Abstract
Arthroscopic lateral release refers to an arthroscopic procedure that incises the lateral stabilizing structures of the patella, in particular, the lateral retinaculum. The lateral retinaculum attaches the lateral patella to the lateral femoral epicondyle, the iliotibial band, and the anterolateral tibia. Arthroscopic lateral release rarely is performed as an isolated procedure and rather is generally performed in combination with medially based stabilization procedures to more effectively allow for medial realignment. The procedure is relatively simple and straightforward, but, if not done for the appropriate indications or if done technically poorly, either it will not achieve the desired result or it may result in additional pain, instability, and weakness. This In Brief article provides an overview of potential complications of lateral release.
Avoidance of Major Complications
To reduce pain and improve patellar tracking, before surgery the surgeon must consider if the indications are appropriate, if other concomitant procedures are needed, if the patterns of patellar and trochlear chondral wear are appropriate, and if the patella is hypermobile. In particular, this includes physical examination notation of patellar tracking, glide, tilt, and lower extremity alignment that may require concomitant medially based tightening or stabilizing procedures. Intraoperatively, care must be taken to avoid excessive release or insufficient release of the retinaculum, achieve good hemostasis, and avoid cautery burns. Postoperatively, motion should be initiated immediately.
Detection and Treatment of Major Complications
Postoperative hemarthrosis should be managed with reassurance, compression, ice, pain medication, and sometimes aspiration or surgical evacuation with cauterization if it inhibits postoperative rehabilitation. Dermal or skin burns need to be managed with wound management and possible plastic surgery consultation. Medial instability may be managed with physical therapy or revision with lateral retinacular repair, and continued pain may require medication, injections, or arthroscopic debridement or patellofemoral replacement.
Summary
Lateral release involves incising the lateral retinaculum of the patellofemoral joint to reduce the lateral vector of force on the patella or to reduce the lateral compressive forces on the lateral patellofemoral joint [3, 4]. The potential benefits are reduction in pain and improvement in patellar stability if done appropriately based on correct indications and technical application. Potential long-term complications are weakening of the extensor function of the knee, creating medial patellar instability, worsening patellofemoral pain, burning the skin from an aggressive release, and failing to correct the original disorder. The only real short-term complication is hemarthrosis. Some errors in judgment (Table 1) and technical errors (Table 2) may affect the result of surgery.
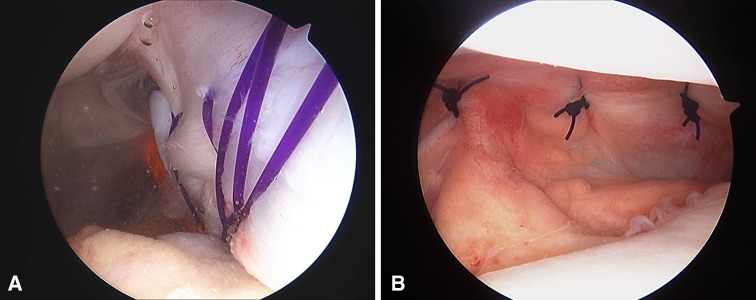
Fig. 1A–B.
(A) An arthroscopic view shows 4-0 PDS (Ethicon Inc, Somerville, NJ, USA) sutures placed arthroscopically incorporating the medial retinaculum for a medial plication. (B) An arthroscopic view of the completed medial retinacular repair is shown.
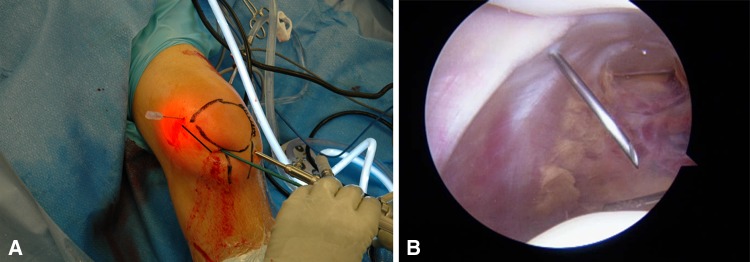
Fig. 2A–B.
