Abstract
Background:
HIV directly affects the brain and produces varied psychiatric manifestations. 10-30% of patients with AIDS were found to have cognitive impairment and the virus is isolated in the CSF in 70% of AIDS patients.
Aim:
The present study is aimed at finding out the prevalence, nature, and extent of cognitive changes in AIDS patients.
Materials and Methods:
The consecutive sample of 33 patients with AIDS attending the ART center of our college were clinically interviewed and administered MMSE, BGT, Wechsler Memory Scale, and International HIV Dementia Scale.
Results:
In clinical assessment, only 1/33 (3%) patients could be diagnosed as dementia in HIV disease (ICD10-F02.4). This confirms the current Indian reports which indicate a lower prevalence of HIV dementia in our population. 2/33 (6%) patients were recognized to have mild cognitive disorder due to HIV disease (ICD10-F06.7). Asymptomatic cognitive impairment is very common in AIDS patients and it was noted in 69% of our study population. In the tests, MMSE was positive in only 3 of the 33 patients (9%) and it was not helpful to recognize cognitive deficits in our patients. The Wechsler Memory Scale was abnormal in 18 of the 33 patients (55%). BGT was abnormal in 48.5% of patients. The International HIV Dementia Scale was the most sensitive instrument and 63.6% the patients had abnormal scores in this scale.
Conclusion:
Tests which assess cognitive and motor speed may be more helpful than clinical psychiatric interview to spot the AIDS patients who have cognitive impairment.
Keywords: AIDS, asymptomatic cognitive impairment, HIV dementia
INTRODUCTION
Neurotrophic HIV directly invades our brain and produces neuropsychiatric manifestations. The most common manifestation described is AIDS dementia complex otherwise labeled as HIV-associated dementia (HAD). The prevalence of HAD reported was about 15-19%.[1] Recent reports suggest a low prevalence rate of cognitive impairment among Indian HIV +ve patients.[2]
Aim of the study
The present study is aimed at finding out the prevalence, nature, and extent of cognitive impairment in AIDS population of our area.
MATERIALS AND METHODS
The new AIDS patients registered at the ART centre of our medical college hospital were taken for this study. All the patients were enrolled after getting informed consent. Exclusion criteria were patients with current or past opportunistic central nervous system (CNS) infections, presence of severe medical, psychiatric, or neurological disorder which would interfere with the ability to cooperate and undergo the clinical and psychometric evaluation.
All the patients were assessed by the ART physician. CD4 cell count and clinical HIV staging were done for all the patients as per WHO criteria. All the 33 patients correspond to stage III based on WHO criteria. The patients were clinically interviewed by the psychiatrist. They were also staged using the Memorial Sloan Kettering Clinical staging system.[3] The patients were administered by MMSE, BGT, Wechsler Memory Scale and International HIV Dementia Scale (IHDS). In short, all the AIDS patients received physical assessment, clinical psychiatric assessment, psychological testing, and CD4 count.
IHDS consists of three subtests (i) timed finger tapping (ii) timed alternating hand sequence test, and (iii) recall of four items in 2 minutes. The IHDS is now used in many studies as a screening test to detect dementia in HIV patients.[4] The patients were administered the above tests in the same sequence as noted above in one or two settings in a relaxed atmosphere.
Description of the sample
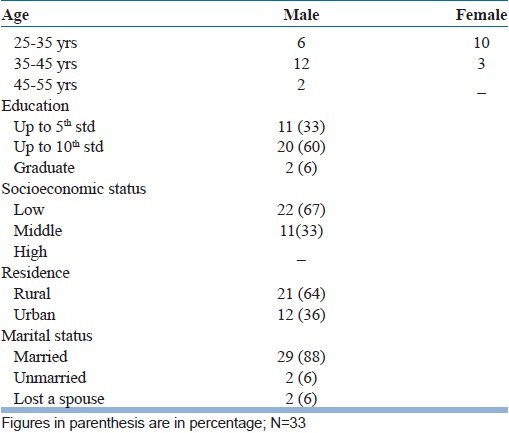
There were 33 patients, their age ranging from 25 to 50 years. There were 20 males and 13 females. A majority of the patients belonged to the low socioeconomic group (22/33). Twenty-one patients came from rural areas and 12 hail from urban areas. Twenty-nine were married and 2 were unmarried. Two patients were widows. Educational status wise, a majority (20) had studied up to SSLC. Eleven patients have studied up to 5th std [Table 1].
