Idiopathic orbital inflammation (IOI) is a benign, non-infective clinical syndrome characterized by inflammation of the orbit without identifiable local or systemic disorders.[1] The exact etiology is unknown, but infection and immune mediated processes have been postulated.[1] Peak incidence of the disease is in middle age with females affected more than men.[1,2] It is rare in paediatric population. In adults, IOI tends to be unilateral, but children more commonly present with bilateral disease. Clinical presentation usually is an acute onset of pain, redness, chemosis, proptosis, and periorbital edema. Decreased vision and diplopia can also occur based on the orbital structures involved.[3]
A 38-year-old woman presented to our hospital with acute onset of protrusion of left eye ball associated with left sided headache and peri orbital pain since 2 months. There was no associated visual disturbance. She was a hypertensive on treatment. Ophthalmic examination showed a visual acuity of 6/9 in both eyes. Left eye was proptotic by 4 mm on exophthalmometry and there was modertae limitation of abduction with diplopia on lateral gaze. Minimal conjunctival congestion was noted. Rest of the anterior and posterior segment evaluation was unremarkable. Blood investigations including fasting blood sugar, renal function test, serum creatinine, thyroid function tests, rhematoid factor, and anti nuclear antibody were normal.
CT scan of Brain was normal. Contrast enhanced CT scan of orbit on the left side showed anterior displacement of the globe. There was a non-enhancing soft tissue mass involving the conal and intraconal compartment in the posterolateral aspect of left orbit. The lesion affected lateral rectus and inferior muscle complex and measured 1.3 × 1.1 cm. There was no associated bony destruction or intracranial extension [Figure 1]. CT para nasal sinuses showed opacification of maxillary sinuses more on left side with hypertrophy of the mucosa [Figure 2].
Figure 1.
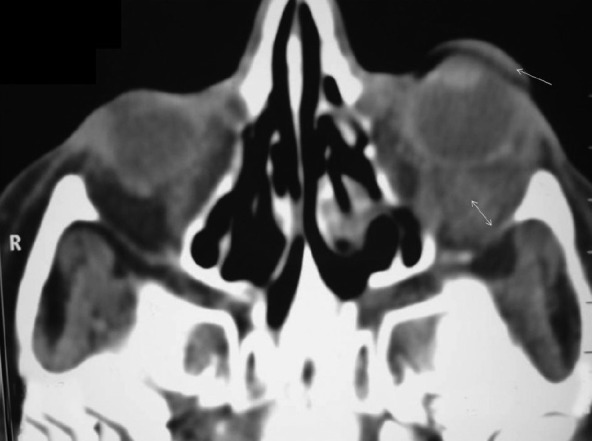
Pre treatment – Contrast enhanced CT scan of orbit axial view showing anterior displacement of the left globe (arrow) and non enhancing soft tissue mass in the left orbit. (double arrow)
Figure 2.
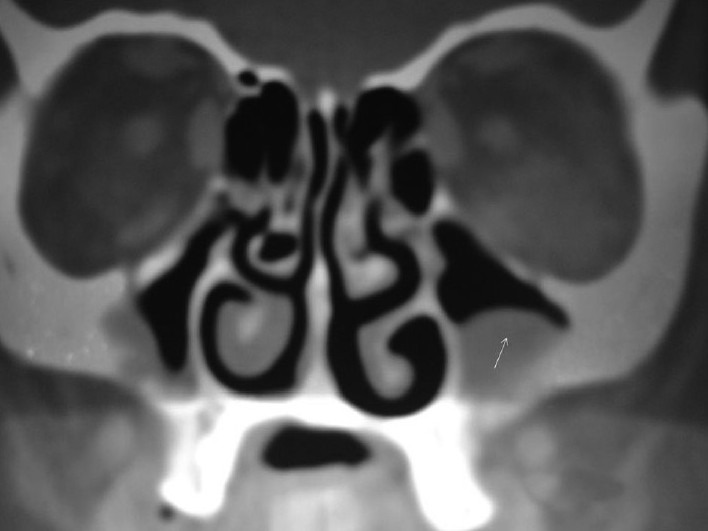
Coronal view of sinuses –maxillary sinus showing haziness and hypertrophy of the mucosa. (arrow)
A provisional diagnosis of left IOI was made based on clinical findings and CT image. The patient was commenced on oral prednisolone 80 mg OD 2 days after a 5 day course of intravenous ceftriaxone 2 gm OD. Antibiotic therapy was initiated in view of the radiological evidence of maxillary sinusitis. After 1 week of treatment with 80 mg, steroids were tapered by10 mg/week and patient was maintained on 10 mg OD for a total duration of 10 weeks. On follow up 6 weeks after commencing treatment she was much better symptomatically with partial resolution of proptosis (3 mm proptosis by exophthalmometry). CT scan of the orbit taken that time showed persistence of the previously reported soft tissue mass with partial resolution. [Figure 3]. On follow up after1 month of stopping steroids the patient was much better symptomatically with reduction in the proptosis and improvement in the motility.
