Abstract
Background
Periprosthetic joint infection has been the leading cause of failure following TKA surgery. The gold standard for infection control has been a two-staged revision TKA. There have been few reports on mid- to long-term survivorship, functional outcomes, and fate of patients with a failed two-stage revision TKA.
Questions/purposes
Therefore, we determined (1) the mid-term survivorship of two-stage revision TKA, (2) the function of patients in whom infection was controlled, and (3) the outcome of patients with a failed two-stage revision due to recurrent infection.
Methods
We retrospectively reviewed 239 patients who underwent 253 two-stage revision TKAs for periprosthetic infection. There were 239 patients (253 knees), 104 men and 135 women, with a mean age of 70 ± 10 years at the time of two-stage revision and a mean BMI of 31.53 ± 6.74 kg/m2. During followup, we obtained WOMAC and The Knee Society Clinical Rating Scores and radiographs. The minimum followup was 1 year (median, 4 years; range, 1–17 years).
Results
Thirty-three patients experienced a failed two-staged TKA. Sixteen patients experienced failure due to recurrent sepsis. There were 17 failures for aseptic causes.
Conclusion
The overall infection-free survivorship for two-stage revision TKA was 85% at 5 years and 78% at 10 years.
Level of Evidence
Level IV, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Infection has occurred in 1% to 2% of primary TKA surgeries and has been the leading cause of failure following TKA [33, 34, 40, 50]. The rate of periprosthetic infection has been declining over the last two to three decades, mostly due to operating room environments and operative techniques [17, 27, 40]. Various methods have been used in the initial treatment of periprosthetic knee infection, including irrigation and debridement [10, 11, 38], direct exchange arthroplasty [6, 16], and two-stage revision TKA with subsequent reimplantation [15, 18]. Incision and drainage has been an attractive option, with low cost and relatively low morbidity; however, the failure rate has been high, ranging between 61% and 82% [4, 5, 7, 23, 30, 35, 38, 39, 41, 44]. There has also been evidence suggesting that patients who failed a previous incision and drainage procedure were more likely to have a higher rate of failure with a subsequent two-stage revision arthroplasty [46]. Single-staged revision TKA for infection has not yet gained the level of support it has had for infected THAs [8, 43], despite two reports showing infection control rates of 90.9% [6] and 89.2% [47]. Insall et al. [29] originally proposed the two-stage revision protocol for infected TKA, which many have considered the gold standard for control of deep periprosthetic infection [3, 49, 51]. This protocol involved the use of antibiotic loaded cement spacers for an interval period, with intravenous antibiotics and the use of antibiotic loaded cement for prosthesis fixation at the time of reimplantation. This two-stage strategy has seen infection-free survival rates of 80% to 100% [2, 3, 9, 10, 12–15, 18–22, 24–26, 29, 36, 39, 42, 45, 47–51]. However, these data require confirmation.
Therefore, we determined (1) the mid-term survivorship of two-stage revision TKA, (2) the function of patients in whom infection was controlled, and (3) the fate of patients who failed a two-stage revision due to recurrent infection.
Patients and Methods
We retrospectively reviewed all 239 patients who underwent 253 two-stage revision TKAs for periprosthetic infection between March 1993 and July 2010. The indications for two-stage surgery were: evidence of chronic infection (ie, symptoms of duration greater than 4 weeks) with an increased c-reactive protein (CRP), a positive culture report from joint aspiration and/or abnormal cell count, and/or intraoperative histology consistent with infection. The contraindications were: patients with documented infection unable to undergo surgery or patients without evidence of infection. For this study, we included any patient who had undergone a two-stage revision TKA procedure for a confirmed infection. Of the 239 patients (253 knees), 104 were men and 135 women, with a mean age of 70 ± 10 years at the time of two-stage revision TKA. The mean BMI was 31.53 ± 6.74 kg/m2. Seventeen (7%) patients required a repeat first-stage procedure due to ongoing infection prior to reimplantation of the definitive prosthesis (Table 1). The minimum followup period was 12 months (median, 48 months; range, 12–276 months). No patients were lost to followup. We did not recall any patients for this study; all data were obtained from medical records and radiographs. Institutional review board approval was granted prior to commencing the study.