Table 1.
Socio demographic characteristics
RESULTS
Only 1 among the 33 patients had HIV-associated dementia complex (HADC). He was 34 yr old. He had Memory Quotient of 62, scored 2 in the Memorial Sloan Kettering scale, his CD4 count was 141. Clinical interviewing revealed severe impairment in daily functioning.
Two other patients out of 33 in our study had Minor Cognitive Motor Disorder. One was 42 yr old. His MMSE score was 22. His M.Q was 106. He scored 1 in the MSK scale. His CD4 count was 144. The other patient with MCMD had CD4 count of 128. MSK score was 1. His MMSE score was 21. His M.Q was 84. Both these patients had only mild subjective impairment of memory [Table 2].
Table 2.
Prevalence of cognitive impairment based on clinical and neuropsychological tests
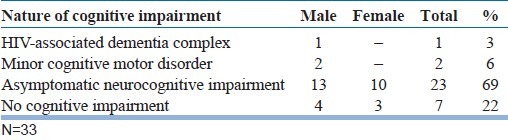
Asymptomatic cognitive impairment is very common in AIDS patients. It was noted in 69% of our sample (23/33).
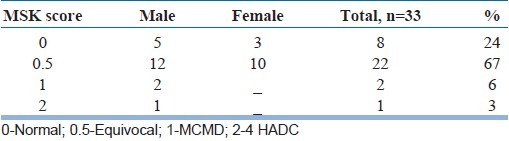
Psychometric findings
Psychometric findings were more abnormal than clinical interview findings with regard to cognitive function in AIDS patients. Seventy-eight percent of AIDS population had some cognitive impairment in their test protocols [Table 3].
Table 3.
The Memorial Sloan Kettering scores
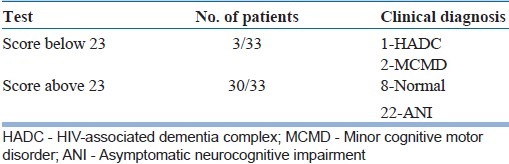
MMSE
MMSE is not very useful to detect the cognitive impairment in AIDS. Only 3/33 (9%) of AIDS patients had abnormal scores. Of these three, one had HADC, the other two had MCMD [Table 4].
Table 4.
Mini mental state examination scores
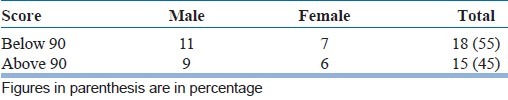
Wechsler memory scale
Mean M.Q of the total AIDS sample (N=33) was 84.8. Range of M.Q varied between 60 and 100. 55% (18/33) had abnormal scores if 90 was taken as cut off M.Q. [Table 5].
Table 5.
Memory quotient scores
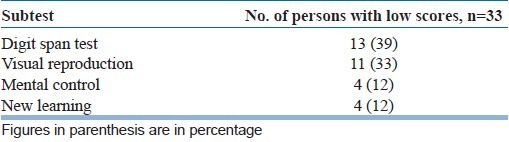
Patients who had low scores performed poorly in digit span test 39% (13/33) and visual reproduction 33% (11/33) [Table 6].
Table 6.
Wechsler memory scale subtest findings
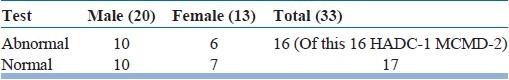
BGT Findings
Out of 33 patients tested, 16 patients showed signs of organicity in BGT (48.5%). No specific pattern was noted in this sample of patients. Distortion, rotation, missing, and other abnormal patterns were noticed in their protocols [Table 7].
Table 7.
Bender Gestalt test findings
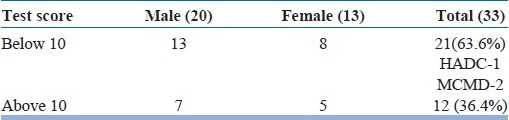
IHDS Findings
IHDS is now used widely in screening HIV patients to identify the presence of cognitive impairment. 63.6% of our study population scored positive in this scale. Of the three subtests alternating hand sequence test was the most sensitive and was abnormal in 63.6% of the study population [Table 8].
Table 8.
