Abstract
Background
Although cross-table lateral radiographs are commonly used to measure acetabular component version after THA, recent studies suggest that CT-based measurement is more accurate. This has been attributed to variations in pelvic tilt, pelvic rotation, and component inclination. Furthermore, it has been suggested, based on limited data, that even with ideal positioning of the cross-table lateral radiograph, CT remains the more accurate modality.
Questions/purposes
We determined whether appropriately positioned cross-table lateral radiographs could provide accurate measurements of acetabular component version, and compared accuracy and reliability of measurements from modified cross-table lateral radiographs with those from standard cross-table lateral radiographs and CT.
Methods
We implanted 27 Sawbones® pelves with an acetabular cup using computer navigation. CT, an AP view of the pelvis, and cross-table lateral and modified cross-table lateral radiographs were performed for each specimen. For the modified cross-table lateral radiograph, the beam angle varied based on the cup inclination as measured on an AP view of the pelvis. Two independent observers measured acetabular component version and inclination. We calculated intraobserver and interobserver reliabilities for each method and compared these with values obtained from navigation presuming that to be the standard for judging accuracy.
Results
Interobserver and intraobserver reliabilities were greater than 0.95 (95% CI, 0.904–0.999) for all measurements. Correlation with navigated values was 0.96 or greater (95% CI, 0.925–0.998) for all methods. Although CT had the highest correlation with navigated values, the correlations for the modified cross-table lateral and cross-table lateral radiographs were similar.
Conclusion
CT allows for accurate measurement of acetabular component version; however, when properly positioned, cross-table lateral radiograph-derived measurements are similarly accurate.
Clinical Relevance
Our results support the use of plain radiographs to obtain important measurements after THA.
Introduction
Acetabular component position is an important determinant of implant stability [12, 15, 20, 26] and bearing surface wear after THA [10, 12, 28, 31]. Malalignment may manifest clinically as reduced impingement-free motion, pain, accelerated wear, instability, or aseptic loosening [24]. Precise measurement of component position is often necessary in the evaluation of patients with postoperative pain or instability. Although inclination can be measured from a standard AP radiograph with little difficulty, measurement of acetabular component version is more difficult, and many orthopaedic surgeons rely on a cross-table lateral radiograph or CT scan to assess acetabular component version in patients after surgery [7, 19, 21, 24, 25].
Numerous definitions for anteversion have been used and therefore some clarification is warranted. Anteversion can be defined in relation to different planes and landmarks, giving rise to the terms true or anatomic anteversion, planar or radiographic anteversion, and operative anteversion. True anteversion is defined as the angle between the projection of the acetabular axis onto the transverse plane and the left-right axis, planar anteversion is the angle between the acetabular axis and the coronal plane, and operative anteversion is the angle between the projection of the acetabular axis onto the sagittal plane and the craniocaudal axis [1, 7, 22, 32]. We will discuss assessment of planar anteversion.
AP and lateral radiographs of the hip often are obtained as part of routine postoperative care after THA. Thus, the ability to accurately measure acetabular component version on standard radiographs is convenient and cost effective. Cross-table lateral radiographs are obtained by flexing the contralateral hip and directing the beam transversely across the operative hip, 45° off the horizontal plane. With the pelvis flat against the table, acetabular component version can be measured as the angle formed by the long axis of the ellipsoid projection of the cup base and a vertical line on the films [7, 32]. Because no calculation is required, measurement of version can be obtained directly with basic imaging software or a goniometer. For these reasons, a cross-table lateral radiograph often is used to assess acetabular component version [4, 7, 23, 27]. However, two recent publications questioned the accuracy of this method [7, 24].
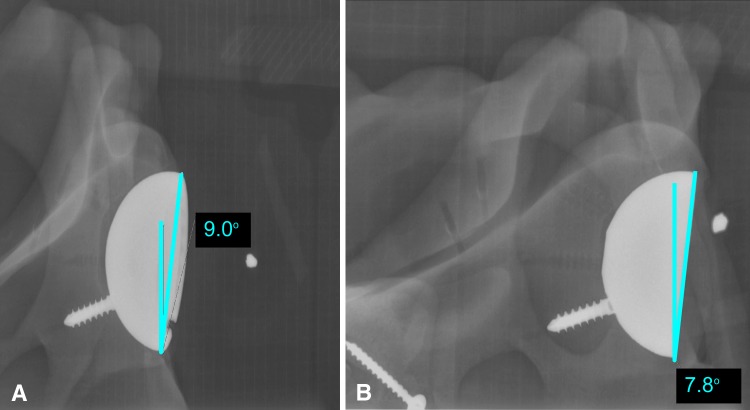
Inaccuracy in version measurements obtained from a cross-table lateral radiograph is attributed to variations in cup inclination angle and alterations in pelvic tilt and rotation [7, 32]. A tilted pelvis changes the radiographic projection and distorts the measurement as the vertical line on the film will not accurately represent the axial plane. Further, a standard cross-table lateral radiograph most closely approximates planar version when cup inclination is 45° [3]; however, clinical studies showed that cup inclination varies dramatically from this number [3, 7]. Based on this, we developed the modified cross-table lateral radiograph, wherein the beam angle for the cross-table lateral view is adjusted based on component inclination. Using this method, the mouth of the cup appears not as a wide ellipse, but rather as a straight line [32] (Fig. 1).