Table 1.
Patient demographic data and summary of septic and aseptic failures
| Demographic | Number |
|---|---|
| Number of patients | 239 (253 knees) |
| Man-to-woman ratio | 104:135 |
| Median followup (years) (range) | 4 (1–17) |
| Mean age (years) | 70 ± 10 |
| Mean BMI (kg/m2) | 32 ± 7 |
| Number of repeat one-stage procedures | 17 (7%) |
| Number of patients failing a two-stage revision | 33 (13%) |
| Number of septic failures | 16 (6%) |
| Number of aseptic failures | 17 (7%) |
| Septic failures treated with: | |
| I&D + component retention and polyethylene exchange + suppressive antibiotics | 4 |
| I&D + component retention and polyethylene exchange | 4 |
| Suppressive antibiotics with no surgery | 4 |
| Above knee amputation | 1 |
| Repeat 2SR TKA | 3 |
| Number of repeat two-stage revisions | 11 (in 11 patients) |
| Causes of aseptic failures: | |
| Loosening | 7 |
| Instability | 5 |
| Pain | 2 |
| Extensor mechanism failure | 1 |
| Osteolysis | 1 |
| Nickel allergy | 1 |
I&D = open debridement.
We took preoperative plain radiographs of all knees. All patients underwent preoperative blood tests, including a full blood count, erythrocyte sedimentation rate (ESR), and CRP. We performed knee fluid aspiration in all patients who had raised inflammatory markers 2 weeks after stopping oral antibiotics. Intraoperative frozen sections were obtained in cases where there was a high index of suspicion for infection despite negative preoperative knee aspiration findings.
The protocol for the first-stage procedure involved removing the prosthesis and cement, and sending five to six specimens for microbiology, including intramedullary specimens from both the femoral and tibial canals and swabs from the knee. All specimens were cultured for aerobic and anaerobic organisms. We then inserted either a static or an articulating polymethylmethacrylate (PMMA) spacer. Over the last decade, we estimated over 90% of our patients were treated with an articulating spacer. Only patients with massive defects or compromised knee stability were treated with nonarticulating spacers.
There were a number of different causative organisms at the time of the initial two-stage revision TKA (Table 2). There were a substantial number of patients with either no growth or unavailable bacterial information. This related to the fact that a substantial proportion of our patient cohort were referred to us from other institutions where records were not available and/or were already undergoing antibiotic treatment, thus compromising bacteriological specimens taken at our institution. We recorded the organisms cultured for patients with a failed two-stage revision TKA, along with the original causative organisms (Table 3). Staphylococcus sp. and methicillin-sensitive Staphylococcus aureus (MSSA) were the most common causative organisms in the index two-stage revisions and subsequent failed two-stage revision TKAs.
Table 2.
Organisms cultured preoperatively or at time of original resection
| Organism | Number of knees |
|---|---|
| Staphylococcus | 53 |
| MSSA | 40 |
| MRSA | 8 |
| Streptococcus | 7 |
| Escherichia coli | 3 |
| Enterobacter | 4 |
| Serratia marcenses | 3 |
| Pseudomonas aeruginosa | 2 |
| Propionibacterium | 2 |
| Bacteroides | 1 |
| Clostridium | 1 |
| Multiorganism | 5 |
| No growth | 68 |
| No results available | 56 |
MSSA = methicillin-sensitive Staphylococcus aureus; MRSA = methicillin-resistant Staphylococcus aureus.
Table 3.
Causative organisms for repeat two-stage revision TKA
| Patient | Revision organism | Repeat revision organism |
|---|---|---|
| 1 | MSSA | MSSA |
| 2 | Multiorganism | Multiorganism |
| 3 | Staphylococcus | Staphylococcus |
| 4 | MSSA | MSSA |
| 5 | No growth | No growth |
| 6 | No growth | No growth |
| 7 | Staphylococcus | Staphylococcus |
| 8 | Staphylococcus | Staphylococcus |
| 9 | MSSA | MSSA |
| 10 | MSSA | MSSA |
| 11 | Staphylococcus | Staphylococcus |
MSSA = methicillin-sensitive Staphylococcus aureus.