The surgeon should correlate the (A) external and (B) internal anatomy to ensure that excessive release is not done proximally. In Illustration A, a line is drawn depicting the course of a lateral release. Illustration B shows the muscle fibers of the vastus lateralis proximal to the spinal needle.
Fig. 3.
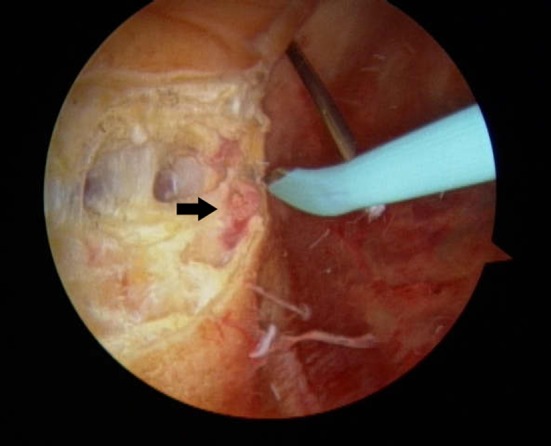
Fibers of the vastus lateralis define the proximal extent of the release (arrow).
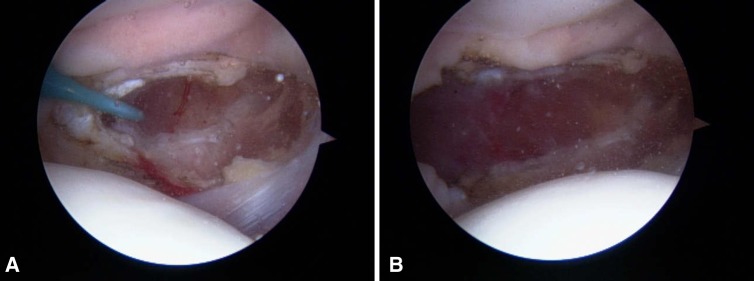
Fig. 4A–B.
(A) The right side of the screen is proximal. The cautery is advanced from proximal to distal to insure adequate release. (B) The completed lateral release is shown.
Table 1.
Complications related to errors in diagnosis and judgment
| Complication | Clinical effect | Prevention | Detection | Remedy |
|---|---|---|---|---|
| Medial laxity persists [3, 4, 6, 9, 11, 12, 14] | Symptoms unchanged | Use correct indications: only clinical indication for isolated procedure is lateral patellar compression syndrome, occasional adult patient with refractory recurrent instability [19]; otherwise adults or children with acute or recurrent instability warrant medial tightening or stabilizing procedure; physical examination of excessive lateral translation of patella with neutral or positive tilt warrants medial tightening or stabilizing procedure; medial tightening procedures include medial retinacular imbrication and medial patellofemoral ligament (MPFL) (Fig. 1) reconstruction or repair | Postoperative symptoms unchanged from preoperative owing to medial laxity: pain, patella instability | Repeat surgery with medial tightening procedure, rehabilitation, alternative interventions appropriate to diagnosis |
| Failure to identify medial patellar or trochlear chondral damage [4, 15] | Transfer pain to medial patellofemoral joint | Thorough arthroscopic evaluation and preoperative imaging examinations to rule out medial chondral injury and abort release if other options available | Postoperative symptoms of medial patellofemoral pain, increased patellofemoral crepitation, increased swelling, or increased pain over medial patellar facet and trochlea by examination | NSAIDs, viscosupplementation, arthroscopic debridement or microfracture of medial lesion |
| Failure to identify patellofemoral arthritis [1, 3, 7, 8] | Continued pain | Do not perform in patients with moderate patellofemoral arthritis by imaging and arthroscopic assessment | Pain/dissatisfaction with procedure | NSAIDs, viscosupplementation, steroid injection, patellofemoral replacement |
| Failure to identify hypermobile patella [3, 4, 7, 8, 13] | Patella medially unstable | Thorough physical examination, history; medial patellar glide less than two quadrants, patellar tilt negative | Postoperative medial instability | Physical therapy with lateral strengthening, bracing, revision partial lateral retinacular repair |
| Inadequate postoperative motion/rehabilitation [3, 4] | Symptoms unchanged | Initiate immediate postoperative motion | Postoperative examination similar to preoperative; postoperative motion needed to maintain separation of retinacular incision to optimize lengthening of retinaculum; keeping the knee in extension after surgery may result in some healing of the retinaculum with little separation thereby defeating the purpose of the release | Physical therapy, repeat surgery |
Table 2.
