Abstract
To investigate the involvement of oxidative stress in the pathogenesis of osteoarthritis (OA), we evaluated the relationship between oxidative stress and articular cartilage degradation by measuring the serum levels of malondialdehyde (MDA, an oxidative stress marker), CTX-II (a type II collagen degradation marker) and CPII (a type II collagen synthesis marker) in obese and hyperlipidemic STR/Ort (STR) and control CBA mice. Seven-week-old osteoarthritic STR male mice (n=10) and control CBA male mice (n=10) were fed standard laboratory food ad libitum. At 35 weeks of age, the mice were sacrificed, and the serum levels of MDA, CTX-II and CPII were determined. Furthermore, histopathological changes were evaluated in the knee joints. Most of the STR mice spontaneously developed OA (18 of the 20 knees). By contrast, the CBA mice developed OA in only 4 of the 20 knees. Importantly, the serum levels of MDA, CTX-II and CPII were elevated to a greater extent in the STR mice compared to levels in the CBA mice. Notably, the level of MDA was correlated with that of CTX-II, but not of CPII. Moreover, the MDA levels were significantly correlated with the serum lipid (total cholesterol and triglyceride) levels as well as body weight. Together these observations suggest that oxidative stress is likely involved in the degradation of type II collagen in articular cartilage, thereby possibly contributing to the development of OA in obese and hyperlipidemic STR mice.
Keywords: oxidative stress, osteoarthritis, STR/Ort, type II collagen, biomarkers
Introduction
Osteoarthritis (OA) is a chronic joint disease characterized by degeneration of the articular cartilage, sclerosis of subchondral bone and osteophyte formation. The incidence of OA increases during every decade of life and by the age of 65 years, almost one-third of the population develops OA of the knee joints (1). Degeneration of articular cartilage is accompanied by chronic pain and significant disability in OA. However, at present no treatment is available which prevents or cures OA. Various factors, including obesity, previous injury and lifestyle, have been related to the pathogenesis of OA. Current concepts of the pathogenic mechanisms of OA suggest a shift in the homeostatic balance between the destruction and synthesis of bone and cartilage (2). Notably, previous studies have indicated the involvement of oxidative stress in the pathogenesis and progression of OA (3).
Oxidative stress is the disturbance in the state of equilibrium of pro-oxidant and anti-oxidant systems in cells and tissues (4,5). Since Harman proposed the promotion of aging by oxidative stress in 1956 (6), the association between oxidative stress and various diseases, such as cancer, diabetes mellitus and hypertension, has been elucidated. Reactive oxygen species (ROS) are highly reactive transient chemical substances, which include nitric oxide, superoxide anion, hydrogen peroxide and hydroxy radical, with the potential to initiate cellular damage by acting on molecules, such as proteins, lipids and nucleic acids. Furthermore, lipid peroxides, i.e., polyunsaturated fatty acids peroxidized by ROS, have also been shown to induce tissue injury (7). Several studies have demonstrated that oxidative damage, due to overproduced ROS from superoxide, may be involved in the pathogenesis of OA (8,9). In this regard, it has been reported that oxidative stress leads to structural and functional changes in chondrocytes and extracellular matrix, when ROS production exceeds the anti-oxidant capacities (3,10,11).
A number of animal models have been developed to investigate the pathology of OA. In STR/Ort (STR) mice, ∼85% of males spontaneously develop the degeneration of knee cartilage from 25 to 35 weeks of age. These pathological changes are closely similar to those in human OA, such as joint space narrowing, subchondral bone sclerosis and osteophyte formation. In STR mice, visceral fat is accumulated in their peritoneal cavities and they are slightly obese. Moreover, STR mice exhibit human hyperlipidemic patient-like symptoms, such as hypercholesterolemia, hypertriglyceridemia, hyperinsulinemia, insulin resistance, dysregulation of nonesterified fatty acids and low serum adiponectin (12).
In this study, to investigate the involvement of oxidative stress in the pathogenesis of OA, we evaluated the relationship between oxidative stress and articular cartilage degradation by measuring the serum levels of biomarkers, such as malondialdehyde (MDA; an oxidative stress marker), CTX-II (a type II collagen degradation marker) and CPII (a type II collagen synthesis marker) in osteoarthritic STR and control CBA mice.
Materials and methods
Animals
All procedures were carried out according to the institutional Animal Care and Committee Guide of Juntendo University School of Medicine. In this study, 7-week-old osteoarthritic STR male mice weighing ∼27 g (n=10) and 7-week-old control CBA male mice weighing ∼26 g (n=10) were purchased from Charles River Japan (Yokohama, Japan). Five mice per cage were housed under a specific pathogen-free condition (controlled temperature of 24±3°C and humidity of 55±15%) and fed standard laboratory food ad libitum. All mice were measured for body weight using a scale every week. All mice were sacrificed at 35 weeks of age.