Patients received intravenous antibiotics for at least 6 weeks, at which point we stopped administering antibiotics. The patients underwent reimplantation when there was no evidence of active infection (usually 4–6 weeks after cessation of antibiotics), determined by a combination of physical examination, serology (CRP < 10 g/l, ESR < 30 mm/hour), joint fluid aspiration (less than 3.0 × 109 cells per liter and no growth), and, when performed, intraoperative histology (less than 5 PMNs per high-powered field).
All patients underwent postoperative followup at 6 weeks, 3 months, 12 months, and yearly thereafter. At each visit, we obtained WOMAC [37] and The Knee Society Clinical Rating Scores [29]. All patients had standing AP, lateral, and skyline radiographs. From the patients’ medical records, we collected the dates of all relevant surgeries, including the index procedure, first and second stage procedures, revision surgeries, and failure surgeries. We also recorded details of the infective organisms. The primary outcome variable was success or failure of a two-stage revision TKA. We recorded failures as any patient that required additional surgery for either septic or aseptic reasons following a two-stage revision. We defined septic failure as pain and/or a loose prosthesis with an increased CRP and a positive culture report from joint aspiration, and/or an abnormal cell count, and/or intraoperative histology consistent with infection. We also recorded the overall outcome for patients who failed a two-stage revision for infection.
We determined the Kaplan-Meier survivorships for aseptic and septic revision endpoints using SPSS® Version 17 (SPSS® Inc., An IBM® Company, Chicago, IL, USA).
Results
The overall infection-free survivorship for two-stage revision TKA was 85% at 5 years and 78% at 10 years (Fig. 1). Thirty-three (13%) patients failed a two-staged TKA: 16 due to recurrent sepsis and 17 due to aseptic causes (Table 1).
Fig. 1.
The graph shows the overall infection-free survivorship for two-stage revision TKA.
The preoperative WOMAC score, and The Knee Society Clinical Rating scores were 48 (± 21) and 64 (± 31), respectively. The postoperative WOMAC and The Knee Society Clinical Rating scores were 60 (± 21) and 129 (± 41), respectively. The difference between the pre- and postoperative WOMAC and The Knee Society Clinical Rating scores were 12 and 65, respectively.
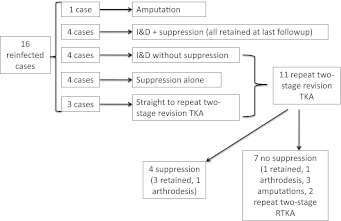
Sixteen patients (16 knees) failed a two-staged revision TKA due to repeat infection (14/16 had positive cultures) at a median of 15 months (range, 5–84 months). Four of these 16 patients were successfully managed with open débridement and polyethylene exchange combined with chronic antibiotic suppression (eg, after 6 weeks of intravenous antibiotics, they were left on oral antibiotics permanently) and remained infection free at minimum of 4 years after surgery. We successfully treated one patient with peripheral vascular disease and a chronically discharging sinus over the knee with an above knee amputation. Eight of these 16 patients went on to repeat two-stage revision TKA following failure of initial management: four underwent open débridement and polyethylene exchange with a short course of postoperative antibiotics (eg, 6 weeks intravenous antibiotics which were then stopped), and four were treated with chronic antibiotic suppression alone. Three of the 16 patients underwent immediate repeat two-stage revision TKA (Fig. 2).
Fig. 2.
The graph summarizes the treatment approach used for reinfected cases. I&D = open débridement.
Of the 11 patients who underwent repeat two-stage revision TKA, four underwent chronic antibiotic suppression postoperatively, while seven did not. At a minimum of 2 years after surgery, three of the four patients who had undergone chronic antibiotic suppression still retained their prosthesis, whilst one patient with rheumatoid arthritis had sustained an extensor mechanism rupture and was subsequently treated with a knee fusion. Only one of the seven (14%) patients not receiving chronic antibiotic suppression still retained their prosthesis at the 2-year followup. The remaining six patients had undergone additional surgery with three above knee amputations, two repeat two-stage revision TKAs, and one knee fusion (Fig. 2).
