Abstract
Objective
This study aimed to examine the secular trends in body mass index (BMI), waist circumference (WC), and the prevalence of general and abdominal obesity among Chinese children and adolescents from 1993 to 2009.
Methods
Data were obtained from the China Health and Nutrition Survey conducted from 1993 to 2009. 9693 children and adolescents aged 6-17years were included in this study, with their height, weight and WC were measured. General obesity was defined using the BMI cutoffs for overweight recommended by the International Obesity Task Force, and abdominal obesity was assessed when a WC above the 90th percentile for sex and age.
Results
Among total participants, mean BMI and WC increased significantly over the period 1993–2009: BMI increased from 17.6 to 17.8 kg/m2, and WC increased from 61.4 to 63.1 cm (both increases P <0.001). The prevalence of general obesity and abdominal obesity increased significantly over the period: general obesity (including overweight) rose from 6.1% to 13.1% and abdominal obesity from 4.9% to 11.7% (both increases P <0.001). WC and abdominal obesity increased at a relatively higher rate than BMI and general obesity. Upward trends in the prevalence of general and abdominal obesity were observed in all subgroups of sex, age and region (all increases P <0.05), except for abdominal obesity in girls aged 13–17 years old (P =0.102).
Conclusion
General and abdominal obesity increased significantly over the past 17 years in Chinese children.
Keywords: trend, body mass index, waist circumference, obesity, children, adolescents, China
Introduction
Many developed countries are facing considerable increases in overweight and obesity among children and adolescents (1,2). In China, along with the rapid economic growth, children and adolescents are becoming increasingly overweight and obese (3,4). Overweight children are more likely to be accompanied with many cardiovascular risk factors (including hypertension and dyslipidemia) and metabolic syndrome (5). Overweight during childhood and adolescence is also a risk factor for adult overweight, hypertension, and even mortality (6). Even among early school-aged children, weight status in childhood appears to be an important determinant of the health risk and obesity in adulthood (7).
In most studies, definitions of overweight and obesity in children and adolescents are based on the reference standards of body mass index (BMI) (3,4,8). However, BMI is a crude measure of adiposity and is unable to distinguish between fat mass and lean body mass, and the changes in BMI include substantial changes in lean mass as well as fat (9). BMI is a poor proxy for central fatness, and it has therefore systematically underestimated the prevalence of obesity in young people (10).
In children and adolescents, abdominal fat distribution, especially visceral fat deposition is more strongly related to the cardiovascular risk factors than whole-body fat (11). Waist circumference (WC) is a highly sensitive and specific measurement of central adiposity in children (10). Abdominal obesity (diagnosed using WC) is proved to be an independent indicator of hypertension, insulin resistance, dyslipidemia, cardiovascular disease, and all-cause mortalityin children and adults (12,13).
Although some studies have reported the trends of overweight and obesity (defined by BMI) in Chinese children (3,4), little data have been available on the secular trends in WC and abdominal obesity among Chinese children and adolescents. Using data from the China Health and Nutrition Surveys (CHNS) conducted from 1993 to 2009, we aimed to examine the secular trends in mean BMI and WC, and prevalence of general and abdominal obesityamong Chinese children and adolescents.
Methods
Study design and population
We used data from the CHNS, which is a national and survey to investigate the health and nutritional status in China. CHNS has been conducted successively in the year of 1989, 1991, 1993, 1997, 2000, 2004, 2006, and 2009. Study sample was drawn from nine provinces (Liaoning, Heilongjiang, Jiangsu, Shandong, Henan, Hubei, Hunan, Guangxi and Guizhou) through a multistage, random cluster process (14). All participants provided informed consents and the study was approved by institutional review board from the University of North Carolina at Chapel Hill and the National Institute for Nutrition and Food Safety, China Center for Disease Control and Prevention.
In this study, 9693 children and adolescents aged 6–17 years were included, with 1368, 2372, 2318, 1521, 1114, and 1000 children and adolescents in the survey years of 1993, 1997, 2000, 2004, 2006, and 2009 respectively. Information on age, sex, region, WC, and BMI were collected, and WC was collected initially from 1993. The sex distributions across the six survey periods were homogeneous.
Measurements
Height was measured to the nearest 0.1 cm without shoes using a portable stadiometer, and weight was measured to the nearest 0.1 kg with lightweight clothing on a calibrated beam scale. BMI was calculated as weight in kilograms divided by the square of height in meters. WC was measured at a point midway between the lowest rib and the iliac crest in a horizontal plane using non-elastic tape. Height, weight and WC were measured by trained examiners following a standard protocol from the World Health Organization (WHO) (15). Height, weight and WC measured two times on one visit were averaged and reported as the corresponding values in this study.
Definitions
The sex- and age-specific BMI cutoff points recommended by the International Obesity Task Force (IOTF)(16) were used to define “general obesity” (overweight and obesity) in children aged 6–17 years, in which the IOTF cutoff points are based on the percentile curve passing through the BMI of 25 kg/m2 at 18 years of age.
