Abstract
Purpose.
We determined whether the street-crossing decisions of subjects with age-related macular degeneration (AMD) were as accurate and precise as those made by young and older subjects with normal vision.
Methods.
Street-crossing decisions in 13 AMD subjects, and 20 young and 20 older control subjects with normal vision were measured along an un-signalized street for nine different gap times. After calculating the discriminability (d') of the street-crossing decision variable for all gap pairs and entering these d' values into a one-dimensional scaling model, the means of each distribution of the decision variable relative to a “center of gravity” were estimated and plotted against gap time. The resultant plot was a nonlinear function. Street-crossing decision accuracy was computed for each subject as the difference between the x-intercept of the nonlinear function (tCOG) and subjects' measured street-crossing time. Street-crossing decision-making precision was computed as the value of the slope of the nonlinear function at tCOG.
Results.
We found that all subjects were precise in their street-crossing decisions (P = 0.55). Significant differences in street-crossing accuracy were found as a function of age (P = 0.003). Compared to either the older normally-sighted (P = 0.018) or AMD (P = 0.019) subjects, the young normally-sighted subjects made the least accurate street-crossing decisions. No significant difference in accuracy was found between the AMD and age-matched normally-sighted subjects (P = 0.90).
Conclusions.
Our data suggested that age and mild central vision loss did not affect significantly a subject's precision in their street-crossing decisions. Age, but not mild central vision loss, significantly affected a subject's accuracy in their street-crossing decisions.
We found that AMD subjects were just as accurate and precise as age-matched normally-sighted subjects in making street-crossing decisions. Our results also indicated that age had a significant effect on street-crossing decision-making accuracy but not on precision.
Introduction
Transportation technology is driven continually to new heights, allowing humans to move about more efficiently and arguably more safely than ever before. However, people still need to cross the street on a daily basis. The task of street-crossing is complex and dangerous, as evidenced by the high number of reported pedestrian injuries and fatalities. In the United States during 2009, a pedestrian was killed on average every 2 hours and injured every 9 minutes, with 24% of all pedestrian fatalities occurring at an intersection.1
A key factor involved with making safe street-crossing decisions is vision. Previous street-crossing studies have shown that visually impaired and blind pedestrians, in comparison with normally-sighted pedestrians, make significantly more unsafe street-crossing decisions,2,3 identify significantly fewer crossable gaps,2–4 take significantly longer to identify a crossable gap,2,4–6 and have significantly reduced safety margins.5 Collectively, the results of these earlier studies demonstrate that pedestrians with vision loss are potentially at risk when crossing the street in part because of their vision loss.
In the Western world, age-related macular degeneration (AMD) is the leading cause of untreatable visual impairment in people aged 65 years and over.7–9 People with AMD may experience a partial or complete loss of their central vision. They may have significantly impaired visual functions, such as visual acuity (VA)10,11 and contrast sensitivity (CS),11–13 and often have scotomas,10,14 which are areas of central visual field (VF) loss in spatially defined locations. The prevalence of AMD increases with age.15–17 This fact, combined with an aging US population,18 will result in a significant increase in the number of older adults with AMD. Consequently, there will be increasingly more pedestrians with vision loss from AMD attempting to cross the street. Therefore, evaluating how accurate and precise pedestrians with AMD are at making safe street-crossing decisions is a very real and urgent issue that must be addressed.
Surprisingly, to our knowledge, only one previous study has assessed directly the street-crossing performance of pedestrians with AMD.5 Geruschat et al. measured the ability of ten subjects with AMD, 14 normally-sighted subjects, and 17 subjects with peripheral VF loss, either from retinitis pigmentosa (RP) or glaucoma, to detect crossable and short gaps in vehicular traffic at an entry and exit lane of a two-lane urban roundabout.5 They found no significant difference between the AMD and age-matched, normally-sighted subjects in their ability to detect correctly crossable vehicular gaps, reject correctly uncrossable vehicular gaps, and detect the number of missed crossing opportunities (i.e., rejecting a vehicular gap time when it was long enough for a crossing). Therefore, these results suggest that despite their vision loss, subjects with AMD are still able to identify accurately crossable and uncrossable vehicular gaps in traffic.
However, the results of Geruschat et al.5 may be biased whereby the ability of the AMD subjects to identify accurately crossable and uncrossable gaps is inflated. This is because in their study there was an over-representation of short, uncrossable vehicular gap times assessed. Geruschat et al. reported that subjects were exposed to a median of 50 crossable gaps and 210 uncrossable gaps.5 The high number of uncrossable gaps occurred most likely because their study was conducted at a high volume roundabout where the constant flow of vehicles resulted in an over-representation of short, uncrossable gaps. In addition, the average ± SD of street-crossing times (combining entry and exit lanes) for their AMD, peripheral VF loss, and normally-sighted subjects were 9.41 ± 2.24, 8.06 ± 2.17, and 6.92 ± 1.77 seconds, respectively. This means that a crossable gap in their study had to be longer in duration than these average crossing times. Consequently, the crossable gap times in the study of Geruschat et al. are very long, especially at a high volume roundabout.5
Therefore, it is possible that it was easy for subjects in the study of Geruschat et al. to determine accurately whether the gap time was short or crossable because the gap times assessed were at extreme ends, either very short or very long in duration.5 The study's easy gap discrimination task may explain why their AMD subjects achieved such high detection rates of uncrossable and crossable vehicular gap times, and hence why no significant difference was found between the AMD and age-matched normally-sighted subjects in their gap detection ability.
Evidence suggesting that subjects with AMD do experience difficulties with making street-crossing decisions is found in their ability to gauge correctly their safety margin as well as how long it takes them to identify a crossable gap. Geruschat et al. found that, compared to the age-matched normally-sighted subjects, the AMD subjects took significantly longer to detect a crossable gap (i.e., increased latency) and they had significantly larger negative safety margins, whereby the AMD subjects did not allow themselves enough time to cross the street.5 Thus, their study demonstrated that AMD subjects are at risk for making unsafe street-crossing decisions when determining crossable vehicular gaps.
