Abstract
The purpose of this study was to examine the melanoma targeting and pharmacokinetic properties of 67Ga-DOTA-GGNle-CycMSHhex {67Ga-1,4,7,10-tetraazacyclononane-1,4,7,10-tetraacetic acid-Gly-Gly-Nle-c[Asp-His-dPhe-Arg-Trp-Lys]-CONH2} and 67Ga-NOTA-GGNle-CycMSHhex {67Ga-1,4,7-triazacyclononane-1,4,7-triacetic acid-Gly-Gly-Nle-c[Asp-His-dPhe-Arg-Trp-Lys]-CONH2} and compare with 67Ga-DOTA-GlyGlu-CycMSH {67Ga-DOTA-Gly-Glu-c[Lys-Nle-Glu-His-dPhe-Arg-Trp-Gly-Arg-Pro-Val-Asp]} we previously reported. DOTA-GGNle-CycMSHhex and NOTA-GGNle-CycMSHhex were synthesized using fluorenylmethyloxy carbonyl (Fmoc) chemistry. The melanocortin-1 (MC1) receptor binding affinity of NOTA-GGNle-CycMSHhex was determined in B16/F1 melanoma cells and compared with DOTA-GGNle-CycMSHhex. The melanoma targeting and pharmacokinetic properties of 67Ga-NOTA-GGNle-CycMSHhex and 67Ga-DOTA-GGNle-CycMSHhex were determined in B16/F1 melanoma-bearing C57 mice. NOTA-GGNle-CycMSHhex and DOTA-GGNle-CycMSHhex displayed comparable MC1 receptor binding affinities (1.6 vs. 2.1 nM) in B16/F1 melanoma cells. Both 67Ga-NOTA-GGNle-CycMSHhex and 67Ga-DOTA-GGNle-CycMSHhex exhibited dramatically enhanced melanoma uptake and reduced renal uptake than 67Ga-DOTA-GlyGlu-CycMSH in B16/F1 melanoma-bearing C57 mice. Furthermore, 67Ga-NOTA-GGNle-CycMSHhexexhibited more favorable radiolabeling conditions (> 85% radiolabeling yields started at 37°C), as well as higher tumor/kidney uptake ratios than 67Ga-DOTA-GGNle-CycMSHhex at 0.5, 2 and 24 h post-injection. High melanoma uptake coupled with low renal uptake highlighted the potential of 67Ga-NOTA-GGNle-CycMSHhexfor melanoma imaging and therapy.
Keywords: Alpha-melanocyte stimulating hormone, 67Ga-labeled, lactam bridge-cyclized peptide, melanoma targeting
INTRODUCTION
It is highly desirable to develop novel melanoma-specific diagnostic and therapeutic agents1–18 for melanoma since no curative treatment is available for patients with metastatic melanoma. Over the past several years, we and others have been interested in developing lactam bridge-cyclized alpha-melanocyte stimulating hormone (α-MSH) peptide radiopharmaceuticals targeting melanocortin-1 (MC1) receptors for melanoma imaging.19–26 Specifically, we have developed two generations of 111In-labeled novel lactam bridge-cyclized α-MSH peptides for melanoma targeting.19–24 The first-generation peptides were designed based on the construct of CycMSH peptide {c[Lys-Nle-Glu-His-dPhe-Arg-Trp-Gly-Arg-Pro-Val-Asp}], which was a 12-amino acid-peptide cyclized by a Lys-Asp lactam bridge. The second-generation peptides built upon the backbone of CycMSHhex peptide {c[Asp-His-dPhe-Arg-Trp-Lys]-CONH2}, which was a 6-amino acid-peptide cyclized by an Asp-Lys lactam bridge. The structural modifications from the first-generation peptides to the second-generation peptides enhanced melanoma uptake and reduced renal uptake of 111In-labeled CycMSHhex peptides.19–24 For instance, 111In-DOTA-Nle-CycMSHhex displayed higher melanoma uptake (19.39 ± 1.65 % ID/g at 2 h post-injection) and lower renal uptake (9.52 ± 0.44 % ID/g at 2 h post-injection) than 111In-DOTA-GlyGlu-CycMSH in B16/F1 melanoma-bearing C57 mice.19,23
In 2009, we reported 67Ga-DOTA-GlyGlu-CycMSH22 as a potential melanoma imaging agent taking advantage of the diagnostic properties of 67Ga (T1/2= 78.3 h, 93, 185 and 300 keV γ-emissions). Both flank primary B16/F1 melanoma and B16/F10 pulmonary melanoma metastases were clearly visualized by SPECT/CT using 67Ga-DOTA-GlyGlu-CycMSH as an imaging probe 2 h post-injection.22 However, despite the substantial tumor uptake (12.93 ± 1.63 %ID/g at 2 h post-injection), 67Ga-DOTA-GlyGlu-CycMSH also exhibited relatively high renal uptake (27.55 ± 7.87 %ID/g at 2 h post-injection) in B16/F1 melanoma-bearing C57 mice.22 It is important to note that 67Ga is also a potential therapeutic radionuclide because of its emissions of Auger and conversion electrons.27 Hence, we managed to reduce the renal uptake of 67Ga-DOTA-GlyGlu-CycMSH via L-lysine co-injection to facilitate its potential therapeutic application. L-lysine co-injection successfully decreased the renal uptake of 67Ga-DOTA-GlyGlu-CycMSH by 69.8% without affecting the melanoma uptake at 2 h post-injection.22
Structural modification on peptide sequence is another way to reduce the renal uptake of radiolabeled α-MSH peptides.22–24 Recently, we found that 111In-DOTA-GGNle-CycMSHhex displayed higher B16/F1 melanoma uptake (19.05 ± 5.04 % ID/g at 2 h post-injection) and reduced renal uptake (6.84 ± 0.92 % ID/g at 2 h post-injection) compared to 111In-DOTA-GlyGlu-CycMSH.22–24 Therefore, we hypothesized that 67Ga-DOTA-GGNle-CycMSHhex would exhibit enhanced melanoma uptake and reduced renal uptake than 67Ga-DOTA-GlyGlu-CycMSH. To examine our hypothesis, we determined the biodistribution of 67Ga-DOTA-GGNle-CycMSHhex in B16/F1 melanoma-bearing C57 mice in this study. Despite the fact that DOTA can form stable complexes with a variety of radionuclides including 67Ga, NOTA can also form stable complex with 67Ga at lower reaction temperature.28–29 Thus, we also determined the melanoma targeting and pharmacokinetic properties of 67Ga-NOTA-GGNle-CycMSHhexin B16/F1 melanoma-bearing C57 mice in this study.
EXPERIMENTAL PROCEDURES
Chemicals and Reagents
Amino acid and resin were purchased from Advanced ChemTech Inc. (Louisville, KY) and Novabiochem (San Diego, CA). NO2AtBu was purchased from CheMatech Inc. (Dijon, France) for peptide synthesis. 125I-Tyr2-[Nle4, d-Phe7]-α-MSH {125I-(Tyr2)-NDP-MSH} was obtained from PerkinElmer, Inc. (Waltham, MA) for receptor binding assay. 67GaCl3 was purchased from MDS Nordion, Inc. (Vancouver, Canada) for radiolabeling. All other chemicals used in this study were purchased from Thermo Fischer Scientific (Waltham, MA) and used without further purification. B16/F1 murine melanoma cells were obtained from American Type Culture Collection (Manassas, VA).