Figure 3.
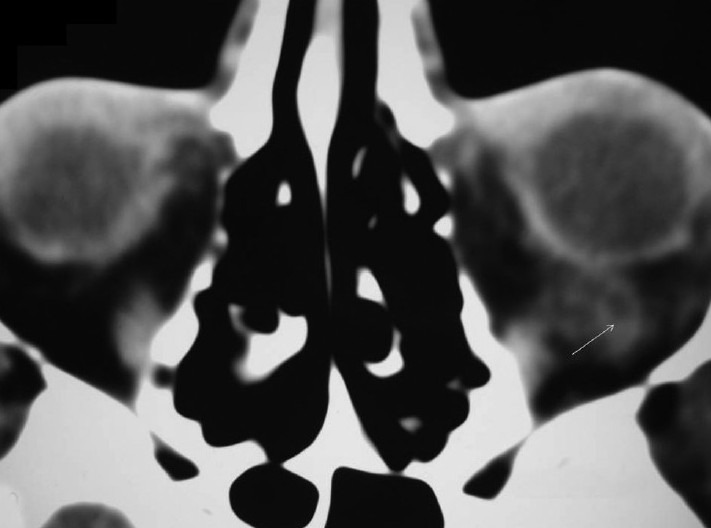
After 6 weeks of starting steroid therapy contrast enhanced CT Scan of orbit axial view showing partial resolution of the soft tissue mass. (arrow)
Contrast, enhanced CT scan of the orbit was repeated after 10 months which showed complete resolution of the soft tissue mass and left proptosis [Figure 4]. Maxillary sinus showed partial resolution of the haziness. This patient is being followed up and is doing well without any recurrence of the symptoms for the last 3 years.
Figure 4.
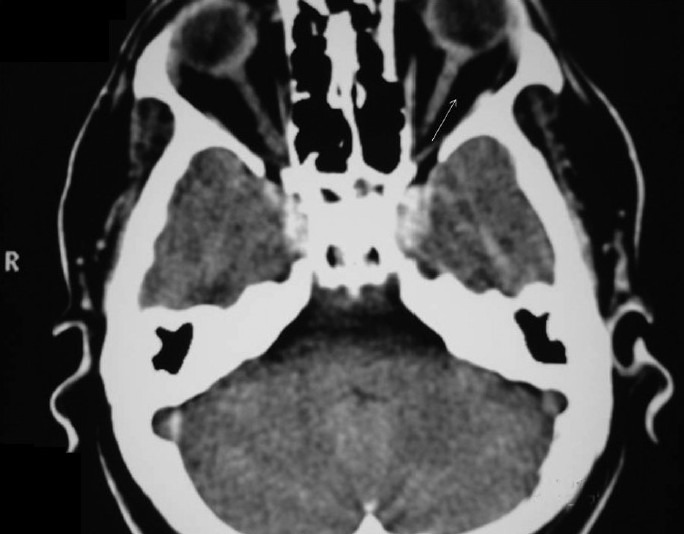
Post treatment – after 10 months – contrast enhanced CT scan of orbit- axial view showing complete resolution of proptosis and soft tissue mass. (arrow)
A recent case control study has shown that idiopathic orbital inflammatory disease is associated with lower socioeconomic status, high BMI, younger age at first child birth, and also use of oral bisphosphonates.[4]
The orbital inflammation is typically nongranulomatous and extra orbital extension is reported in 8.9% of cases.[5] In cases of extraorbital extension biopsy is mandatory to rule out infectious and systemic diseases with clinical similarities. However, chronic and recurrent cases present a diagnostic and therapeutic challenge, as they may masquerade another diagnosis.[6] In bilateral cases lymphoma and thyroid dysfunction have to be ruled out. There is a close histologic resemblance between endocrine exophthalmos and myositic orbital pseudotumor. Even though the clinical tests are negative, the patient may develop thyroid dysfunction later.