Given that subjects with AMD are at risk for making unsafe street-crossing decisions,5 the steady growth in the prevalence of AMD, and the lack of empirical studies assessing the street-crossing performance of AMD subjects, more research is required to systematically assess the gap detection and discrimination ability of subjects with AMD. The aim of our study was to measure and compare the accuracy and precision of street-crossing decisions made by young and older subjects with normal vision to subjects with varying degrees of vision loss from AMD over a wide range of vehicular gap times. We hypothesized that the street-crossing decision-making performance of the normally-sighted subjects, irrespective of age, would be significantly better than the performance of the AMD subjects. We also hypothesized that as the level of vision loss from AMD increased (characterized by worsening VA and CS, and increasing scotoma size), the level of accuracy and precision in AMD subjects' street-crossing decision-making performance would also decline.
Methods
Subjects
A total of 53 adult subjects participated in the study; 13 subjects with either dry or wet AMD, 20 young control subjects with normal vision, and 20 older control subjects with normal vision. The normally-sighted subjects were recruited from the local community or through a relationship with another subject. The AMD subjects were recruited from the Indiana University School of Optometry's Primary Care and Vision Rehabilitation Service clinics. Significant differences in age existed between the normally-sighted and AMD subject groups (1-way ANOVA, F(2,52) = 681.20, P < 0.001). As expected, the young normally-sighted subjects were significantly younger than the older normally-sighted (independent t-test, t(1,38) = 29.36 P < 0.001) and AMD (independent t-test, t(1,31) = 24.98, P < 0.001) subjects. The older normally-sighted subjects did not differ in age from the AMD subjects (independent t-test, t(1,31) = −0.15, P = 0.89).
Three visual functions were assessed in each subject: VA, CS, and VF. The average results of these assessments for all three subject groups are presented in Table 1.
Table 1. .
Subject Characteristics
|
Subject Group |
# of Subjects |
Age, y* |
Vision Function* |
|||
|
Binocular Visual Acuity, Log MAR |
Binocular Contrast Sensitivity, Log CS |
Average VF Extent Radius in Better Eye, deg |
Average Scotoma Radius in Better Eye, deg |
|||
| Young normally-sighted | 20 | 25.25 ± 2.16 | −0.15 ± 0.06 | 1.66 ± 0.03 | 56.25 ± 6.37 | NA |
| Older normally-sighted | 20 | 79.14 ± 7.92 | 0.03 ± 0.13 | 1.56 ± 0.11 | 40.04 ± 9.91 | NA |
| AMD | 13 | 78.74 ± 7.52 | 0.53 ± 0.47 | 1.24 ± 0.38 | 40.49 ± 13.10 | 1.44 ± 2.21 |
NA, not applicable.
Results listed as mean ± 1 SD.
Each subject's binocular VA was assessed using an Early Treatment Diabetic Retinopathy Study (ETDRS) acuity chart,19 which was transilluminated to approximately 100 candela/m2 (cd/m−2). Each subject's threshold binocular VA was reported as the logarithm of the minimum angle of resolution (log MAR) using the scoring of Bailey et al.20 As expected, significant differences in binocular VA were found across the groups (1-way ANOVA, F(2,52) = 36.40, P < 0.001). Specifically, the young normally-sighted subjects had significantly better binocular VA than either the older normally-sighted (independent t-test, t(1,38) = 6.03, P < 0.001) and AMD (independent t-test, t(1,31) = 5.18, P = 0.0002) subjects, and the AMD subjects had significantly worse binocular VA than the older normally-sighted subjects (independent t-test, t(1,31) = 3.69, P = 0.003).
A Pelli-Robson letter contrast sensitivity chart21 positioned at 1 m with overhead illumination of 85 cd/m−2 was used to measure the binocular CS in each subject. The binocular threshold log CS was determined using the scoring of Elliott et al.22,23 Significant differences in the binocular CS were found across groups (Kruskal-Wallis 1-way ANOVA, χ22 = 34.96, P < 0.001). The binocular CS of the young normally-sighted subjects was significantly better than the older normally-sighted (Wilcoxon rank sums test, z = −4.51, P < 0.0001) and AMD (Wilcoxon rank sums test, z = −4.95, P < 0.0001) subjects. The binocular CS of the AMD subjects was significantly worse than the older normally-sighted subjects (Wilcoxon rank sums test, z = −3.12, P < 0.0001).
Kinetic perimetry was performed on each subject using a Goldmann bowl perimeter (III4e target on a background luminance of 10 cd/m−2) to assess monocular VFs along 24 meridians from radii of 700 vertically and 900 horizontally. Located inside the bowl of the Goldmann perimeter was a central target on which subjects were instructed to fixate. The AMD subjects were instructed to use eccentric fixation, presumably with their preferred retinal locus (PRL), during the VF assessment. VF extent and the position of any central scotomas were recorded for all subjects. The average VF extent (radius) in each eye was computed for each subject by averaging the VF extent along each meridian. The eye that had the greatest average VF extent (radius) was reported as the average VF extent (radius) in the better eye. Significant differences in the average VF extent (radius) in the better eye were found across the groups (1-way ANOVA, F(2,51) = 17.16, P < 0.001). Specifically, the young normally-sighted subjects had a significantly larger average VF extent in the better eye than either the older normally-sighted (independent t-test, t(1,38) = −6.15, P < 0.001) and AMD (independent t-test, t(1,31) = −3.90, P = 0.002) subjects. The average VF extent in the better eye of the AMD subjects did not differ from the older normally-sighted subjects (independent t-test, t(1,30) = 0.11, P = 0.92).
The extent, position, and size of any central scotomas within the central 300 radius VF along 12 meridians was also assessed in all subjects' right and left eyes using a Bjerrum (tangent) screen with a 5/1000 W Traquair target. The Bjerrum (tangent) screen had a screen illuminance of 112 lux. Subjects wore their own distance prescription and were instructed to fixate on a large, centrally located letter “E” target. The AMD subjects were instructed to use eccentric fixation, presumably with their PRL, during the VF assessment. The average radius of the scotoma in each eye, in degrees, across the eight principal meridians of the scotoma were computed. The eye that had the smallest average scotoma (radius) was reported as the average scotoma size (radius) in the better eye. As expected, the age-matched younger and older normally-sighted subjects had no central scotomas, while five of the 13 AMD subjects had a scotoma in the better eye that was on average (SD) 1.440 (2.210) in radius.