Peptide Synthesis and Receptor Binding Assay
DOTA-GGNle-CycMSHhex was synthesized, purified by RP-HPLC and characterized by liquid chromatography-mass spectrometry (LC-MS) according to our published procedure.24 New NOTA-GGNle-CycMSHhex was synthesized using Fmoc chemistry. Briefly, the intermediate scaffold of Fmoc-Asp(O-2-PhiPr)-His(Trt)-dPhe-Arg(Pbf)-Trp(Boc)-Lys(Mtt) was synthesized on H2N-Novagel resin by an Advanced ChemTech multiple-peptide synthesizer (Louisville, KY). Generally, 70 µmol of resin, 210 µmol of each Fmoc-protected amino acid and NO2AtBu were used for the synthesis. The protecting groups of Mtt and 2-phenylisopropyl were removed by 2.5% of trifluoroacetic acid (TFA) for peptide cyclization. The cyclization reaction was achieved on the resin by an overnight reaction in dimethylformamide (DMF) using benzotriazole-1-yl-oxy-tris-pyrrolidino-phosphonium-hexafluorophosphate (PyBOP) as a coupling agent in the presence of N,N-diisopropylethylamine (DIEA). After the cyclization, the moiety of NO2AtBu-CH2-Gly-Gly-Nle was coupled to the cyclic intermediate scaffold to yield NO2AtBu-CH2-Gly-Gly-Nle-Cyclic[Asp-His(Trt)-dPhe-Arg(Pbf)-Trp(Boc)-Lys] on the resin. All protecting groups were totally removed and the peptide was cleaved from the resin by treating with a mixture of trifluoroacetic acid (TFA), thioanisole, phenol, water, ethanedithiol and triisopropylsilane (87.5:2.5:2.5:2.5:2.5:2.5) for 2 h at 25°C. The peptide was precipitated and washed with ice-cold ether four times, purified by RP-HPLC on a Grace Vydac C-18 reverse phase analytical column (Vydac 218TP54: 5 µm, 4.6 mm i.d. × 250 mm), and characterized by LC-MS. The MC1 receptor binding affinity (IC50 value) of NOTA-GGNle-CycMSHhexwas determined in B16/F1 melanoma cells by in vitro competitive receptor binding assay according to our published procedure24 and compared with DOTA-GGNle-CycMSHhex.
Effects of Reaction Time and Temperature on 67Ga Radiolabeling Yield
NOTA can form stable complex with 67Ga at lower temperature than DOTA.28–29 To examine the effects of reaction time and temperature on radiolabeling yield, DOTA-GGNle-CycMSHhexand NOTA-GGNle-CycMSHhex were radiolabeled with 67Ga in a 0.5 M NH4OAc-buffered solution (pH 3.5) at different temperatures for different reaction time points, respectively. Briefly, 10 µL of 67GaCl3 (18.5–37.0 MBq in 0.05 M HCl), 10 µL of 1 mg/mL DOTA-GGNle-CycMSHhexor NOTA-GGNle-CycMSHhex aqueous solution and 100 µL of 0.5 M NH4OAc (pH 3.5) were added into a reaction vial and incubated at 25, 37, 45 and 75°C for 5, 15, 30 and 45 min, respectively. After the incubation, 10 µL of 0.5% EDTA aqueous solution was added into each reaction vial to bind unbound 67Ga3+. The radiolabeling yield of each peptide was determined by Waters RP-HPLC (Milford, MA) on a Grace Vadyc C-18 reverse phase analytical column (Deerfield, IL) using the following gradient at a flow rate of 1 mL/min. The mobile phase consisted of solvent A (20 mM HCl aqueous solution) and solvent B (100% CH3CN). The gradient was initiated and kept at 82:18 A/B for 3 min followed by a linear gradient of 82:18 A/B to 72:28 A/B over 20 min. Then, the gradient was changed from 72:28 A/B to 10:90 A/B over 3 min followed by an additional 5 min at 10:90 A/B. Thereafter, the gradient was changed from 10:90 A/B to 82:18 A/B over 3 min.
Biodistribution Studies
All animal studies were conducted in compliance with Institutional Animal Care and Use Committee approval. The melanoma targeting and pharmacokinetic properties of 67Ga-DOTA-GGNle-CycMSHhex and 67Ga-NOTA-GGNle-CycMSHhex were determined in B16/F1 melanoma-bearing C57 female mice (Harlan, Indianapolis, IN). The C57 mice were subcutaneously inoculated with 1 × 106 B16/F1 cells on the right flank for each mouse to generate B16/F1 tumors. The weights of tumors reached approximately 0.2 g 10 days post cell inoculation. Each melanoma-bearing mouse was injected with 0.037 MBq of 67Ga-DOTA-GGNle-CycMSHhex or 67Ga-NOTA-GGNle-CycMSHhex via the tail vein. Groups of 5 mice were sacrificed at 0.5, 2, 4 and 24 h post-injection, and tumors and organs of interest were harvested, weighed and counted. Blood values were taken as 6.5% of the whole-body weight. The specificity of tumor uptake of 67Ga-DOTA-GGNle-CycMSHhex or 67Ga-NOTA-GGNle-CycMSHhex was determined by co-injecting 10 µg (6.07 nmol) of unlabeled NDP-MSH peptide at 2 h post-injection.
Melanoma Imaging with 67Ga-NOTA-GGNle-CycMSHhex
67Ga-NOTA-GGNle-CycMSHhexexhibited more favorable radiolabeling conditions (> 85% radiolabeling yields at 37°C for 30 min), as well as higher tumor/kidney uptake ratio than 67Ga-DOTA-GGNle-CycMSHhex at 2 h post-injection. Thus, we further evaluated the melanoma imaging property of 67Ga-NOTA-GGNle-CycMSHhex. Approximately 11.1 MBq of 67Ga-NOTA-GGNle-CycMSHhex was injected into a B16/F1 melanoma-bearing mouse via the tail vein. The mouse was euthanized for small animal SPECT/CT (Nano-SPECT/CT®, Bioscan) imaging at 2 h post-injection. The CT imaging was immediately followed by single photon emission computed tomography (SPECT) imaging of whole-body. The SPECT scans of 24 projections were acquired. Reconstructed SPECT and CT data were visualized and co-registered using InVivoScope (Bioscan, Washington DC).
Statistical Analysis
Statistical analysis was performed using the Student’s t-test for unpaired data. A 95% confidence level was chosen to determine the significance of the difference in tumor and renal uptake between 67Ga-NOTA-GGNle-CycMSHhex and 67Ga-DOTA-GGNle-CycMSHhex, as well as the significance of the difference in tumor uptake between 67Ga-NOTA-GGNle-CycMSHhex with/without NDP-MSH co-injection, and between 67Ga-DOTA-GGNle-CycMSHhex with/without NDP-MSH co-injection. The differences at the 95% confidence level (p<0.05) were considered significant.