Fig. 1A–B.
(A) The image shows how the standard cross-table lateral radiograph was modified. (B) With adjustment of the beam angle to match component inclination, the mouth of the cup was projected as a straight line as opposed to an ellipse.
Some authors have advocated CT as the gold-standard imaging modality for measuring acetabular component version to mitigate the errors seen with cross-table lateral radiographs caused by poorly standardized patient positioning and variable beam-angle orientation [7, 24]; however, increased cost and ionizing radiation exposure are major drawbacks to CT imaging. The ideal imaging technique for measuring acetabular component version would have the accuracy of CT, but the ease and reduced cost and radiation exposure inherent to plain radiographs. We hypothesized that if pelvic positioning and beam angle orientation were properly standardized, a cross-table lateral radiograph would provide comparable accuracy to CT for measuring acetabular component position.
The purposes of this study were twofold: we wished to (1) determine whether acetabular component version could be measured accurately with a properly positioned cross-table lateral radiograph, and (2) establish the relative accuracy and reliability of CT, cross-table lateral and modified cross-table lateral radiographs for measuring acetabular component version.
Materials and Methods
We implanted 27 Sawbones® pelves (Pacific Research Laboratories, Vashon, WA, USA) with a noncemented R3® (Smith & Nephew, Memphis, TN, USA) acetabular cup and one screw using imageless navigation (Smith & Nephew). Each Sawbones® pelvis was secured to a vice grip on an operating table during implantation, and each pelvis was implanted with one cup. Twenty-seven distinct cup positions were randomly generated, using a customizable, online random number-generating program, within a range of 30° anteversion, 15° retroversion, and 20° to 60° cup inclination (Table 1). After cup implantation, we securely fixed specimens in radiolucent cardboard boxes so three landmarks, the sacrum and bilateral posterior-superior iliac spines, were securely tied to the floor of the box to minimize pelvic tilt. We then covered the boxes with a lid to blind the radiology technician to the actual cup position. Approval for this controlled laboratory study was obtained from the Radiology Department research review panel.
Table 1.
Navigated component positions for 27 specimens
| Specimen number | Inclination angle (degrees) | Anteversion angle (degrees) |
|---|---|---|
| 1 | 40 | −8 |
| 2 | 25 | −4 |
| 3 | 32 | 10 |
| 4 | 16 | −6 |
| 5 | 53 | 0 |
| 6 | 42 | 6 |
| 7 | 33 | 24 |
| 8 | 41 | −9 |
| 9 | 33 | 7 |
| 10 | 32 | 12 |
| 11 | 46 | −4 |
| 12 | 26 | 19 |
| 13 | 45 | 30 |
| 14 | 56 | −6 |
| 15 | 15 | 23 |
| 16 | 33 | 18 |
| 17 | 58 | −11 |
| 18 | 33 | 8 |
| 19 | 27 | 0 |
| 20 | 58 | −8 |
| 21 | 53 | 4 |
| 22 | 55 | −9 |
| 23 | 43 | 10 |
| 24 | 31 | −13 |
| 25 | 41 | 9 |
| 26 | 27 | −2 |
| 27 | 35 | 6 |
Previous analysis of a similar study by Ghelman et al. [7], studying the performance of radiography versus CT for determination of acetabular component version, found intraclass correlation (ICC) of 0.698. Using a more conservative estimate of a null hypothesis ICC of 0.750, we determined that a sample size of 27 subjects with two observations per subject achieved 81% power to detect an ICC of 0.900 with a significance level set at p ≤ 0.05.
The cephalic margin of the pelvis was indicated on the box, but the radiology technician otherwise was blinded to the orientation of the pelvis. An AP view of the pelvis, cross-table lateral, and modified cross-table lateral radiographs then were acquired of each specimen. The modified cross-table lateral image was taken as the final image with the x-ray tube directed toward the pelvis at the angle the technician previously measured acetabular component inclination on the AP view of the pelvis, thus resulting in the x-ray beam being parallel to the base of the cup. For example, if the component appeared implanted at 40° abduction on the AP view of the pelvis, the beam angle was adjusted from 45° used to image the cross-table lateral view, to 40° for the modified cross-table lateral view.