For this study, subjects were required to self-report being independent travelers who regularly crossed streets unaided and who self-reported having no history of a physical disorder that affected their walking abilities. Subjects also were required to have good cognitive function as determined by obtaining a score of 24 or greater on the Mini-Mental State Exam (MMSE).24 All subjects were unfamiliar with the intersection used in the study.
Informed consent was obtained from each subject after the nature and possible consequences of the study were described. The study followed the tenets of the Declaration of Helsinki and was approved by the Institutional Review Board of Indiana University.
The Street Test Site
The test site used in our study was an un-signalized, urban, two-way street located within Bloomington, IN. Each lane was ∼4.50 m wide and the two lanes were separated by a 4.70-m wide median strip (Fig. 1). Subjects stood along the curb of one of the lanes at a location called the “crossing point” and were required to make street-crossing decisions where the traffic approached from just one direction. The crossing point location did not change throughout the study. The street used in the study was selected for its steady flow of traffic as well as for its minimal visual and auditory distractions.
Figure 1. .
The un-signalized street used in our study to assess street-crossing decision-making ability. In the foreground on the left-hand side is one of the sensors that was used to calculate the vehicular gap times. The stool on the left-hand side is positioned by the crossing point where subjects made their street-crossing decisions.
Vehicular Gap Time Measurements
The methods used to measure the vehicular gap times have been described previously.25 In summary, two custom-made sensors were used to compute the vehicular speeds and gap times of approaching vehicles. Each sensor comprised a 15 × 15 cm water- and light-proof box that contained two identically sized and vertically orientated apertures at the front of the box. Behind each aperture were two identical optical systems that focused entering light onto two photodetectors positioned at the rear of each box. The sensors were positioned along the curb on the same side of the street where subjects stood to make their street-crossing decisions, approximately 0 and 15 m to the right of the crossing point. Positioned on the other side of the street along the curb of the median strip, were two low-powered lasers (<5 mW) that were aligned with the bottom aperture (photodetector) in each sensor. The lasers and sensors were positioned at the approximate height of a passing vehicle's bumper bar using tripods, and the sensors sent their recorded information to a portable computer via serial cables.
The photodetectors continuously recorded the incident light intensity and the readings were sent to a portable computer. Unlike the top optical path, which was exposed to ambient (environmental) light only, the bottom optical path was exposed to ambient light in addition to the light emitted from the laser. To improve the detection of the laser beam, intensity readings from the top photodetector were subtracted from the intensity readings from the bottom detector. Whenever the path of the laser beam was interrupted by an approaching vehicle, the event was recorded and time stamped. Vehicular velocity was computed by dividing the known distance separating the two sensors by the time difference between the two sensor signals. The physical gap time was calculated as the difference between the time of the “prompt” signal (refer to the Experimental Procedure below for an explanation of the “prompt” signal) and the time the approaching vehicle was detected first by the sensor positioned at the crossing point.
Experimental Procedure
The experimental procedure used to record subjects' street-crossing decisions has been reported previously.25 In summary, to provide subjects with pertinent information about the distance and the time required to cross the street physically, subjects crossed the street four times at their usual street-crossing pace before any street-crossing decisions were recorded. Subjects were always accompanied by an experimenter while they crossed the street and these measurements also were used later when analyzing the accuracy of each subject's street-crossing decisions.
Subjects were required to make street-crossing decisions using their habitual vision and hearing while they stood at the crossing point. Even though up to four subjects could be assessed concurrently, the average number of subjects who were tested in a typical experimental session in our study was three. When there was more than one subject being tested in a given session, subjects were staggered around the crossing point so as not to obstruct the vision and hearing of another participating subject.
At the commencement of each trial, subjects were instructed to direct their head forward with their eyes closed while wearing earbuds that played white noise. This was done to prevent subjects from sampling pertinent visual and auditory street-crossing information before a street-crossing decision had to be made. When subjects heard an audible “get ready” signal, which was delivered through the earbuds, the white noise stopped playing and subjects were instructed to immediately turn their head to “view” and “listen” to gaps in vehicular traffic for two seconds. A two second “sampling period” was selected because normally-sighted and low vision subjects have been shown to require between 1 and 1.7 seconds to make a street-crossing decision.5 Individual latency times (i.e., the time required to make a street-crossing decision) were not measured in our study. The latency period for all subjects in our study was the two-second sampling period.
At the end of this sampling period, an audible “prompt” signal was given through the earbuds, upon which the white noise resumed playing. Upon hearing the “prompt” signal, subjects were required immediately to close their eyes and turn their head so that it again faced forward while concurrently giving their street-crossing decision. Pilot testing revealed that the ability of subjects to hear traffic during the two-second sampling period was not significantly affected while wearing the earbuds.
The street-crossing decision was based on the subject's perception of whether or not there was enough time to cross at the time of the prompt signal. Thus subjects, at the time of the prompt signal, were required to judge whether the vehicular gap time between them and a single approaching vehicle was longer or shorter in duration than their crossing time. Subjects used a 5-point rating scale when making their street-crossing decision: rating 1 – subjects felt that at the time of the prompt signal there definitely was not enough time to cross, rating 2 – there probably was not enough time to cross, rating 3 – subjects were unsure whether or not there was enough time to cross at the time of the prompt signal, rating 4 – there probably was enough time to cross at the time of the prompt signal, and rating 5 – there definitely was enough time to cross. Subjects' street-crossing decisions (ratings) were recorded automatically using custom software as they pressed a button apparatus that was attached to a portable computer. Therefore, subjects gave their ratings independently of each other and pressed the button apparatus the same number of times corresponding to the desired rating number.
