Abstract
Cemento-ossifying fibroma is a benign fibro-osseous lesion belonging to the same category as fibrous dysplasia and cementifying dysplasia. These are slow-growing lesions that are seen in the third and fourth decades of life. Both the ossifying fibroma and cemento-ossifying fibroma represent two extremes of the same disease process since histologically both contain bone and cementum. However, the term cemento-ossifying fibroma is justified on the basis of clinical and radiological correlation. Radiographs have become an essential tool in the diagnosis of lesions in the jaw, where the anatomy is complex. Nowadays, CT provides information for diagnosis as well as treatment planning. In this case series, we report three cases of cemento-ossifying fibroma that were histologically confirmed and discuss the imaging findings.
Keywords: Benign fibro-osseous lesion, cemento-ossifying fibroma, radiographic features
INTRODUCTION

Cemento-ossifying fibroma (COF) is a rare, benign fibro-osseous lesion of the jaws exhibiting well-circumscribed, unilocular radiolucency mixed with radiopacity based on the type of mineralized tissue it contains.[1] The origin of COF has been associated with the periodontal membrane that has multipotent cells capable of forming cementum, lamellar bone, and fibrous tissue.
In 1872, Menzel gave the first description of a variant of ossifying fibroma and called it as cement-ossifying fibroma.[2] It was later described by Montegomery in 1927. Makek suggested the term ‘benign periodontoma’ based on its origin.[3] In 1971, WHO classified COF under cementum forming lesions that also included fibrous dysplasia, ossifying fibroma, and cementifying fibroma. However, in 2005, the term was reduced to ossifying fibroma.[4]
Clinically, these tumors manifest as a slow-growing mass that may be asymptomatic and would be seen on a routine orthopantomogram. The histological representation usually contains cementum, immature bony trabeculae that may also be seen in fibrous dysplasia. A definitive diagnosis is usually established based on the correlation between clinical, radiological, and histological findings.[5] We report a case series of three COF, two of which are seen in the maxilla and one in the mandible.
CASE REPORTS
Case 1
A 32-year-old female patient presented to our department with a complaint of swelling in the region of the upper front teeth. The swelling started 5 months earlier and had gradually increased in size. No pain was reported in the region of the swelling. On intra-oral examination, a diffuse swelling was seen in the region of teeth 21-23 on the labial aspect. The swelling was 4 × 3 cm in size and had obliterated the labial vestibule in relation to teeth 21- 23. There were no secondary changes. The left maxillary lateral incisor was displaced distally. On palpation, the swelling was hard, non-tender, and was not fluctuant and compressible. The patient was subjected to a series of conventional radiographs, and computed tomography para-nasal sinus (CT PNS) view scan.
Intra-oral periapical radiograph of left maxillary anterior region, maxillary occlusal [Figure 1] and orthopantomograph [Figure 2] revealed a well-circumscribed unilocular radiolucency in the left anterior maxillary region in relation to the left maxillary central and lateral incisor. The radiolucency was surrounded by a radiopaque border. Left maxillary central incisor was displaced mesially and left maxillary lateral incisor distally.
Figure 1.
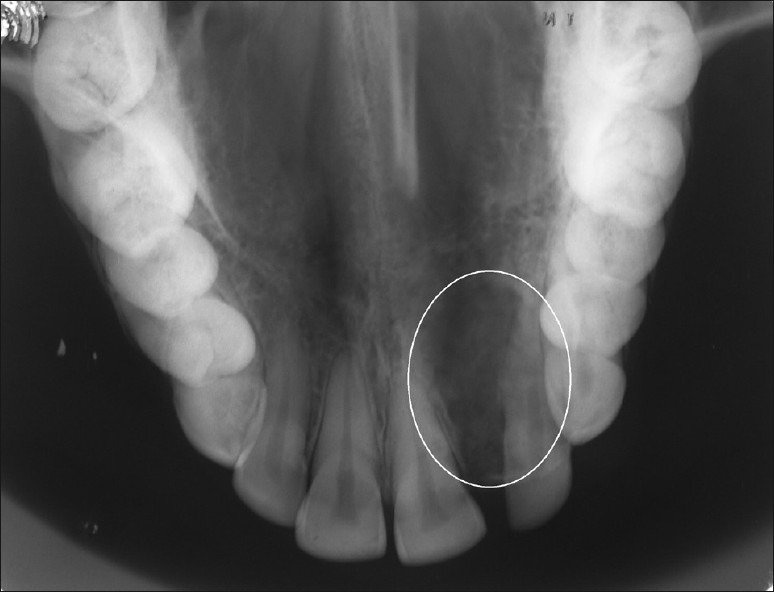
Maxillary occlusal radiograph reveals a unilocular well-circumscribed radiolucency with thin cortication in the periphery (circled area).