Tissue preparation and histopathological examination
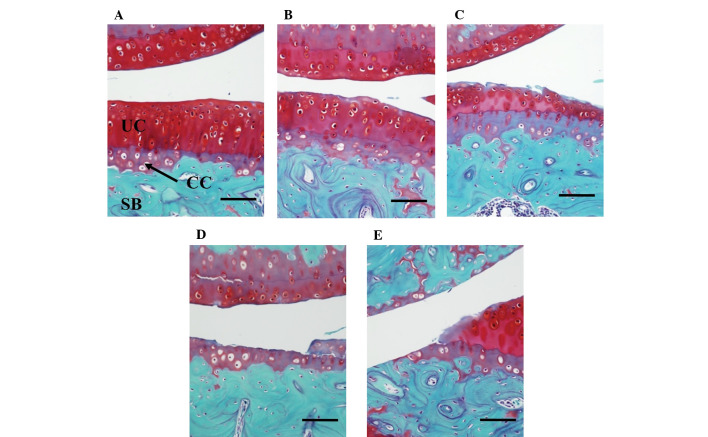
Histopathological changes were evaluated on the sagittal sections of cartilage in the weight-bearing area of the medial tibiofemoral compartment. The whole knee joint samples were dissected and fixed in 10% formalin for 24 h. They were then decalcificated by Gooding and Stewart’s fluid (equal volume of 10% formalin and 10% formic acid solution) and embedded in paraffin. Sections (5 μm) were stained with Safranin O. Grading of OA progression in the medial tibiofemoral compartment was performed according to the procedure previously described (13,14) (grade 0, no apparent change; grade 1, superficial fibrillation of articular cartilage; grade 2, defects limited to uncalcified cartilage; grade 3, defects extending into calcified cartilage; grade 4, exposure of subchondral bone at the articular surface) (Fig. 1). In this study, histopathological changes with grade 1 or more were considered to be OA.
Figure 1.
Histopathological grading of articular cartilage in STR mice. The sagittal sections of cartilage in the weight-bearing area of the medial tibiofemoral compartment were stained with Safranin O. The severity of the OA lesion was graded on a scale of 0–4 according to the procedure previously described (13,14). (A) Grade 0, no apparent changes; (B) grade 1, superficial fibrillation of articular cartilage; (C) grade 2, defects limited to uncalcified cartilage; (D) grade 3, defects extending into calcified cartilage; (E) grade 4, exposure of subchondral bone. Scale bar, 500 μm; CC, calcified cartilage; UC, uncalcified cartilage; SB, subchondral bone.
Assays of type II collagen degradation/synthesis markers and malondialdehyde
Blood was obtained from the heart of the mice at 35 weeks of age, and sera were stored in aliquots at −80°C. Serum CTX-II (15) was assayed with a serum Pre-Clinical CartiLaps ELISA kit (Nordic Bioscience Diagnostic A/S, Herlev, Denmark), which detects C-telopeptide degradation products of type II collagen (CTX-II) in the sera. By contrast, serum CPII (15) was assayed with a Procollagen type II C-propeptide ELISA kit (IBEX Technologies Inc., Montreal, Canada), which detects carboxy propeptide of type II collagen (C-propeptide, also referred to as CPII) in the sera. CPII is cleaved from type II procollagen during the processing of newly synthesized procollagen and thus can be used as a type II collagen-synthesis marker.
Serum MDA was assayed with a TBARS Assay kit (Cayman Chemical Company, USA). MDA is a naturally occurring product of lipid peroxidation (16,17).
Assay of the serum concentrations of total cholesterol and triglyceride
The serum concentrations of total cholesterol and triglyceride were measured using Cholesterol E and L-Type Triglyceride M (Wako Pure Chemical Industries, Ltd., Osaka, Japan), respectively.
Statistical analyses
Data are presented as the mean ± SD and were analyzed for significant differences using the Student’s t-test (StatView 5.0 program; SAS Institute Inc., NC, USA). Correlation analysis was also performed with the StatView 5.0 program. A p-value of <0.05 was considered to be statistically significant.
Results
Evaluation of body weight and serum levels of total cholesterol and triglyceride
During the experimental periods, the body weight of STR mice was consistently higher compared to that of the CBA mice (p<0.05) (Fig. 2A). Moreover, the serum levels of total cholesterol and triglyceride were significantly higher in the obese STR mice compared with levels in the control CBA mice (Fig. 2B and C).
Figure 2.