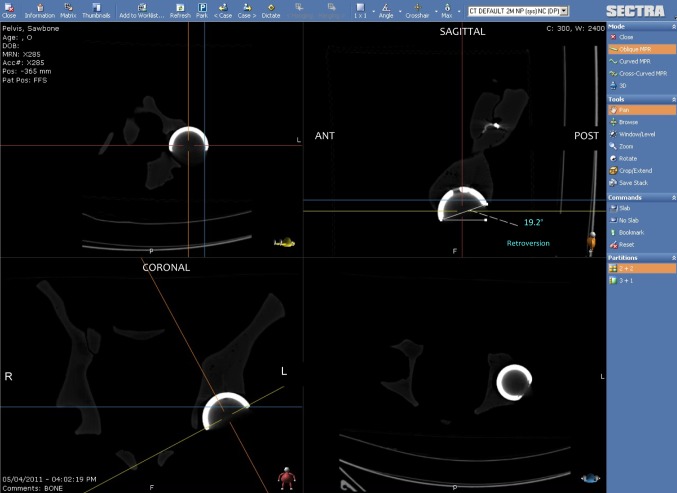
We performed CT of each specimen on a Philips Brilliance 16-slice CT scanner (Philips, Andover, MA, USA), acquiring 1-mm contiguous axial images. We then manipulated the images using a multiplanar reformatting function in our picture archiving communication system (PACS) into coronal and sagittal orthogonal images to accurately measure acetabular component version (Fig. 2).
Fig. 2.
The image shows how the multiplanar reconstruction function in our picture archiving communication system (PACS) was used to directly measure version. The standard technique of measuring on the axial CT image was modified to account for acetabular inclination when measuring version.
To ensure appropriate blinding and prevent bias, we assigned each radiograph or CT a randomized serial number, allowing the images to be dissociated from the specimen numbers so one measurement would not influence the next. Two independent, blinded observers (BG, CG) measured component version on the cross-table lateral and modified cross-table lateral radiographs and CT, and component inclination on the AP radiograph of the pelvis (Fig. 3). Each observer performed measurements on two separate occasions at least 1 week apart.
Fig. 3.
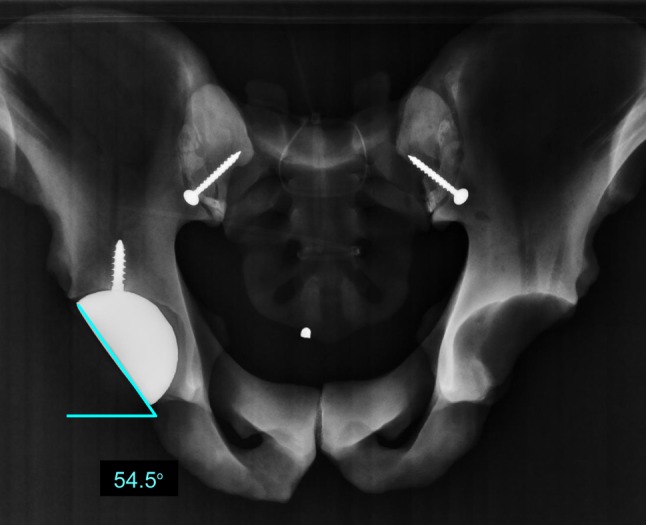
The image shows how the inclination angle was measured relative to the horizontal axis on an AP radiograph of the pelvis.
We evaluated specimen characteristics using means and standard deviations for continuous variables and frequencies and percentages for discrete variables. Two-way mixed model ICCs on absolute agreement were used to determine interobserver and intraobserver reliabilities [29]. Finally, we compared the readings of the two observers with the navigated values to evaluate the consistency of the readings. To assess the precision of our estimates, we calculated 95% CIs for each correlation. All p values reported were results from two-sided tests. Statistical analyses were conducted using SPSS® software, version 15.0 (IBM Inc, Chicago, IL, USA).
Results
As expected, measurement of inclination on AP views of the pelvis was reliable and accurate with all interobserver and intraobserver reliability coefficients of 0.988 or greater (Table 2). Comparison of inclination measurements to navigated values showed a high level of consistency, with correlation coefficients of 0.988 or greater (Table 3).
Table 2.
Intraobserver and interobserver agreement in radiographic measurements
| Measurement | Inclination (AP view of pelvis) | 95% CI | Acetabular component version (cross-table lateral) | 95% CI | Acetabular component version (modified cross-table lateral) | 95% CI | Acetabular component version (CT) | 95% CI |
|---|---|---|---|---|---|---|---|---|
| Interobserver | 0.995 | 0.992–0.998 | 0.995 | 0.992–0.998 | 0.996 | 0.993–0.998 | 0.985 | 0.974–0.993 |
| Intraobserver 1 | 0.988 | 0.973–0.994 | 0.997 | 0.992–0.998 | 0.999 | 0.999–0.999 | 0.988 | 0.974–0.989 |
| Intraobserver 2 | 0.998 | 0.995–0.999 | 0.987 | 0.971–0.994 | 0.985 | 0.968–0.993 | 0.956 | 0.904–0.980 |
Table 3.