Figure 2.
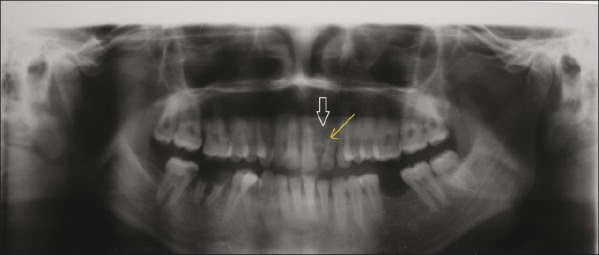
An orthopantomograph reveals a well-circumscribed unilocular radiolucency (broad arrow) and a displaced lateral incisor (thin arrow).
CT PNS view and 3D CT [Figures 3 and 4] demonstrated an expansile cystic lesion with well demarcated margins arising from the alveolar surface of the maxilla with areas of calcification.
Figure 3.
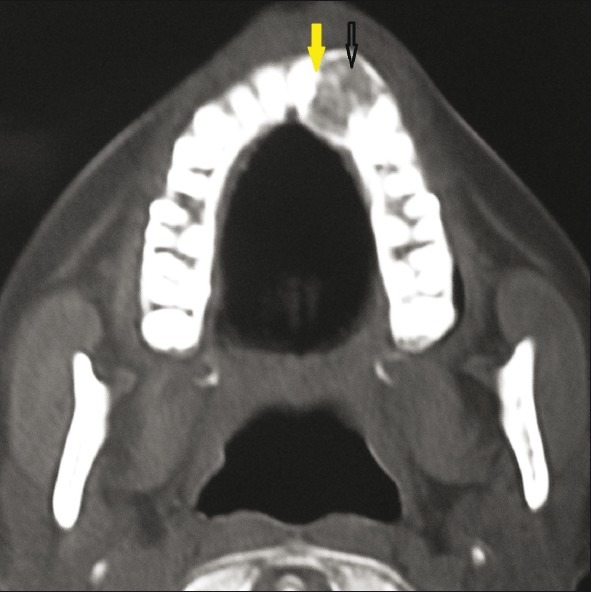
CT Para nasal view shows an expansile lesion with well-demarcated margins and area of calcification (black arrow) in the left maxilla with a displaced maxillary left lateral incisor (yellow arrow).
Figure 4.
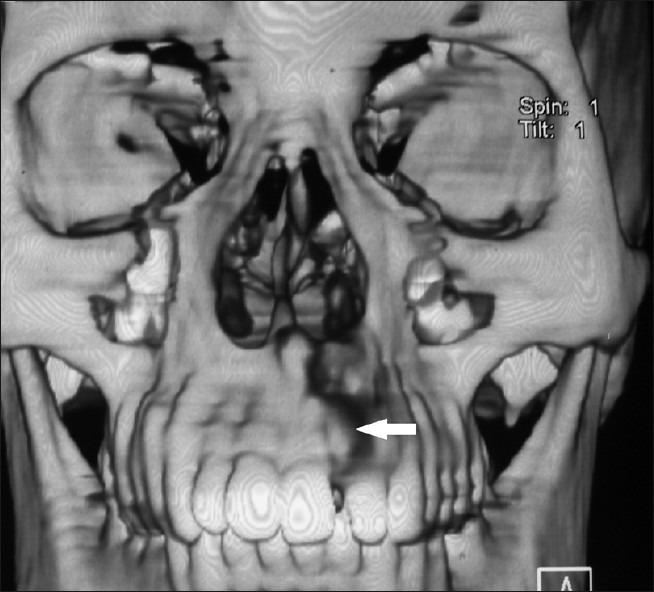
3D CT reveals an expansile lesion (white arrow) on the alveolar surface of the maxilla.
