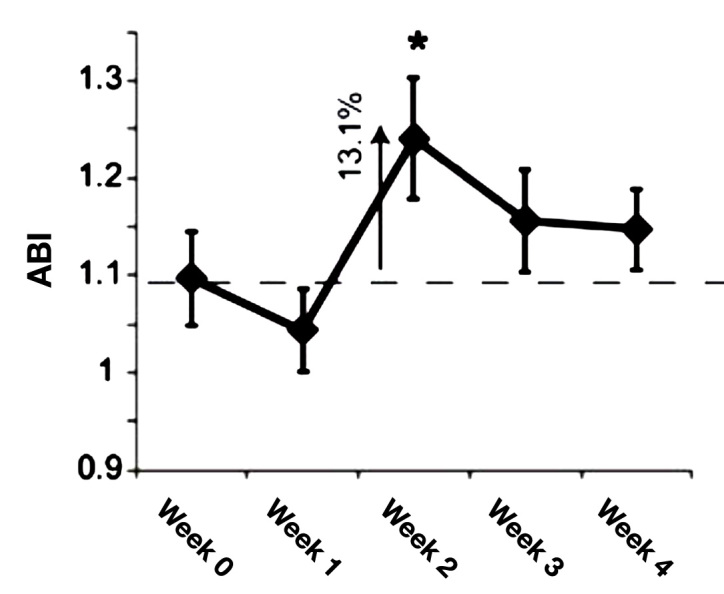
Change in ABI. The asterisk denotes a value significantly different from baseline.
No study-related adverse events occurred during the study.
Discussion
Results of this pilot, uncontrolled study demonstrated a statistically significant decrease in calf circumference, foot circumference, and cutaneous water content after wearing mild compression diabetic socks for 4 weeks. Further, there was no occurrence of skin lesions, abrasions, ulcerations, gangrene, pressure-related skin damage, clinical signs of LE underperfusion such as pain, new onset of tingling, numbness, or any other study-related adverse events, demonstrating the safety of the mild compression diabetic socks in patients with diabetes. Compression has been used successfully in patients with ABI as low as 0.5.24 Supervised reduced compression of 15–25 mm Hg has been advised for patients with moderate to severe PAD (ABI 0.5–0.85) and a vascular referral in cases where the ABI < 0.5.25–28
The findings correlated well with other studies that assessed the effect of mild compression in patients with concomitant LE edema secondary to venous insufficiency and PAD. One study assessed 2011 ulcerated legs, of which over 1416 had venous reflex. Of the 1416, 13.6% had moderate arterial disease and 2.2% had severe arterial disease. The healing rates by 36 weeks were 68% in moderate disease and 87% in normal. The authors concluded that a protocol including supervised modified compression and selective revascularization achieved good healing rates for mixed arterial and venous leg ulceration.29 Reduced compression therapy of 28 mm Hg was shown to be safe in patients with an ankle–brachial pressure index of 0.5–0.8 in a small study of 15 patients.30 A clinical case review examined the outcomes in two groups of diabetes patients with edema and venous ulceration or preulcerative conditions. Patients with adequate arterial circulation received the standard four-layer compression. Patients with compromised peripheral circulation had the highly elastic third layer eliminated. Healing occurred in 67% of patients with compromised peripheral circulation and in 81% of the patients with adequate arterial circulation. No acute progression of lower limb ischemia was noted, demonstrating the safety of mild compression in patients with concomitant edema and PAD.31 Finally, in a meta-analysis, compression with 10–20 mm Hg was found to have a clear effect on edema and symptoms as compared with <10 mm Hg pressure, placebo stockings, or no treatment (p < .001).32
The statistically significant increase in ABI was noted after the patients had worn the mild compression diabetic socks for 2 weeks. This finding coincides with literature that cited an increase in ABI following LE compression via either compression bandaging or mechanical compression pumps.33–37 This compression-related increase in ABI has been theorized to be secondary to arteriolar vaso-dilatation induced either myogenically by reduced transmural pressure or by vasodilatory substance release from the increased venous shear stress and veno–arterial interactions.37 Measurement of toe pulsation to detect macrocirculation and laser Doppler flowmetry to assess microcirculation of the dermal capillary system all demonstrated positive effects on the capillary system after two weeks of compression therapy38 and may have significant positive effects on overall microperfusion.39
Limitations of the study include the small sample size, the inability to ensure patient compliance to wearing the diabetic compression socks, human imprecision with girth measurements, the inability to have all patients assessed at the same time of day, and that the ABI was the primary evaluation for LE vascularity. While the ABI remains one of the cornerstones of the assessment process aimed at reducing bandage-pressure damage and is recommended by the American Diabetes Association Consensus as an initial assessment of vascularity in patients with diabetes, its accuracy can be affected by variations in systolic pressure and calcifications of the vessels commonly seen in patients with diabetes. Many have questioned the reliance on a single value as a cutoff point for treatment.40–43 Another limitation is that the ABI values obtained at subsequent visits were measured as soon as the compression socks were removed. While it would be ideal to measure both macrovascularity and microvascularity while the patient is wearing the diabetic compression socks, the closed-toe design of diabetic socks makes such measurements impractical. Given the clinical and budgetary limitations of this initial study, we believe that measuring the ABI at baseline and immediately after the compression socks are removed while the edema is still controlled is a reasonable end point to grossly measure the control of edema on perfusion.