Since different populations have different growth pattern and fat accumulation (17), there are no international representative curves for WC. We used the age- and sex-specific WC reference standard of Chinese children and adolescents to define abdominal obesity. Subjects with a WC above the 90th percentile for sex and age were defined as abdominally obese according to the Bogalusa Heart Study (18). For children aged 7–17 years, abdominal obesity was defined according to the WC reference values of Chinese children and adolescents, which was developed based on national surveillance data (19). However, this local reference did not include WC reference value for children aged 6 years old. In this study, abdominal obesity in children aged 6 years old was defined using the 90th WC percentile from the Physical Fitness and Health Surveillance of Chinese School Students in 2005 (20).
Statistical analysis
SPSS version 13.0 (SPSS, Inc., Chicago, Illinois) was used for data statistical analysis. We calculated the absolute changes and relative changes in the mean values of BMI, WC and the prevalence of general and abdominal obesity to further examine the magnitude of changes over time. Multiple linear regression analysis was conducted to assess the time trends in BMI and WC, and logistical regression models were used to assess the secular trends in prevalence of general and abdominal obesity from 1993 to 2009, after controlling for the covariates of age, sex and region. P<0.05 was considered statistically significant.
Results
Table I shows the trends in BMI and WC of Chinese children and adolescents from 1993 to 2009. Among total participants, mean BMI increased slightly across 6 study periods (P<0.001), with the absolute increase of only 0.2kg/m2 and the relative increase of 1.1% from 1993 to 2009. After stratified by sex and age, mean BMI increased in boys of all age and girls aged 6–12-years (all increases P<0.001), while no significant trend was observed in adolescent girls aged 13–17 years (P=0.552). BMI increased more rapidly in boys aged 6–12 years than their adolescent peers (4.3% vs. 3.7% of relative increase). After stratified by region, mean BMI increased more dramatically in urban subjects than in their rural counterparts (0.8kg/m2 vs. −0.1kg/m2 of absolute difference, and 4.6% vs. −0.6% of relative increase).
Table I.
Trends in BMI and WC among Chinese Children and Adolescents: the CHNS 1993–2009.
| 1993 | 1997 | 2000 | 2004 | 2006 | 2009 | Absolute differencea | Relative change, %b | P for trendc | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||||||
| n | Mean (SE) | n | Mean (SE) | n | Mean (SE) | n | Mean (SE) | n | Mean (SE) | n | Mean (SE) | ||||
| BMI (kg/m2) | |||||||||||||||
| Total | 1368 | 17.6(0.1) | 2372 | 17.2(0.1) | 2318 | 17.6(0.1) | 1521 | 17.8(0.1) | 1114 | 17.7(0.1) | 1000 | 17.8(0.1) | 0.2 | 1.1 | <0.001 |
| Boys | |||||||||||||||
| 6–12 years | 358 | 16.1(0.1) | 800 | 16.3(0.1) | 708 | 16.7(0.1) | 423 | 16.6(0.1) | 343 | 16.8(0.2) | 341 | 16.8(0.2) | 0.7 | 4.3 | <0.001 |
| 13–17 years | 354 | 18.8(0.1) | 441 | 19.0(0.1) | 529 | 18.9(0.1) | 383 | 19.4(0.1) | 242 | 19.2(0.2) | 214 | 19.5(0.2) | 0.7 | 3.7 | <0.001 |
| Girls | |||||||||||||||