Case 2
A middle-aged female patient presented to our department with a complaint of swelling in the region of the right cheek. Patient history revealed that the swelling had started spontaneously 6 months earlier as a small one and had gradually increased in size. Patient did not give any history of pain. On intra-oral examination, a single diffuse swelling was present in the right zygomatic region. On palpitation, the swelling was found to be hard and non-tender. No secondary changes were seen.
Intra-orally, a diffuse swelling was present in the alveolar mucosa in relation to the buccal aspect of teeth 13 to 16. The surface of the lesion was smooth. It was associated with Grade II mobility in relation to teeth 14 and 15.
Intra-oral periapical radiograph of teeth 13 to 16 revealed a mixed radiopaque and radiolucent lesion with more areas of dense radiopacities. Maxillary right second premolar appeared to be displaced. The crown and root outline of tooth 16 was obscured by the dense radiopacity.
Orthopantomogram revealed a diffuse radiopacity with areas of radiolucency in the region of teeth 13 to 16. Maxillary right second premolar are displaced [Figure 5].
Figure 5.
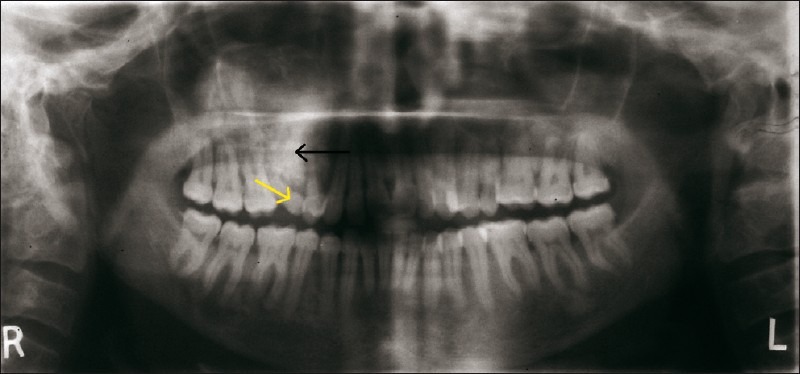
An orthopantomogram reveals diffuse radiolucency with areas of radiopacity (black arrow) in the region of right maxillary canine to molar region. Maxillary right second premolar (yellow arrow) appears to be displaced.
CT PNS of right maxilla showed a well-defined expansile lesion with sclerotic margin and scattered amorphous calcification and teeth within [Figures 6 and 7]. The lesion involved the floor of the maxillary sinus [Figure 7].
Figure 6.
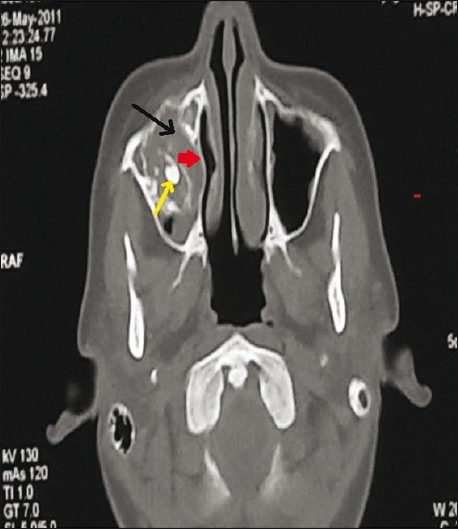
CT axial view shows a well-defined expansile lesion (black arrow) with sclerotic margin (red arrow), scattered amorphous calcification and teeth within the lesion (yellow arrow).
Figure 7.
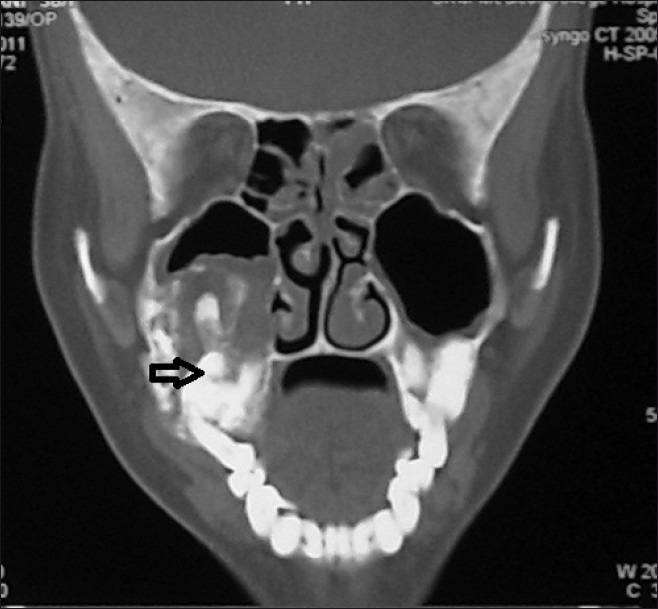
CT coronal view shows an expansile lesion in the right maxilla exhibiting features of calcification, presence of teeth displaced due to the lesion (black arrow) and involving the floor of the maxillary sinus.