Radiologists’ measurements versus navigated values
| Reader | Inclination AP view of the pelvis | 95% CI | Acetabular component version (cross-table lateral radiograph) | 95% CI | Acetabular component version (modified cross-table lateral radiograph) | 95% CI | Acetabular component version (CT) | 95% CI |
|---|---|---|---|---|---|---|---|---|
| Radiologist 1 | 0.988 | 0.976–0.994 | 0.966 | 0.936–0.984 | 0.971 | 0.945–0.986 | 0.980 | 0.962–0.990 |
| Radiologist 2 | 0.995 | 0.991–0.998 | 0.96 | 0.925–0.981 | 0.963 | 0.93–0.982 | 0.968 | 0.939–0.984 |
Accuracy of acetabular component version measurements in properly positioned cross-table lateral radiographs also was high. Correlation coefficients when compared with navigated values were 0.966 and 0.960 for the two observers (Table 3). Mean absolute differences between navigated and cross-table lateral radiographs measured values were 4.34° and 4.68° for the two observers (SD, 5.05 and 5.27) (Table 4).
Table 4.
Mean error comparison*
| Comparison groups | p value |
|---|---|
| Observer 1 | |
| CT versus cross-table lateral radiograph | 0.302 |
| CT versus modified cross-table lateral radiograph | 0.241 |
| Cross-table lateral radiograph versus modified cross-table lateral radiograph | 0.935 |
| Observer 2 | |
| CT versus cross-table lateral radiograph | 0.470 |
| CT versus modified cross-table lateral radiograph | 0.334 |
| Cross-table lateral radiograph versus modified cross-table lateral radiograph | 0.775 |
* Results of paired t-tests.
Measurement by all methods correlated closely with navigated values.
Relative accuracy was greatest for CT-based measurements (ICC, 0.980 and 0.968), followed by modified cross-table lateral (ICC, 0.971 and 0.963) and then cross-table lateral-based measurements (Table 3), but these differences were small and differences in mean measurement error between methods were insignificant (Table 4).
Interobserver reliabilities were slightly higher for modified cross-table lateral and cross-table lateral-based measurements (0.996 and 0.995 respectively) than for CT-based measurements (0.985) (Table 2). Intraobserver reliabilities also were slightly higher with modified cross-table lateral and cross-table lateral-based measurements than with CT (Table 2). Similarly, differences were noted in mean interobserver error between CT and modified cross-table lateral-based measurements (2.2 +/− 2.5 versus 1.2 +/− 1.5; p = 0.052). The difference was less pronounced between CT and cross-table lateral measurements (1.3 +/− 1.7; p = 0.089) (Tables 5 and 6).
Table 5.
Mean difference (degrees) between measurements
| Angle | Interobserver | SD | Intraobserver 1 | SD | Intraobserver 2 | SD | Mean error 1 | SD | Mean error 2 | SD |
|---|---|---|---|---|---|---|---|---|---|---|
| Inclination | 1.90 | 0.90 | 2.4 | 1.53 | 0.83 | 0.80 | 3.09 | 1.59 | 1.94 | 1.54 |
| Acetabular component version on CT | 2.23 | 2.46 | 0.74 | 0.79 | 2.81 | 4.79 | 3.46 | 2.93 | 4.15 | 3.11 |
| Acetabular component version on cross-table lateral radiographs | 1.28 | 1.70 | 1.32 | 0.84 | 1.27 | 2.83 | 4.34 | 5.05 | 4.68 | 5.27 |
| Acetabular component version on modified cross-table lateral radiographs | 1.23 | 1.45 | 0.59 | 0.43 | 1.6 | 3.05 | 4.41 | 4.46 | 4.94 | 4.68 |
Table 6.
Mean interobserver difference comparison*
| Comparison groups | p value |
|---|---|
| CT versus cross-table lateral radiograph | 0.089 |
| CT versus modified cross-table lateral radiograph | 0.052 |
| Cross-table lateral radiograph versus modified cross-table lateral radiograph | 0.794 |
* Results of paired t-tests.
Discussion
Accurate assessment of acetabular component version is critical when evaluating patients with pain or instability after THA. Although numerous methods have been described [7, 13, 19, 21, 32], recent studies have suggested that CT should be the gold standard owing to its accuracy and precision [7, 24]. The cross-table lateral radiograph is a commonly used modality [7, 18]. In an era of increasing awareness of healthcare spending and the ill effects of radiation exposure, the benefits of plain radiographs over CT are obvious. The purposes of this study were twofold. We wished to (1) determine whether acetabular component version could be measured accurately with a properly positioned cross-table lateral radiograph and (2) establish the relative accuracy and reliability of CT, and cross-table lateral and modified cross-table lateral radiographs for measuring acetabular component version.