Street-crossing decisions were collected for nine different categories of vehicular gap times. Vehicular gap times that ranged from 0 to 1 second in duration were binned into gap time category “1.” Vehicular gap times that ranged from 1 to 2 seconds in duration were binned into gap time category “2.” The process of binning the vehicular gap times into one-second increments continued for the remaining seven gap time categories with the final gap time category binning all vehicular gap times equal to or longer than 8 seconds as gap time category “9.” The vehicular gap time was determined as the duration in time between the “prompt” signal and when the first approaching vehicle reached the crossing point. To collect street-crossing decisions for each gap time category, the time at which the “prompt” signal was given varied across trials and was estimated from the approaching vehicle's speed. A minimum of 10 trials were collected for each gap time category and unlike in the study of Geruschat et al.,5 there was an even distribution of trials in each of the nine gap time categories assessed. Dividing the assessed gap times into “crossable” and “short” gap times as defined by Geruschat et al.,5 our study had a total of 3253 crossable gaps and 2622 short gaps.
The vehicular gap times were based on the day-to-day traffic flow of vehicles traveling along the test street. Sources of variability arising from varying vehicular speeds, and acoustic variations from different vehicle makes and models across trials did not need to be controlled as they simply combined with all other sources of variability in the decision variable.25 The average velocity (SD) of the vehicles used to generate the different vehicular gap times in our study was 43.8 (10.3) km/h. The test street had a sign posted vehicular speed limit of 48.3 km/h (≡ 30 miles/h).
Subjects also were instructed to give their rating immediately following the prompt signal (to prevent additional sampling of sensory information), assume that they were crossing the street at their regular walking pace, never assume that the approaching vehicle(s) will slow down or yield to them, and never give a response (rating) when something prevented them from making a judgment (e.g., a lapse in attention, or they sneezed).
Acknowledging that masking sounds can interfere with a subject's ability to make street-crossing decisions, trials were conducted only when the experimenter believed that there were minimal background (masking) sounds present. If there was a sudden change in background noise during a trial (e.g., a paramedic siren sounded), that trial was aborted and not used in any data analyses.
Before the collection of any street-crossing decisions, practice trials were given until the subject demonstrated to the experimenter that the instructions and experimental task were understood and could be implemented. Test sessions typically were conducted between 9 a.m. and 12 p.m., and only on days with clear weather (i.e., never on days when there was fog, snow, or rain (including drizzle), or when it was dark). The average ± SD temperature across all test days was 24 ± 3°C.
Data Analysis
The outcome measures used to quantify subjects' level of accuracy and precision in street-crossing decision-making were bias and the slope of a nonlinear function, respectively. These two outcome measures have been developed and validated previously.25 In summary, using each subject's crossability ratings data, receiver operating characteristic (ROC) curves were estimated for all possible gap pairs. The discriminability (d') of the street-crossing decision variable for each subject was estimated by computing the area under each ROC curve for all 36 gap pairs and converting these results into 36 different z scores. The means of each distribution of the decision variable for the nine different gap time categories were estimated relative to a “center of gravity” (COG) by inputting the 36 d' values into a one-dimensional scaling model (i.e., a Guttman loss function).
Plotting the estimated means of the nine distributions of the decision variable relative to the COG as a function of gap time revealed that the data were characterized as a nonlinear function. Using nonlinear regression, the best fitting nonlinear function was estimated for each subject.
From each subject's best-fitting nonlinear function two measurement parameters were calculated: the x-intercept, referred to as tCOG, and the derivative of the nonlinear function at tCOG. The tCOG is the time (in seconds) at which the subject transitions from classifying gap times as being “not enough time to cross” to being “enough time to cross.”25 Subtracting each subject's averaged street-crossing time from their x-intercept (tCOG) is a measure of the level of accuracy in each subject's street-crossing decision-making.25 Better accuracy in street-crossing decision-making is quantified as having a bias value that is close or equal to zero.25 A positive bias value implies that although the person is less accurate in their street-crossing decision-making ability they are more risk averse in their decision-making. A negative bias value implies that the person is inaccurate and risky when making street-crossing decisions as they classify gap times that are shorter in duration than their actual crossing time as being “enough time to cross.”25
A measure of subjects' precision in their street-crossing decision-making is provided by the derivative of the nonlinear function at tCOG.25 When the slope is steep (i.e., a large derivative value) this can be interpreted to mean that the subject is precise in their street-crossing decision-making. This is because the subject's criterion for crossing changes quickly over a small range of vehicular gap times. The converse is true for subjects with shallow slopes or small derivative values.
To assess whether subjects were accurate in their street-crossing decision-making, the distribution of bias values for each subject group was tested to determine if it were significantly different from zero using the Wilcoxon signed-rank test. (The distributions of bias values were not normal.) Wilcoxon rank sum tests also were performed to look for significant differences in bias values between subject groups. Spearman correlations also were performed to look for any relationship between subjects' bias values and age and vision measures (VA, CS, VF extent, and scotoma size).
Wilcoxon rank sum tests were also performed on the derivative values at tCOG to look for significant differences in precision between subject groups. (The distributions of derivative values at tCOG were not normal.) Spearman correlations also were performed to assess for any relationship between derivative values at tCOG and age and vision measures (VA, CS, VF extent, and scotoma size).
With the exception of the one-dimensional scaling modeling, which was performed using SYSTAT10 (SPSS Inc., Chicago, IL), all statistical analyses, including the nonlinear regressions, were performed using JMP 8.0 (SAS Institute Inc., Cary, NC). Nonparametric statistical analyses were performed on data distributions that were not normal, while parametric statistical analyses were performed on normally-distributed data.