Case 3
A 52-year-old female patient presented with a swelling in the right lower back tooth. The swelling had started 6 months earlier and had gradually increased in size. There was no history of pain associated with the swelling. The patient was a diabetic for more than 20 years.
Clinical examination revealed a single diffuse swelling measuring about 4 × 3 cm in size in relation to buccal and lingual aspect of mandibular premolar to molar region on the right side. There was evidence of buccal and lingual cortical plate expansion. The swelling lacked tenderness, had a smooth surface, and was hard. There was Grade III mobility in the right mandibular second premolar and second molar. Mandibular first molar teeth had been extracted 2 years earlier.
Mandibular occlusal radiograph, right lateral skull OPG, and CT were advised.
Mandibular occlusal radiograph [Figure 8] of the right side revealed a lesion expanding both the buccal and lingual cortical plates in the posterior mandible in relation to mandibular first premolar to molar region. The lesion showed mixed radiolucent and radiopaque areas.
Figure 8.

Mandibular occlusal radiograph of right side reveals the expansion of buccal (black arrow) and lingual (white arrow) cortical plates.
Orthopantomograph [Figure 9] and right lateral skull [Figure 10] view revealed a well-defined lesion extending from mesial surface of mandibular first premolar to distal part of mandibular second molar. There was a corticated outline, delineating the interior of the lesion from the surrounding adjacent normal bone. Areas of mixed radiopacity and radiolucency represented the internal architecture of the lesion. Mandibular second molar was displaced mesially with evidence of root resorption and mandibular second premolar was displaced distally. There was thinning and bowing of the inferior border of the mandible.
Figure 9.
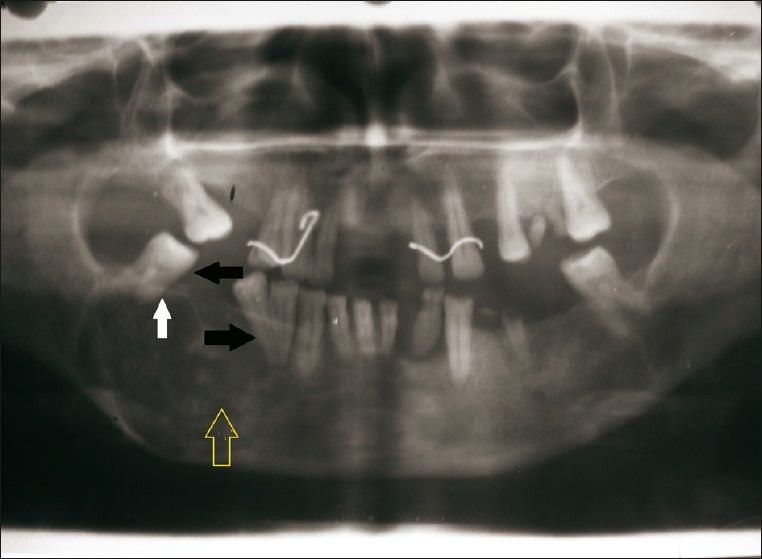
Orthopantograph reveals a mixed radiolucent-radiopaque lesion (yellow arrow) extending from mandibular first premolar to molar region. The image shows displacement of mandibular right second molar and second premolar (black arrow). There is evidence of root resorption in mandibular right second molar (white arrow).
Figure 10.