International HIV dementia scale findings
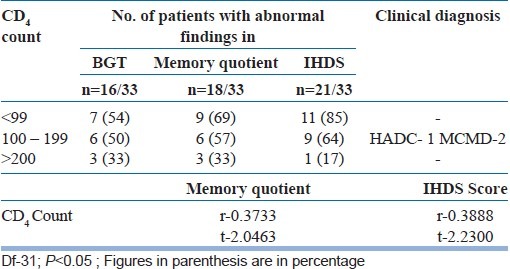
CD4 and cognitive deficit
CD4 cell count reflects the individual's immunity while viral load defines the severity of viral infection. Viral load was not assessed in our patients as facilities to carry out the test were not available locally. Positive correlation was found between low CD4 count and more neurocognitive impairment in our study. Low CD4 count is one of the commonly identified risk factor for the development of HIV dementia. Reduced CD4 level is associated with a 60% increase in the odds of having HIV dementia [Table 9].
Table 9.
Correlation of CD4 count with the test findings
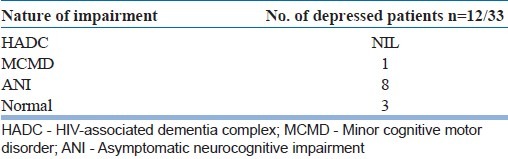
Depression and cognition in AIDS
One of the factors discussed in relation to cognitive impairment in HIV +ve individuals is co-morbid depression. Out of the 33 patients in our study, 12 were depressed based on clinical diagnosis. All of them had depression of mild intensity only and this may not be a causal factor in their cognitive performance. Of this 12, one had MCMD, 8 had ANI and 3 scored normal in the tests [Table 10].
Table 10.
Nature of impairment among the depressed patients
DISCUSSION
Dementia in AIDS indicates an increased risk of mortality.[5] The presence of dementia will interfere with ART treatment, which is the bed rock of AIDS management. ART has again proved to be useful in improving the cognitive impairment.[6] Hence, it is imperative that cognitive impairment should be recognized early in a HIV +ve patient to enhance drug compliance to ART. This will improve quality of life, increase longevity of life, and arrest further deterioration of brain function.
HIV enters the brain shortly after infection and has a predilection for subcortical brain areas. The cognitive impairment is attributed to HIV replication in brain and liberation of inflammatory neurotoxins leading to impairment of natural host repair mechanisms. This leads to neuronal dysfunction, injury, or death.[7]
American Academy of Neurology Task Force on AIDS[8] describes two neurobehavioral disorders in HIV.
HIV-Associated Dementia Complex (HADC)
HIV-Associated Minor Cognitive Motor Disorder (MCMD)
This is widely accepted now. This correlates to ICD10-F02.4-dementia in HIV disease and ICD10-F06.7-mild cognitive disorder due to HIV disease. The difference between 1 and 2 is severity of cognitive impairment and degree of impairment in daily living. In HADC, defects are moderate to severe and interfere with day-to-day living. In MCMD, the psychological defects are mild and cause only mild functional impairment.
The HIV Neurobehavioral Research Centre (HNRC), San Diego, has proposed inclusion of an Asymptomatic Neurocognitive Impairment (ANI) category in addition to the above two categories described.[9] Cognitive disturbances are essential to diagnose this category. The decline in daily functioning, motor or other behavioral abnormalities were not present in these individuals. Autopsy findings in these patients again supported the inclusion of this category.
Indian literature about HIV and psychiatry are few. Rao[10] compared asymptomatic HIV +ve and HIV −ve patients attending STD clinic at Madurai. Both the groups had similar prevalence rate for the common mental disorders. No patient with cognitive deficit was noted in that report. Psychiatric morbidity survey in AIDS was done using clinical interviews, GHQ and BPRS by Mittal et al.[11] Of the 100 patients in their ART center, none was reported to have HADC or MCMD.
Asymptomatic HIV +ve patients were studied by Satapathy et al.[12] 90% of these patients were noted to have psychiatric illness. Adjustment disorders and depression was the common diagnosis. None of the patients were found to have cognitive defects in this study. The above studies were clinical studies and neuropsychological tests were not used in these studies. Mild cognitive deficits cannot be recognized with only clinical interview methods.
Singh et al.[13] assessed cognitive functions in clinically asymptomatic HIV +ve individuals. They found significant cognitive dysfunction in HIV +ve individuals compared to seronegative individuals on a battery of neuropsychological tests. None of their 50 HIV +ve individuals were found to have HADC or MCMD. 50 HIV +ve patients in stages I, II, and III were compared with 50 controls using the digit span test, word association test, and other tests by Mandal et al.[14] HIV +ve individuals scored poor in all tests but the values were statistically significant in digit symbol substitution test, controlled word association test, and trail making test.
