Abstract
Background
Lateral release of a tight lateral retinaculum in a TKA is intended to correct patellar maltracking but the widely used inside-out technique has associated risks. We describe an alternate stepwise outside-in technique, with titrated release intended to maximize the chance of preserving the superior lateral genicular artery (SLGA).
Description of Technique
Patellar maltracking was judged by a no-thumb technique and graded as I and Ia: normal and near normal tracking; II: patella tilted; III: patella subluxed; or IV: patella dislocated. Outside-in release was performed in three progressive steps. Step-1 release was from the midpatella to the upper tibial border, Step-2 release was from the midpatella to the proximal pole of the patella, and Step-3 release was proximal to the superior pole of the patella with sectioning of the SLGA.
Methods
We retrospectively reviewed records of 1884 patients operated on between 2002 to 2008. Two hundred five patients (11%) had lateral release performed, and 177 of those 205 patients (86%) were reviewed. Patellofemoral function was assessed clinically by The Knee Society score. Radiographs were examined for patellar tilt, shift, and avascular necrosis. The minimum followup was 22 months (median 48 months; range, 22–105 months).
Results
The SLGA was preserved in 155 (76%) patients. At last followup, no patient had patellar maltracking, patellar fracture, or avascular necrosis. Six of 177 (3%) patients had anterior knee pain. Female patients and high-flex components had a higher incidence of release and midvastus arthrotomy had a lower incidence of release.
Conclusions
Stepwise release of the lateral retinaculum by an outside-in technique allowed minimum necessary retinacular release, preserving the SLGA in 76% of patients. No complications were seen at followup with functional and radiographic examinations.
Level of Evidence
Level IV, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Patellar maltracking in TKA can cause a range of postoperative problems such as chronic pain, restricted ROM, and can hamper ambulation with frank dislocation [23, 25, 26]. The incidence of patellar-related issues complicating knee arthroplasty varies between 4% and 10% [3, 7, 20, 21]. Patellar maltracking can be dealt with in several ways at surgery. Lateral release of the tight lateral retinaculum is one well-described option in the literature [14, 34] and has been reported as being performed in 3.8% to 45% of patients [18–21, 37]. Complications include patellar avascularity [24, 31, 36] and patellar fracture [29, 31, 35]. Pie crusting of the retinaculum and lateral peel are other less frequently used techniques [5, 11, 32].
Inside-out and outside-in techniques used for lateral release reportedly improve patellar tracking [12, 20, 21, 34, 37]. The inside-out technique is used more frequently because of its ease of performing, ie, in an already opened joint. However, this involves breaching the synovial cover, which exposes the joint to the subcutaneous plane under the skin. Thus, the potential chances of wound discoloration and risk of spread of superficial infection into the joint are increased [15]. However, with the outside-in technique, the synovial cover is left intact under the retinaculum, with no direct exposure of the joint to the subcutaneous plane [34].
In 2009 Strachan et al. reported a “staged” (six stages) outside-in technique in a proximal to distal manner [34]. We began using an outside-in technique in 2000 and have developed it in a manner that is simple to perform. Our technique allows the lateral release to be titrated in a stepwise, progressive manner. The literature does not describe any stepwise release with the inside-out technique. Technically, we found it was easier to control the extent of release when viewed from outside, in relation to the patella than from inside the joint. Our stepwise release is in a distal to proximal manner, which allows us to minimize the extent of release according to need and maximize the chances of preserving the superior lateral genicular artery (SLGA).
We describe our surgical technique performed in 205 of 1884 TKAs. For this study, we (1) determined the number of cases in which the SLGA was preserved; (2) determined whether there was a correlation between the grade of patellar maltracking corrected and the extent of lateral release; (3) assessed patellofemoral function and radiographic patellar tilt, shift, avascularity, and fracture in 177 of these knees; (4) determined whether surgical approach, type of joint implant, and use of computer-assisted surgery (CAS) had any effect on the incidence of lateral release; and (5) determined whether sex and type of preoperative deformity had any effect on the frequency of lateral release.