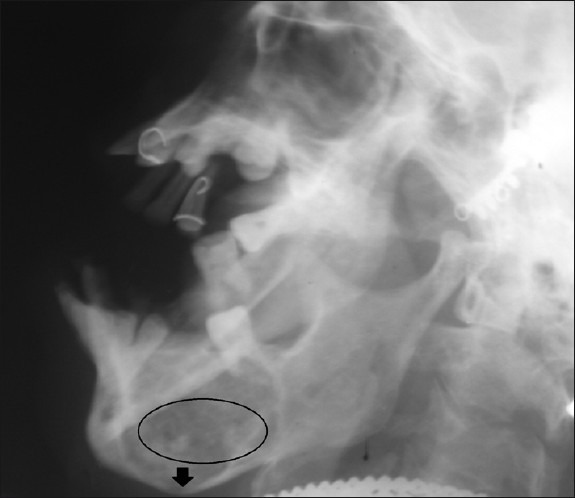
Right lateral skull radiograph shows mixed radiolucent and radiopaque lesion (circle) surrounded by a corticated border in relation to posterior mandible. There is thinning and bowing of the inferior border of the mandible (black arrow).
CT [Figures 11 and 12] revealed expansile abnormality in the right side of the mandible with non-coalescing foci of mineralization, indicating it to be a low density lesion. Low density may represent fibrous tissue giving it a ground glass appearance. There was equidistant expansion of the buccal and lingual cortical plates. The margins were intact.
Figure 11.
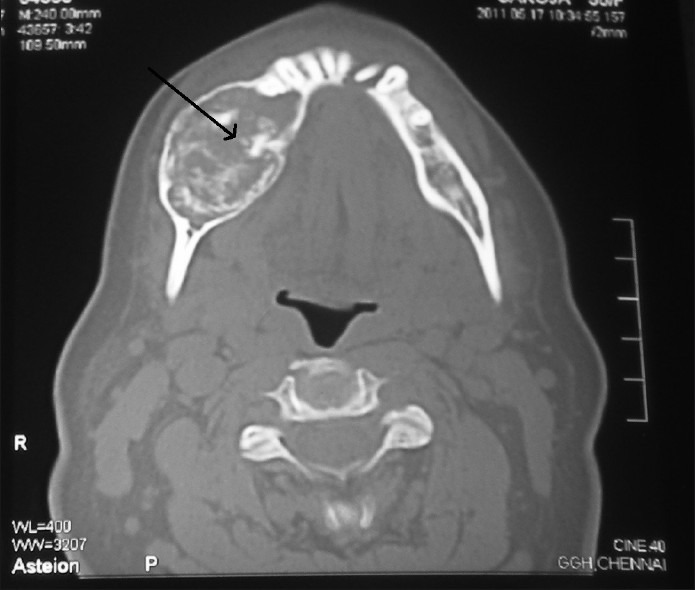
CT axial view shows an expansile lesion in the right mandible with equidirectional expansion, the margins are intact and there is a non-coalescing foci of mineralisation (black arrow).
Figure 12.
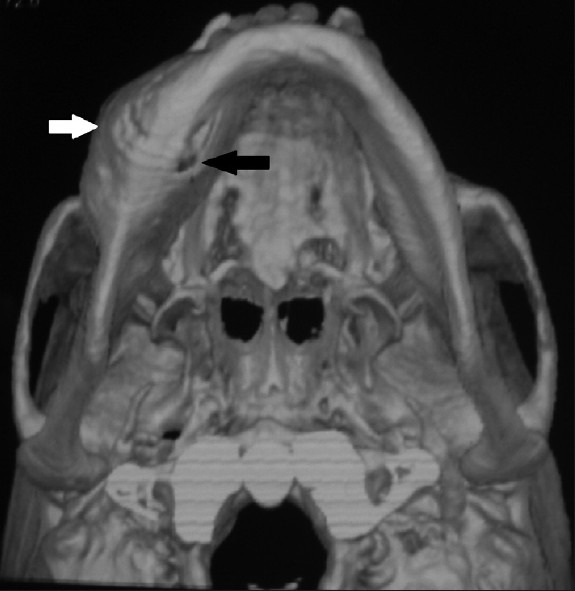
3D CT reveals abnormality in the right mandible with expansion of the buccal (white arrow) and lingual cortical plates (black arrow).
A provisional diagnosis of benign neoplasm of bone which could be either odontogenic/non-odontogenic was made. A differential diagnosis of ameloblastoma, CEOT, odontogenic myxoma, cemento-ossifying fibroma, and fibrous dysplasia was considered.