Discussion
Infection has occurred in approximately 1% to 2% of primary TKA surgeries and has been the leading cause of failure following TKA [33, 34, 40, 50]. Surgeons have used various methods in the initial treatment of periprosthetic knee infection, including irrigation and débridement, direct exchange arthroplasty, and two-stage revision arthroplasty with subsequent reimplantation. There has been limited data published regarding mid- to long-term survivorship and clinical outcomes following two-stage revision TKA, as well as the fate of patients who experienced a failed two-stage revision TKA.
Therefore, we determined (1) the mid-term survivorship of two-stage revision TKA, (2) the function of patients in whom infection was controlled, and (3) the fate of patients who experienced a failed two-stage revision due to recurrent infection.
We recognized the limitations to our study. First, while we collected the data prospectively, the study was a retrospective analysis and had the inherent limitations of a retrospective study design; specifically, the inability to obtain all data that may be helpful, such as the identification of the infecting organism and the total number and nature of surgical interventions the patients had all ready undergone prior to being referred to our center. Second, there were also a number of potential confounding factors, such as the use of static versus articulating antibiotic loaded spacers, the use of varying antibiotic regimes, a number of different surgeons performing the operative procedures, and patient comorbidities. Although this may have been the largest study looking at the outcomes of two-stage revision TKAs, we had inadequate power to stratify by these confounding factors to determine whether any influenced the control of infection. Third, there were 17 aseptic failures in which clinical examination findings, normal serology, negative aspiration results (absence of growth and cell count within normal limits), and frozen section were used to determine the absence of ongoing infection. However, no system or method is perfect, and certainly some aseptic failures could have represented ongoing infection. The patient with presumed metal allergy had a normal workup as above and was, therefore, a diagnosis of exclusion, although this also could have been a missed infection.
Our overall infection-free survivorship for two-stage revision TKA was 85% at 5 years and 78% at 10 years. The literature indicated that eradication of infection following a two-stage revision TKA has been successful in 85% to 95% of cases at short-term followup [15, 20, 24, 26, 29] (Table 4). Our 10-year survivorship results were similar to previously reported studies. Haleem et al. [18] published their 10-year survivorship results of 77% for implant revision for any cause in a series of 96 knees. Goldman et al. [15] reported on 64 knees treated with a two-stage revision protocol, and, despite not using antibiotic loaded cement, also reported a 10-year survivorship of 77%.
Table 4.
Success of two-stage revision TKA
| Study | Year published | Number of successful patients (%) | Mean followup (months) | Resistant organism (%) | Definition of failure |
|---|---|---|---|---|---|
| Insall et al. [28] | 1983 | 10/11 (91) | 34 | NR | Recurrence of infection |
| Wilde and Ruth [49] | 1988 | 9/10 (90) | 33 | NR | Recurrence of infection |
| Booth and Lotke [2] | 1989 | 24/25 (96) | 25 | NR | Recurrence of infection |
| Teeny et al. [48] | 1990 | 10/10 (100) | 42.5 | NR | Recurrence of infection |
| Wilson et al. [50] | 1990 | 16/20 (80) | 34 | NR | Recurrence of infection |
| Masri et al. [36] | 1994 | 22/24 (92) | 26 | NR | Recurrence of infection |
| Goldman et al. [15] | 1996 | 58/64 (91) | 90 | NR | Recurrence of infection |
| Hirakawa et al. [24] | 1998 | 41/55 (75) | 62 | 11 | Recurrence of infection |
| Fehring et al. [13] | 2000 | 51/55 (93) | 36 | NR | Recurrence of infection |
| Durbhakula et al. [12] | 2004 | 22/24 (92) | 33 | 20 | Recurrence of infection |
| Haleem et al. [18] | 2004 | 87/96 (91) | 86 | NR | Recurrence of infection |
| Cuckler [9] | 2005 | 43/44 (98) | NR | 11 | Recurrence of infection |
| Hoffman et al. [26] | 2005 | 44/50 (88) | 30 | 4 | Recurrence of infection |
| Hart and Jones [22] | 2006 | 42/48 (88) | 48.5 | 2 | Recurrence of infection |
| Kurd et al. [32] | 2010 | 70/96 (73) | 34.5 | 50 | Recurrence of infection |
| Mahmud et al. [current study] | 2012 | 220/236 (93) | 48 | 4 | Recurrence of infection |
NR = not recorded.