Corticosteroids are the cornerstone of therapy in acute cases. Around 37% of patients treated with steroids showed failure to resolve.[7,8] This condition will call for further evaluation including surgical biopsy to rule out other causes such as lymphoma, metastatic disease, and Wegener's granulamatosis.[7,8] In these situations methotrexate, cyclophosphamide, and other anti-neoplastic agents can be used. Radiotherapy is another modality of treatment. An alternative mode of treatment in recurrent and recalcitrant cases is with infliximab which is a TNF-alpha blocker.[6] Clinical improvement with this therapy suggests that TNF mediated inflammation may be involved in the pathogenesis of orbital inflammatory disease. Reactivation of tuberculosis and the possible risk of lymphoma to be kept in mind while treating the patients with infliximab.
Clinically our case appears to be the nonsclerosing type (abrupt onset, absence of bony destruction and intracranial extension, and the dramatic response to systemic steroids).[9] Simultaneous occurrence of paranasal sinusitis and IOI disease has been reported in the literature. Our experience with this case highlight the fact that a diagnosis of IOI disease can be reached with simple clinical judgement combined with radiological evaluation. A swift response to steroids is confirmatory and eliminates the need for invasive investigational procedures like orbital biopsy.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Yuen SJ, Rubin PA. Idiopathic orbital Inflamation: Ocular mechanism and clinicopathology. Ophthalmol Clin North Am. 2002;15:121–6. doi: 10.1016/s0896-1549(01)00003-7. [DOI] [PubMed] [Google Scholar]
- 2.Weber AL, Romo LV, Sabates NR. Pseudotumor of the orbit.Clinical, pathologic, and radiologic evaluation. Radiol Clin North Am. 1999;37:151–68. doi: 10.1016/s0033-8389(05)70084-1. [DOI] [PubMed] [Google Scholar]
- 3.Golnik KC. Neuro-opthalmologic manifestation of systemic disease: Rheumatology/inflammatory. Ophthalmol Clin North Am. 2004;17:389–96. doi: 10.1016/j.ohc.2004.05.004. [DOI] [PubMed] [Google Scholar]
- 4.Bijlsma WR, van Gils CH, Paridaens D, Mourits MP, Kalmann R. Risk factors for idiopathic orbital inflamation:A case-control study. Br J Ophthalmol. 2011;95:360–4. doi: 10.1136/bjo.2009.175190. [DOI] [PubMed] [Google Scholar]
- 5.Mahr MA, Salomao DR, Garrity JA. Inflamatory orbital pseudotumor with extension beyond the orbit. Am J Ophthalmol. 2004;138:396–400. doi: 10.1016/j.ajo.2004.04.026. [DOI] [PubMed] [Google Scholar]
- 6.Garrity JA, Coleman AW, Matteson EL, Eggenberger ER, Waitzman DM. Treatment of recalcitrant idiopathic orbital inflamation (chronic orbital myositis) with Infliximab. Am J Ophthalmol. 2004;138:925–30. doi: 10.1016/j.ajo.2004.06.077. [DOI] [PubMed] [Google Scholar]
- 7.Rubin PA, Foster CS. Etiology and management of idiopathic orbital inflammation. Am J Ophthalmol. 2004;136:1041–3. doi: 10.1016/j.ajo.2004.09.032. [DOI] [PubMed] [Google Scholar]
- 8.Jabs DA, Rosenbaum JT, Foster S. Perspective; Guidelines for the use of Immunosupressive drugs in patients with ocular Inflamatory disorderes. Am J Ophthalmol. 2000;130:492–513. doi: 10.1016/s0002-9394(00)00659-0. [DOI] [PubMed] [Google Scholar]
- 9.Scott IU, Siatkowski RM. Idiopathic orbital myositis. Curr Opin Rheumatol. 1997;9:504–12. doi: 10.1097/00002281-199711000-00005. [DOI] [PubMed] [Google Scholar]