Results
Accuracy in Street-Crossing Decision-Making
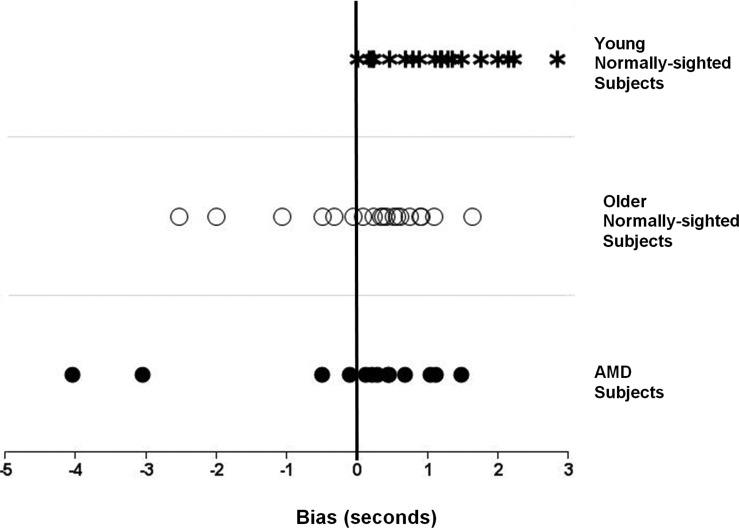
The median (and 25th and 75th percentiles) bias values for the three different subject groups are listed in Table 2 and illustrated in Figure 2.
Table 2. .
The Median (and 25th and 75th Percentiles) of Bias (Measure of Accuracy) and Derivative of Nonlinear Function at tCOG (Measure of Precision) Values Measured in Each Subject Group
|
Subject Group |
Street-Crossing Decision Outcome Variable |
|
|
Bias, s |
Derivative of Non-Linear Function at tCOG |
|
| Young normally sighted | 1.14 (0.45, 1.68) | 0.62 (0.50, 0.79) |
| Old normally sighted | 0.36 (−0.27, 0.70) | 0.57 (0.35, 0.76) |
| AMD | 0.29 (−0.30, 0.86) | 0.59 (0.48, 0.82) |
tCOG, the time in seconds at which the subject's response transitions from “not enough time to cross” to “enough time to cross.”25
Figure 2. .
Plot of street-crossing bias values measured in each subject group shows the distribution of bias values for each subject group. There is a tendency for the older normally-sighted and AMD subjects to have more negative bias values compared to the young normally-sighted subjects. Negative bias values represent an unsafe street-crossing strategy, while positive bias values represent a safe street-crossing strategy.
The bias values of the older, age-matched normally-sighted and AMD subjects were on average not significantly different from zero (Wilcoxon signed-rank test, z = 35.00, P = 0.20 and z = 12.50, P = 0.41 for the older normally-sighted and AMD subjects, respectively). Thus older adults, even those with central vision loss from AMD, were relatively accurate at making street-crossing decisions. The bias values of the young normally-sighted subjects were on average significantly different from zero (Wilcoxon signed-rank test, z = −16.00, P = 0.02). However the median and 25th and 75th percentile bias values were all positive (Table 2 and Fig. 2), indicating that the young normally-sighted subjects allowed themselves enough time to cross. Positive bias values represent a safe street-crossing strategy, while negative bias values represent an unsafe street-crossing strategy.
No significant difference in bias values were found between the older normally-sighted and AMD subjects (Wilcoxon rank sum test, z = −0.13, P = 0.90). The bias values of the young normally-sighted subjects were significantly different from the older, normally-sighted subjects (Wilcoxon rank sum test, z = −3.02, P = 0.003) as well as to the AMD subjects (Wilcoxon rank sum test, z = −2.75, P = 0.006).
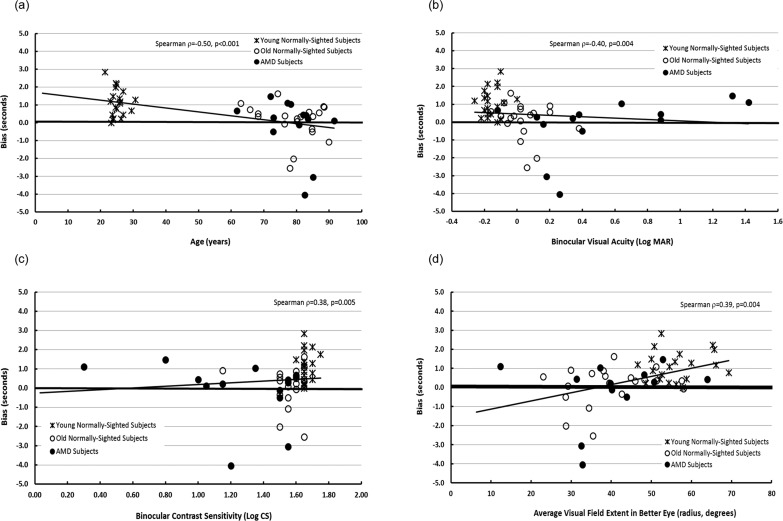
As expected, scores on the various vision tests were related to one another since significant correlations were found between many of the vision measures (Table 3). Similarly, we found that accuracy in street-crossing decision-making (quantified by bias) was correlated to precision in street-crossing decision-making (quantified by the derivative value of the nonlinear function at tCOG, Table 3). Significant correlations also were found between the level of accuracy (quantified by bias) in subjects' street-crossing decisions and age, and all measures of vision assessed in our study with the exception of the size of a binocular scotoma, (i.e., VA, CS, VF extent). The Spearman rho and P values of all correlations are detailed in Table 3, and selected correlations are illustrated in Figure 3.
Table 3. .
Correlation Matrix Listing Spearman Rho (ρ) between Street-Crossing Accuracy (Quantified by Bias), Precision (Quantified by the Derivative of a Non-Linear Function at tCOG), Age, and Vision Measures
|
|
1 |
2 |
3 |
4 |
5 |
6 |
| Age | ||||||
| Binocular VA | 0.7039* | |||||
| Binocular CS | −0.7000* | −0.8425* | ||||
| Average VF extent (radius) in better eye | −0.6829* | −0.5698* | 0.6806* | |||
| Average monocular scotoma size (radius) in better eye | 0.2474‡ | 0.4283† | −0.4461* | −0.1076‡ | ||
| Precision (derivative of a non-linear function at tcog) | −0.1940 | −0.0837‡ | 0.2490‡ | 0.3269 | −0.0964‡ | |
| Accuracy (bias) | −0.4934* | −0.3927† | 0.3824† | 0.3920† | −0.0542‡ | 0.2135‡ |
P < 0.001.
P ≤ 0.01.
P > 0.05.
Figure 3. .