An incision biopsy was performed under local anesthesia and the tissue was preserved in formalin and sent for histopathology examination.
Histopathology revealed presence of hypercellular fibrous tissue, cementum-like particles blending in the stroma, and few intense basophilic dystrophic calcifications. Further, correlating with the clinical and radiological features, a final diagnosis of cement-ossifying fibroma was arrived.
DISCUSSION
Fibro-osseous lesions are of utmost significance for the oral and maxillofacial radiologists. Pathology for all the fibro-osseous lesions are similar and require clinical and radiological correlation.[6]
Cemento-osssifying fibroma is a fibro-osseous neoplasm classified by WHO under non-odontogenic tumor derived from multipotent blast cells of mesenchymal tissue of periodontium.[5] The fibrous connective tissue of the periodontal membrane is composed of collagen, oxytalan fibers, and mucopolysaccharides which has the capacity to produce bone, cementum, and fibrous tissue. These blastic cells under pathological conditions can produce tumors related to bone, cementum, and fibrous tissue.[7]
Clinically it presents as a slow growing tumor of the jaw most often seen between the third and fourth decades of life. They occur more frequently in women than in men and the predilection for the site is mostly in the mandibular premolar region.[5] Our case 3 shows the lesion in the posterior region of the mandible in concordance with the previous reports. However, the other two cases were seen in the maxillary region.
The growth is asymptomatic, although the patient may present with a swelling resulting in asymmetry.[5] In our cases, the patients presented with asymptomatic swelling that persisted for a long duration.
Most reports suggest earlier trauma in the area of the lesion. Trauma acts as a predisposing factor which shows that it is not a true neoplasm but possibly, a connective tissue reaction.[5] Various authors have agreed that infection and dental extraction stimulate the periodontal membrane to produce and deposit cementum.[4] Our cases reported here did not reveal any history of trauma in both the maxillary cases; however, case 3 showed COF arising at the extracted site confirming the above findings.
Degree of mineralization determines the radiographic presentation. In the early stages, COF may appear as unilocular or multilocular radiolucent lesion and as the lesion matures, transformation of the lucent lesion in to a radiopaque one takes place resulting in a lesion with mixed density. The margin of the lesion is relatively well defined and shows the presence of sclerotic rim in the host bone as a result of peripheral osteocondensation.[5]
The radiographic pattern for cemento-ossifying fibroma has been described by various authors. Waldron and Giansanti (1973)[8] had reported that COF showed lytic lesions in 26% of cases, 63% were lytic with radiopaque foci, and 12% were diffuse and homogenous appearance. On the contrary, Barberi et al., (2003)[9] catergorized the radiographic pattern as follows: defined lesion without scelorotic rim (40%), defined lesion with sclerotic rim (45%), and lesion with ill-defined border (15%).[8] In our cases, both Case 1 and 3 satisfy the findings of Waldron et al.[8] and Barberi et al.[9] They showed radiopaque foci with a sclerotic rim. In Case 2, there was no sclerotic border visible in the orthopantomograph. However, CT image revealed mixed density with a thick sclerotic rim suggesting an intact cortex involving the maxillary sinus wall.
The important diagnostic feature in COF is that it shows a centrifugal growth pattern, expanding equally in all directions which produces a round tumor mass.[2,3] The CT picture in all our cases show expanded buccal and lingual cortical plates with thinning and intact margins concluding the benign nature of the lesion. There was upward bowing of the floor of the maxillary sinus which is a key diagnostic feature of COF.[3] Most common finding in the mandibular lesion is the inferior bowing of the lower border of mandible.[1] Both these features were expressed in Case 2 and 3, respectively.
Root resorption may be evident. Displacement of the adjacent teeth[1] is also seen in all our cases suggesting that this tumor is in active proliferating stage and is continuously enlarging.