RESULTS
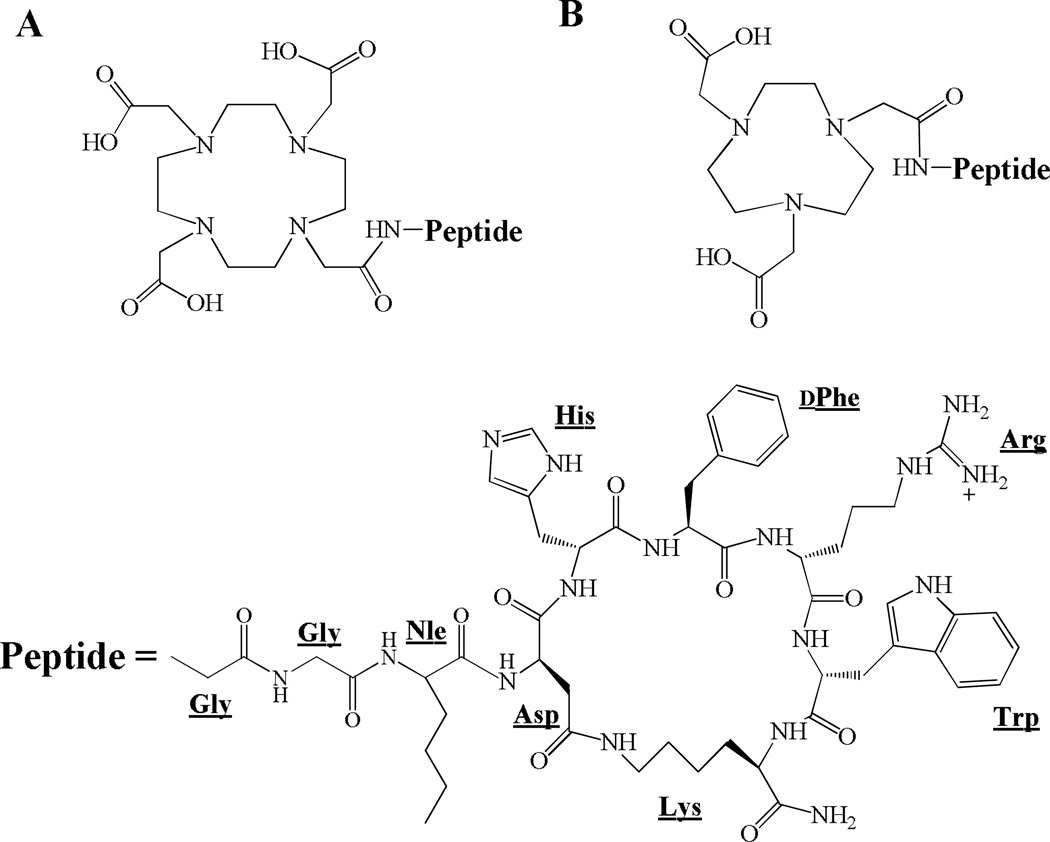
New NOTA-GGNle-CycMSHhex was synthesized and purified by RP-HPLC. NOTA-GGNle-CycMSHhex displayed greater than 90% chemical purity after HPLC purification with 30% synthetic yield. The identity of NOTA-GGNle-CycMSHhex was confirmed by electrospray ionization mass spectrometry. The calculated and found molecular weights of NOTA-GGNle-CycMSHhex were 1381 and 1381, respectively. Meanwhile, DOTA-GGNle-CycMSHhex was synthesized and characterized according to our published procedure24 for comparison. The calculated and found molecular weights of DOTA-GGNle-CycMSHhex were 1368 and 1368, respectively. The schematic structures of NOTA-GGNle-CycMSHhex and DOTA-GGNle-CycMSHhex are shown in Figure 1. The IC50 value of NOTA-GGNle-CycMSHhex was 1.6 nM in B16/F1 melanoma cells, which was comparable to that of DOTA-GGNle-CycMSHhex (2.1 nM).24
Figure 1.
Schematic structures of DOTA-GGNle-CycMSHhex (A) and NOTA-GGNle-CycMSHhex(B).
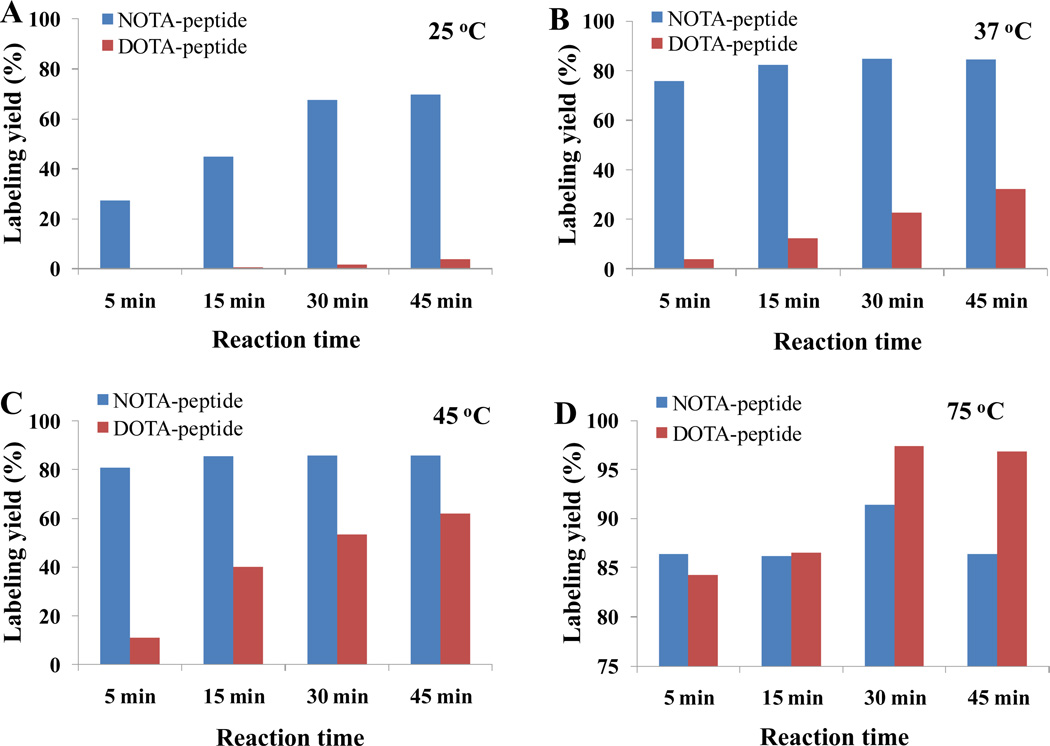
The effects of reaction time and temperature on radiolabeling yields are presented in Figure 2. The radiolabeling yield of 67Ga-DOTA-GGNle-CycMSHhex or 67Ga-NOTA-GGNle-CycMSHhex was reaction time-dependent at 25°C, 37°C, 45°C and 75°C, respectively. The radiolabeling yield improved when the reaction time prolonged from 5 min to 45 min. For instance, as showed in Figure 2 at 25°C, the radiolabeling yield of 67Ga-NOTA-GGNle-CycMSHhexwas 27% after 5 min incubation, and was 70% after 45 min incubation. Meanwhile, the time-dependent fashion was observed for 67Ga-DOTA-GGNle-CycMSHhex as well despite the fact that the radiolabeling yield of 67Ga-DOTA-GGNle-CycMSHhex was lower than 5% at 25°C even after 45 min incubation. The radiolabeling yield of 67Ga-DOTA-GGNle-CycMSHhex or 67Ga-NOTA-GGNle-CycMSHhex was reaction temperature-dependent after 5, 15, 30 and 45 min incubation, respectively. The radiolabeling yield increased when the reaction temperature elevated from 25°C to 75°C. For example, as showed in Figure 2 after 30 min incubation, the radiolabeling yield of 67Ga-NOTA-GGNle-CycMSHhexwas 67% at 25°C and was 91% at 75°C. Similarly, the radiolabeling yield of 67Ga-DOTA-GGNle-CycMSHhexwas less than 5% at 25°C and was 97% at 75°C. Overall, the radiolabeling yield of 67Ga-NOTA-GGNle-CycMSHhex could reach greater than 85% started from 37°C, whereas the radiolabeling yield of 67Ga-DOTA-GGNle-CycMSHhex could achieve greater than 84% only at 75°C. After we examined the effects of reaction time and temperature on radiolabeling yield, we performed peptide radiolabeling at 75°C for 30 min for biodistribution and imaging studies. DOTA-GGNle-CycMSHhex and NOTA-GGNle-CycMSHhex were readily labeled with 67Ga in a 0.5 M NH4OAc-buffered solution (pH 3.5) with greater than 90% radiolabeling yields. 67Ga-DOTA-GGNle-CycMSHhex and 67Ga-NOTA-GGNle-CycMSHhex were completely separated from their excess non-labeled peptides by RP-HPLC. The retention times of 67Ga-DOTA-GGNle-CycMSHhex and 67Ga-NOTA-GGNle-CycMSHhex were 16.3 and 16.4 min, respectively.