Scatterplots between street-crossing accuracy (quantified by bias) and age and binocular VA, CS, and average VF extent – better eye. Positive and negative bias values represent a safe and unsafe street-crossing strategy, respectively.
Precision in Street-Crossing Decision-Making
The median (and 25th and 75th percentiles) derivative values of the nonlinear function at tCOG for the three different subject groups are listed in Table 2.
No significant differences in the level of precision were found between the different subject groups (Kruskal-Wallis 1-way ANOVA, χ22 = 1.21, P = 0.55). Therefore, subjects on average displayed similar levels of precision in their street-crossing decision-making irrespective of their age or vision status.
The only significant correlation found between vision and the level of precision in subjects' street-crossing decision-making performance was with the average binocular VF extent (Spearman r = 0.35, P = 0.01, Table 3).
Discussion
The primary aim of our study was to compare the street-crossing decision-making performance of young and older subjects with normal vision to that of subjects with varying degrees of vision loss from AMD. We found no significant difference in the accuracy and precision of street-crossing decisions between the AMD and older (age-matched) control subjects with normal vision. We also found that the distribution of bias values for both these subject groups were not significantly different from zero. Collectively, these findings suggest that the street-crossing decision-making performance of the AMD subjects were comparable to that of the normally-sighted age-matched control subjects. As a result, it appears that subjects with central vision loss from AMD, using their hearing and habitual impaired vision, are able to compensate for their vision loss regarding their ability to make judgments about when it is safe to cross the street.
The performance of the AMD and age-matched normally-sighted subjects in our study agree with the results of Geruschat et al.5 who assessed a smaller number and range of gap times compared to those assessed in our study. Geruschat et al. found no significant difference between AMD and age-matched, normally-sighted subjects in their rates of correctly identifying crossable and uncrossable vehicular gaps, as well as their rate of missing street-crossing opportunities (i.e., incorrectly rejecting vehicular gap times that were long enough for a crossing).5
Our results also indirectly supported the findings of Hassan,26 who found no significant difference in street-crossing decision accuracy and precision between ten visually impaired and 13 age-matched subjects with normal vision. While the visually impaired subjects of Hassan's study did not suffer from AMD, they did have central vision loss, since their subjects were all legally-blind based on VA.26
A possible explanation as to why our study and others5,26 have found that subjects with either AMD or central vision loss appear to be as good as age-matched normally-sighted subjects in making safe and accurate street-crossing decisions, may relate to the visual functions that were used by subjects to make street-crossing decisions. It is possible that the AMD subjects in our study compensated for their central vision loss by using their remaining peripheral VF to estimate the time required to cross the street and the vehicular gap time. However, this statement would need to be verified with further research, since we did not measure the gaze behavior of subjects in our study. The importance of the peripheral VF in street-crossing decision-making at un-signalized streets has been shown previously by Cheong et al.,3 who reported that subjects with severe peripheral VF loss had significantly impaired performance compared to age-matched controls with normal vision when making street-crossing decisions.
The AMD subjects evaluated in our study only experienced mild visual impairment from AMD. The mean binocular VA of the AMD subjects was ∼20/60−1 (≅0.53 log MAR, Table 1) and only five out of the 13 AMD subjects had a monocular scotoma in at least one eye. Therefore, it is possible that the ability of AMD subjects to make accurate and precise street-crossing decisions may be preserved until very late in the disease when the VA and CS are impaired severely, and when large central scotomas are present. This may explain why we found no significant difference in performance between our age-matched normally-sighted subjects and those with mild visual impairment from AMD. Geruschat et al.5 also found no significant difference in street-crossing decision-making ability between their AMD and age-matched normally-sighted subjects. Interestingly, their AMD subjects were moderately visually impaired, since the mean binocular VA of their AMD subjects was ∼20/120 (≅0.80 log MAR). Consequently, more research with a larger number of subjects, including those with more severe visual impairment, is required to evaluate fully the effects of vision loss from AMD on street-crossing decision-making performance.
Another possible explanation of our results may relate to the complexity of the street-crossing environment/task used in our study. Subjects in our study made street-crossing decisions where a single lane of traffic approached from just one direction. In the study of Geruschat et al.,5 street-crossing decisions were measured as subjects monitored two lanes of traffic approaching from just one direction. Interestingly, both their study5 and our study found no significant difference in street-crossing decision-making performance between the age-matched normally-sighted and AMD subjects. In contrast, Cheong et al.3 measured street-crossing decisions along a two-way street, and found a significant difference in performance between their peripheral VF loss and age-matched control subjects. While the vision loss of their low vision subjects is different from that experienced by AMD subjects, it is possible that a contributing factor for the significant difference in performance between their subject groups may have been due to the more complex street-crossing environment of the two-way street. Making crossing decisions where traffic approaches from just one direction, as was the case in our study, may be an easier task for pedestrians compared to making crossing decisions when two vehicles are approaching from opposite directions, like that at a two-way street. Oxley et al.27 showed that the complexity of the street-crossing environment can influence crossing behavior in normally-sighted subjects. They found that on a one-way street, the crossing behavior of young and elderly normally-sighted pedestrians was similar, while on a two-way street, the elderly pedestrians made more unsafe crossings than the young pedestrians. These findings suggest that the complexity of the street-crossing environment can impact the ability of normally-sighted pedestrians to cross the street safely.
Other factors that may affect street-crossing accuracy may include the vehicular speed of the approaching vehicle,28,29 as well as the ambient sound level and auditory characteristics30 of the crossing environment. Further investigation is warranted to examine how the complexity and characteristics of the street-crossing environment (such as vehicular speed and the auditory environment) affect street-crossing decision-making in low vision pedestrians.