| 6–12 years | 311 | 15.9(0.1) | 721 | 16.0(0.1) | 610 | 16.3(0.1) | 383 | 16.4(0.1) | 307 | 16.5(0.2) | 269 | 16.6(0.2) | 0.7 | 4.4 | <0.001 |
| 13–17 years | 345 | 19.3(0.1) | 410 | 19.2(0.1) | 471 | 19.0(0.1) | 332 | 19.3(0.1) | 222 | 19.1(0.2) | 176 | 19.2(0.2) | −0.1 | −0.5 | 0.552 |
| Region | |||||||||||||||
| Urban | 434 | 17.5(0.1) | 725 | 17.6(0.1) | 640 | 18.0(0.1) | 434 | 18.3(0.2) | 324 | 18.4(0.2) | 269 | 18.3(0.2) | 0.8 | 4.6 | <0.001 |
| Rural | 934 | 17.6(0.1) | 1647 | 17.1(0.1) | 1678 | 17.4(0.1) | 1087 | 17.7(0.1) | 790 | 17.4(0.1) | 731 | 17.5(0.1) | −0.1 | −0.6 | <0.001 |
| WC (cm) | |||||||||||||||
| Total | 1368 | 61.4(0.2) | 2372 | 60.6(0.2) | 2318 | 62.2(0.2) | 1521 | 62.9(0.2) | 1114 | 62.4(0.3) | 1000 | 63.1(0.3) | 1.7 | 2.8 | <0.001 |
| Boys | |||||||||||||||
| 6–12 years | 358 | 56.5(0.4) | 800 | 57.5(0.2) | 708 | 59.3(0.3) | 423 | 58.5(0.4) | 343 | 58.6(0.5) | 341 | 60.2(0.5) | 3.7 | 6.5 | <0.001 |
| 13–17 years | 354 | 67.2(0.4) | 441 | 67.8(0.3) | 529 | 68.1(0.3) | 383 | 70.3(0.4) | 242 | 70.9(0.6) | 214 | 70.6(0.6) | 3.4 | 5.1 | <0.001 |
| Girls | |||||||||||||||
| 6–12 years | 311 | 55.4(0.4) | 721 | 56.4(0.2) | 610 | 57.4(0.3) | 383 | 56.7(0.4) | 307 | 56.6(0.4) | 269 | 58.2(0.5) | 2.8 | 5.1 | 0.024 |
| 13–17 years | 345 | 65.9(0.4) | 410 | 66.3(0.3) | 471 | 66.3(0.3) | 332 | 67.1(0.4) | 222 | 67.1(0.4) | 176 | 66.9(0.6) | 1.0 | 1.5 | 0.001 |
| Region | |||||||||||||||
| Urban | 434 | 61.8(0.4) | 725 | 61.4(0.3) | 640 | 63.5(0.3) | 434 | 64.2(0.5) | 324 | 64.7(0.6) | 269 | 63.8(0.6) | 2.0 | 3.2 | <0.001 |
| Rural | 934 | 61.2(0.3) | 1647 | 60.2(0.2) | 1678 | 61.7(0.2) | 1087 | 62.4(0.3) | 790 | 61.5(0.3) | 731 | 62.8(0.4) | 1.6 | 2.6 | <0.001 |
difference between 1993 and 2009.
relative change between 1993 and 2009.
Trends in mean BMI and WC across the study periods were tested using linear regression model adjusted for sex, age and region.
Different from BMI, mean WC increased significantly across 6 study periods (P<0.001), with more rapid increase in boys than in girls. Either in boys or in girls, upward trends in mean WC were still observed in all subgroups of age (all increases P<0.03), with larger absolute and relative increases in children than in adolescents (for boys: 3.7cm vs. 3.4cm of absolute increase, and 6.5% vs. 5.1% of relative increase; for girls: 2.8cm vs. 1.0cm of absolute increase, and 5.1% vs. 1.5% of relative increase). WC increased from 1993 to 2009 in both urban and rural subjects (both increases P<0.001), with larger increase in urban subjects than those living in rural areas (2.0cm vs. 1.6cm of absolute increase, and 3.2% vs. 2.6% of relative increase).
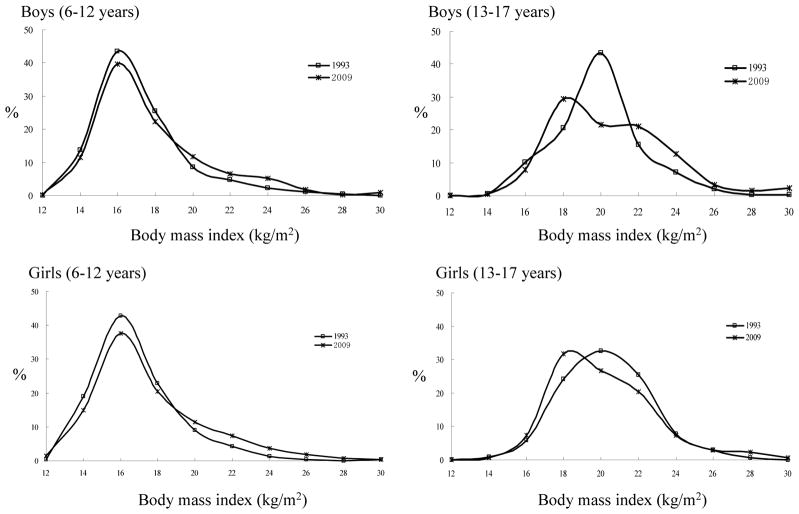
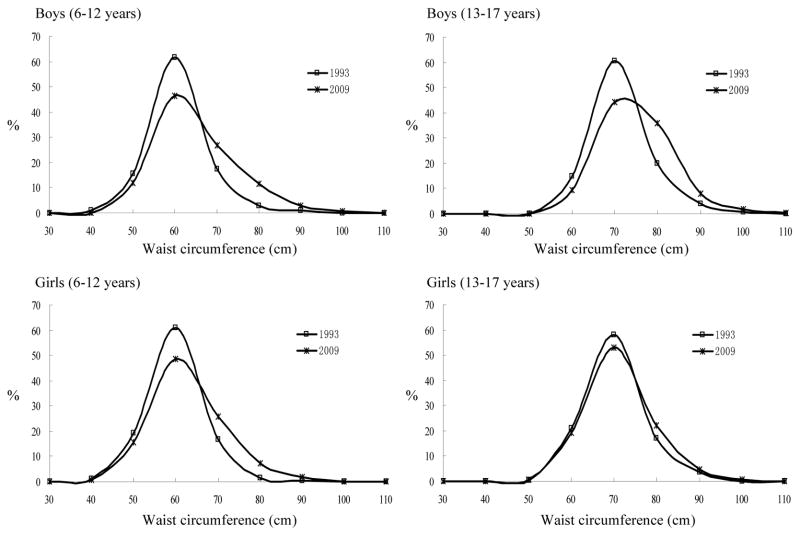
Figure 1 displays the distribution of BMI among Chinese children and adolescents in 1993 and 2009. In all boys and some girls (aged 6–12 years old), higher BMI distribution shifted slightly to the right from 1993 to 2009. While in those girls aged 13–17 years old, no significant shift in the BMI distribution was found in 2009. The distribution curves of WC in Chinese boys and girls from 1993 and 2009 are displayed in figure 2. In both boys and girls, the distribution of higher WC shifted slightly to the right from 1993 to 2009. The increase of WC was larger in boys than in girls.
