Self-management is a key component of diabetes therapy.1 We developed a real-time partially automated interactive system—DialBetics—to achieve diabetes self-management. This is the first system combining information technology and natural language processing (NLP) that performs real-time automated text communication with patients, increasing their convenience while minimizing health care providers’ workload and cost.2 A pilot study was conducted to assess the safety, usability, and impact of remote health-data monitoring on patient hemoglobin A1c (HbA1c) outcomes and the effect of home blood pressure monitoring as a way of managing the complications related to diabetes.3
DialBetics comprises three modules:
Data transmission—patients’ blood glucose, blood pressure, body weight, and pedometer counts are measured at home and sent to the server twice a day.
Evaluation—data are automatically evaluated following the Japan Diabetes Society (JDS) guideline’s targeted values—optimally, blood sugar <110 mg/dl before breakfast and <140 mg/dl at bedtime; blood pressure <130/80 mm Hg; and pedometer count >10,000. It determines if each reading satisfies guideline requirements then sends results to each patient’s smartphone. Abnormal readings—defined as blood sugar >400 mg/dl or <40 mg/dl and systolic blood pressure >220 mm Hg—are reported as “Dr. Call,” meaning a physician will check the data and interact with the patient if necessary.
-
Communication
-
(a)
patients’ voice/text messages about meals and exercise are sent to the server;
-
(b)
messages by voice are converted to text and matched with text in the system’s database;
-
(c)
advice on lifestyle modification, matched to the patients’ input about diet and exercise, is returned to each patient (Figure 1).
-
(a)
Figure 1.
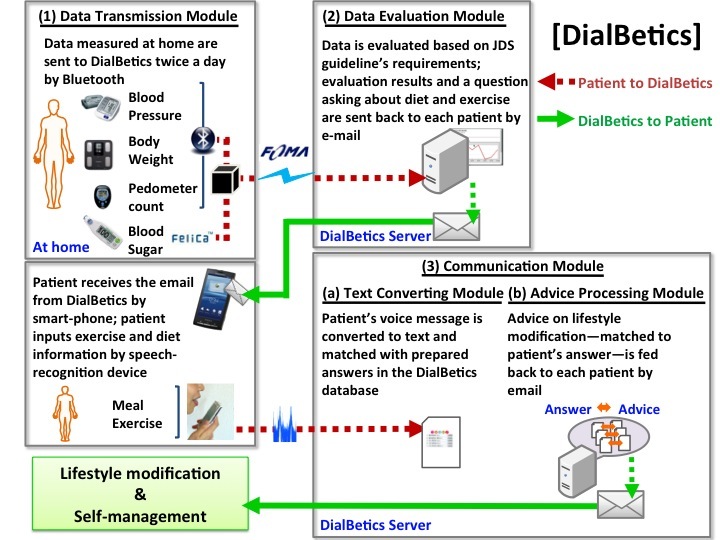
An overview of DialBetics.
For (b) and (c), the NLP-based disambiguate system allows our system to choose database words with high agreement rates for the patients’ input.4 Eleven patients who had been diagnosed with type 2 diabetes more than 5 years ago were recruited from a university hospital for a 1 month pilot study (age 61.9 ± 8.7 years, body mass index 24.6 ± 4.5 kg/m2, and HbA1c 6.79 ± 0.58%). To be eligible, patients had to be free of any severe complications—serum creatinine below 1.5 mg/dl, no proliferative retinopathy—and had to be able to exercise. Eligible patients gave consent, and the study was approved by the Institutional Review Board.
DialBetics was found accurate and safe in data transmission, evaluation, and text communication for patients whose HbA1c was around 7%. All subjects were satisfied with it and were enthusiastic about receiving real-time advice on lifestyle modification. Mean HbA1c significantly decreased 0.26% after 1 month (HbA1c 6.53 ± 0.84%, p = .02). The message processing success rate was 73.6%, which can be improved by expanding the database. Notably, it showed eight patients that their mean blood pressures did not meet the JDS goal for hypertension therapy. Because no readings were defined as “Dr. Call,” a physician’s time was not required. The study suggested that not only blood glucose monitoring but also home blood pressure monitoring might improve care of diabetes by revealing uncontrolled blood pressure, which was frequently overlooked in regular hospital visits. We plan to validate these study findings in the larger randomized controlled trial with a longer duration (in progress).
Glossary
- (HbA1c)
hemoglobin A1c
- (JDS)
Japan Diabetes Society
- (NLP)
natural language processing
References
- 1.American Diabetes Association Standards of medical care in diabetes—2010. Diabetes Care. 2010;33(Suppl 1):S11–S61. doi: 10.2337/dc10-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Russell-Minda E, Jutai J, Speechley M, Bradley K, Chudyk A, Petrella R. Health technologies for monitoring and managing diabetes: a systematic review. J Diabetes Sci Technol. 2009;3(6):1460–1471. doi: 10.1177/193229680900300628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. UK Prospective Diabetes Study Group. BMJ. 1998;317(7160):703–713. [PMC free article] [PubMed] [Google Scholar]
- 4.Aramaki E, Imai T, Miyo K, Ohe K. Orthographic Disambiguation Incorporating Transliterated Probability, International Joint Conference on Natural Language Processing. IJCNLP2008. 2008:48–55. [Google Scholar]