Figure 2.
Effects of reaction time and temperature on radiolabeling yields of 67Ga-DOTA-GGNle-CycMSHhex and 67Ga-NOTA-GGNle-CycMSHhex.
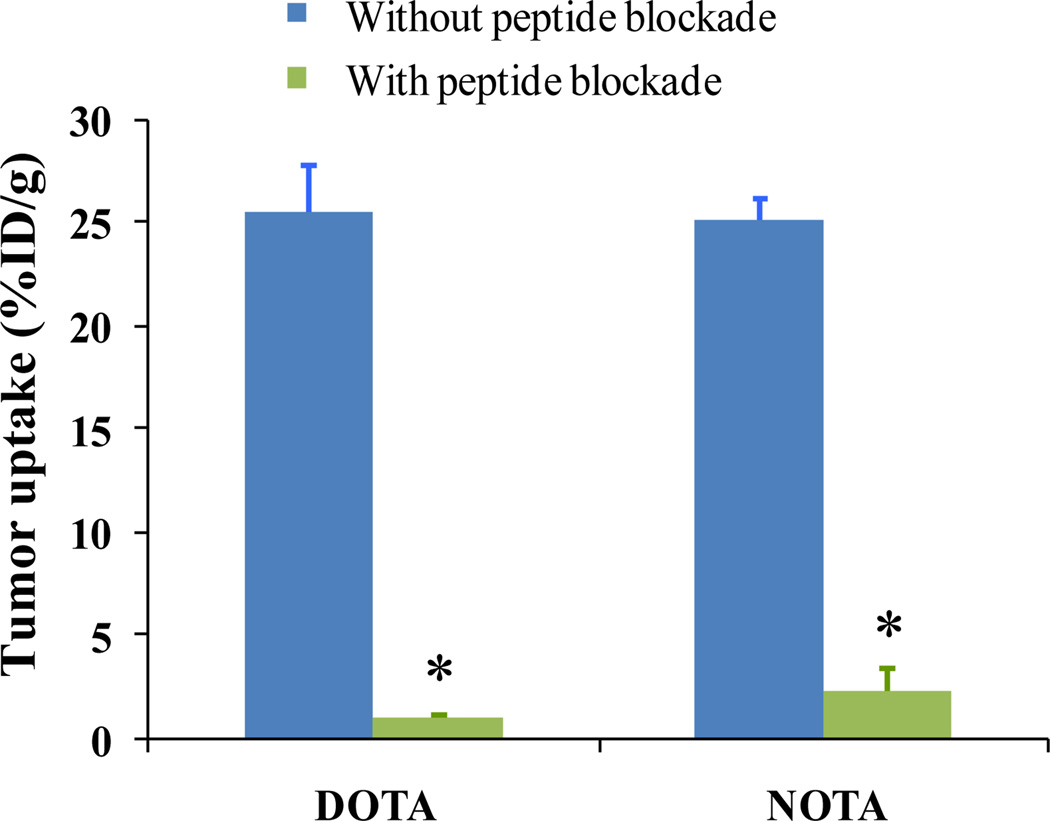
The melanoma targeting and pharmacokinetic properties of 67Ga-DOTA-GGNle-CycMSHhex and 67Ga-NOTA-GGNle-CycMSHhex were determined in B16/F1 melanoma-bearing C57 mice. The biodistribution results of 67Ga-DOTA-GGNle-CycMSHhex and 67Ga-NOTA-GGNle-CycMSHhexb are presented in Table 1. 67Ga-DOTA-GGNle-CycMSHhex exhibited rapid high melanoma uptake and prolonged tumor retention. The tumor uptake of 67Ga-DOTA-GGNle-CycMSHhex was 26.96 ± 3.82 % ID/g at 0.5 h post-injection. 67Ga-DOTA-GGNle-CycMSHhex displayed similar high tumor uptake (25.53 ± 2.22 and 25.13 ± 4.13 % ID/g) at 2 and 4 h post-injection. Even at 24 h post-injection, there was 7.54 ± 1.19 % ID/g of 67Ga-DOTA-GGNle-CycMSHhex activity remained in the tumor. Approximately 96.3% of the tumor uptake of 67Ga-DOTA-GGNle-CycMSHhex was blocked by 10 µg (6.07 nmol) of non-radiolabeled NDP-MSH (p<0.05) (Figure 3), demonstrating that the tumor uptake was specific and MC1 receptor-mediated. Whole-body clearance of 67Ga-DOTA-GGNle-CycMSHhex was rapid, with 84.9% of the injected radioactivity cleared through the urinary system by 2 h post-injection. Normal organ uptake of 67Ga-DOTA-GGNle-CycMSHhex was lower than 1.68 % ID/g except for the kidneys at 2, 4 and 24 h post-injection. The kidney uptake was 8.90 ± 1.81 % ID/g at 2 h post-injection and decreased to 5.60 ± 1.24 % ID/g at 24 h post-injection. High tumor uptake and prolonged retention coupled with rapid whole-body clearance resulted in high tumor/blood and high tumor/normal organ uptake ratios achieved as early as 0.5 h post-injection. The tumor/kidney uptake ratio of 67Ga-DOTA-GGNle-CycMSHhex was 1.64, 2.87, 2.98 and 1.35 at 0.5, 2, 4 and 24 h post-injection, respectively.
Table 1.