Figure 1.
Distribution of body mass index in Chinese children and adolescents from 1993 to 2009
Figure 2.
Distribution of waist circumference in Chinese children and adolescents from 1993 to 2009
Table II shows the secular trends in prevalence of general obesity and abdominal obesity from 1993 to 2009. After adjustment of sex, age and region, upward trends in the prevalence of general obesity and abdominal obesity were observed among total participants (both increases P<0.001), with absolute increases of 7.0 and 6.8 percentage points for general obesity and abdominal obesity respectively. Compared with girls of the same age, boys aged 6–12 years had smaller increases in the prevalence of general obesity and abdominal obesity, while those adolescent boys had greater increases in the prevalence. After stratified by sex and age and region, upward trends in the prevalence of general obesity were still observed in all subgroups (all increases P<0.05). Either in boys or in girls, adolescents had larger relative increase in general obesity than their counterparts aged 6–12 years old. Urban participants had larger absolute and relative increases in the prevalence of general obesity than their rural counterparts (11.1 vs. 5.5 percentage points of absolute increase, and 185.0% vs. 90.2% of relative increase).
Table II.
Trends in prevalence of general and abdominal obesity among Chinese Children and Adolescents: the CHNS 1993–2009.
| 1993 | 1997 | 2000 | 2004 | 2006 | 2009 | Absolute difference, %b | Relative change, %c | P for trendd | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||||||
| n | % (SE) | n | % (SE) | n | % (SE) | n | % (SE) | n | % (SE) | n | % (SE) | ||||
| General obesitya | |||||||||||||||
| Total | 1368 | 6.1(0.6) | 2372 | 7.0(0.5) | 2318 | 7.4(0.5) | 1521 | 10.1(0.8) | 1114 | 10.3(0.9) | 1000 | 13.1(1.1) | 7.0 | 114.8 | <0.001 |
| Boys | |||||||||||||||
| 6–12 years | 358 | 10.1(1.6) | 800 | 9.5(1.0) | 708 | 9.7(1.1) | 423 | 13.2(1.6) | 343 | 13.7(1.9) | 341 | 15.5(2.0) | 5.4 | 53.5 | <0.001 |
| 13–17 years | 354 | 3.7(1.0) | 441 | 5.2(1.1) | 529 | 6.2(1.1) | 383 | 7.3(1.3) | 242 | 8.7(1.8) | 214 | 12.6(2.3) | 8.9 | 240.5 | <0.001 |
| Girls | |||||||||||||||
| 6–12 years | 311 | 7.4(1.5) | 721 | 7.8(1.0) | 610 | 8.0(1.1) | 383 | 13.6(1.8) | 307 | 12.4(1.9) | 269 | 14.5(2.1) | 7.1 | 96.0 | <0.001 |
| 13–17 years | 345 | 3.2(0.9) | 410 | 2.9(0.8) | 471 | 4.5(1.0) | 332 | 5.1(1.2) | 222 | 4.1(1.3) | 176 | 6.8(1.9) | 3.6 | 112.5 | 0.042 |
| Region | |||||||||||||||
| Urban | 434 | 6.0(1.1) | 725 | 8.1(1.0) | 640 | 9.8(1.2) | 434 | 12.9(1.6) | 324 | 11.4(1.8) | 269 | 17.1(2.3) | 11.1 | 185.0 | <0.001 |
| Rural | 934 | 6.1(0.8) | 1647 | 6.6(0.6) | 1678 | 6.5(0.6) | 1087 | 8.9(0.9) | 790 | 9.9(1.1) | 731 | 11.6(1.2) | 5.5 | 90.2 | <0.001 |
| Abdominal obesity | |||||||||||||||
| Total | 1368 | 4.9(0.6) | 2372 | 5.1(0.5) | 2318 | 7.0(0.5) | 1521 | 9.4(0.7) | 1114 | 8.5(0.8) | 1000 | 11.7(1.0) | 6.8 | 138.8 | <0.001 |
| Boys | |||||||||||||||
| 6–12 years | 358 | 3.4(1.0) | 800 | 3.1(0.6) | 708 | 5.2(0.8) | 423 | 6.1(1.2) | 343 | 6.7(1.4) | 341 | 11.1(1.7) | 7.7 | 226.5 | <0.001 |
| 13–17 years | 354 | 4.5(1.1) | 441 | 3.9(0.9) | 529 | 7.6(1.1) | 383 | 11.5(1.6) | 242 | 12.8(2.1) | 214 | 11.7(2.2) | 7.2 | 160.0 | <0.001 |
| Girls | |||||||||||||||
| 6–12 years | 311 | 3.2(1.0) | 721 | 5.8(0.9) | 610 | 6.1(1.0) | 383 | 8.4(1.4) | 307 | 6.2(1.4) | 269 | 13.0(2.1) | 9.8 | 306.3 | <0.001 |
| 13–17 years | 345 | 8.4(1.5) | 410 | 9.0(1.4) | 471 | 10.2(1.4) | 332 | 12.3(1.8) | 222 | 9.9(2.0) | 176 | 10.8(2.3) | 2.4 | 28.6 | 0.102 |
| Region | |||||||||||||||
| Urban | 434 | 7.4(1.3) | 725 | 6.3(0.9) | 640 | 8.9(1.1) | 434 | 13.8(1.7) | 324 | 10.2(1.7) | 269 | 13.0(2.1) | 5.6 | 75.7 | <0.001 |
| Rural | 934 | 3.7(0.6) | 1647 | 4.6(0.5) | 1678 | 6.3(0.6) | 1087 | 7.6(0.8) | 790 | 7.8(1.0) | 731 | 11.2(1.2) | 7.5 | 202.7 | <0.001 |
including overweight.