Studies from west show that 15% of AIDS patients have HADC.[1] Our study population is similar to this group of western study population in their severity. Only 1 out of 33 patients with AIDS in our study have HADC i.e., 3.03% unlike 15% in the west. This finding again is in correlation to Chandra's report which indicates only 1.4% cognitive impairment in HIV +ve patients in India. They recorded HADC in 6 out of 427 HIV +ve asymptomatic individuals. They propose that a compromised chemotactic function of C-Tat protein in our population may be the factor underlying the low incidence of cognitive impairment of our patients.[15]
Gupta et al. found 60.5% of HIV +ve individuals have mild to moderate cognitive deficits in the domains of word fluency, working memory, and learning.[16] None of their 119 HIV +ve individuals had severe cognitive deficits. Similar findings were noted in our study i.e. 69% of our population had mild to moderate cognitive impairments but were clinically asymptomatic.
Folstein MMSE was developed for use in screening cortical dementia and it is relatively less sensitive to detect the subcortical dementia due to HIV infection.[5] This was confirmed by our study. Only 3 out of our 33 patients scored low in MMSE.
We also found that patients who had low memory quotient performed poorly in digit span test (39%) and visual reproduction (33%). This is in conformity to Gupta's report which shows greater impairment of visual working memory in patients with CD4 count less than 200 cells/mm.[16]
Riedel[17] has administered the IHDS scale to the asymptomatic HIV +ve population in Pune and found that 35% of them have abnormal scores in this test. Our study is from the AIDS population and 63.6% of them scored positive in this scale. Using the cut-off ≤10, the test is reported to be sensitive in 80% of patients and specificity reported in about 55%.[4] Of the three subsets alternating hand sequence test was the most sensitive and was abnormal in 63.6% of the study population. This test assesses the psychomotor speed. Stern et al.[18] findings were similar in nature. Psychomotor slowing is the only neurobehavioral deficit in asymptomatic HIV +ve individuals described by them in their report.
Chang et al.[19] report a positive correlation between low CD4 count and cognitive impairment in his patients. Positive correlation was found between low CD4 count and more neurocognitive impairment in our study also.
Limitation of the study
As our study was done in a small group it is difficult to apply the results on the general population.
CONCLUSION
Prevalence of HIV-associated dementia complex (HADC) is less in our AIDS population. It is only 3% compared to 15-19% reported from the west. HIV-associated Minor cognitive motor disorder constitutes 6% of our study population.
Based on neuropsychological tests cognitive impairment is noted in up to 78% of AIDS patients. But only 9% of the patients were found to have cognitive impairment clinically. Hence, more than clinical interview, neuropsychological tests are more useful to spot cognitive impairment in HIV +ve individuals. Psychomotor slowing was the most common neuropsychological defect noted in our AIDS patients.
Advent of ART leads to more longevity of HIV patients and psychiatric co-morbidity is bound to increase now. Early and periodic neuropsychological screening of HIV +ve asymptomatic individuals is a must in future to spot the cognitive deficits at an early stage. This may help us in arresting the progression of the disease by early institution of ART therapy as HIV dementia is an indication for ART. HIV dementia may as well be reversible in many patients. Former U.S. President Mr. Bill Clinton calls HIV epidemic as a Disaster of the 20th century. We are going to face more of HIV orphans and neuropsychiatric AIDS in our future. Only concerted efforts by all of us will reduce the impact of this unmitigated disaster in our society.