This study has numerous limitations. First, this study was an in vitro study, which clearly deviated from imaging obtained in clinical practice. Specifically, we largely eliminated the patient positioning variables (pelvic tilt and rotation) which produce error in clinical practice and used model pelves with set dimensions as opposed to the anatomic variation seen in the general population. Although a limitation, it was a calculated decision. If our findings showed considerable inaccuracy in cross-table lateral-based measurements, even in our controlled scenario, then further attempts to modify clinical protocols for cross-table lateral radiographs would be futile because the optimal accuracy of these measurements would be unacceptable regardless of protocol. Our decision to perform this study using Sawbones® specimens allowed for a high degree of control in pelvic tilt and rotation, which provided a sense of the maximum accuracy that could be achieved with appropriate modification of clinical imaging protocols. Second, we had two assumptions in our protocol for the modified cross-table lateral radiograph. The principle of adjusting the beam angle to match component inclination angle was sound and supported by previous studies [6, 32]. Using fluoroscopy to bring the beam angle in line with the component inclination angle [6, 13] was based on a study by Yao et al. [32], who found that version on the axiolateral cross-table lateral radiograph is equal to planar anteversion when the beam angulation matches inclination. Our protocol sought to reproduce this concept by measuring inclination on the AP radiograph and using this to adjust the beam angle. This approach first assumes accurate measurement of component inclination on the AP view of the pelvis by the technician adjusting the beam angle. Although our data showed the accuracy and reliability of this measurement when performed by two trained radiologists, we did not specifically evaluate the performance of the radiology technician in this regard. Although the technician had experience in musculoskeletal imaging and was trained by our radiologist in these measurements, it is possible that his measurements were less accurate. The approach also assumes the beam angle could be positioned accurately at the desired angle. This may have been more difficult in practice than in concept. Although this may have been a shortcoming of the modified cross-table lateral radiograph, we presumed the attempt to approximate inclination angle with the angle of the beam could be a relatively simple modification to the standard protocol that might have direct application in clinical practice; therefore, assessment of accuracy of the modified cross-table lateral radiograph-based measurement seemed worthwhile. Third, no gold standard exists to validate radiographic or CT-based acetabular component version measurements in vitro or in vivo [7]. Therefore, we used computer navigation as an independent measure of acetabular component version and compared radiographic measurements with the navigated values. An intrinsic error in computer navigation-based measurements, which we used as a third measure of anteversion to compare with our radiographic measurements, has been reported [2, 30]. To diminish error, navigated cup placement was performed by one operator (BAM) under ideal in vitro conditions. Several conditions in our experiment mitigate factors described as compromising navigated results in vivo. Specifically, we assume landmark identification and registration errors would be diminished in our study compared with in vivo scenarios where the overlying soft tissue can interfere with these processes [2]. Furthermore, the standardization of dimensions in manufactured pelves alleviates concerns regarding compensation for differences in pelvic tilt as described by Dorr et al. [5] and Lembeck et al. [14]. We believe these values have relevance to our study as navigated values reference from extraarticular anatomic landmarks of the bony pelvis (namely, the pubic tubercles and anterior-superior iliac spines) to set a reference plane for the pelvis, similar to the manner in which CT measurements are taken, and thus should be independent of the position of the pelvis.
We observed a high degree of accuracy in cross-table lateral radiograph-based acetabular component version measurement when positioning variables are appropriately controlled. Although no gold standard exists for measurement of anteversion [6], two studies evaluating the reliability of cross-table lateral radiograph-based acetabular component version measurement have used CT as the standard for comparison [7, 24]. Nunley et al. [24] compared serial cross-table lateral radiograph measurements with CT-based measurements and found a strong correlation of 0.82. In a similar comparison, Ghelman et al. [7] reported a correlation of 0.69. Both studies used clinical images, and therefore pelvic tilt and rotation were not fixed. As we expected correlations in our in vitro scenario were significantly higher than those reported in these clinical studies (Table 7), showing the importance of appropriate positioning in clinical practice. In addition, Ghelman et al. [7] created an in vitro scenario, similar to ours, using imageless navigation in Sawbones® pelves to implant acetabular components in various degrees of anteversion and inclination and compared navigated values with CT and cross-table lateral radiograph-based measurements as an in vitro test of accuracy. The ICC reported for CT was 0.862 as opposed to 0.779 and 0.786 for cross-table lateral radiographs measured by two observers. However, sample size was small, using only four specimens and cup positions. We observed considerably higher correlations in our appropriately powered study, which we believe to be a more correct estimate of the accuracy of cross-table lateral radiographs which can be obtained when pelvic positioning is optimized.