difference between 1993 and 2009.
relative change between 1993 and 2009.
Trends in the prevalence of general and abdominal obesity were tested using logistic regression model adjusted for sex, age and region.
Over the past 17 years, the prevalence of abdominal obesity in Chinese children and adolescents aged 6–17 years old increased by 192.3% (from 3.9% to 11.4%) for boys and 105.1% (from 5.9% to 12.1%) for girls. In the stratified analysis, the prevalence of abdominal obesity increased significantly over the 6 study periods in the two agegroups of boys (both increases P<0.001), with larger absolute and relative increases in boys aged 6–12 years. However, the trends in abdominal obesity of girls were different from boys. The prevalence of abdominal obesity increased significantly in girls aged 6–12 years old (P<0.001), but no significant trend was observed among adolescent girls (P=0.102). Different from general obesity, rural participants had larger absolute and relative increases of abdominal obesity than their urban counterparts (7.5 vs. 5.6 percentage points of absolute increase, and 202.7% vs. 75.7% of relative increase).
Discussion
In this study, we observed the secular upward trends in general and abdominal obesity among Chinese children and adolescents from 1993 to 2009. WC and abdominal obesity increased at a relatively higher rate than BMI and general obesity over the past decades. Compared with girls of the same age, boys aged 6–12 years had smaller increases in the prevalence of general obesity and abdominal obesity, while those adolescent boys had greater increases in the prevalence. Compared with their peers aged 6–12 years old, adolescents had larger relative increases of general obesity and smaller increases of abdominal obesity. Compared with those lived in rural areas, urban subjects had larger increases of general obesity, but smaller increase of abdominal obesity.
Many previous studies have reported the upward trends in overweight and obesity among children and adolescents in China (3,4,21). Among total participants aged 6 to 17 years old, the prevalence of general obesity (including overweight) increased significantly from 6.1% in 1993 to 13.1% in 2009, an increase of 7.0 percentage points in 17 years. In some previous studies, which also used IOTF reference to define overweight and obesity, the prevalence of overweight (including obesity) increased from 4.7% in 1991 to 10.5% in 2004 among 6 to 18-year-olds (21), and increased from 5.2% in 1991 to 13.2% in 2006 among 7 to 17-year-olds (4). Our results were consistent with these previous results.
Some countries have reported the prevalence of abdominal fat distribution based on WC measurements (10,22,23). The prevalence of abdominal obesity using the index of WC in children aged 6–12 years old was higher in Greek children (12.5% in boys and 14.2% in girls) (23) than in our Chinese children of similar age (11.1% in boys and 13.0% in girls in 2009). However, due to the different reference in WC, results from different studies should be compared with caution. Over the past 17 years, the prevalence of abdominal obesity in Chinese children and adolescents aged 6–17 years old increased by 192.3% (from 3.9% to 11.4%) for boys and 105.1% (from 5.9% to 12.1%) for girls. The relative changes were greatly higher than their age-matched peers from US, which were 61.0% (from 10.5% to 16.9%) for boys and 72.6% (from 10.6% to 18.3%) for girls between 1988–1994 and 1999–2004 (22). Additionally, Our results also showed that WC and abdominal obesity increased at a relatively higher rate than BMI and general obesity over the past decades, which was consistent with the data from British children aged 11–16 years old (10).