We demonstrated an improvement in the mean pre- and postoperative WOMAC and The Knee Society Clinical Rating scores, indicating an improvement in function following two-stage revision TKA when performed for infection. Other reports in the literature also supported our findings. Anderson et al. [1] reported an increase in the modified Hospital for Special Surgery scores following two-stage revision TKA. Haleem et al. [18] also reported an improvement in the median The Knee Society Score in their series.
When looking at the fate of patients failing a two-stage revision TKA, we found that chronic antibiotic suppression following repeat two-stage revision TKA was associated with an increased likelihood of prosthesis retention when compared to those patients not receiving chronic antibiotic suppression. Hanssen et al. [21] described the fate of 24 patients (24 knees) treated for reinfection following failed two-stage revision TKA. Their final outcome included 10 knees treated successfully with arthrodesis, five knees treated with suppressive antibiotics (four of these knees failed suppressive therapy), four above-the-knee amputations, three persistent pseudarthroses of the knee, one resection arthroplasty, and one uninfected prosthesis. Our experience of antibiotic suppression alone was poor, and this was reflected in the literature [17, 31, 52]. This method did not treat the infection definitively and only suppressed it, making it a treatment option only for patients who are not good surgical candidates for two-stage revision TKA. The disadvantages of this treatment included the development of resistant bacterial strains, antibiotic toxicity, and painful loosening of the prosthesis.
While the success of a two-stage revision TKA, regarding both controlling infection and improving functional outcomes, supported it as the treatment of choice, this review highlighted the difficulty in treating this complex group of patients. In addition, a careful review of patients who failed a two-stage revision TKA, while not representing large numbers, suggested that chronic antibiotic suppression combined with surgical intervention may be useful in achieving eventual success.
Acknowledgments
The authors thank Dr. Robert B. Bourne for his important contributions to this paper and Lyndsay Somerville for her assistance with extracting data from the database and providing statistical analysis.
Footnotes
The institution of all authors has received funding from DePuy (Warsaw, IN, USA), Smith & Nephew (Memphis, TN, USA), and Stryker (Mahwah, NJ, USA). One or more of the authors consults for Smith & Nephew (DDN, RWM) and DePuy (SJM).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Anderson JA, Sculco PK, Heitkemper S, Mayman DJ, Bostrom MP, Sculco TP. An articulating spacer to treat and mobilize patients with infected total knee arthroplasty. J Arthroplasty. 2009;24:631–635. doi: 10.1016/j.arth.2008.04.003. [DOI] [PubMed] [Google Scholar]
- 2.Booth RE, Lotke PA. The results of spacer block technique in revision of infected total knee arthroplasty. Clin Orthop Relat Res. 1989;248:57–60. [PubMed] [Google Scholar]
- 3.Borden LS, Gearen PF. Infected total knee arthroplasty: a protocol for management. J Arthroplasty. 1987;2:27–36. doi: 10.1016/S0883-5403(87)80028-1. [DOI] [PubMed] [Google Scholar]
- 4.Bradbury T, Fehring TK, Taunton M, Hanssen A, Azzam K, Parvizi J, Odum S. The fate of acute methicillin-resistant Staphylococcus aureus periprosthetic knee infections treated by open debridement and retention of components. J Arthroplasty. 2009;24(Suppl. 6):101–104. doi: 10.1016/j.arth.2009.04.028. [DOI] [PubMed] [Google Scholar]