Surgical Technique
All surgeries were performed by the senior author (RNM) with use of a pneumatic tourniquet, inflated with the knee in flexion. The skin incision was anterior midline. The arthrotomy was either a medial parapatellar or midvastus. The lateral patellofemoral ligament was released as part of the joint approach. The patellar cut was made by partial eversion to 90° and then subluxated laterally. Partial fat pad excision and a tibial cut first method was used. The transepicondylar line was the reference for femoral component rotation, which was further verified with the tibial cut in 90° flexion. The femoral component was centralized on the femur in the mediolateral axis with no lateralization. Tibial component rotation was established to match the femoral component with trial implants in place and the knee in extension. Original patellar thickness was maintained. The patellar button was medialized sufficiently to rest in the middle of the femoral groove. Patellar tracking was evaluated with trial implants in place. The implants then were cemented and the tourniquet deflated. Patellofemoral tracking was reevaluated from full extension to full possible flexion, using the no-thumb technique. The senior author (RNM) devised the following grading system (Table 1) Grade I and Ia: normal and near normal tracking (Fig. 1A–B); Grade II: patella tilted (Fig. 2); Grade III: patella subluxed (Fig. 3); and Grade IV: patella dislocated. All patients with Grades 2, 3, and 4 tracking underwent lateral release. Twenty patients with Grades 1 and 1a tracking also had release owing to excessive lateral overhang of the femoral component.
Table 1.
Grading of patellar tracking
| Grade | Definition | Description |
|---|---|---|
| 1 | Normal tracking | Patellar insert in full contact with the femoral component trochlear groove medially and laterally (Fig. 1A) |
| 1a | Near-normal tracking | Same as Grade 1, except that the medial facet of the patella is lifted off the medial femoral trochlea; the separation of the patellar medial facet from the medial femoral trochlea is less than 2 mm (Fig. 1B) |
| 2 | Tilting of patella | Similar to Grade 1a, except that the patellar medial facet is lifted away from the medial femoral trochlea by more than 2 mm (Fig. 2) |
| 3 | Subluxation of patella | The medial and lateral facets of the patellar insert are not in contact with their respective parts on the trochlear groove, but some portion of the laterally displaced insert is still in contact with the metal of the femoral component (Fig. 3) |
| 4 | Dislocation of patella | The patellar insert is completely displaced lateral to the femoral component and not in contact with any part of the metal |
Fig. 1A–B.
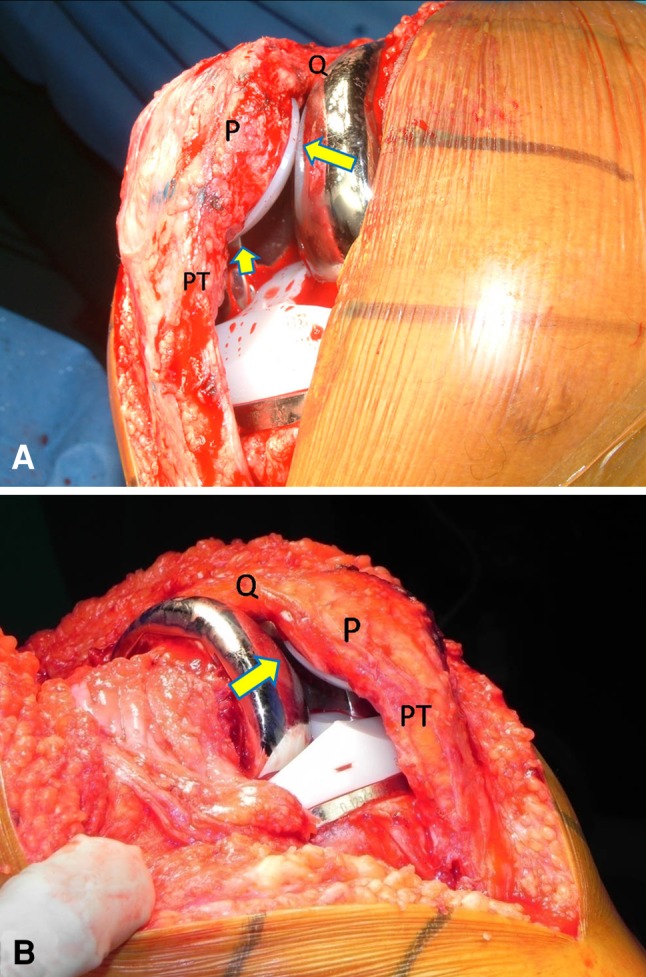
(A) Grade 1 tracking (normal tracking) is shown. The medial facet is touching the medial femoral trochlea (large arrow). The lateral facet is touching the lateral femoral trochlea (small arrow). (B) Grade 1a tracking (near-normal tracking) is shown. The medial facet of the patella is lifted off the medial femoral trochlea by less than 2 mm (arrow). Q = quadriceps; P = patella; PT = patellar tendon.