The differential diagnosis which are to be considered are fibrous dysplasia, cement-osseous dysplasia, condensing osteitis, pindborgs tumor, and odontoma.[10]
Fibrous dysplasia has a blending margin with the surrounding bone and has a linear expansion of the cortex. The expanded cortex cannot be in exact parallel relationship, thereby failing to produce a round tumor mass which is seen in COF.[7]
Ccemento-osseous dysplasia show the presence of bony cysts with a wide sclerotic border. Also cemento-osseous dysplasia is multifocal while COF is not.[10]
Vitality test will help in differentiating the COF from condensing osteitis.[5] Pindborgs tumor may be associated with impacted teeth and shows an appearance of driven snow in the radiograph.[2]
Odontoma will show presence of tooth-like structure whereas COF shows a radiopaque foci.[5] Case 2 revealed amorphous calcification along with a supernumerary teeth. The calcified area was thought to be odontoma; however, other features such as mixed density and histopathology confirmed the diagnosis of COF.
Treatment of COF is mainly done by enucleation of small-sized ossifying fibromas and mono-bloc resection with bone reconstruction for larger sized cement-ossifying fibromas. Since it is radio-resistant and to avoid post-radiation complications, radiotherapy is complicated.[1]
Prognosis of this lesion is fair; however, relapse of COF is higher in case of maxillary COF compared to the mandibular ones due to the greater difficulty of their surgical removal and their larger size at the time of presentation.[1]
CONCLUSIONS
The above-discussed three case reports describe the variations in radiological appearances of cement-ossifying fibroma and also highlight the importance of clinical and imaging aspects in diagnosis of COF. Conventional radiographs, as well as specialized radiographs, such as computed tomography help in describing lesions of the jaws in terms of location, expansion of cortical plates, internal architecture, periphery of the lesion, and the effect of the lesion on adjacent structures. Thus, a definitive provisional diagnosis can be arrived at prior to histopathological examination. Imaging also plays a pivotal role in outlining the treatment plan for cement-ossifying fibroma.
Footnotes
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2012/2/1/52/100373
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.White SC, Pharoah MJ. Oral Radiology. 6th ed. China: Mosby Co; 2009. pp. 440–1. [Google Scholar]
- 2.Sarwar HG, Jindal MK, Ahamad SS. Cemento-ossifying fibroma-a rare case. J Indian Soc Pedod Prev Dent. 2008;26:128–31. doi: 10.4103/0970-4388.43195. [DOI] [PubMed] [Google Scholar]
- 3.Langlais RP, Langland OE, Nortje CI. Diagnostic imaging of the jaws. Baltimore: Williams and Wilkins; 1995. p. 555. [Google Scholar]
- 4.Liu Y, You M, Wang H, Yang Z, Miao J, Shimizutani K, et al. Ossifying fibromas of the jaw bone: 20 cases. Dentomaxillofac Radiol. 2010;39:57–63. doi: 10.1259/dmfr/96330046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Galdeano-Areanas M, Crespo-Pinilla JI, Alvarez-Otero R, Espeso-Ferrero A, Verrier-Hernandez A. Fibroma cement-osificante gingival mandibular. Presentication de un caso. Med Oral. 2004;9:176–9. [PubMed] [Google Scholar]
- 6.Macdonald-Jankowaski DS. Fibro-osseous lesions of the face and jaws. Clin Radiol. 2004;59:11–25. doi: 10.1016/j.crad.2003.07.003. [DOI] [PubMed] [Google Scholar]
- 7.Gulati A, Rao NN, Radhakrishnan RA. Fibrous dysplasia and ossifying fibroma-an advent in their diagnosis. J Clin Exp Dent. 2011;3:e297–302. [Google Scholar]
- 8.Waldron CA, Giansanti JS. Benign fibro-osseous lesions of the jaws: A clinico radiologic histologic review of sixty five cases. Oral Surg Oral Med Oral Pathol. 1973;35:340–50. doi: 10.1016/0030-4220(73)90072-8. [DOI] [PubMed] [Google Scholar]
- 9.Barberi A, Cappabianca S, Collela G. Bilateral cement-ossifying fibroma of the maxillary sinus. Br J Radiol. 2003;76:279–80. doi: 10.1259/bjr.76.904.760279. [DOI] [PubMed] [Google Scholar]
- 10.Araki M, Matsumato K, Matsumato N, Honda K, Ohki H, Komiyama K. Unusual radiographic appearance of ossifying fibroma in the left mandibular angle. Dentomaxillofac Radiol. 2010;39:314–19. doi: 10.1259/dmfr/81820042. [DOI] [PMC free article] [PubMed] [Google Scholar]