- 5.Brandt CM, Sistrunk WW, Duffy MC, Hanssen AD, Steckelberg JM, Ilstrup DM, Osmon DR. Staphylococcus aureus prosthetic joint infection treated with debridement and prosthesis retention. Clin Infect Dis. 1997;24:914–919. doi: 10.1093/clinids/24.5.914. [DOI] [PubMed] [Google Scholar]
- 6.Buechel FF, Femino FP, D’Alessio J. Primary exchange revision arthroplasty for infected total knee replacement: a long-term study. Am J Orthop. 2004;33:190–198. [PubMed] [Google Scholar]
- 7.Burger RR, Basch T, Hopson CN. Implant salvage in infected total knee arthroplasty. Clin Orthop Relat Res. 1991;273:105–112. [PubMed] [Google Scholar]
- 8.Callaghan JJ, Katz RP, Johnston RC. One-stage revision surgery of the infected hip. a minimum 10-year follow-up study. Clin Orthop Relat Res. 1999;369:139–143. doi: 10.1097/00003086-199912000-00014. [DOI] [PubMed] [Google Scholar]
- 9.Cuckler JM. The infected total knee. J Arthroplasty. 2005;20(Suppl. 2):33–36. doi: 10.1016/j.arth.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 10.Deirmengian C, Greenbaum J, Lotke PA, Booth RE, Lonner JH. Limited success with open debridement and retention of components in the treatment of acute Staphylococcus aureus infections after total knee arthroplasty. J Arthroplasty. 2003;18(Suppl. 1):22–26. doi: 10.1016/S0883-5403(03)00288-2. [DOI] [PubMed] [Google Scholar]
- 11.Deirmengian C, Greenbaum J, Stern J, Braffman M, Lotke PA, Booth RE, Jr, Lonner JH. Open debridement of acute gram-positive infections after total knee arthroplasty. Clin Orthop Relat Res. 2003;416:129–134. doi: 10.1097/01.blo.0000092996.90435.35. [DOI] [PubMed] [Google Scholar]
- 12.Durbhakula SM, Czajka J, Fuchs MD, Uhl RL. Antibiotic-loaded articulating cement spacer in the 2-stage exchange of infected total knee arthroplasty. J Arthroplasty. 2004;19:768–774. doi: 10.1016/j.arth.2004.02.036. [DOI] [PubMed] [Google Scholar]
- 13.Fehring TK, Odum S, Calton TF, Mason JB. Articulating versus static spacers in revision total knee arthroplasty for sepsis. The Ranawat Award. Clin Orthop Relat Res. 2000;380:9–16. doi: 10.1097/00003086-200011000-00003. [DOI] [PubMed] [Google Scholar]
- 14.Freeman MG, Fehring TK, Odum SM, Fehring K, Griffin WL. Bohannon Mason J. Functional advantage of articulating versus static spacers in 2-stage revision for total knee arthroplasty infection. J Arthroplasty. 2007;22:1116–1121. doi: 10.1016/j.arth.2007.04.009. [DOI] [PubMed] [Google Scholar]
- 15.Goldman RT, Scuderi GR, Insall JN. Two-stage reimplantation for infected total knee replacement. Clin Orthop Relat Res. 1996;331:118–124. doi: 10.1097/00003086-199610000-00016. [DOI] [PubMed] [Google Scholar]
- 16.Goskan SB, Freeman MA. One-stage reimplantation for infected total knee arthroplasty. J Bone Joint Surg Br. 1992;74:78–82. doi: 10.1302/0301-620X.74B1.1732271. [DOI] [PubMed] [Google Scholar]
- 17.Grogan TJ, Dorey F, Rollins J, Amstutz HC. Deep sepsis following total knee arthroplasty: ten-year experience at the University of California at Los Angeles Medical Center. J Bone Joint Surg Am. 1986;68:226–234. [PubMed] [Google Scholar]
- 18.Haleem AA, Berry DJ, Hanssen AD. Mid-term to long-term follow-up of two-stage reimplantation for infected total knee arthroplasty. Clin Orthop Relat Res. 2004;428:35–39. doi: 10.1097/01.blo.0000147713.64235.73. [DOI] [PubMed] [Google Scholar]
- 19.Hanssen AD. Managing the infected knee: as good as it gets. J Arthroplasty. 2002;17(Suppl. 1):98–101. doi: 10.1054/arth.2002.32458. [DOI] [PubMed] [Google Scholar]
- 20.Hanssen AD, Rand JA, Osmon DR. Treatment of the infected total knee arthroplasty with insertion of another prosthesis: the effect of antibiotic-impregnated bone cement. Clin Orthop Relat Res. 1994;309:44–55. [PubMed] [Google Scholar]