Fig. 2.
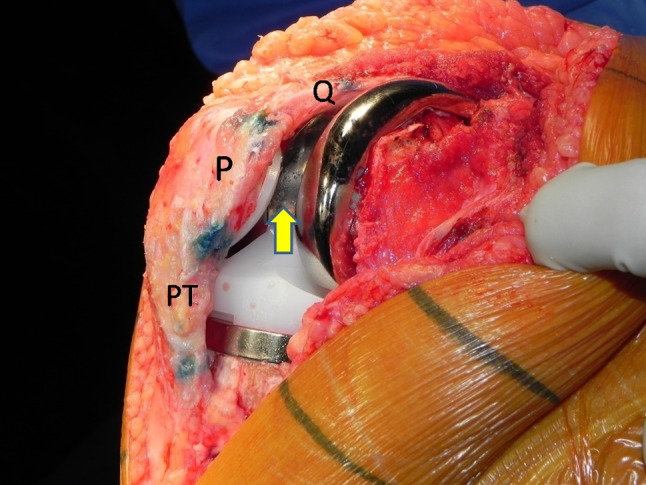
Grade 2 tracking is shown. The medial facet of the patella is lifted off the medial femoral trochlea by more than 2 mm (arrow). Q = quadriceps; P = patella; PT = patellar tendon.
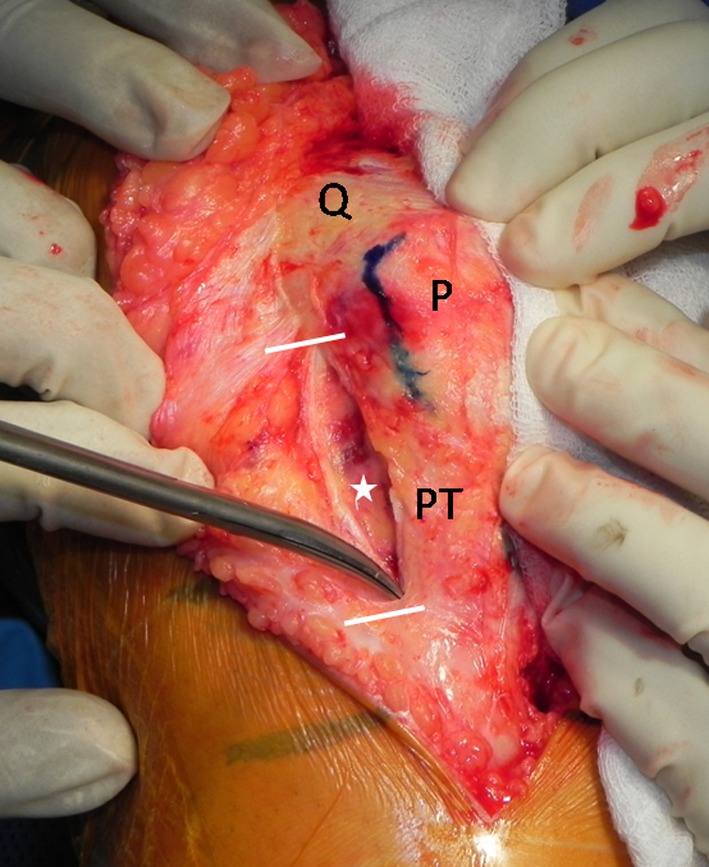
Fig. 3.