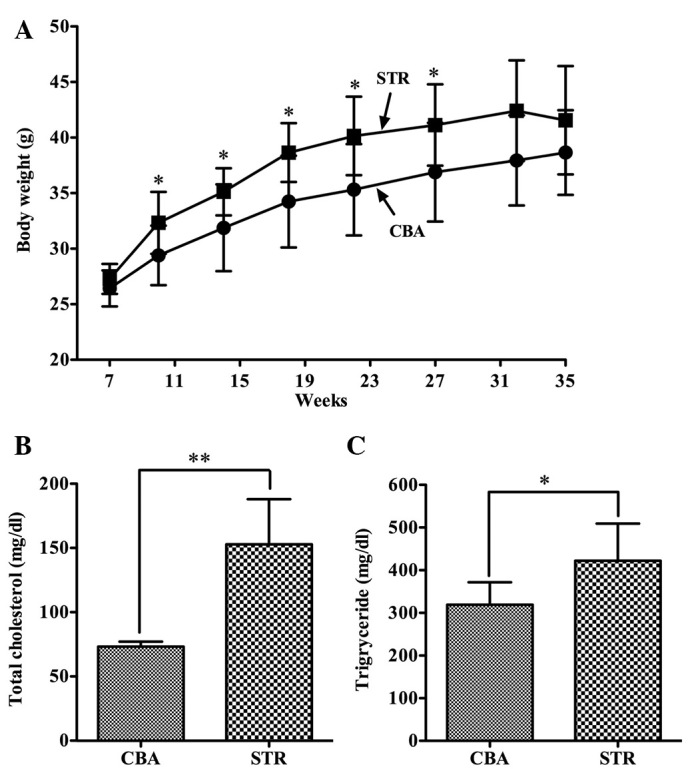
Body weight change and serum levels of total cholesterol and triglyceride in STR and CBA mice. Body weight change (A) during experimental periods and serum levels of total cholesterol (B) and triglyceride (C) at 35 weeks of age were compared between STR and CBA mice. Data represent the mean ± SD of ten animals in each group. *p<0.05, **p<0.01.
Evaluation of histopathological changes in articular cartilage
STR mice spontaneously developed OA in 18 of the 20 knees at 35 weeks (grade 0, 2 knees; grade 1, 6 knees; grade 2, 3 knees; grade 3, 3 knees; grade 4, 6 knees) (Table I). By contrast, control CBA mice developed OA only in 4 of the 20 knees (grade 0, 16 knees; grade 1, 2 knees; grade 2, 0 knee; grade 3, 1 knee; grade 4, 1 knee).
Table I.
Histopahological grading of cartilage degradation in CBA and STR mice.
| Histpathological grade | CBA mice (20 knees/10 mice) | STR mice (20 knees/10 mice) |
|---|---|---|
| 0 | 16 | 2 |
| 1 | 2 | 6 |
| 2 | 0 | 3 |
| 3 | 1 | 3 |
| 4 | 1 | 6 |
Histpathological changes with grade 1 or more were considered to be OA.
Evaluation of type II collagen degradation/synthesis and oxidative stress markers
The levels of CTX-II were 29.51±16.98 pg/ml in the STR mice and 20.04±11.74 pg/ml in the CBA mice at 35 weeks and were slightly higher in the STR mice than in the CBA mice (p=0.22) (Fig. 3A). Furthermore, the levels of CPII were 1478.56±835.75 pg/ml in the STR mice and 621.45±277.7 pg/ml in the CBA mice at 35 weeks, and were significantly elevated in the STR mice compared to levels in the CBA mice (p<0.05) (Fig. 3B).
Figure 3.
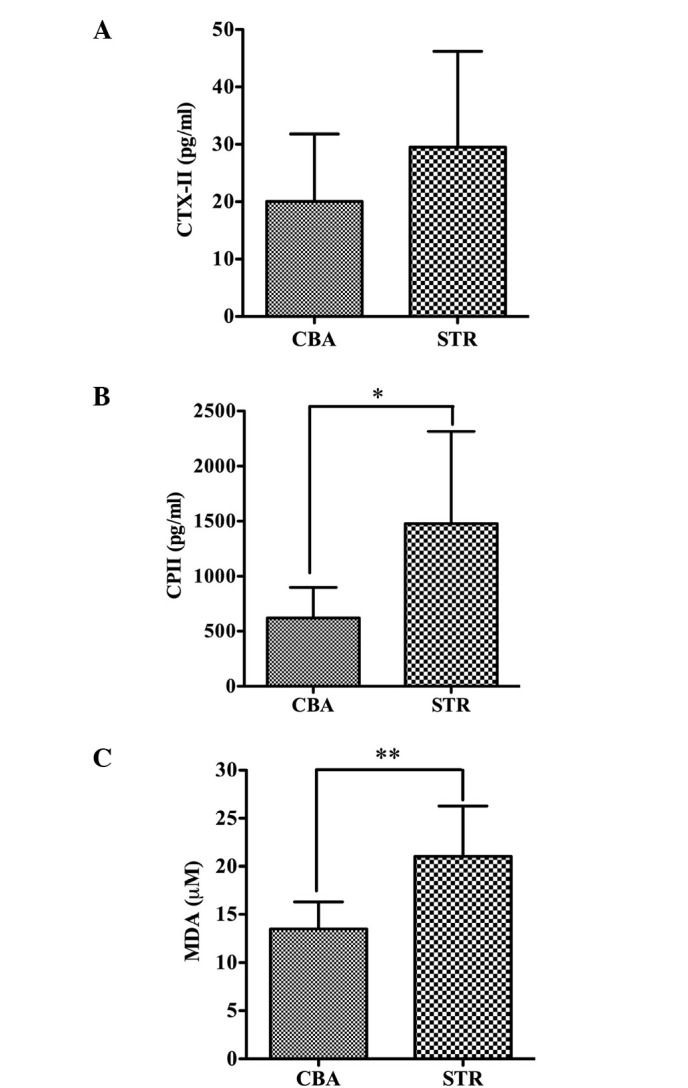
Serum levels of CTX-II, CPII and MDA in STR and CBA mice. CTX-II (A), CPII (B) and MDA (C) at 35 weeks of age were compared between STR and CBA mice. Data represent the mean ± SD of ten animals in each group. *p<0.05, **p<0.01.