Table 7.
Reported accuracy of CT and cross-table lateral-based measurement
| Study | Measurement modality compared | Number | Correlation coefficient | Mean error |
|---|---|---|---|---|
| Nunley et al. [24] | Cross-table lateral radiograph versus CT* | 119 | 0.82 | |
| Ghelman et al. [7] | Cross-table lateral radiograph versus CT* | 42 | 0.69 | 8.7° |
| CT versus navigation | 4 | 0.862 | 6.75° | |
| Cross-table lateral radiograph versus navigation | 4 | 0.779 and 0.786 | 9.3° and 8.2° | |
| Current study | CT versus navigation | 27 | 0.980 and 0.968 | 3.46° and 4.15° |
| Cross-table lateral radiograph versus navigation | 27 | 0.966 and 0.960 | 4.34° and 4.68° |
* Comparison of angles derived from clinical images as opposed to images of model specimens.
Furthermore, we compared the relative accuracy and reliability of acetabular component version measurements obtained from cross-table lateral and modified cross-table lateral radiographs and CT. Although correlation with navigated values was greatest for CT, followed by modified cross-table lateral and cross-table lateral radiographs, these differences were small and differences in measurement error were not statistically significant between groups. The observed differences may have been related to small variations in pelvic positioning which were difficult to eliminate, even in our highly controlled scenario. Thus we showed that cross-table lateral radiograph-based measurements closely approximate the accuracy of CT when pelvic positioning is controlled. In addition, the accuracy of the modified cross-table lateral radiograph matched that of CT and the cross-table lateral radiograph. Our modification of the standard cross-table lateral radiograph, which was conceived in an effort to control for variations in component inclination, did correlate more closely to CT and navigation-based measurements; however, in our controlled setting, measurement by all three methods was highly accurate and differences did not reach statistical significance. Our post hoc subgroup analysis showed decreased error at the extremes of inclination with the modified cross-table lateral radiograph compared with the cross-table lateral radiograph, however our study was not powered for this comparison and differences were not statistically significant. Comparison of our measurement accuracy to numbers reported in clinical studies [7, 24] showed an improvement in baseline accuracy of the cross-table lateral radiograph in our controlled scenario. This suggests that, although control for component inclination may improve accuracy of measurements, other variables such as pelvic tilt or obliquity may have played a larger role in determining the accuracy of the cross-table lateral radiograph in clinical practice. Measurement reliability for the modified cross-table lateral radiograph, in terms of intraobserver and interobserver measurement error, was actually greater than CT in our controlled scenario. This may have resulted from the simplicity of the measurement on a single image compared with the multiple cuts available for measurement on CT scans. Although these findings were statistically significant, the difference was small and therefore the clinical significance is questionable. Some studies have assessed the reliability of measurements from either AP or cross-table lateral radiographs and our findings are consistent with the literature (Table 8) [7–9, 11, 16, 17].
Table 8.
Reported interobserver reliability for radiographic version measurements
| Study | Measurement modality compared | Interobserver reliability intraclass correlation coefficient | Mean error +/− SD for interobserver reliability |
|---|---|---|---|
| Hassan et al. [8] | Acetabular component version from AP radiograph of ex vivo cup | 0.97–0.99 | |
| Kalteis et al. [11] | Acetabular component version from AP radiograph of pelvis | 2.3° +/− 2.3° | |
| Liaw et al. [16] | Acetabular component version from AP radiograph of pelvis | 1.0° +/− 0.7° | |
| Liaw et al. [17] | Acetabular component version from AP radiograph of pelvis | 0.5° +/− 0.7° | |
| Hayakawa et al. [[9] | Acetabular component version from AP radiograph of pelvis | 1.4° +/− 3.1° | |
| Ghelman et al. [7] | Acetabular component version from cross-table lateral radiograph | 0.96 | 2.4° +/− 2.4° |
| Current study | Acetabular component version from cross-table lateral radiograph | 0.99 | 1.28° +/− 1.7° |
The greatest challenge in any in vitro study is in the translation of findings into the clinical setting, and our study was no different. We showed that although CT is the most accurate modality for measurement of acetabular component version, properly positioned plain radiographs also are accurate. In light of the obvious cost and health benefits for the patient, the pursuit of imaging protocols that minimize positioning variables which may result in measurement error is worthwhile and appropriate. Future research directed at clinical modification of imaging protocols to improve measurement accuracy on plain radiographs is warranted. Modification of the cross-table lateral radiograph by adjustment of beam angle to match component inclination angle may be one step toward improvement of accuracy and reliability in a clinical setting. Additional adjustments should be aimed at limitation of pelvic tilt and rotation. As we work to balance the benefits of advanced imaging with the crisis in health-care spending and the ill effects of radiation exposure, our results support the modification of imaging protocols to improve the accuracy and reliability of version measurements attainable with plain cross-table lateral radiographs.