It appears that age and vision loss did not affect the precision of street-crossing decisions, since no significant differences were found in street-crossing precision as a function of subject group and age. Furthermore, the correlations between precision and age and most vision measures also were not significant. Therefore all subjects, even those with central vision loss, were consistent in their decision-making behavior. We did find a significant positive correlation between street-crossing decision-making precision and the average VF extent in the better eye, which suggested that pedestrians became increasingly more precise with increasing VF extent. A possible explanation for this finding may arise from the fact that a greater VF extent enables a pedestrian to see more of the crossing environment and approaching vehicle within a single glance compared to a person with a small VF extent. As a result, a pedestrian with small VF extents may be forced to make repeatable fixations within a short period of time to acquire pertinent street-crossing information from which they can make a crossing decision. Making multiple fixations within a given area over a short period of time presumably is difficult, especially when some of the items of interest, such as an approaching vehicle, are moving. This difficulty may decrease the ability of a pedestrian with small VF extents to obtain repeatedly all of the information required to make a street-crossing decision. As a result, the pedestrian's level of precision in street-crossing decision-making is decreased. More research, however, is required to confirm our explanation of the relationship between precision and VF extent, especially since we did not measure fixation behavior in our subjects. However, the results of Cheong et al.3 provide some support of our explanation, since they found that subjects with severe peripheral VF loss not only made significantly more unsafe street-crossing decisions, but also fixated over a significantly smaller area and made fewer fixations on relevant street-crossing objects compared to age-matched normally-sighted subjects. Thus, the findings of our study and that of Cheong et al.3 suggest that the peripheral VF may have an important role in street-crossing decision-making at un-signalized streets.
An age effect was observed with the accuracy of street-crossing decisions. We found that the bias values of the young normally-sighted subjects not only were significantly different from zero, but also were significantly different from the bias values of the older, normally-sighted and AMD subjects. This suggested that young adults with normal vision are less accurate in making street-crossing decisions compared to older adults, including those with central vision loss. A possible reason why the young normally-sighted subjects were inaccurate compared to either the older, normally-sighted and AMD subjects, may be because they were more risk averse. The amount of inaccuracy observed in the young normally-sighted subjects was positive in value (median bias was 1.14 seconds, see Table 2). The functional implications of a positive bias value is that subjects adopt a less risky street-crossing strategy because they classify gap times that are longer in duration than their street-crossing time as being “enough time to cross.”25 In our study, the young normally-sighted subjects classified only those vehicular gaps that were at least 1.14 seconds longer in duration than their actual crossing time as being “enough time to cross the street.” Consequently, while the young normally-sighted subjects were inaccurate in their street-crossing decisions, they had, indeed, still adopted a safe street-crossing strategy, since they still allowed themselves enough time to cross.
While the bias values of the elderly normally-sighted and AMD subjects were not significantly different from zero, there was a tendency for more of the older normally-sighted and AMD subjects to have negative bias values compared to the young normally-sighted subjects (Fig. 2). The percentages of subjects who had negative bias values within each subject group were 5%, 30%, and 20% for the young normally-sighted, older normally-sighted, and AMD subjects, respectively. Furthermore, the minimum bias values for each subject group were −0.01 seconds for the young normally-sighted subjects, −2.54 seconds for the older normally-sighted subjects, and −4.05 seconds for the AMD subjects (Table 2). Therefore, not only did more elderly subjects have negative bias values compared to the young normally-sighted subjects, but they also had the worst negative bias values.
Negative bias values are interpreted to mean that subjects display less safe street-crossing decision-making behavior because they classify vehicular gap times that are shorter in duration than their actual crossing time as being “enough time to cross.”25 The association between age and negative bias was confirmed in our study by the significant negative correlation found between bias and age (Table 2 and Fig. 3a). In addition, significant correlations were found between bias and VA, CS, and VF extent (Table 2 and Figs. 3b–d). These findings suggest that accuracy in street-crossing decision-making declines with increasing age and worsening binocular VA, CS, and VF extent. Therefore, while we found that the older normally-sighted and AMD subjects as a group made accurate street-crossing decisions, there is a tendency that as pedestrians age and lose vision, they are at risk for making unsafe street-crossing decisions.
Our finding that older normally-sighted and AMD subjects tended to have more negative bias values and, hence, make potentially unsafe street-crossing decisions supports the findings of Oxley et al.,31 and Dommes and Cavallo.28 Both studies found that young normally-sighted subjects performed significantly better than older normally-sighted subjects when making safe street-crossing decisions.
As illustrated in Figure 2, there were two older normally-sighted and two AMD subjects who had negative bias values that were much lower compared to the other subjects in their group. An examination of their age and vision status revealed that these subjects had small VF extents and were among the oldest assessed in our study (Figs. 3a, 3d). However, there were other subjects who had similar binocular VF extents and were similar in age, but whose bias values either were close to zero or positive in value. It is unclear to us as to why this subset of subjects performed so differently compared to the other subjects in their group. Consequently, more research is required to determine which factor(s), including examining the role of hearing alone in street-crossing decision-making, predisposes a pedestrian to have a negative, unsafe bias value. This information is important because it can be used to identify accurately those subjects who are at risk for making unsafe street-crossing decisions, so that they subsequently can be referred for specific orientation and mobility (O&M) training in street-crossing decision-making at un-signalized streets.
In summary, we found that AMD subjects with mild central vision loss were just as accurate and precise as age-matched normally-sighted subjects in making street-crossing decisions. Our results also indicated that age had a significant effect on street-crossing decision-making accuracy, but not on precision. While we found that young normally-sighted subjects were the least accurate in their street-crossing decisions compared to older normally-sighted and AMD subjects with mild central vision loss, they still adopted a safe street-crossing strategy. We also found that the older normally-sighted and AMD subjects with mild central vision loss tended to have more negative bias values that can lead to unsafe street-crossing decisions. More research, however, is required to confirm our findings, especially in patients with severe vision loss from AMD and to evaluate whether street-crossing decision-making performance is influenced by the complexity of the street.
Footnotes
Supported by NIH/NEI Grant R03 EY014874-05 (SEH) and a Beta Sigma Kappa Student Research Award (BDS).