This initial study indicated that mild compression diabetic socks helped reduce swelling in diabetes patients with LE edema without compromising vascularity. The statistically significant elevation in ABI warrants further investigation in both macrovascular and microvascular assessments.
Acknowledgments
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Diabetes and Digestive and Kidney Diseases or the National Institutes of Health.
Glossary
Abbreviations
- (ABI)
ankle–brachial index
- (ANOVA)
analysis of variance
- (BMI)
body mass index
- (CI)
confidence interval
- (LE)
lower extremity
- (PAD)
peripheral arterial disease
- (VPT)
vibration perception threshold
Funding
Funding for this pilot study was provided by Sigvaris Inc. (Peachtree, GA), the manufacturer of the compression diabetic socks. However, the sponsor played no role in the collection, analysis, or interpretation of the study data. Partial support of this work was also supplied by T35DK074390 from the National Institute of Diabetes and Digestive and Kidney Diseases.
References
- 1.Centers for Disease Control and Prevention. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2011. National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States, 2011. [Google Scholar]
- 2.Brodovicz KG, McNaughton K, Uemura N, Meininger G, Girman CJ, Yale SH. Reliability and feasibility of methods to quantitatively assess peripheral edema. Clin Med Res. 2009;7(1-2):21–31. doi: 10.3121/cmr.2009.819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fries R. [Differential diagnosis of leg edema] MMW Fortschr Med. 2004;146(16):39–41. [PubMed] [Google Scholar]
- 4.Powell AA, Armstrong MA. Peripheral edema. Am Fam Physician. 1997;55(5):1721–1726. [PubMed] [Google Scholar]
- 5.Ely JW, Osheroff JA, Chambliss ML, Ebell MH. Approach to leg edema of unclear etiology. J Am Board Fam Med. 2006;19(2):148–160. doi: 10.3122/jabfm.19.2.148. [DOI] [PubMed] [Google Scholar]
- 6.Eberhardt RT, Raffetto JD. Chronic venous insufficiency. Circulation. 2005;111(18):2398–2409. doi: 10.1161/01.CIR.0000164199.72440.08. [DOI] [PubMed] [Google Scholar]
- 7.Escobar C, Blanes I, Ruiz A, Vinuesa D, Montero M, Rodríguez M, Barbera G, Manzano L. Prevalence and clinical profile and management of peripheral arterial disease in elderly patients with diabetes. Eur J Intern Med. 2011;22(3):275–281. doi: 10.1016/j.ejim.2011.02.001. [DOI] [PubMed] [Google Scholar]
- 8.Park DJ, Han SK, Kim WK. Is the foot elevation the optimal position for wound healing of a diabetic foot? J Plast Reconstr Aesthet Surg. 2010 Mar;63(3):561–564. doi: 10.1016/j.bjps.2008.11.042. [DOI] [PubMed] [Google Scholar]
- 9.Izadi K, Ganchi P. Chronic wounds. Clin Plast Surg. 2005;32(2):209–222. doi: 10.1016/j.cps.2004.11.011. [DOI] [PubMed] [Google Scholar]
- 10.Johnson WC, Grant HI, Baldwin D, Hamilton JV, Dion JM. Supplemental oxygen and dependent positioning as adjunctive measures to improve forefoot tissue oxygenation. Arch Surg. 1988;123(10):1227–1230. doi: 10.1001/archsurg.1988.01400340053009. [DOI] [PubMed] [Google Scholar]
- 11.Moosa HH, Peitzman AB, Makaroun MS, Webster MW, Steed DL. Transcutaneous oxygen measurements in lower extremity ischemia: effects of position, oxygen inhalation, and arterial reconstruction. Surgery. 1988;103(2):193–198. [PubMed] [Google Scholar]
- 12.Stemmer R, Marescaux J, Furderer C. [Compression therapy of the lower extremities particularly with compression stockings] Hautarzt. 1980;31(7):355–365. [PubMed] [Google Scholar]