Sex differences in general and abdominal obesity were observed in the present study. During almost every study year, boys had higher prevalence of general obesity than girls, while the prevalence of abdominal obesity was higher in girls, which was consistent with other results (23). Previous study has reported that the prevalence of overweight rose in boys and girls aged 7–12 years, but no trend was observed in girls aged 13–17 years (4). In this study, we found the significant trend in general obesity among adolescent girls. However, there was no significant trend in the prevalence of abdominal obesity in adolescent girls. Probable reason is that adolescent girls, especially those female students in high school, are more concerned about their weights and desire for a slim physique (24). In addition, the sex differences in overweight trends may also be related to the emerging social pressure of preference for thinness among female adolescents and their guardians (25). In this study, the prevalence of general and abdominal obesity increased more rapidly in girls than in boys when the participants were in their childhood of 6–12 years, but the trend reversed itself when subjects were in their adolescence. The sex differences have been reported in the relations among diet, physical activity, and abdominal fat accumulation both in children and adults, with discrepant results in many studies (26,27). Moreover, the sex differences may be related to the society’s traditional preference for sons particularly in rural areas, and boys are likely to enjoy more of the family’s resources (4). However, the effect of gender remains unclear, and more investigations are needed to further prove the sex differences.
Our results showed that adolescents had larger relative increases of general obesity than their peers aged 6–12 years old. However, the increase in abdominal obesity was lower for the older age group than for the younger age group. This is probably because that many adolescents became generally overweight mostly due to the substantial increases in lean mass but not fat mass. Younger children may be more heavily affected by various contributory factors to obesity than older children (21,28). Adolescents who perceive them to be overweight may be inclined to control their weight more than their children counterparts (21).
Compared with those lived in rural areas, urban subjects had larger increases of general obesity, but smaller increases of abdominal obesity. Results from the previous study showed that the largest changes in the prevalence of overweight and obesity were observed among urban children (4), which is consistent with our findings. Economic development and change in dietary pattern might help explain the findings between the two regions. Socio-economic status (SES) has been proved to influence the prevalence of childhood overweight and obesity (29). In China, urban residents have higher SES than those living in rural areas. Like adults, children and adolescents in high SES have better access to energy-dense foods (30). However, previous study also showed that populations with lower SES have more opportunities to be exposed to the factors causing obesity (31). This may explain why we observed the larger increases in the prevalence of abdominal obesity in rural subjects than their counterparts lived in urban areas.
Obesity is proved to be an interactive symptom of many genetic and environmental factors. As genes may not substantially change during short period, the rapid increase in obesity indicates the important role of environmental and social factors (32). However, little is known about the determinants of visceral fat deposition among children and adolescents. Among children, increases in the prevalence of obesity are likely due to the interactive effects among increased caloric consumption, increased sedentary lifestyle, and decreased physical activity (33). Data showed that Chinese pattern of food consumption have changed into high consumption of animal food between 1991 and 2004 (34), which may partly explain the increasing trends in general and abdominal obesity among Chinese children and adolescents. Physical activity has been already proved to be a critical determinant of visceral fat in adults (35). Some studies have reported that physical activities (either self-reported activity or the structured physical activity) are negatively associated with WC and visceral fat in children (36,37). However, there is scarce evidence about whether some other factors, such as weight and feeding history or current dietary intake, are related to the abdominal fat distribution among children and adolescents (38). Further studies should be conducted to explore the determinants of overweight and obesity in children and adolescents.
We must mention that the results from this study were credible and powerful due to the nationally representative sample and rigorous quality control. However, there are several limitations existed in this study. Firstly, we used Chinese WC reference values to define abdominal obesity among children and adolescents. Caution should be exercised when the prevalence of abdominal obesity in this study is compared with results of other studies. Secondly, there must be many factors (including dietary and physical activities) related to the general and abdominal obesity among children and adolescents, which hadn’t been considered in the analysis of this study. Secular changes in these factors of obesity may result in the secular trends in obesity. Further studies should be conducted to assess the possible reasons of the trends in obesity.
In conclusion, general and abdominal obesity in Chinese children and adolescents increased significantly across the past 17 years. Some effective preventive and treatment measures are urgently needed to prevent the epidemic, and finally reduce the risk of obesity-related diseases.
Acknowledgments
This study was supported by the NIH (R01-HD30880, DK056350, and R01-HD38700) and the China Postdoctoral Science Foundation funded project (no. 20100481252).We thank the National Institute of Nutrition and Food Safety, China Center for Disease Control and Prevention, Carolina Population Center, the University of North Carolina at Chapel Hill, and the Fogarty International Center, the NIH for financial support for CHNS data collection and analysis files from 1989 to 2009, and both parties plus the China-Japan Friendship Hospital, Ministry of Health for support for CHNS 2009 and future surveys.