Biodistribution of 67Ga-DOTA-GGNle-CycMSHhex and 67Ga-NOTA-GGNle-CycMSHhex in B16/F1 melanoma-bearing C57 mice. The data were presented as percent injected dose/gram or as percent injected dose (Mean ± SD, n=5)
| 67Ga-DOTA-GGNle-CycMSHhex | 67Ga-NOTA-GGNle-CycMSHhex | |||||||
|---|---|---|---|---|---|---|---|---|
| Tissues | 0.5 h | 2 h | 4 h | 24 h | 0.5 h | 2 h | 4 h | 24 h |
| Percent injected dose/gram (%ID/g) | ||||||||
| Tumor | 26.96±3.82 | 25.53±2.22 | 25.13±4.13 | 7.54±1.19 | 20.59±1.97* | 25.12±1.03 | 18.17±4.89 | 7.95±2.58 |
| Brain | 0.25±0.07 | 0.15±0.12 | 0.08±0.03 | 0.06±0.03 | 0.21±0.01 | 0.11±0.07 | 0.08±0.03 | 0.08±0.02 |
| Blood | 3.33±1.08 | 0.97±0.91 | 0.53±0.25 | 0.29±0.05 | 2.25±0.09 | 0.40±0.19 | 1.02±0.06 | 0.55±0.12 |
| Heart | 1.64±0.18 | 0.23±0.09 | 0.24±0.04 | 0.37±0.08 | 1.52±0.28 | 0.45±0.09 | 0.39±0.17 | 0.96±0.39 |
| Lung | 3.23±0.07 | 0.40±0.15 | 0.36±0.08 | 0.32±0.19 | 3.71±0.25 | 0.54±0.04 | 0.30±0.10 | 0.35±0.08 |
| Liver | 1.82±0.13 | 0.86±0.19 | 0.85±0.02 | 0.54±0.14 | 1.28±0.14 | 0.59±0.09 | 0.54±0.05 | 0.50±0.12 |
| Spleen | 1.39±0.13 | 0.44±0.09 | 0.64±0.06 | 0.52±0.16 | 1.25±0.11 | 0.67±0.19 | 0.57±0.14 | 0.85±0.23 |
| Stomach | 2.51±0.50 | 1.68±0.50 | 1.26±0.11 | 0.62±0.23 | 1.79±0.22 | 1.62±0.63 | 1.45±0.23 | 1.21±0.40 |
| Kidneys | 16.42±2.99 | 8.90±1.81 | 8.44±0.11 | 5.60±1.24 | 11.67±0.06* | 8.34±3.25 | 7.58±2.70 | 2.74±0.64* |
| Muscle | 0.75±0.20 | 0.34±0.10 | 0.32±0.07 | 0.30±0.18 | 0.73±0.26 | 0.34±0.12 | 0.33±0.11 | 0.99±0.56 |
| Pancreas | 0.83±0.26 | 0.34±0.07 | 0.23±0.06 | 0.37±0.06 | 1.03±0.16 | 0.54±0.13 | 0.36±0.04 | 0.88±0.31 |
| Bone | 1.44±0.63 | 1.04±0.24 | 0.87±0.09 | 0.72±0.70 | 1.95±0.08 | 0.91±0.56 | 0.96±0.87 | 0.71±0.24 |
| Skin | 5.31±2.35 | 0.84±0.25 | 0.81±0.22 | 0.76±0.21 | 4.00±0.32 | 0.54±0.35 | 0.65±0.24 | 0.96±0.24 |
| Percent injected dose (%ID) | ||||||||
| Intestines | 1.60±0.30 | 1.52±1.14 | 0.98±0.18 | 0.46±0.06 | 1.86±0.24 | 1.22±0.97 | 0.91±0.05 | 1.23±0.35 |
| Urine | 59.37±5.31 | 84.91±2.81 | 87.75±1.44 | 92.72±1.09 | 54.16±13.08 | 84.02±5.71 | 86.39±3.94 | 94.57±0.25 |
| Uptake ratio of tumor/normal tissue | ||||||||
| Tumor/liver | 14.84 | 29.73 | 29.66 | 13.86 | 16.09 | 42.39 | 33.40 | 15.75 |
| Tumor/kidney | 1.64 | 2.87 | 2.98 | 1.35 | 1.76 | 3.01 | 2.40 | 2.90 |
| Tumor/lung | 8.35 | 63.55 | 69.97 | 23.35 | 5.54 | 46.37 | 60.24 | 22.52 |
| Tumor/muscle | 35.77 | 76.04 | 78.34 | 25.47 | 28.19 | 74.55 | 54.71 | 8.05 |
| Tumor/blood | 8.10 | 26.21 | 47.74 | 25.56 | 9.14 | 62.93 | 17.75 | 14.46 |
| Tumor/skin | 5.08 | 30.44 | 31.10 | 9.95 | 5.15 | 46.35 | 28.10 | 8.27 |
P<0.05 for determining significance of differences in tumor and kidney uptake between 67Ga-DOTA-GGNle-CycMSHhex and 67Ga-NOTA-GGNle-CycMSHhex at the same time point.
Figure 3.
The tumor uptake of 67Ga-DOTA-GGNle-CycMSHhex (DOTA) and 67Ga-NOTA-GGNle-CycMSHhex (NOTA) with ( ) or without (
) or without ( ) 10 µg of NDP-MSH blockade at 2 h post-injection. *p<0.05.
) 10 µg of NDP-MSH blockade at 2 h post-injection. *p<0.05.
67Ga-NOTA-GGNle-CycMSHhex showed comparable high melanoma uptake with 67Ga-DOTA-GGNle-CycMSHhex at 2 and 24 h post-injection. The tumor uptake of 67Ga-NOTA-GGNle-CycMSHhex was 20.59 ± 1.57 % ID/g at 0.5 h post-injection. 67Ga-NOTA-GGNle-CycMSHhex reached its peak tumor uptake of 25.12 ± 1.03 % ID/g at 2 h post-injection. The tumor uptake of 67Ga-NOTA-GGNle-CycMSHhex was 18.17 ± 4.89 and 7.95 ± 2.58 % ID/g at 4 and 24 h post-injection. Approximately 90.8% of the tumor uptake of 67Ga-NOTA-GGNle-CycMSHhex was blocked by 10 µg (6.07 nmol) of non-radiolabeled NDP-MSH (p<0.05) (Figure 3), demonstrating that the tumor uptake was specific and MC1 receptor-mediated. Whole-body clearance of 67Ga-NOTA-GGNle-CycMSHhex was rapid, with 84.1% of the injected radioactivity cleared through the urinary system by 2 h post-injection. Normal organ uptakes of 67Ga-NOTA-GGNle-CycMSHhex were lower than 1.62 % ID/g except for the kidneys at 2, 4 and 24 h post-injection. The kidney uptake was 8.34 ± 3.25 % ID/g at 2 h post-injection and decreased to 2.74 ± 0.64 % ID/g at 24 h post-injection. High tumor uptake and prolonged retention coupled with rapid whole-body clearance resulted in high tumor/blood and high tumor/normal organ uptake ratios achieved as early as 0.5 h post-injection. The tumor/kidney uptake ratio of 67Ga-DOTA-GGNle-CycMSHhex was 1.76, 3.01, 2.40 and 2.90 at 0.5, 2, 4 and 24 h post-injection, respectively.
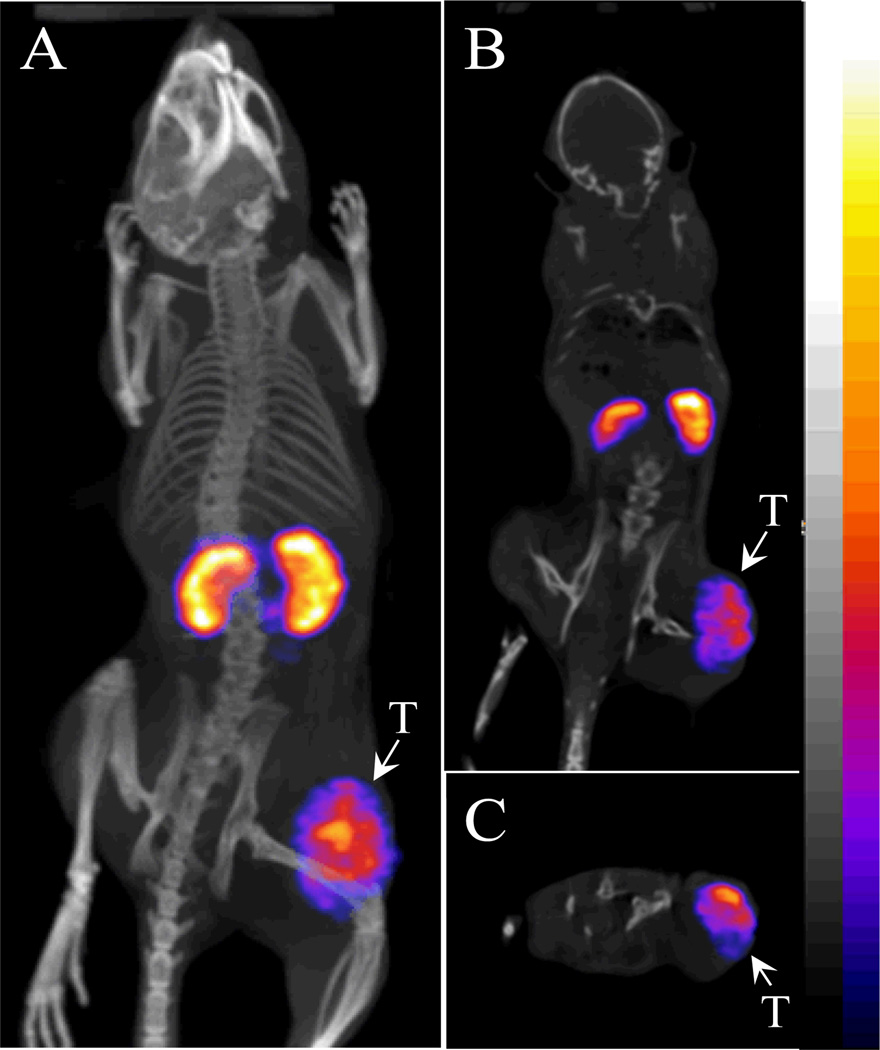
67Ga-NOTA-GGNle-CycMSHhexexhibited more favorable radiolabeling conditions (> 85% radiolabeling yields started at 37°C), as well as higher tumor/kidney uptake ratio than 67Ga-DOTA-GGNle-CycMSHhex at 2 h post-injection. Therefore, we further evaluated the melanoma imaging properties of 67Ga-NOTA-GGNle-CycMSHhex at 2 h post-injection. The whole-body, coronal and transversal SPECT/CT images are presented in Figure 5. The melanoma tumors were clearly visualized by SPECT/CT using 67Ga-NOTA-GGNle-CycMSHhex as an imaging probe. 67Ga-NOTA-GGNle-CycMSHhex exhibited high tumor to normal organ uptake ratios except for the kidneys, which was consistent with the biodistribution results.