Importantly, the levels of MDA were 21.04±5.23 μM in the STR/Ort mice and 13.48±5.23 μM in the CBA mice at 35 weeks, and were significantly higher in the STR mice than levels in the CBA mice (p<0.01) (Fig. 3C).
Correlation analysis of the biomarkers for oxidative stress and type II collagen metabolism
To evaluate the effect of oxidative stress on type II collagen metabolism, correlation analysis was performed between the levels of serum MDA and CTX-II or CPII at 35 weeks of age in the CBA and STR mice. Notably, the MDA levels were correlated with the CTX-II levels (r=0.55, p<0.05) (Fig. 4A); however, the MDA levels were not correlated with the CP-II levels (r=−0.06, p=0.81) (Fig. 4B). These observations indicate that oxidative stress (the elevation of MDA levels) is associated with the degradation, but not the synthesis of type II collagen in articular cartilage, and that the levels of CTX-II and CPII are unlikely to be changed in parallel within the body, although the levels of both type II collagen degradation and synthesis markers (CTX-II and CPII, respectively) are elevated in osteoarthritic STR mice (Fig. 3A and B). To test the latter possibility, the correlation between CTX-II and CPII levels was analyzed. As expected, there was no significant correlation between the two parameters (r=0.003, p=0.99) (Fig. 4C).
Figure 4.
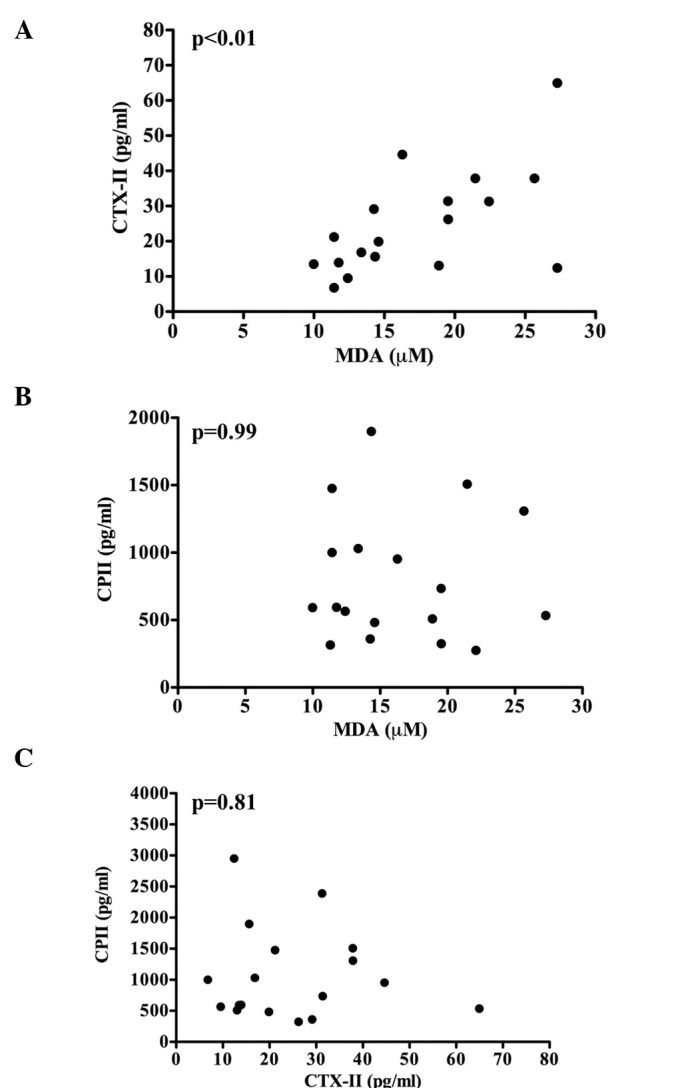
Correlation analysis of CTX-II, CPII and MDA in CTR and CBA mice. Correlation analysis was performed between CTX-II and MDA (A), CPII and MDA (B), and CPII and CTX-II (C), using serum samples from STR and CBA mice. P-values are indicated in the panels.