Footnotes
Declaration of interest:
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- 1.Barath A, Boda K, Tichy M, Karoly E, Turi S. International comparison of blood pressure and BMI values in schoolchildren aged 11–16 years. Acta Paediatr. 2010;99:251–5. doi: 10.1111/j.1651-2227.2009.01541.x. [DOI] [PubMed] [Google Scholar]
- 2.Kolle E, Steene-Johannessen J, Holme I, Andersen LB, Anderssen SA. Secular trends in adiposity in norwegian 9-year-olds from 1999-2000 to 2005. BMC Public Health. 2009;9:389. doi: 10.1186/1471-2458-9-389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Li Y, Schouten EG, Hu X, Cui Z, Luan D, Ma G. Obesity prevalence and time trend among youngsters in china, 1982–2002. Asia Pac J Clin Nutr. 2008;17:131–7. [PubMed] [Google Scholar]
- 4.Cui Z, Huxley R, Wu Y, Dibley MJ. Temporal trends in overweight and obesity of children and adolescents from nine provinces in china from 1991–2006. Int J Pediatr Obes. 2010;5:365–74. doi: 10.3109/17477166.2010.490262. [DOI] [PubMed] [Google Scholar]
- 5.Freedman DS, Katzmarzyk PT, Dietz WH, Srinivasan SR, Berenson GS. Relation of body mass index and skinfold thicknesses to cardiovascular disease risk factors in children: The bogalusa heart study. Am J Clin Nutr. 2009;90:210–6. doi: 10.3945/ajcn.2009.27525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Field AE, Cook NR, Gillman MW. Weight status in childhood as a predictor of becoming overweight or hypertensive in early adulthood. Obes Res. 2005;13:163–9. doi: 10.1038/oby.2005.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Salbe AD, Weyer C, Lindsay RS, Ravussin E, Tataranni PA. Assessing risk factors for obesity between childhood and adolescence: I. Birth weight, childhood adiposity, parental obesity, insulin, and leptin. Pediatrics. 2002;110:299–306. doi: 10.1542/peds.110.2.299. [DOI] [PubMed] [Google Scholar]
- 8.Rokholm B, Baker JL, Sorensen TI. The levelling off of the obesity epidemic since the year 1999--a review of evidence and perspectives. Obes Rev. 2010;11:835–46. doi: 10.1111/j.1467-789X.2010.00810.x. [DOI] [PubMed] [Google Scholar]
- 9.Demerath EW, Schubert CM, Maynard LM, et al. Do changes in body mass index percentile reflect changes in body composition in children? Data from the fels longitudinal study. Pediatrics. 2006;117:e487–95. doi: 10.1542/peds.2005-0572. [DOI] [PubMed] [Google Scholar]
- 10.McCarthy HD, Ellis SM, Cole TJ. Central overweight and obesity in british youth aged 11–16 years: Cross sectional surveys of waist circumference. BMJ. 2003;326:624. doi: 10.1136/bmj.326.7390.624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Weiss R, Dufour S, Taksali SE, et al. Prediabetes in obese youth: A syndrome of impaired glucose tolerance, severe insulin resistance, and altered myocellular and abdominal fat partitioning. Lancet. 2003;362:951–7. doi: 10.1016/S0140-6736(03)14364-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee S, Bacha F, Arslanian SA. Waist circumference, blood pressure, and lipid components of the metabolic syndrome. J Pediatr. 2006;149:809–16. doi: 10.1016/j.jpeds.2006.08.075. [DOI] [PubMed] [Google Scholar]
- 13.Zhang C, Rexrode KM, van Dam RM, Li TY, Hu FB. Abdominal obesity and the risk of all-cause, cardiovascular, and cancer mortality: Sixteen years of follow-up in us women. Circulation. 2008;117:1658–67. doi: 10.1161/CIRCULATIONAHA.107.739714. [DOI] [PubMed] [Google Scholar]
- 14.Popkin BM, Du S, Zhai F, Zhang B. Cohort profile: The china health and nutrition survey--monitoring and understanding socio-economic and health change in china, 1989-2011. Int J Epidemiol. 2011;39:1435–40. doi: 10.1093/ije/dyp322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.WHO. Report of a WHO Expert Committee Technical Report Series. World Health Organization; Geneva: 1995. Physical Status: The Use and Interpretation of Anthropometry. [PubMed] [Google Scholar]
- 16.Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: International survey. BMJ. 2000;320:1240–3. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fernandez JR, Redden DT, Pietrobelli A, Allison DB. Waist circumference percentiles in nationally representative samples of african-american, european-american, and mexican-american children and adolescents. J Pediatr. 2004;145:439–44. doi: 10.1016/j.jpeds.2004.06.044. [DOI] [PubMed] [Google Scholar]
- 18.Freedman DS, Serdula MK, Srinivasan SR, Berenson GS. Relation of circumferences and skinfold thicknesses to lipid and insulin concentrations in children and adolescents: The bogalusa heart study. Am J Clin Nutr. 1999;69:308–17. doi: 10.1093/ajcn/69.2.308. [DOI] [PubMed] [Google Scholar]