Figure 5.
Representative whole-body (A), coronal (B) and transversal (C) SPECT/CT images of a B16/F1 melanoma-bearing C57 mouse at 2 h post-injection of 67Ga-NOTA-GGNle-CycMSHhex. The tumor lesions (T) were highlighted with arrows on the images.
DISCUSSION
Gallium-67 is an attractive SPECT radionuclide with a half-life of 78.3 h and three gamma-emissions (38% 93 keV, 24% 185 keV and 16% 300 keV) (30–33). Meanwhile, 67Ga is also a potential therapeutic radionuclide due to its emissions of Auger and conversion electrons.27 Both linear and cyclic 67Ga-labeled α-MSH peptides8,22 have been reported for melanoma imaging over the past several years. Initially, Froidevaux et al. reported the linear 67Ga-DOTA-NAPamide, which exhibited 9.43 ± 1.06 and 3.10 ± 0.36 %ID/g of B16/F1 melanoma uptake at 4 and 24 post-injection, respectively.8 Thereafter, we reported the lactam bridge-cyclized 67Ga-DOTA-GlyGlu-CycMSH.22 The B16/F1 melanoma uptake of 67Ga-DOTA-GlyGlu-CycMSH was 14% less than that of 67Ga-DOTA-NAPamide at 4 h post-injection, whereas the B16/F1 melanoma uptake of 67Ga-DOTA-GlyGlu-CycMSH was 1.6 times the melanoma uptake of 67Ga-DOTA-NAPamide at 24 h post-injection. Surprisingly, the renal uptake of 67Ga-DOTA-GlyGlu-CycMSH was 5.7 and 10.3 times the renal uptake of 67Ga-DOTA-NAPamide at 4 and 24 h post-injection, respectively. Dramatic difference in renal uptake between 67Ga-DOTA-GlyGlu-CycMSH and 67Ga-DOTA-NAPamide was likely due to their structural differences.
Recently, we have identified a novel class of lactam bridge-cyclized α-MSH peptides with enhanced melanoma uptake and reduced renal uptake.23,24 Specifically, 111In-DOTA-GGNle-CycMSHhex exhibited the highest tumor/kidney uptake ratios (2.8 and 2.7 at 2 and 4 h post-injection) among all reported 111In-labeled cyclic peptides.23,24 Thus, we were interested in determining whether or not 67Ga-DOTA-GGNle-CycMSHhex could display higher melanoma uptake and lower renal uptake compared to 67Ga-DOTA-GlyGlu-CycMSH in this study. Meanwhile, we also evaluated 67Ga-NOTA-GGNle-CycMSHhex because NOTA can also form a stable complex with 67Ga even at lower reaction temperature than DOTA.28,29 As we anticipated, NOTA-GGNle-CycMSHhex showed comparable MC1 receptor binding affinity with DOTA-GGNle-CycMSHhex (1.6 vs. 2.1 nM). In terms of radiolabeling yield, 67Ga-NOTA-GGNle-CycMSHhex could reach 70% and 85% radiolabeling yields even at 25°C and 37°C, respectively. Meanwhile, the radiolabeling yield of 67Ga-DOTA-GGNle-CycMSHhex could be greater than 85% only at 75°C. At 75°C, both 67Ga-NOTA-GGNle-CycMSHhex and 67Ga-DOTA-GGNle-CycMSHhex could achieve greater than 90% radiolabeling yield after 30 min incubation. It was important to note that high radiolabeling yield of 67Ga-NOTA-GGNle-CycMSHhexat 37°C represented a distinct practical advantage compared to 67Ga-DOTA-GGNle-CycMSHhex.
The biodistribution results supported our hypothesis. 67Ga-DOTA-GGNle-CycMSHhex exhibited higher melanoma uptake and lower renal uptake compared to 67Ga-DOTA-GlyGlu-CycMSH. The tumor uptake of 67Ga-DOTA-GGNle-CycMSHhex was 3.1, 2.0 and 3.1 times the tumor uptake of 67Ga-DOTA-GlyGlu-CycMSH at 0.5, 2 and 4 h post-injection, respectively. Meanwhile, the renal uptake of 67Ga-DOTA-GGNle-CycMSHhex was only 69%, 32%, 37% and 27% of the renal uptake of 67Ga-DOTA-GlyGlu-CycMSH at 0.5, 2, 4 and 24 h post-injection, respectively. The increased tumor uptake and decreased renal uptake dramatically improved the tumor to kidney uptake ratios of 67Ga-DOTA-GGNle-CycMSHhex at all time points investigated in this study (Table 1). The tumor to kidney uptake ratio of 67Ga-DOTA-GGNle-CycMSHhex was 4.6, 6.2, 8.3 and 5.6 times those of 67Ga-DOTA-GlyGlu-CycMSH at 0.5, 2, 4 and 24 h post-injection, respectively.
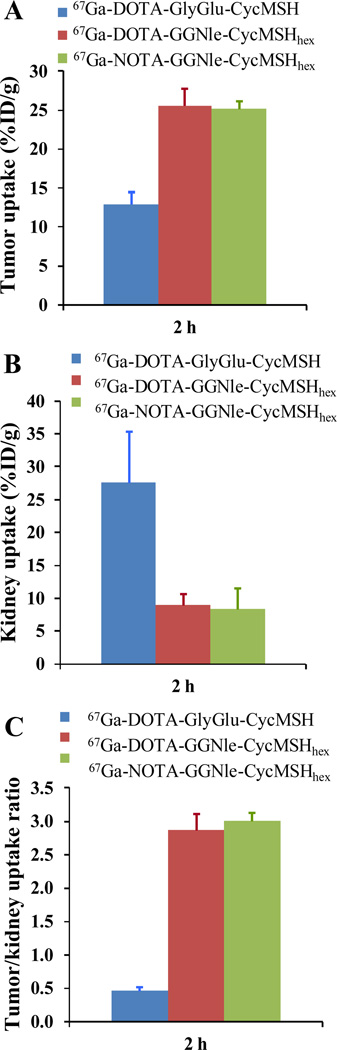
67Ga-NOTA-GGNle-CycMSHhex displayed comparable high melanoma uptake with 67Ga-DOTA-GGNle-CycMSHhex at 2 and 24 h post-injection. Meanwhile, 67Ga-NOTA-GGNle-CycMSHhex exhibited comparable renal uptake with 67Ga-DOTA-GGNle-CycMSHhex at 2 and 4 h post-injection. Interestingly, the renal uptake of with 67Ga-NOTA-GGNle-CycMSHhex was only 71% and 49% of that of 67Ga-DOTA-GGNle-CycMSHhex at 0.5 and 24 h post-injection. The further reduced renal uptake resulted in higher tumor/kidney uptake ratios of 67Ga-NOTA-GGNle-CycMSHhex than 67Ga-DOTA-GGNle-CycMSHhex at 0.5 and 24 h post-injection. Moreover, 67Ga-NOTA-GGNle-CycMSHhex showed slightly higher tumor/kidney uptake ratio than 67Ga-DOTA-GGNle-CycMSHhex at 2 h post-injection (Figure 4). We have demonstrated that L-lysine co-injection decreased the renal uptake of 67Ga-DOTA-GlyGlu-CycMSH by 69.8% at 2 h post-injection in our previous report.22 In this study, the renal uptake of 67Ga-NOTA-GGNle-CycMSHhex and 67Ga-DOTA-GGNle-CycMSHhex was only 30% and 32% of the renal uptake of 67Ga-DOTA-GlyGlu-CycMSH at 2 h post-injection (Figure 4). Dramatic difference in renal uptake among 67Ga-DOTA-GlyGlu-CycMSH, 67Ga-NOTA-GGNle-CycMSHhex and 67Ga-DOTA-GGNle-CycMSHhex was likely due to their structural differences.