- 13.Burnand KG, Layer GT. Graduated elastic stockings. Br Med J (Clin Res Ed) 1986;293(6541):224–225. doi: 10.1136/bmj.293.6541.224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Elhadd TA, Robb R, Jung RT, Stonebridge PA, Belch JJ. Pilot study of prevalence of asymptomatic peripheral arterial occlusive disease in patients with diabetes attending a hospital clinic. Pract Diabetes Int. 1999;16:163–166. [Google Scholar]
- 15.Brown JR, Brown AM. Nonprescription, padded, lightweight support socks in treatment of mild to moderate lower extremity venous insufficiency. J Am Osteopath Assoc. 1995 Mar;95(3):173–181. [PubMed] [Google Scholar]
- 16.Boulton AJ, Armstrong DG, Albert SF, Frykberg RG, Hellman R, Kirkman MS, Lavery LA, LeMaster JW, Mills JL Sr, Mueller MJ, Sheehan P, Wukich DK. Comprehensive foot examination and risk assessment. A report of the Task Force of the Foot Care Interest Group of the American Diabetes Association, with endorsement by the American Association of Clinical Endocrinologists. Phys Ther. 2008;88(11):1436–1443. doi: 10.1093/ptj/88.11.1436. [DOI] [PubMed] [Google Scholar]
- 17.Nuutinen J, Ikäheimo R, Lahtinen T. Validation of a new dielectric device to assess changes of tissue water in skin and subcutaneous fat. Physiol Meas. 2004;25(2):447–454. doi: 10.1088/0967-3334/25/2/004. [DOI] [PubMed] [Google Scholar]
- 18.Dayan SH, Arkins JP, Sharma V, Paterson E, Barnes D. A phase 2, double-blind, randomized, placebo-controlled trial of a novel nutritional supplement product to promote healthy skin. J Drugs Dermatol. 2011;10(10):1106–1114. [PubMed] [Google Scholar]
- 19.Bates-Jensen BM, McCreath HE, Pongquan V. Subepidermal moisture is associated with early pressure ulcer damage in nursing home residents with dark skin tones: pilot findings. J Wound Ostomy Continence Nurs. 2009;36(3):277–284. doi: 10.1097/WON.0b013e3181a19e53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bates-Jensen BM, McCreath HE, Pongquan V, Apeles NC. Subepidermal moisture differentiates erythema and stage I pressure ulcers in nursing home residents. Wound Repair Regen. 2008;16(2):189–197. doi: 10.1111/j.1524-475X.2008.00359.x. [DOI] [PubMed] [Google Scholar]
- 21.Mayrovitz HN. Assessing lymphedema by tissue indentation force and local tissue water. Lymphology. 2009;42(2):88–98. [PubMed] [Google Scholar]
- 22.American Diabetes Association. Peripheral arterial disease in people with diabetes. Diabetes Care. 2003;26(12):3333–3341. doi: 10.2337/diacare.26.12.3333. [DOI] [PubMed] [Google Scholar]
- 23.Khan TH, Farooqui FA, Niazi K. Critical review of the ankle brachial index. Curr Cardiol Rev. 2008;4(2):101–106. doi: 10.2174/157340308784245810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.RNC Institute CfE-bn. London: RCN Institute; 1998. Clinical practice guidelines: the management of patients with venous leg ulcers. [Google Scholar]
- 25.Franks PJ, Moffatt CJ, Connolly M, Bosanquet N, Oldroyd MI, Greenhalgh RM, McCollum CN. Factors associated with healing leg ulceration with high compression. Age Ageing. 1995;24(5):407–410. doi: 10.1093/ageing/24.5.407. [DOI] [PubMed] [Google Scholar]
- 26.Arthur J, Lewis P. When is reduced-compression bandaging safe and effective? J Wound Care. 2000;9(10):469–471. doi: 10.12968/jowc.2000.9.10.26301. [DOI] [PubMed] [Google Scholar]
- 27.Scottish Intercollegiate Guidelines Network. SIGN Publication 26. Edinburgh: SIGN Publications; 1998. The care of patients with chronic leg ulcer: a national clinical guideline. [Google Scholar]