- 19.Ma GS, Ji CY, Ma J, et al. Waist circumference reference values for screening cardiovascular risk factors in Chinese children and adolescents. Biomed Environ Sci. 2010;23:21–31. doi: 10.1016/s0895-3988(10)60027-x. [DOI] [PubMed] [Google Scholar]
- 20.Research group of Chinese students' physical fitness and health. Report on the physical fitness and health surveillance of chinese school students. Beijing Science and Technology Publishing Company; Beijing: 2005. [Google Scholar]
- 21.Zhang J, Seo DC, Kolbe L, Middlestadt S, Zhao W. Trends in overweight among school children and adolescents in seven Chinese provinces, from 1991–2004. Int J Pediatr Obes. 2010;5:375–82. doi: 10.3109/17477161003592592. [DOI] [PubMed] [Google Scholar]
- 22.Li C, Ford ES, Mokdad AH, Cook S. Recent trends in waist circumference and waist-height ratio among us children and adolescents. Pediatrics. 2006;118:e1390–8. doi: 10.1542/peds.2006-1062. [DOI] [PubMed] [Google Scholar]
- 23.Tzotzas T, Kapantais E, Tziomalos K, et al. Prevalence of overweight and abdominal obesity in Greek children 6–12 years old: Results from the national epidemiological survey. Hippokratia. 2011;15:48–53. [PMC free article] [PubMed] [Google Scholar]
- 24.Xie B, Liu C, Chou CP, et al. Weight perception and psychological factors in chinese adolescents. J Adolesc Health. 2003;33:202–10. doi: 10.1016/s1054-139x(03)00099-5. [DOI] [PubMed] [Google Scholar]
- 25.Wang Y, Monteiro C, Popkin BM. Trends of obesity and underweight in older children and adolescents in the united states, brazil, china, and russia. Am J Clin Nutr. 2002;75:971–7. doi: 10.1093/ajcn/75.6.971. [DOI] [PubMed] [Google Scholar]
- 26.Treuth MS, Hou N, Young DR, Maynard LM. Accelerometry-measured activity or sedentary time and overweight in rural boys and girls. Obes Res. 2005;13:1606–14. doi: 10.1038/oby.2005.197. [DOI] [PubMed] [Google Scholar]
- 27.Yang X, Telama R, Viikari J, Raitakari OT. Risk of obesity in relation to physical activity tracking from youth to adulthood. Med Sci Sports Exerc. 2006;38:919–25. doi: 10.1249/01.mss.0000218121.19703.f7. [DOI] [PubMed] [Google Scholar]
- 28.Yoshinaga M, Shimago A, Koriyama C, et al. Rapid increase in the prevalence of obesity in elementary school children. Int J Obes Relat Metab Disord. 2004;28:494–9. doi: 10.1038/sj.ijo.0802608. [DOI] [PubMed] [Google Scholar]
- 29.Liou TH, Huang YC, Chou P. Prevalence and secular trends in overweight and obese taiwanese children and adolescents in 1991–2003. Ann Hum Biol. 2009;36:176–85. doi: 10.1080/03014460802691174. [DOI] [PubMed] [Google Scholar]
- 30.Wang Y. Cross-national comparison of childhood obesity: The epidemic and the relationship between obesity and socioeconomic status. Int J Epidemiol. 2001;30:1129–36. doi: 10.1093/ije/30.5.1129. [DOI] [PubMed] [Google Scholar]
- 31.Gordon-Larsen P, Nelson MC, Page P, Popkin BM. Inequality in the built environment underlies key health disparities in physical activity and obesity. Pediatrics. 2006;117:417–24. doi: 10.1542/peds.2005-0058. [DOI] [PubMed] [Google Scholar]
- 32.Rosenbaum M, Leibel RL. The physiology of body weight regulation: Relevance to the etiology of obesity in children. Pediatrics. 1998;101:525–39. [PubMed] [Google Scholar]
- 33.McMurray RG, Harrell JS, Deng S, Bradley CB, Cox LM, Bangdiwala SI. The influence of physical activity, socioeconomic status, and ethnicity on the weight status of adolescents. Obes Res. 2000;8:130–9. doi: 10.1038/oby.2000.14. [DOI] [PubMed] [Google Scholar]
- 34.Zhai F, Wang H, Du S, et al. Prospective study on nutrition transition in china. Nutr Rev. 2009;67 (Suppl 1):S56–61. doi: 10.1111/j.1753-4887.2009.00160.x. [DOI] [PubMed] [Google Scholar]
- 35.Riechman SE, Schoen RE, Weissfeld JL, Thaete FL, Kriska AM. Association of physical activity and visceral adipose tissue in older women and men. Obes Res. 2002;10:1065–73. doi: 10.1038/oby.2002.144. [DOI] [PubMed] [Google Scholar]
- 36.Klein-Platat C, Oujaa M, Wagner A, et al. Physical activity is inversely related to waist circumference in 12-y-old french adolescents. Int J Obes (Lond) 2005;29:9–14. doi: 10.1038/sj.ijo.0802740. [DOI] [PubMed] [Google Scholar]
- 37.Saelens BE, Seeley RJ, van Schaick K, Donnelly LF, O'Brien KJ. Visceral abdominal fat is correlated with whole-body fat and physical activity among 8-y-old children at risk of obesity. Am J Clin Nutr. 2007;85:46–53. doi: 10.1093/ajcn/85.1.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Goran MI. Visceral fat in prepubertal children: Influence of obesity, anthropometry, ethnicity, gender, diet, and growth. Am J Hum Biol. 1999;11:201–7. doi: 10.1002/(SICI)1520-6300(1999)11:2<201::AID-AJHB8>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]