Correlation analysis of oxidative stress and serum lipids
A higher level of MDA in the obese and hyperlipidemic STR mice (Fig. 2B and C) suggests a possibility that the MDA levels may be associated with serum lipid levels. To test this, we analyzed the correlation between the serum levels of MDA and total cholesterol or triglyceride. As expected, there was a significant correlation between serum MDA and lipid (total cholesterol or triglyceride) levels (r=0.63, p<0.01 and r=0.53, p<0.05, respectively) (Fig. 5A and B). Importantly, there was also a significant correlation between MDA levels and body weight (r=0.47, p<0.05) (Fig. 5C).
Figure 5.
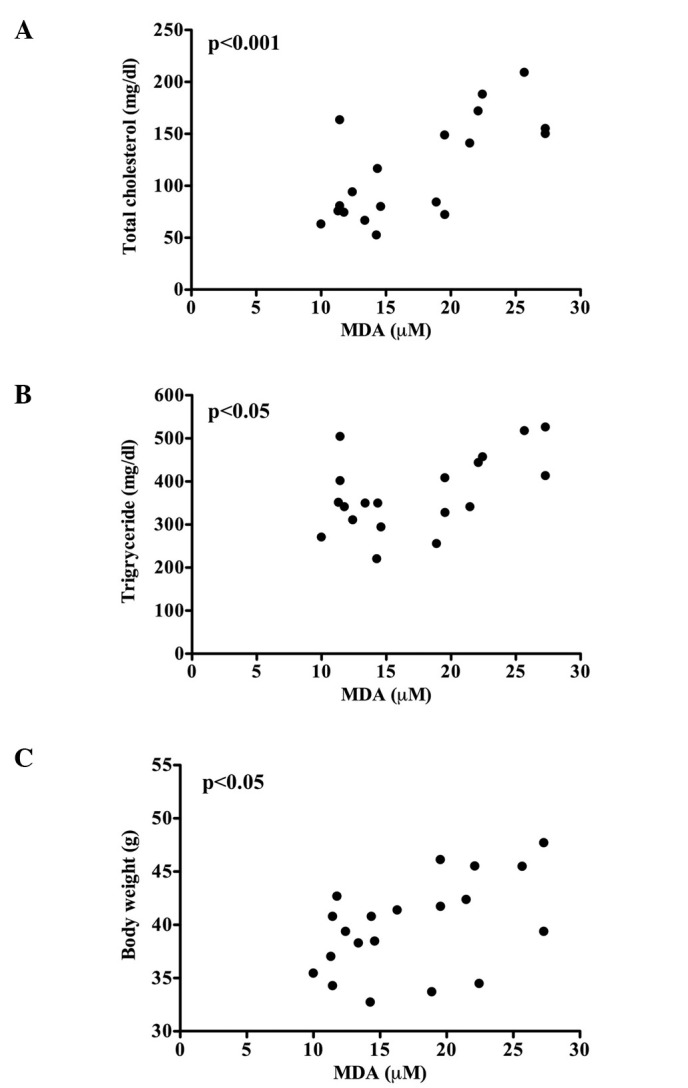
Correlation analysis of the serum levels of total cholesterol, triglyceride and MDA in STR and CBA mice. Correlation analysis was performed between total cholesterol and MDA (A) and triglyceride and MDA (B), using serum samples from STR and CBA mice. Correlation analysis was also performed between body weight and the serum levels of MDA (C). P-values are shown in the panels.
Discussion
Oxidative stress induces tissue injury via the production of ROS. Among biomolecules, lipids are particularly susceptible to oxidation and are transformed into lipid peroxides by oxidation. The accumulated lipid peroxides are involved, not only in tissue injury, but also in the development and progression of various diseases, such as lifestyle-related diseases (atherosclerosis, diabetes mellitus, dementia and cancer) (18,19). In addition, ROS are capable of inducing apoptotic cell death in chondrocytes and, more importantly, they induce the degradation of aggrecan and collagen in articular cartilage (20,21). In this context, it has been reported that chondrocyte-derived ROS mediate degradation of aggrecan and that various antioxidants prevent the degradation process (22). Together these observations suggest that oxidative stress is involved in the pathogenesis and progression of OA via the degradation of articular cartilage components.
MDA is a toxic aldehyde end-product of lipid peroxidation, which functions as a key molecule for cellular injury in both plants and animals. Thus, MDA is widely used as an indicator of oxidative stress in cells and tissues (16,17). Furthermore, MDA has been demonstrated to mediate the oxidative degradation of cartilage collagen (23).
Type II collagen is a major constituent of articular cartilage, representing 90–95% of the total collagen content and forming the fibrillar structure that gives cartilage its tensile strength (24). Among several reported biomarkers (15), components of type II collagen are recognized as the most important biomarkers for OA (25). Actually, it has been reported that CTX-II levels in patients with knee OA are significantly higher compared to levels in non-OA controls (26). Moreover, correlations have been shown between the CTX-II levels and the stage of OA (26–28), the radiographic changes of OA (29,30), or the knee pain in symptomatic OA (31). Thus, CTX-II is considered to be a reliable marker of cartilage degradation. Furthermore, it has been suggested that abnormalities in the metabolism (degradation and synthesis) of type II collagen play a key role in the pathogenesis of OA (32), and that the C-propeptide of type II procollagen (CPII), released extracellularly from the newly synthesized molecule, is directly related to type II collagen synthesis in healthy and osteoarthritic articular cartilages (33). Thus, we utilized CPII as a type II collagen synthesis marker.