Complications related to technical errors at the time of surgery
| Complication | Clinical effect | Prevention | Detection | Remedy |
|---|---|---|---|---|
| Excessive release [4, 7, 13] | Medial instability | Do not release vastus lateralis unless salvage/refractory (Fig. 2) | Medial patella subluxation/dislocation, excessive medial glide, medial apprehension test, positive gravity subluxation test | Revision with lateral retinacular repair and imbrication/bracing/rehabilitation |
| Excessive release [2, 3] | Weakness | Do not release vastus lateralis unless salvage/refractory | Significant quadriceps weakness by examination with atrophy | Revision with lateral retinacular repair and imbrication/bracing/rehabilitation |
| Insufficient release [3, 5] | Symptoms unchanged | Release to level of muscle fibers proximally and include patellotibial ligament distally (Figs. 3 and 4) | Postoperative examination similar to preoperative | Ensure adequate release intraoperatively (observe muscle fibers) and extend to anterolateral portal |
| Failure to cauterize superolateral geniculate [3, 4, 16–18] | Painful hemarthrosis | Reduce pressure or flow to identify bleeding before closure, use cautery device, do not elevate tourniquet unless necessary | Postoperative hemarthrosis | Ice, compression, pain medications, modalities, aspiration, repeat arthroscopy with evacuation of hematoma/cauterization |
| Failure to avoid past point with cautery and maintain visualization [3, 10] | Burn skin/dermis | Avoid past point with cautery and maintain visualization | Skin burn | Local wound care |
Footnotes
Each author certifies that he or she, or a member of their immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
References
- 1.Aderinto J, Cobb AG. Lateral release for patellofemoral arthritis. Arthroscopy. 2002;18:399–403. doi: 10.1053/jars.2002.32306. [DOI] [PubMed] [Google Scholar]
- 2.Blasier RB, Ciullo JV. Rupture of the quadriceps tendon after arthroscopic lateral release. Arthroscopy. 1986;2:262–263. doi: 10.1016/S0749-8063(86)80082-2. [DOI] [PubMed] [Google Scholar]
- 3.Ford DH, Post WR. Open or arthroscopic lateral release: indications, techniques, and rehabilitation. Clin Sports Med. 1997;16:29–49. doi: 10.1016/S0278-5919(05)70006-5. [DOI] [PubMed] [Google Scholar]
- 4.Fulkerson JP. Diagnosis and treatment of patients with patellofemoral pain. Am J Sports Med. 2002;30:447–456. doi: 10.1177/03635465020300032501. [DOI] [PubMed] [Google Scholar]
- 5.Hallisey MJ, Doherty N, Bennett WF, Fulkerson JP. Anatomy of the junction of the vastus lateralis tendon and the patella. J Bone Joint Surg Am. 1987;69:545–549. [PubMed] [Google Scholar]
- 6.Hautamaa PV, Fithian DC, Kaufman KR, Daniel DM, Pohlmeyer AM. Medial soft tissue restraints in lateral patellar instability and repair. Clin Orthop Relat Res. 1998;349:174–182. doi: 10.1097/00003086-199804000-00021. [DOI] [PubMed] [Google Scholar]