- 28.Marston W, Vowden K. Understanding compression therapy: EWMA Position document. London: MEP Ltd.; 2003. Compression therapy, a guide to safe practice. [Google Scholar]
- 29.Humphreys ML, Stewart AH, Gohel MS, Taylor M, Whyman MR, Poskitt KR. Management of mixed arterial and venous leg ulcers. Br J Surg. 2007;94(9):1104–1107. doi: 10.1002/bjs.5757. [DOI] [PubMed] [Google Scholar]
- 30.Jünger M, Hasse H, Ladwig A. St. Paul: 3M Health Care; 2010. Compression therapy in patients with peripheral arterial occlusive disease: A prospective clinical study with the 3M Coban 2 Layer Lite Compression System for ABPI≥0.5. [Google Scholar]
- 31.Bowering CK. Use of layered compression bandages in diabetic patients. Experience in patients with lower leg ulceration, peripheral edema, and features of venous and arterial disease. Adv Wound Care. 1998;11(3):129–135. [PubMed] [Google Scholar]
- 32.Amsler F, Blättler W. Compression therapy for occupational leg symptoms and chronic venous disorders - a meta-analysis of randomised controlled trials. Eur J Vasc Endovasc Surg. 2008;35(3):366–372. doi: 10.1016/j.ejvs.2007.09.021. [DOI] [PubMed] [Google Scholar]
- 33.Kavros SJ, Delis KT, Turner NS, Voll AE, Liedl DA, Gloviczki P, Rooke TW. Improving limb salvage in critical ischemia with intermittent pneumatic compression: a controlled study with 18-month follow-up. J Vasc Surg. 2008;47(3):543–549. doi: 10.1016/j.jvs.2007.11.043. [DOI] [PubMed] [Google Scholar]
- 34.De Haro J, Acin F, Florez A, Bleda S, Fernandez JL. A prospective randomized controlled study with intermittent mechanical compression of the calf in patients with claudication. J Vasc Surg. 2010;51(4):857–862. doi: 10.1016/j.jvs.2009.10.116. [DOI] [PubMed] [Google Scholar]
- 35.Slovut DP, Sullivan TM. Critical limb ischemia: medical and surgical management. Vasc Med. 2008;13(3):281–291. doi: 10.1177/1358863X08091485. [DOI] [PubMed] [Google Scholar]
- 36.Kalodiki E, Giannoukas AD. Intermittent pneumatic compression (IPC) in the treatment of peripheral arterial occlusive disease (PAOD)--a useful tool or just another device? Eur J Vasc Endovasc Surg. 2007;33(3):309–310. doi: 10.1016/j.ejvs.2006.11.006. [DOI] [PubMed] [Google Scholar]
- 37.Mayrovitz HN, Macdonald JM. Medical compression: effects on pulsatile leg blood flow. Int Angiol. 2010;29(5):436–441. [PubMed] [Google Scholar]
- 38.Sakurai T, Terui N. Effects of sympathetically induced vasomotion on tissue-capillary fluid exchange. Am J Physiol Heart Circ Physiol. 2006;291(4):H1761–7. doi: 10.1152/ajpheart.00280.2006. [DOI] [PubMed] [Google Scholar]
- 39.Heising S, Haase H, Sippel K, Riedel F, Jünger M. Cutaneous vasomotion in patients with chronic venous insufficiency and the influence of compression therapy. Clin Hemorheol Microcirc. 2009;41(1):57–66. doi: 10.3233/CH-2009-1155. [DOI] [PubMed] [Google Scholar]
- 40.Andersen CA. Noninvasive assessment of lower extremity hemodynamics in individuals with diabetes mellitus. J Vasc Surg. 2010;52(3 Suppl):76S–80S. doi: 10.1016/j.jvs.2010.06.012. [DOI] [PubMed] [Google Scholar]
- 41.Faglia E. Characteristics of peripheral arterial disease and its relevance to the diabetic population. Int J Low Extrem Wounds. 2011;10(3):152–166. doi: 10.1177/1534734611417352. [DOI] [PubMed] [Google Scholar]
- 42.Carser DG. Do we need to reappraise our method of interpreting the ankle brachial pressure index? J Wound Care. 2001;10(3):59–62. doi: 10.12968/jowc.2001.10.3.26065. [DOI] [PubMed] [Google Scholar]
- 43.Vowden P. Doppler ultrasound in the management of the diabetic foot. Diabetic Foot. 1999;2(1):16–17. [Google Scholar]