Male STR mice spontaneously develop knee OA via the degeneration of cartilage. Their pathological changes are comparable to those in human OA. STR mice are slightly obese, and visceral fat is accumulated in their peritoneal cavities. Moreover, STR mice exhibit hypercholesterolemia, hypertriglyceridemia, hyperinsulinemia, insulin resistance, dysregulation of nonesterified fatty acids and low serum adiponectin, as in human hyperlipidemic patients. Thus, STR mice can be used as a model for investigating the involvement of dyslipidemia in the underlying mechanism for OA (12).
In the present study, we revealed that the body weight was significantly higher in the STR mice compared to that of the control CBA mice during almost the entire experimental period (Fig. 2A), and that total cholesterol and triglyceride levels were also significantly higher in the STR mice than those in the control CBA mice (Fig. 2B and C). Furthermore, the level of MDA, an oxidative stress marker, was significantly higher in the STR mice than that in the CBA mice (Fig. 3C). To date, large scale clinical studies, such as the Framingham Study, have indicated a correlation between body mass index and the urinary 8-epi-prostaglandin-F2α level (a parameter of oxidative stress), an increase in the oxidative stress level due to obesity (34) and a close association between visceral fat accumulation (metabolic syndrome) and oxidative stress (35).
Based on these findings, our observations strongly suggest that the oxidative stress level is higher in obese and hyperlipidemic STR mice than in CBA mice. In fact, there was a significant correlation between serum MDA and total cholesterol, triglyceride or body weight (Fig. 5A–C). Moreover, the level of CTX-II, a type II collagen degradation marker, was higher in the STR mice than in the CBA mice (Fig. 3A), and histopathological evaluation demonstrated spontaneous development of OA in the STR mice. In addition, there was a significant correlation between serum MDA and CTX-II levels (Fig. 4A). Together these observations indicate that oxidative stress is involved in the degradation of type II collagen in articular cartilage, thereby possibly promoting the development of OA in obese and hyperlipidemic STR mice. To note, the level of CPII, a type II collagen synthesis marker, was significantly increased in the osteoarthritic STR mice compared to that of the control CBA mice (Fig. 4B), although oxidative stress has been reported to suppress collagen synthesis (36). Since the synthesis of type II collagen has been reported to increase in OA (33), the higher level of CPII in the STR mice may indicate a compensatory increase in type II collagen synthesis during the process of cartilage degradation. The present finding that oxidative stress is possibly associated with type II collagen degradation provides a novel insight into the pathogenesis of secondary OA, which is caused by factors associated with lifestyle-related diseases (obesity, diabetes and dyslipidemia).
In conclusion, the present study using obese and hyperlipidemic STR mice suggests that oxidative stress is associated with the development of OA, possibly via the degradation of type II collagen in articular cartilage.
Acknowledgments
The authors would like to thank Dr Katsumi Miyahara and Dr Atsushi Furuhata (Division of Biomedical Imaging Research, Juntendo University Graduate School of Medicine) for the technical expertise in the staining of the articular tissues. This study was partially supported by the High Technology Research Center Grant from the Ministry of Education, Culture, Sports, Science and Technology of Japan.
References
- 1.Shah R, Raska K, Jr, Tiku ML. The presence of molecular markers of in vivo lipid peroxidation in osteoarthritic cartilage. Arthritis Rheum. 2005;52:2799–2807. doi: 10.1002/art.21239. [DOI] [PubMed] [Google Scholar]
- 2.Hamerman D. The biology of osteoarthritis. N Engl J Med. 1989;320:1322–1330. doi: 10.1056/NEJM198905183202006. [DOI] [PubMed] [Google Scholar]
- 3.Henrotin YE, Bruckner P, Pujol JP. The role of reactive oxygen species in homeostasis and degradation of cartilage. Osteoarthritis Cartilage. 2003;11:747–755. doi: 10.1016/s1063-4584(03)00150-x. [DOI] [PubMed] [Google Scholar]