- 7.Hughston JC, Deese M. Medial subluxation of the patella as a complication of lateral retinacular release. Am J Sports Med. 1988;16:383–388. doi: 10.1177/036354658801600413. [DOI] [PubMed] [Google Scholar]
- 8.Kolowich PA, Paulos LE, Rosenberg TD, Farnsworth S. Lateral release of the patella: indications and contraindications. Am J Sports Med. 1990;18:359–365. doi: 10.1177/036354659001800405. [DOI] [PubMed] [Google Scholar]
- 9.Krompinger WJ, Fulkerson JP. Lateral retinacular release for intractable lateral retinacular pain. Clin Orthop Relat Res. 1983;179:191–193. doi: 10.1097/00003086-198310000-00029. [DOI] [PubMed] [Google Scholar]
- 10.Lord MJ, Maltry JA, Shall LM. Thermal injury resulting from arthroscopic lateral retinacular release by electrocautery: report of three cases and a review of the literature. Arthroscopy. 1991;7:33–37. doi: 10.1016/0749-8063(91)90074-8. [DOI] [PubMed] [Google Scholar]
- 11.Myers P, Williams A, Dodds R, Bulow J. The three-in-one proximal and distal soft tissue patellar realignment procedure: results, and its place in the management of patellofemoral instability. Am J Sports Med. 1999;27:575–579. doi: 10.1177/03635465990270050501. [DOI] [PubMed] [Google Scholar]
- 12.Nietosvaara Y, Paukku R, Palmu S, Donell ST. Acute patellar dislocation in children and adolescents: surgical technique. J Bone Joint Surg Am. 2009;91(suppl 2 pt 1):139–145. doi: 10.2106/JBJS.H.01289. [DOI] [PubMed] [Google Scholar]
- 13.Nonweiler DE, DeLee JC. The diagnosis and treatment of medial subluxation of the patella after lateral retinacular release. Am J Sports Med. 1994;22:680–686. doi: 10.1177/036354659402200517. [DOI] [PubMed] [Google Scholar]
- 14.Palmu S, Kallio PE, Donell ST, Helenius I, Nietosvaara Y. Acute patellar dislocation in children and adolescents: a randomized clinical trial. J Bone Joint Surg Am. 2008;90:463–470. doi: 10.2106/JBJS.G.00072. [DOI] [PubMed] [Google Scholar]
- 15.Sallay PI, Poggi J, Speer KP, Garrett WE. Acute dislocation of the patella: a correlative pathoanatomic study. Am J Sports Med. 1996;24:52–60. doi: 10.1177/036354659602400110. [DOI] [PubMed] [Google Scholar]
- 16.Schneider T, Fink B, Abel R, Jerosch J, Schulitz KP. Hemarthrosis as a major complication after arthroscopic subcutaneous lateral retinacular release: a prospective study. Am J Knee Surg. 1998;11:95–100. [PubMed] [Google Scholar]
- 17.Small NC. An analysis of complications in lateral retinacular release procedures. Arthroscopy. 1989;5:282–286. doi: 10.1016/0749-8063(89)90142-4. [DOI] [PubMed] [Google Scholar]
- 18.Vialle R, Tanguy JY, Cronier P, Fournier HD, Papon X, Mercier P. Anatomic and radioanatomic study of the lateral genicular arteries: application to prevention of postoperative hemarthrosis after arthroscopic lateral retinacular release. Surg Radiol Anat. 1999;21:49–53. doi: 10.1007/BF01635052. [DOI] [PubMed] [Google Scholar]
- 19.Woods GW, Elkousy HA, O’Connor DP. Arthroscopic release of the vastus lateralis tendon for recurrent patellar dislocation. Am J Sports Med. 2006;34:824–831. doi: 10.1177/0363546505282617. [DOI] [PubMed] [Google Scholar]