Acknowledgments
We thank Kristine Leggett, Clinical Research Coordinator for the Department of Radiology, for assisting in the coordination of this study between two departments. We also thank Joseph Nguyen MPH, of the biostatistics department, who was instrumental in data analysis.
Footnotes
David Mayman receives support in the form of paid consultancy from Smith & Nephew (Memphis, TN, USA) and BrainLAB Inc, (Westchester, IL, USA). He has stock in OrthAlign Inc. The remaining authors have no financial disclosures. Institutional support for this study was received in the form of donated components and instrumentation from Smith & Nephew and Brain lab.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved or waived approval for the reporting of this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Ackland MK, Bourne WB, Uhthoff HK. Anteversion of the acetabular cup: measurement of angle after total hip replacement. J Bone Joint Surg Br. 1986;68:409–413. doi: 10.1302/0301-620X.68B3.3733807. [DOI] [PubMed] [Google Scholar]
- 2.Blendea S, Troccaz J, Ravey JN, Merloz P. Image-free cup navigation inaccuracy: a two-study approach. Comput Aided Surg. 2007;12:176–180. doi: 10.3109/10929080701374265. [DOI] [PubMed] [Google Scholar]
- 3.Callanan MC, Jarrett B, Bragdon CR, Zurakowski D, Rubash HE, Freiberg AA, Malchau H. The John Charnley Award: Risk factors for cup malpositioning: quality improvement through a joint registry at a tertiary hospital. Clin Orthop Relat Res. 2011;469:319–329. doi: 10.1007/s11999-010-1487-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Calvert GT, Devane PA, Fielden J, Adams K, Horne JG. A double-blind, prospective, randomized controlled trial comparing highly cross-linked and conventional polyethylene in primary total hip arthroplasty. J Arthroplasty. 2009;24:505–510. doi: 10.1016/j.arth.2008.02.011. [DOI] [PubMed] [Google Scholar]
- 5.Dorr LD, Malik A, Wan Z, Long WT, Harris M. Precision and bias of imageless computer navigation and surgeon estimates for acetabular component position. Clin Orthop Relat Res. 2007;465:92–99. doi: 10.1097/BLO.0b013e3181560c51. [DOI] [PubMed] [Google Scholar]
- 6.Ghelman B. Radiographic localization of the acetabular component of a hip prosthesis. Radiology. 1979;130:540–542. doi: 10.1148/130.2.540. [DOI] [PubMed] [Google Scholar]
- 7.Ghelman B, Kepler CK, Lyman S, Della Valle AG. CT outperforms radiography for determination of acetabular cup version after THA. Clin Orthop Relat Res. 2009;467:2362–2370. doi: 10.1007/s11999-009-0774-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hassan DM, Johnston GH, Dust WN, Watson LG, Cassidy D. Radiographic calculation of anteversion in acetabular prostheses. J Arthroplasty. 1995;10:369–372. doi: 10.1016/S0883-5403(05)80187-1. [DOI] [PubMed] [Google Scholar]
- 9.Hayakawa K, Minoda Y, Aihara M, Sakawa A, Ohzono K, Tada K. Acetabular component orientation in intra- and postoperative positions in total hip arthroplasty. Arch Orthop Trauma Surg. 2009;129:1151–1156. doi: 10.1007/s00402-008-0638-2. [DOI] [PubMed] [Google Scholar]
- 10.Hirakawa K, Mitsugi N, Koshino T, Saito T, Hirasawa Y, Kubo T. Effect of acetabular cup position and orientation in cemented total hip arthroplasty. Clin Orthop Relat Res. 2001;388:135–142. doi: 10.1097/00003086-200107000-00020. [DOI] [PubMed] [Google Scholar]
- 11.Kalteis T, Handel M, Herold T, Perlick L, Paetzel C, Grifka J. Position of the acetabular cup: accuracy of radiographic calculation compared to CT-based measurement. Eur J Radiol. 2006;58:294–300. doi: 10.1016/j.ejrad.2005.10.003. [DOI] [PubMed] [Google Scholar]
- 12.Kennedy JG, Rogers WB, Soffe KE, Sullivan RJ, Griffen DG, Sheehan LJ. Effect of acetabular component orientation on recurrent dislocation, pelvic osteolysis, polyethylene wear, and component migration. J Arthroplasty. 1998;13:530–534. doi: 10.1016/S0883-5403(98)90052-3. [DOI] [PubMed] [Google Scholar]