- 21.Hanssen AD, Trousdale RT, Osmon DR. Patient outcome with reinfection following reimplantation for the infected total knee arthroplasty. Clin Orthop Relat Res. 1995;321:55–67. [PubMed] [Google Scholar]
- 22.Hart WJ, Jones RS. Two-stage revision of infected total knee replacements using articulating cement spacers and short- term antibiotic therapy. J Bone Joint Surg Br. 2006;88:1011–1015. doi: 10.2106/JBJS.E.01077. [DOI] [PubMed] [Google Scholar]
- 23.Hartman MB, Fehring TK, Jordan L, Norton JH. Periprosthetic knee sepsis: the role of irrigation and debridement. Clin Orthop Relat Res. 1991;273:113–118. [PubMed] [Google Scholar]
- 24.Hirakawa K, Stulberg BN, Wilde AH, Bauer TW, Secic M. Results of 2-stage reimplantation for infected total knee arthroplasty. J Arthroplasty. 1998;13:22–28. doi: 10.1016/S0883-5403(98)90071-7. [DOI] [PubMed] [Google Scholar]
- 25.Hofmann AA, Goldberg T, Tanner AM, Kurtin SM. Treatment of infected total knee arthroplasty using an articulating spacer: 2–12-year experience. Clin Orthop Relat Res. 2005;430:125–131. doi: 10.1097/01.blo.0000149241.77924.01. [DOI] [PubMed] [Google Scholar]
- 26.Hofmann AA, Kane KR, Tkach TK, Plaster RL, Camargo MP. Treatment of infected total knee arthroplasty using an articulating spacer. Clin Orthop Relat Res. 1995;321:45–54. [PubMed] [Google Scholar]
- 27.Huotari K, Lyytikäinen O. The Hospital Infection Surveillance Team: impact of post-discharge surveillance on the rate of surgical site infection after orthopaedic surgery. Infect Control Hosp Epidemiol. 2006;27:1324–1329. doi: 10.1086/509840. [DOI] [PubMed] [Google Scholar]
- 28.Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;248:13–14. [PubMed] [Google Scholar]
- 29.Insall JN, Thompson FM, Brause BD. Two-stage reimplantation for the salvage of infected total knee arthroplasty. J Bone Joint Surg Am. 1983;65:1087–1098. [PubMed] [Google Scholar]
- 30.Ivey FM, Hicks CA, Calhoun JH, Mader JT. Treatment options for infected knee arthroplasties. Rev Inf Dis. 1990;12:468–478. doi: 10.1093/clinids/12.3.468. [DOI] [PubMed] [Google Scholar]
- 31.Johnson DP, Bannister GC. The outcome of infected arthroplasty of the knee. J Bone Joint Surg Br. 1986;68:289–291. doi: 10.1302/0301-620X.68B2.3958017. [DOI] [PubMed] [Google Scholar]
- 32.Kurd M, Ghanem E, Steinbrecher J, Parvizi J. Two-stage exchange knee arthroplasty. Does resistance of the infecting organism influence the outcome? Clin Orthop Relat Res. 2010;468:2060–2066. doi: 10.1007/s11999-010-1296-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kurtz SM, Lau E, Schmier J, Ong K, Zhao K, Parvizi J. Infection burden for hip and knee arthroplasty in the United States. J Arthroplasty. 2008;23:984–991. doi: 10.1016/j.arth.2007.10.017. [DOI] [PubMed] [Google Scholar]
- 34.Kurtz SM, Ong KL, Lau E, Bozic KJ, Berry D, Parvizi J. Prosthetic joint infection risk after TKA in the Medicare population. Clin Orthop Relat Res. 2010;468:52–56. doi: 10.1007/s11999-009-1013-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Marculescu CE, Berbari EF, Hanssen AD, Steckelberg JM, Harmsen SW, Mandrekar JN, Osmon DR. Outcome of prosthetic joint infections treated with debridement and retention of components. Clin Infect Dis. 2006;42:471–478. doi: 10.1086/499234. [DOI] [PubMed] [Google Scholar]
- 36.Masri BA, Kendall RW, Duncan CP, Beauchamp CP, McGraw RW, Bora B. Two-stage exchange arthroplasty using a functional antibiotic-loaded spacer in the treatment of the infected knee replacement: the Vancouver experience. Semin Arthroplasty. 1994;5:122–136. [PubMed] [Google Scholar]