- 4.Khan IM, Gilbert SJ, Caterson B, Sandell LJ, Archer CW. Oxidative stress induces expression of osteoarthritis markers procollagen IIA and 3B3(-) in adult bovine articular cartilage. Osteoarthritis Cartilage. 2008;16:698–707. doi: 10.1016/j.joca.2007.10.004. [DOI] [PubMed] [Google Scholar]
- 5.Finkel T, Holbrook NJ. Oxidants, oxidative stress and the biology of ageing. Nature. 2000;408:239–247. doi: 10.1038/35041687. [DOI] [PubMed] [Google Scholar]
- 6.Harman D. Aging: a theory based on free radical and radiation chemistry. J Gerontol. 1956;11:298–300. doi: 10.1093/geronj/11.3.298. [DOI] [PubMed] [Google Scholar]
- 7.Gey KF. On the antioxidant hypothesis with regard to arteriosclerosis. Bibl Nutr Dieta. 1986;37:53–91. doi: 10.1159/000412175. [DOI] [PubMed] [Google Scholar]
- 8.Valvason C, Musacchio E, Pozzuoli A, Ramonda R, Aldegheri R, Punzi L. Influence of glucosamine sulphate on oxidative stress in human osteoarthritic chondrocytes: effects on HO-1, p22 (Phox) and iNOS expression. Rheumatology. 2008;47:31–35. doi: 10.1093/rheumatology/kem289. [DOI] [PubMed] [Google Scholar]
- 9.Melchiorri C, Meliconi R, Frizziero L, Silvestri T, Pulsatelli L, Mazzetti I, Borzi RM, Uguccioni M, Facchini A. Enhanced and coordinated in vivo expression of inflammatory cytokines and nitric oxide synthase by chondrocytes from patients with osteoarthritis. Arthritis Rheum. 1998;41:2165–2174. doi: 10.1002/1529-0131(199812)41:12<2165::AID-ART11>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 10.Mathy-Hartert M, Hogge L, Sanchez C, Deby-Dupont G, Crielaard JM, Henrotin Y. Interleukin-1beta and interleukin-6 disturb the antioxidant enzyme system in bovine chondrocytes: a possible explanation for oxidative stress generation. Osteoarthritis Cartilage. 2008;16:756–763. doi: 10.1016/j.joca.2007.10.009. [DOI] [PubMed] [Google Scholar]
- 11.Henrotin Y, Kurz B, Aigner T. Oxygen and reactive oxygen species in cartilage degradation: friends or foes? Osteoarthritis Cartilage. 2005;13:643–654. doi: 10.1016/j.joca.2005.04.002. [DOI] [PubMed] [Google Scholar]
- 12.Uchida K, Urabe K, Naruse K, Ogawa Z, Mabuchi K, Itoman M. Hyperlipidemia and hyperinsulinemia in the spontaneous osteoarthritis mouse model, STR/Ort. Exp Anim. 2009;58:181–187. doi: 10.1538/expanim.58.181. [DOI] [PubMed] [Google Scholar]
- 13.Walton M. Degenerative joint disease in the mouse knee joint; histological observations. J Pathol. 1977;123:109–122. doi: 10.1002/path.1711230207. [DOI] [PubMed] [Google Scholar]
- 14.Schunke M, Tillmann B, Bruck M, Muller-Ruckholtz W. Morphologic characteristics of developing osteoarthritic lesions in the knee cartilage of STR/IN mice. Arthritis Rheum. 1988;31:898–905. doi: 10.1002/art.1780310711. [DOI] [PubMed] [Google Scholar]
- 15.Rousseau JC, Delmas PD. Biological markers in osteoarthritis. Nat Clin Pract Rheumatol. 2007;3:346–356. doi: 10.1038/ncprheum0508. [DOI] [PubMed] [Google Scholar]
- 16.Yagi K. Simple assay for the level of total lipid peroxides in serum or plasma. Methods Mol Biol. 1998;108:101–106. doi: 10.1385/0-89603-472-0:101. [DOI] [PubMed] [Google Scholar]
- 17.Armstrong D, Browne R. The analysis of free radicals, lipid peroxides, antioxidant enzymes and compounds to oxidative stress as applied to the clinical chemistry laboratory. Adv Exp Med Biol. 1994;366:43–58. doi: 10.1007/978-1-4615-1833-4_4. [DOI] [PubMed] [Google Scholar]
- 18.Witztum JL, Steinberg D. Role of oxidized low density lipoprotein in atherogenesis. J Clin Invest. 1991;88:1785–1792. doi: 10.1172/JCI115499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kinoshita M, Oikawa S, Hayasaka K, Sekikawa A, Nagashima T, Toyota T, Miyazawa T. Age-related increases in plasma phosphatidylcholine hydroperoxide concentrations in control subjects and patients with hyperlipidemia. Clin Chem. 2000;46:822–828. [PubMed] [Google Scholar]
- 20.Carlo MD, Jr, Loeser RF. Increased oxidative stress with aging reduces chondrocyte survival: correlation with intracellular glutathione levels. Arthritis Rheum. 2003;48:3419–3430. doi: 10.1002/art.11338. [DOI] [PubMed] [Google Scholar]
- 21.Bates EJ, Harper GS, Lowther DA, Preston BN. Effect of oxygen-derived reactive species on cartilage proteoglycanhyaluronate aggregates. Biochem Int. 1984;8:629–637. [PubMed] [Google Scholar]