Figure 4.
The comparisons of tumor (A) and kidney (B) uptake, and tumor/kidney uptake ratios (C) at 2 h post-injection among 67Ga-DOTA-GlyGlu-CycMSH ( ), 67Ga-DOTA-GGNle-CycMSHhex (
), 67Ga-DOTA-GGNle-CycMSHhex ( ) and 67Ga-NOTA-GGNle-CycMSHhex (
) and 67Ga-NOTA-GGNle-CycMSHhex ( ).
).
Despite the fact that the melanoma lesions could be visualized by SPECT/CT using 67Ga-DOTA-GlyGlu-CycMSH as an imaging probe,22 67Ga-NOTA-GGNle-CycMSHhex exhibited higher tumor imaging contrast (Figure 5) than 67Ga-DOTA-GlyGlu-CycMSH. Higher melanoma uptake coupled with lower renal uptake underscored the potential therapeutic application of 67Ga-NOTA-GGNle-CycMSHhex. It will be interesting to examine the therapeutic efficacy of 67Ga-NOTA-GGNle-CycMSHhex in melanoma-bearing mouse model taking advantage of the therapeutic properties of 67Ga in the future. Another potential application of NOTA-GGNle-CycMSHhex peptide is to develop 68Ga-NOTA-GGNle-CycMSHhex for positron emission tomography (PET) imaging of melanoma. Gallium-68 is an attractive PET radionuclide with a half-life of 68 min and can be easily obtained via an in-house commercial 68Ge-68Ga generator. The combination of 68Ga-NOTA-GGNle-CycMSHhex with PET, taking advantage of the outstanding imaging properties of PET and receptor-targeting properties of 68Ga-NOTA-GGNle-CycMSHhex, will offer an exciting opportunity for sensitive tumor-specific imaging of melanoma metastases.
In conclusion, both 67Ga-NOTA-GGNle-CycMSHhex and 67Ga-DOTA-GGNle-CycMSHhex exhibited dramatically enhanced melanoma uptake and reduced renal uptake than 67Ga-DOTA-GlyGlu-CycMSH in B16/F1 melanoma bearing C57 mice. 67Ga-NOTA-GGNle-CycMSHhexexhibited more favorable radiolabeling conditions (> 85% radiolabeling yields started at 37°C), as well as higher tumor/kidney uptake ratio than 67Ga-DOTA-GGNle-CycMSHhex at 0.5, 2 and 24 h post-injection. High melanoma uptake coupled with low renal uptake highlighted the potential of 67Ga-NOTA-GGNle-CycMSHhexfor melanoma imaging and therapy.
ACKNOWLEDGMENTS
We thank Dr. Jianquan Yang for his technical assistance. This work was supported in part by the NIH grant NM-INBRE P20RR016480/P20GM103451 and University of New Mexico HSC RAC Award. The image in this article was generated by the Keck-UNM Small Animal Imaging Resource established with funding from the W.M. Keck Foundation and the University of New Mexico Cancer Research and Treatment Center (NIH P30 CA118100).
REFERENCES
- 1.Giblin MF, Wang NN, Hoffman TJ, Jurisson SS, Quinn TP. Design and characterization of α-melanotropin peptide analogs cyclized through rhenium and technetium metal coordination. Proc. Natl. Acad. Sci. U.S.A. 1998;95:12814–12818. doi: 10.1073/pnas.95.22.12814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen J, Cheng Z, Hoffman TJ, Jurisson SS, Quinn TP. Melanoma-targeting properties of 99mtechnetium-labeled cyclic alpha-melanocyte-stimulating hormone peptide analogues. Cancer Res. 2000;60:5649–5658. [PubMed] [Google Scholar]
- 3.Chen J, Cheng Z, Owen NK, Hoffman TJ, Miao Y, Jurisson SS, Quinn TP. Evaluation of an 111In-DOTA-rhenium cyclized alpha-MSH analog: a novel cyclic-peptide analog with improved tumor-targeting properties. J. Nucl. Med. 2001;42:1847–1855. [PubMed] [Google Scholar]
- 4.Miao Y, Owen NK, Whitener D, Gallazzi F, Hoffman TJ, Quinn TP. In vivo evaluation of 188Re-labeled alpha-melanocyte stimulating hormone peptide analogs for melanoma therapy. Int. J. Cancer. 2002;101:480–487. doi: 10.1002/ijc.10640. [DOI] [PubMed] [Google Scholar]
- 5.Froidevaux S, Calame-Christe M, Tanner H, Sumanovski L, Eberle AN. A novel DOTA-alpha-melanocyte-stimulating hormone analog for metastatic melanoma diagnosis. J. Nucl. Med. 2002;43:1699–1706. [PubMed] [Google Scholar]
- 6.Cheng Z, Chen J, Miao Y, Owen NK, Quinn TP, Jurisson SS. Modification of the structure of a metallopeptide: synthesis and biological evaluation of 111In-labeled DOTA-conjugated rhenium-cyclized alpha-MSH analogues. J. Med. Chem. 2002;45:3048–3056. doi: 10.1021/jm010408m. [DOI] [PubMed] [Google Scholar]
- 7.Miao Y, Whitener D, Feng W, Owen NK, Chen J, Quinn TP. Evaluation of the human melanoma targeting properties of radiolabeled alpha-melanocyte stimulating hormone peptide analogues. Bioconjug. Chem. 2003;14:1177–1184. doi: 10.1021/bc034069i. [DOI] [PubMed] [Google Scholar]
- 8.Froidevaux S, Calame-Christe M, Schuhmacher J, Tanner H, Saffrich R, Henze M, Eberle AN. A gallium-labeled DOTA-alpha-melanocyte-stimulating hormone analog for PET imaging of melanoma metastases. J. Nucl. Med. 2004;45:116–123. [PubMed] [Google Scholar]
- 9.Miao Y, Owen NK, Fisher DR, Hoffman TJ, Quinn TP. Therapeutic efficacy of a 188Re-labeled alpha-melanocyte-stimulating hormone peptide analog in murine and human melanoma-bearing mouse models. J. Nucl. Med. 2005;46:121–129. [PubMed] [Google Scholar]
- 10.Froidevaux S, Calame-Christe M, Tanner H, Eberle AN. Melanoma targeting with DOTA-alpha-melanocyte-stimulating hormone analogs: structural parameters affecting tumor uptake and kidney uptake. J. Nucl. Med. 2005;46:887–895. [PubMed] [Google Scholar]
- 11.Miao Y, Hylarides M, Fisher DR, Shelton T, Moore H, Wester DW, Fritzberg AR, Winkelmann CT, Hoffman TJ, Quinn TP. Melanoma therapy via peptide-targeted alpha-radiation. Clin. Cancer Res. 2005;11:5616–5621. doi: 10.1158/1078-0432.CCR-05-0619. [DOI] [PubMed] [Google Scholar]
- 12.McQuade P, Miao Y, Yoo J, Quinn TP, Welch MJ, Lewis JS. Imaging of melanoma using 64Cu- and 86Y-DOTA-ReCCMSH(Arg11), a cyclized peptide analogue of alpha-MSH. J. Med. Chem. 2005;48:2985–2992. doi: 10.1021/jm0490282. [DOI] [PubMed] [Google Scholar]