ACKNOWLEDGMENTS
The authors express our sincere thanks to the Assistant Professor and PG's of Department of Psychiatry, Thanjavur Medical College and all the Staffs of the Art Centre, Thanjavur Medical College for their kind cooperation and support.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Mc Arthur JC, Moover DR, Bacellor H, Miller EN, Cohen BA, Becker JT, et al. Dementia in AIDS patients: Incidence and risk factors. Multicenter AIDS cohort study. Neurology. 1993;43:2245–52. doi: 10.1212/wnl.43.11.2245. [DOI] [PubMed] [Google Scholar]
- 2.Chandra PS, Desai G, Ranjan S. HIV and psychiatric disorders. Indian J Med Res. 2005;121:451–67. [PubMed] [Google Scholar]
- 3.Price RW, Brew BJ. The AIDS Dementia Complex. J Infect Dis. 1988;158:1079–83. doi: 10.1093/infdis/158.5.1079. [DOI] [PubMed] [Google Scholar]
- 4.Sacktor NC, Wong M, Nekarujja N, Skolasky RL, Selnes OA, Musisi S, et al. The international HIV dementia scale: A new rapid screening test for HIV dementia. AIDS. 2005;19:1367–74. [PubMed] [Google Scholar]
- 5.Citron K, Broullette MJ, Bechett A. HIV and psychiatry. 35. Cambridge, England: Cambridge University Press; 2005. [Google Scholar]
- 6.Ferrando S, Van Gorp W, McElhiney M, Goggin K, Sewell M, Rabkin J, et al. Highly active ART in HIV infections; benefits for neuropsychological function. AIDS. 1998;12:65–70. doi: 10.1097/00002030-199808000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Tyor WR, Wesselringh SL, Griffin JW, Mc Arthur JC, Griffin DE. Unifying hypothesis for the pathogenesis of HIV associated dementia complex. J Acquir Immune Defic Syndr Hum Retrovirol. 1995:379–88. [PubMed] [Google Scholar]
- 8.American Academy of Neurology AIDS Task Force. Nomenclature and Research case definition for neurological manifestation of Human Immunodeficiency virus type-I (HIV- I) infection. Neurology. 1991;41:778–85. doi: 10.1212/wnl.41.6.778. [DOI] [PubMed] [Google Scholar]
- 9.Cherner M, Cystique L, Heaton RK. Neuropathological confirmation of definitional criteria for human immunodeficiency virus associated neurocognitive disorders. J Neurovirol. 2007;13:23–8. doi: 10.1080/13550280601089175. [DOI] [PubMed] [Google Scholar]
- 10.Venkoba Rao A, Swaminathan R, Venkataraman MK. A clinical and behavioural study of HIV infected subjects. Indian J Psychiatry. 1991;33:95–163. [PMC free article] [PubMed] [Google Scholar]
- 11.Mittal A, Pathah PK, Shina BC. Psychiatric morbidity in AIDS patients. Indian J Psychiatry. 2000;42:427–39. [Google Scholar]
- 12.Satapathy R, Murali Krishna M, Ashok Babu M, Vijayagopal M. A study of psychiatric manifestations of physically asymptomatic HIV-I seropositive individuals. Indian J Psychiatry. 2000;42:427–33. [PMC free article] [PubMed] [Google Scholar]
- 13.Singh H, Sharma CS, Chakraborthy PK, Sattar FA. Cognitive dysfunction in clinically asymptomatic HIV seronegative individuals. Indian J Psychiatry. 2001;43:162–70. [Google Scholar]
- 14.Mandal N, Singh OP, Bhattacharya S, Chatterji S, Biswas A, Sen S. Neurocognitive impairment in early HIV positive individuals. J Indian Med Assoc. 2008;106:442–9. [PubMed] [Google Scholar]
- 15.Ranga U, Shankarappa R, Siddappa NB, Ramakrishna L, Nagendran R, Mahalingam M, et al. Tat protein of Human Immuno Deficiency Virus Type - I Subtype C Strains is a Defective chemokine. J Virol. 2004;78:2586–90. doi: 10.1128/JVI.78.5.2586-2590.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gupta JD, Satishchandra P, Gopukumar K, Wilkie F, Waldrop-Valverde D, Ellis R, et al. Neuropsychological deficits in human immunodeficiency virus type 1 Clade C-seropositive adults from South India. J Neurovirol. 2007;13:195–202. doi: 10.1080/13550280701258407. [DOI] [PubMed] [Google Scholar]
- 17.Riedel D, Ghate M, Nene M, Paranjape R, Mehendale S, Bollinger R, et al. Screening for Human Immunodeficiency Virus (HIV) dementia in a HIV clade C infected population in India. J Neurovirol. 2006;12:34–8. doi: 10.1080/13550280500516500. [DOI] [PubMed] [Google Scholar]
- 18.Stern Y. Neuropsychological evaluation of the HIV patient. Psychiatr Clin North Am. 1994;17:25–34. [PubMed] [Google Scholar]
- 19.Chang L, Ernst T, Leonardo-Yee M, Walot I, Singer E. Cerebral metabolite abnormalities correlate with clinical severity of HIV-I cognitive motor complex. Neurology. 1999;52:100–8. doi: 10.1212/wnl.52.1.100. [DOI] [PubMed] [Google Scholar]