- 13.Langton DJ, Sprowson AP, Mahadeva D, Bhatnagar S, Holland JP, Nargol AVF. Cup anteversion in hip resurfacing: validation of EBRA and the presentation of a simple clinical grading system. J Arthroplasty. 2010;25:607–613. doi: 10.1016/j.arth.2009.08.020. [DOI] [PubMed] [Google Scholar]
- 14.Lembeck B, Mueller O, Reize P, Wuelker N. Pelvic tilt makes acetabular cup navigation inaccurate. Acta Orthop. 2005;76:517–523. doi: 10.1080/17453670510041501. [DOI] [PubMed] [Google Scholar]
- 15.Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60:217–220. [PubMed] [Google Scholar]
- 16.Liaw CK, Hou SM, Yang RS, Wu TY, Fuh CS. A new tool for measuring cup orientation in total hip arthroplasties from plain radiographs. Clin Orthop Relat Res. 2006;451:134–139. doi: 10.1097/01.blo.0000223988.41776.fa. [DOI] [PubMed] [Google Scholar]
- 17.Liaw CK, Yang RS, Hou SM, Wu TY, Fuh CS. Measurement of the acetabular cup anteversion on simulated radiographs. J Arthroplasty. 2009;24:468–474. doi: 10.1016/j.arth.2007.10.029. [DOI] [PubMed] [Google Scholar]
- 18.Malik A, Wan Z, Jaramaz B, Bowman G, Dorr LD. A validation model for measurement of acetabular component position. J Arthroplasty. 2010;25:812–819. doi: 10.1016/j.arth.2009.04.021. [DOI] [PubMed] [Google Scholar]
- 19.Markel DC, Andary JL, Pagano P, Nasser S. Assessment of acetabular version by plain radiograph. Am J Orthop (Belle Mead NJ). 2007;36:39–41. [PubMed] [Google Scholar]
- 20.McCollum DE, Gray WJ. Dislocation after total hip arthroplasty: causes and prevention. Clin Orthop Relat Res. 1990;261:159–170. [PubMed] [Google Scholar]
- 21.Mian SW, Truchly G, Pflum FA. Computed tomography measurement of acetabular cup anteversion and retroversion in total hip arthroplasty. Clin Orthop Relat Res. 1992;276:206–209. [PubMed] [Google Scholar]
- 22.Murray DW. The definition and measurement of acetabular orientation. J Bone Joint Surg Br. 1993;75:228–232. doi: 10.1302/0301-620X.75B2.8444942. [DOI] [PubMed] [Google Scholar]
- 23.Najarian BC, Kilgore JE, Markel DC. Evaluation of component positioning in primary total hip arthroplasty using an imageless navigation device compared with traditional methods. J Arthroplasty. 2009;24:15–21. doi: 10.1016/j.arth.2008.01.004. [DOI] [PubMed] [Google Scholar]
- 24.Nunley RM, Keeney JA, Zhu J, Clohisy JC, Barrack RL. The reliability and variation of acetabular component anteversion measurements from cross-table lateral radiographs. J Arthroplasty. 2011;26:84–87. doi: 10.1016/j.arth.2011.03.039. [DOI] [PubMed] [Google Scholar]
- 25.Padgett DE, Hendrix SL, Mologne TS, Peterson DA, Holley KA. Effectiveness of an acetabular positioning device in primary total hip arthroplasty. HSS J. 2005;1:64–67. doi: 10.1007/s11420-005-0109-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ritter MA. Dislocation and subluxation of the total hip replacement. Clin Orthop Relat Res. 1976;121:92–94. [PubMed] [Google Scholar]
- 27.Sah AP, Estok DM., 2nd Dislocation rate after conversion from hip hemiarthroplasty to total hip arthroplasty. J Bone Joint Surg Am. 2008;90:506–516. doi: 10.2106/JBJS.G.00479. [DOI] [PubMed] [Google Scholar]
- 28.Schmalzried TP, Guttmann D, Grecula M, Amstutz HC. The relationship between the design, position, and articular wear of acetabular components inserted without cement and the development of pelvic osteolysis. J Bone Joint Surg Am. 1994;76:677–688. doi: 10.2106/00004623-199405000-00008. [DOI] [PubMed] [Google Scholar]
- 29.Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86:420–428. doi: 10.1037/0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- 30.Spencer JM, Day RE, Sloan KE, Beaver RJ. Computer navigation of the acetabular component: a cadaver reliability study. J Bone Joint Surg Br. 2006;88:972–975. doi: 10.1302/0301-620X.88B7.17468. [DOI] [PubMed] [Google Scholar]
- 31.Wan Z, Boutary M, Dorr LD. The influence of acetabular component position on wear in total hip arthroplasty. J Arthroplasty. 2008;23:51–56. doi: 10.1016/j.arth.2007.06.008. [DOI] [PubMed] [Google Scholar]
- 32.Yao L, Yao J, Gold RH. Measurement of acetabular version on the axiolateral radiograph. Clin Orthop Relat Res. 1995;316:106–111. [PubMed] [Google Scholar]