- 22.Tiku ML, Gupta S, Deshmukh DR. Aggrecan degradation in chondrocytes is mediated by reactive oxygen species and protected by antioxidants. Free Radic Res. 1999;30:395–405. doi: 10.1080/10715769900300431. [DOI] [PubMed] [Google Scholar]
- 23.Tiku ML, Allison GT, Naik K, Karry SK. Malondialdehyde oxidation of cartilage collagen by chondrocyte. Osteoarthritis Cartilage. 2003;11:159–166. doi: 10.1016/s1063-4584(02)00348-5. [DOI] [PubMed] [Google Scholar]
- 24.Garnero P, Rousseau JC, Delmas PD. Molecular basis and clinical use of biochemical markers of bone, cartilage, and synovium in joint disease. Arthritis Rheum. 2000;43:953–968. doi: 10.1002/1529-0131(200005)43:5<953::AID-ANR1>3.0.CO;2-Q. [DOI] [PubMed] [Google Scholar]
- 25.Garnero P, Piperno M, Gineyts E, Christgau S, Delmas PD, Vignon E. Cross sectional evaluation of biochemical markers of bone, cartilage, and synovial tissue metabolism in patients with knee osteoarthritis: relations with disease activity and joint damage. Ann Rheum Dis. 2001;60:619–626. doi: 10.1136/ard.60.6.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Garnero P, Ayral X, Rousseau JC, Christgau S, Sandell LJ, Daugados M, Delmas PD. Uncoupling of type II collagen synthesis and degradation predicts progression of joint damage in patients with knee osteoarthritis. Arthritis Rheum. 2002;46:2613–2624. doi: 10.1002/art.10576. [DOI] [PubMed] [Google Scholar]
- 27.Garnero P, Conrozier T, Christgau S, Mathieu P, Delmas PD, Vignon E. Urinary type II collagen C-telopeptide levels are increased in patients with rapidly destructive hip osteoarthritis. Ann Rheum Dis. 2003;62:939–943. doi: 10.1136/ard.62.10.939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Reijman M, Hazes JM, Bierma-Zeinstra SM, Koes BW, Christgau S, Christiansen C, Uitterlinden AG, Pols HA. A new marker for osteoarthritis: cross-sectional and longitudinal approach. Arthritis Rheum. 2004;50:2471–2478. doi: 10.1002/art.20332. [DOI] [PubMed] [Google Scholar]
- 29.Jordan KM, Syddall HE, Garnero P, Gineyts E, Dennison EM, Sayer AA, Delmas PD, Cooper C, Arden NK. Urinary CTX-II and glucosyl-galactosyl-pyridinoline are associated with the presense and severity of radiographic knee osteoarthritis in men. Ann Rheum Dis. 2006;65:871–877. doi: 10.1136/ard.2005.042895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Meulenbelt I, Kloppenburg M, Kroon HM, et al. Urinary CTX-II levels are associated with radiographic subtypes of osteoarthritis in hip, knee, hand, and facet joints in subjects with familial osteoarthritis at multiple sites: the GARP study. Ann Rheum Dis. 2006;65:360–365. doi: 10.1136/ard.2005.040642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhai G, Cicuttini F, Ding C, Scott F, Garnero P, Jones G. Correlates of knee pain in younger subjects. Clin Rheumatol. 2007;26:75–80. doi: 10.1007/s10067-006-0248-8. [DOI] [PubMed] [Google Scholar]
- 32.Poole AR, Ionescu M, Fitzcharles MA, Billinghurst RC. The assessment of cartilage degradation in vivo: development of an immunoassay for the measurement in body fluids of type II collagen cleaved by collagenases. J Immunol Methods. 2004;294:145–153. doi: 10.1016/j.jim.2004.09.005. [DOI] [PubMed] [Google Scholar]
- 33.Nelson F, Dahlberg L, Laverty S, Reiner A, Pidoux I, Ionescu M, Fraser GL, Brooks E, Tanzer M, Rosenberg LC, Dieppe P, Poole AR. Evidence for altered synthesis of type II collagen in patients with osteoarthritis. J Clin Invest. 1998;102:2115–2125. doi: 10.1172/JCI4853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Keaney JF, Jr, Larson MG, Vasan RS, Wilson PW, Lipinska I, Corey D, Massaro JM, Sutherland P, Vita JA, Benjamin EJ. Obesity and systemic oxidative stress: clinical correlates of oxidative stress in the Framingham Study. Arterioscler Thromb Vasc Biol. 2003;23:434–439. doi: 10.1161/01.ATV.0000058402.34138.11. [DOI] [PubMed] [Google Scholar]
- 35.Fujita K, Nishizawa H, Funahashi T, Shimomura I, Shimabukuro M. Systemic oxidative stress is associated with visceral fat accumulation and the metabolic syndrome. Circ J. 2006;70:1437–1442. doi: 10.1253/circj.70.1437. [DOI] [PubMed] [Google Scholar]
- 36.Siwik DA, Pagano PJ, Colucci WS. Oxidative stress regulates collagen synthesis and matrix metalloproteinase activity in cardiac fibroblasts. Am J Physiol Cell Physiol. 2001;280:C53–C60. doi: 10.1152/ajpcell.2001.280.1.C53. [DOI] [PubMed] [Google Scholar]