- 37.McConnell S, Kolopack P, Davis M. The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC): a review of its utility and measurement properties. Arthritis Rheum. 2001;45:453–461. doi: 10.1002/1529-0131(200110)45:5<453::AID-ART365>3.0.CO;2-W. [DOI] [PubMed] [Google Scholar]
- 38.Mont MA, Waldman B, Banerjee C, Pacheco IH, Hunderford DS. Multiple irrigation, debridement, and retention of components in infected total knee arthroplasty. J Arthroplasty. 1997;12:426–433. doi: 10.1016/S0883-5403(97)90199-6. [DOI] [PubMed] [Google Scholar]
- 39.Morrey BF, Westholm F, Schoifet S, Rand JA, Bryan RS. Long- term results of various treatment options for infected total knee arthroplasty. Clin Orthop Relat Res. 1989;248:120–128. [PubMed] [Google Scholar]
- 40.Peersman G, Laskin R, Davis J, Peterson M. Infection in total knee replacement: a retrospective review of 6489 total knee replacements. Clin Orthop Relat Res. 2001;392:15–23. doi: 10.1097/00003086-200111000-00003. [DOI] [PubMed] [Google Scholar]
- 41.Rand JA. Alternatives to reimplantation for salvage of the total knee arthroplasty complicated by infection. J Bone Joint Surg Am. 1993;75:282–289. doi: 10.2106/00004623-199302000-00018. [DOI] [PubMed] [Google Scholar]
- 42.Rand JA, Bryan RS, Morrey BF, Westholm F. Management of infected total knee arthroplasty. Clin Orthop Relat Res. 1986;205:75–85. [PubMed] [Google Scholar]
- 43.Rudelli S, Uip D, Honda E, Lima AL. One-stage revision of infected total hip arthroplasty with bone graft. J Arthroplasty. 2008;23:1165–1177. doi: 10.1016/j.arth.2007.08.010. [DOI] [PubMed] [Google Scholar]
- 44.Schoifet SD, Morrey BF. Treatment of infection after total knee arthroplasty by débridement with retention of components. J Bone Joint Surg Am. 1990;72:1383–1390. [PubMed] [Google Scholar]
- 45.Segawa H, Tsukayama DT, Kyle RF, Becker DA, Gustilo RB. Infection after total knee arthroplasty: A retrospective study of the treatment of eighty-one infections. J Bone Joint Surg Am. 1999;81:1434–1445. doi: 10.2106/00004623-199910000-00008. [DOI] [PubMed] [Google Scholar]
- 46.Sherrell JC, Fehring TK, Odum S, Hansen E, Zmistowski B, Dennos A, Kalore N. Fate of two-stage reimplantation after failed irrigation and debridement for periprosthetic knee infection. Clin Orthop Relat Res. 2011;469:18–25. doi: 10.1007/s11999-010-1434-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Silva M, Tharani R, Schmalzried TP. Results of direct exchange or debridement of the infected total knee arthroplasty. Clin Orthop Relat Res. 2002;404:125–131. doi: 10.1097/00003086-200211000-00022. [DOI] [PubMed] [Google Scholar]
- 48.Teeny SM, Dorr L, Murata G, Conaty P. Treatment of infected total knee arthroplasty. J Arthroplasty. 1990;5:35–39. doi: 10.1016/S0883-5403(06)80007-0. [DOI] [PubMed] [Google Scholar]
- 49.Wilde AH, Ruth JT. Two-stage reimplantation in infected total knee arthroplasty. Clin Orthop Relat Res. 1988;236:23–35. [PubMed] [Google Scholar]
- 50.Wilson MG, Kelley K, Thornhill TS. Infection as a complication of total knee-replacement arthroplasty. J Bone Joint Surg Am. 1990;72:878–883. [PubMed] [Google Scholar]
- 51.Windsor RE, Insall JN, Urs WK, Miller DV, Brause BD. Two-stage reimplantation for the salvage of total knee arthroplasty complicated by infection: further followup and refinement of indications. J Bone Joint Surg Am. 1990;72:272–278. [PubMed] [Google Scholar]
- 52.Woods GW, Lionberger DR, Tullos HS. Failed total knee arthroplasty: revision and arthrodesis for infection and non-infectious complications. Clin Orthop Relat Res. 1983;173:184–190. [PubMed] [Google Scholar]