- 13.Miao Y, Hoffman TJ, Quinn TP. Tumor-targeting properties of 90Y- and 177Lu-labeled α-melanocyte stimulating hormone peptide analogues in a murine melanoma model. Nucl. Med. Biol. 2005;32:485–493. doi: 10.1016/j.nucmedbio.2005.03.007. [DOI] [PubMed] [Google Scholar]
- 14.Miao Y, Fisher DR, Quinn TP. Reducing renal uptake of 90Y and 177Lu labeled alpha-melanocyte stimulating hormone peptide analogues. Nucl. Med. Biol. 2006;33:723–733. doi: 10.1016/j.nucmedbio.2006.06.005. [DOI] [PubMed] [Google Scholar]
- 15.Wei L, Butcher C, Miao Y, Gallazzi F, Quinn TP, Welch MJ, Lewis JS. Synthesis and biologic evaluation of 64Cu-labeled rhenium-cyclized alpha-MSH peptide analog using a cross-bridged cyclam chelator. J. Nucl. Med. 2007;48:64–72. [PubMed] [Google Scholar]
- 16.Cheng Z, Xiong Z, Subbarayan M, Chen X, Gambhir SS. 64Cu-labeled alpha-melanocyte-stimulating hormone analog for MicroPET imaging of melanocortin 1 receptor expression. Bioconjug. Chem. 2007;18:765–772. doi: 10.1021/bc060306g. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Miao Y, Benwell K, Quinn TP. 99mTc- and 111In-labeled alpha-melanocyte-stimulating hormone peptides as imaging probes for primary and pulmonary metastatic melanoma detection. J. Nucl. Med. 2007;48:73–80. [PubMed] [Google Scholar]
- 18.Miao Y, Shelton T, Quinn TP. Therapeutic efficacy of a 177Lu-labeled DOTA conjugated alpha-melanocyte-stimulating hormone peptide in a murine melanoma-bearing mouse model. Cancer Biother. Radiopharm. 2007;22:333–341. doi: 10.1089/cbr.2007.376.A. [DOI] [PubMed] [Google Scholar]
- 19.Miao Y, Gallazzi F, Guo H, Quinn TP. 111In-labeled lactam bridge-cyclized alpha-melanocyte stimulating hormone peptide analogues for melanoma imaging. Bioconjug. Chem. 2008;19:539–547. doi: 10.1021/bc700317w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Guo H, Shenoy N, Gershman BM, Yang J, Sklar LA, Miao Y. Metastatic melanoma imaging with an 111In-labeled lactam bridge-cyclized alpha-melanocyte-stimulating hormone peptide. Nucl. Med. Biol. 2009;36:267–276. doi: 10.1016/j.nucmedbio.2009.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Guo H, Yang J, Gallazzi F, Prossnitz ER, Sklar LA, Miao Y. Effect of DOTA position on melanoma targeting and pharmacokinetic properties of 111In-labeled lactam bridge-cyclized α-melanocyte stimulating hormone peptide. Bioconjug. Chem. 2009;20:2162–2168. doi: 10.1021/bc9003475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Guo H, Yang J, Shenoy N, Miao Y. Gallium-67-labeled lactam bridge-cyclized alpha-melanocyte stimulating hormone peptide for primary and metastatic melanoma imaging. Bioconjug. Chem. 2009;20:2356–2363. doi: 10.1021/bc900428x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Guo H, Yang J, Gallazzi F, Miao Y. Reduction of the ring size of radiolabeled lactam bridge-cyclized alpha-MSH peptide resulting in enhanced melanoma uptake. J. Nucl. Med. 2010;51:418–426. doi: 10.2967/jnumed.109.071787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Guo H, Yang J, Gallazzi F, Miao Y. Effects of the amino acid linkers on melanoma-targeting and pharmacokinetic properties of Indium-111-labeled lactam bridge-cyclized α-MSH peptides. J. Nucl. Med. 2011;52:608–616. doi: 10.2967/jnumed.110.086009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Raposinho PD, Xavier C, Correia JD, Falcao S, Gomes P, Santos I. Melanoma targeting with alpha-melanocyte stimulating hormone analogs labeled with fac-[99mTc(CO)3]+: effect of cyclization on tumor-seeking properties. J. Biol. Inorg. Chem. 2008;13:449–459. doi: 10.1007/s00775-007-0338-3. [DOI] [PubMed] [Google Scholar]
- 26.Raposinho PD, Correia JD, Alves S, Botelho MF, Santos AC, Santos I. A 99mTc(CO)3-labeled pyrazolyl–α-melanocyte-stimulating hormone analog conjugate for melanoma targeting. Nucl. Med. Biol. 2008;35:91–99. doi: 10.1016/j.nucmedbio.2007.08.001. [DOI] [PubMed] [Google Scholar]
- 27.Mariani G, Bodei L, Adelstein SJ, Kassis AI. Emerging roles for radiometabolic therapy of tumors based on auger electron emission. J. Nucl. Med. 2000;41:1519–1521. [PubMed] [Google Scholar]
- 28.Clarke ET, Martell AE. Stabilities of trivalent metal ion complexes of the tetraacetate derivatives of 12-, 13-, and 14-membered tetraazamacrocycles. Inorg. Chim. Acta. 1991;190:37–46. [Google Scholar]
- 29.Clarke ET, Martell AE. Stabilities of the Fe(III), Ga(III) and In(III) chelators of N,N’,N”-triazacyclononanetriacetic acid. Inorg. Chim. Acta. 1991;181:273–280. [Google Scholar]
- 30.Green MA, Welch MJ. Gallium radiopharmaceutical chemistry. Int. J. Rad. Appl. Instrum. B. 1989;16:435–448. doi: 10.1016/0883-2897(89)90053-6. [DOI] [PubMed] [Google Scholar]
- 31.Anderson CJ, Welch MJ. Radiometal-labeled agents (non-technetium) for diagnostic imaging. Chem. Rev. 1999;99:2219–2234. doi: 10.1021/cr980451q. [DOI] [PubMed] [Google Scholar]
- 32.Eisenwiener K, Prata MI, Buschmann I, Zhang HW, Santos AC, Wenger S, Reubi JC, Mäecke HR. NODAGATOC, a new chelator-coupled somatostatin analogue labeled with [67/68Ga] and [111In] for SPECT, PET, and targeted therapeutic applications of somatostatin receptor (hsst2) expression tumors. Bioconjug. Chem. 2002;13:530–541. doi: 10.1021/bc010074f. [DOI] [PubMed] [Google Scholar]
- 33.Zhernosekov K, Aschoff P, Filosofov D, Jahn M, Jennewein M, Adrian HJ, Bihl H, Rösch F. Visualisation of a somatostatin receptor-expressing tumour with 67Ga-DOTATOC SPECT. Eur. J. Nucl. Med. Mol. Imaging. 2005;32:1129. doi: 10.1007/s00259-005-1864-2. [DOI] [PubMed] [Google Scholar]