Disclosure: S. E. Hassan, None; B. D. Snyder, None
References
- 1.National Highway Traffic Safety Administration Traffic Safety Facts 2009 Data. Washington, DC: National Highway Traffic Safety Administration's National Center for Statistics and Analysis; 2009 [Google Scholar]
- 2.Ashmead DH, Guth D, Wall RS, Long RG, Ponchillia PE. Street crossing by sighted and blind pedestrians at a modern roundabout. J Transport Eng. 2005;131:812–821 [Google Scholar]
- 3.Cheong AM, Geruschat DR, Congdon N. Traffic gap judgment in people with significant peripheral field loss. Optom Vis Sci. 2008;85:26–36 [DOI] [PubMed] [Google Scholar]
- 4.Guth D, Ashmead D, Long R, Ponchillia P, Wall R. Blind pedestrians' vehicular gap detection at roundabout intersections. Proceedings of the 11th International Mobility Conference. South Africa; Stellenbosch, 2003 [Google Scholar]
- 5.Geruschat DR, Fujiwara K, Wall Emerson RS. Traffic gap detection for pedestrians with low vision. Optom Vis Sci. 2011;88:208–216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guth D, Ashmead D, Long R, Wall R, Ponchillia P. Blind and sighted pedestrians' judgments of gaps in traffic at roundabouts. Hum Factors. 2005;47:314–331 [DOI] [PubMed] [Google Scholar]
- 7.Coleman HR, Chan CC, Ferris FL 3rd, Chew EY. Age-related macular degeneration. Lancet. 2008;372:1835–1845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jager RD, Mieler WF, Miller JW. Age-related macular degeneration. New Engl J Med. 2008;358:2606–2617 [DOI] [PubMed] [Google Scholar]
- 9.Resnikoff S, Pascolini D, Etya'ale D, et al. Global data on visual impairment in the year 2002. Bull World Health Organ. 2004;82:844–851 [PMC free article] [PubMed] [Google Scholar]
- 10.Lovie-Kitchin JE, Bowman KJ. Senile Macular Degeneration – Management and Rehabilitation. Boston, MA: Butterworths; 1985 [Google Scholar]
- 11.Vinding T. Age-related macular degeneration – an epidemiological study of 1000 elderly individuals. Acta Ophthalmol Scand. 1995;217 (Suppl):2–32 [PubMed] [Google Scholar]
- 12.Hampton GR, Nelsen PT. Age-Related Macular Degeneration: Principles and Practice. New York, NY: Raven Press; 1992 [Google Scholar]
- 13.Loshin DS, White J. Contrast sensitivity – the visual rehabilitation of the patient with macular degeneration. Arch Ophthalmol. 1984;102:1303–1306 [DOI] [PubMed] [Google Scholar]
- 14.Swann PG, Lovie-Kitchin JE. Age-related maculopathy. II: the nature of central visual field loss. Ophthalmic Physiol Opt. 1990;11:59–70 [PubMed] [Google Scholar]
- 15.Congdon N, O'Colmain B, Klaver CC, et al. Causes and prevalence of visual impairment among adults in the United States. Arch Ophthalmol. 2004;122:477–485 [DOI] [PubMed] [Google Scholar]
- 16.Klein BE, Klein R. Forecasting age-related macular degeneration through 2050. JAMA. 2009;301:2152–2153 [DOI] [PubMed] [Google Scholar]
- 17.Rein DB, Wittenborn JS, Zhang X, et al. Forecasting age-related macular degeneration through the year 2050: the potential impact of new treatments. Arch Ophthalmol. 2009;127:533–540 [DOI] [PubMed] [Google Scholar]
- 18.He W, Sengupta M, Velkoff VA, DeBarros KA. 65+ in the United States: 2005. Current Population Reports. Washington, DC: U.S. Census Bureau; 2005 [Google Scholar]
- 19.Ferris FL, Kassoff A, Bresnick G, Bailey I. New visual acuity charts for clinical research. Am J Ophthalmol. 1982;94:91–96 [PubMed] [Google Scholar]
- 20.Bailey IL, Lovie JE. New design principles for visual acuity letter charts. Amer J Optom Physiol Opt. 1976;53:740–745 [DOI] [PubMed] [Google Scholar]
- 21.Pelli DG, Robson JG, Wilkins AJ. The design of a new letter chart for measuring contrast sensitivity. Clin Vis Sci. 1988;2:187–199 [Google Scholar]
- 22.Elliott DB, Bullimore MA, Bailey IL. Improving the reliability of the Pelli-Robson contrast sensitivity test. Clin Vis Sci. 1991;6:471–475 [Google Scholar]
- 23.Elliott DB, Whitaker D, Bonette L. Differences in the legibility of letters at contrast threshold using the Pelli-Robson chart. Ophthalmic Physiol Opt. 1990;10:323–326 [DOI] [PubMed] [Google Scholar]
- 24.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading cognitive state of patients for the clinician. J Pyschiatr Res. 1975;12:189–198 [DOI] [PubMed] [Google Scholar]
- 25.Hassan SE, Massof RW. Measurements of street-crossing decision-making in pedestrians with low vision. Accid Prev Anal. In press [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hassan SE. Are normally sighted, visually impaired, and blind pedestrians accurate and reliable at making street crossing decisions? Invest Ophthalmol Vis Sci. 2012;53:2593–2600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Oxley J, Fildes B, Ihsen E, Charlton J, Day R. Differences in traffic judgements between young and old pedestrians. Accid Annal Prev. 1997;29:839–847 [DOI] [PubMed] [Google Scholar]
- 28.Dommes A, Cavallo V. The role of perceptual, cognitive, and motor abilities in street-crossing decisions of young and older pedestrians. Ophthalmic Physiol Opt. 2011;31:292–301 [DOI] [PubMed] [Google Scholar]
- 29.Lobjois R, Cavallo V. Age-related differences in street-crossing decisions: 6he effects of vehicle speed and time constraints on gap selection in an estimation task. Accid Anal Prev. 2007;39:934–943 [DOI] [PubMed] [Google Scholar]
- 30.Emerson RW, Sauerburger D. Detecting approaching vehicles at streets with no traffic control. J Vis Impair Blind. 2008;102:747–760 [PMC free article] [PubMed] [Google Scholar]
- 31.Oxley JA, Ihsen E, Fildes BN, Charlton JL, Day RH. Crossing roads safely: an experimental study of age differences in gap selection by pedestrians. Accid Anal Prev. 2005;37:962–971 [DOI] [PubMed] [Google Scholar]