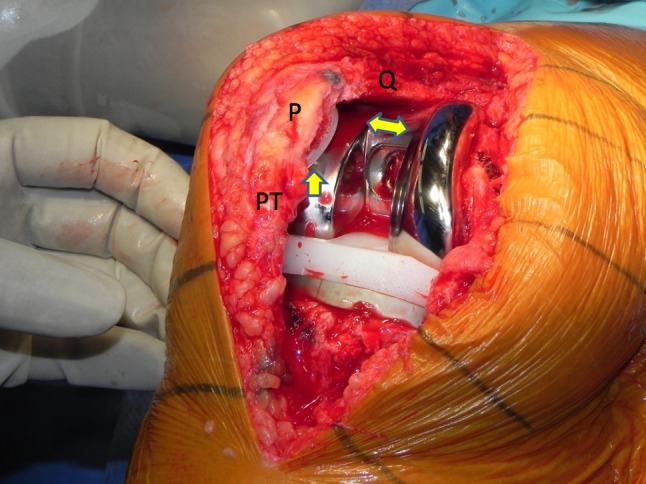
Grade 3 tracking is shown. The medial and lateral facets of the patellar insert are not in contact with their respective parts on the trochlear groove (double arrow). A portion of the laterally displaced medial facet is in contact with the lateral aspect of the femoral component (small arrow). Q = quadriceps; P = patella; PT = patellar tendon.
Our outside-in technique started with raising the lateral skin flap over the patella in a plane deep to the deep fascia to expose the lateral retinaculum. A nick with a sharp Number 15 blade was made in the retinaculum at the midpatellar level 1 cm lateral to the patella (Fig. 4). Step 1 consisted of first separating the retinaculum from the synovial lining underneath, then splitting distally from this starting point to the upper tibial border (Fig. 5). Dissecting scissors were used for this step, taking care not to puncture the synovial lining. Tracking was reexamined to assess the need for a Step 2 release.
Fig. 4.
The beginning of an outside-in lateral retinacular release is shown. A Number 15 surgical blade is used to nick the retinaculum 1 cm lateral to the patella at the midpatellar level. Q = quadriceps; P = patella; PT = patellar tendon.
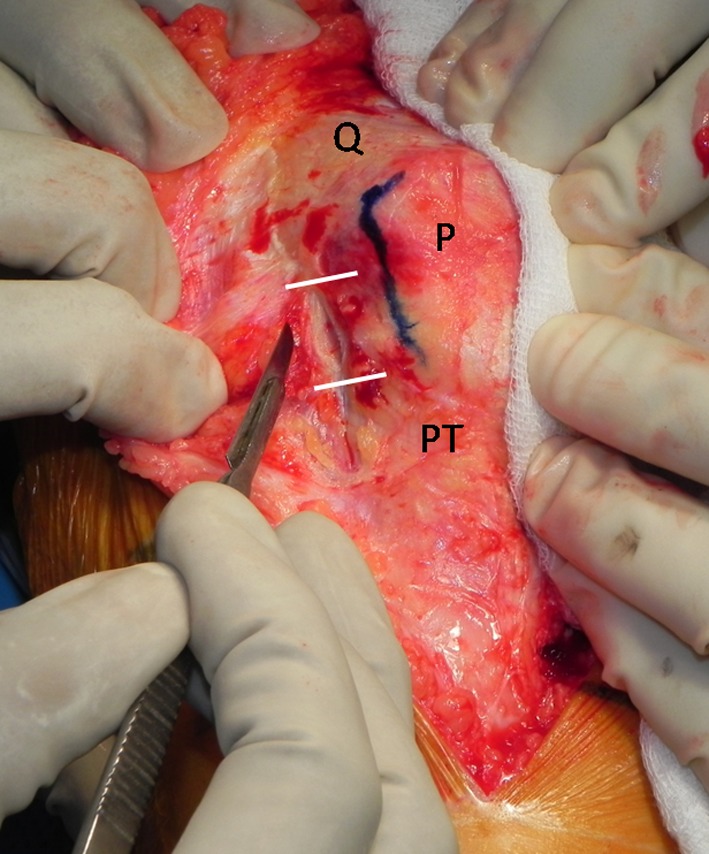
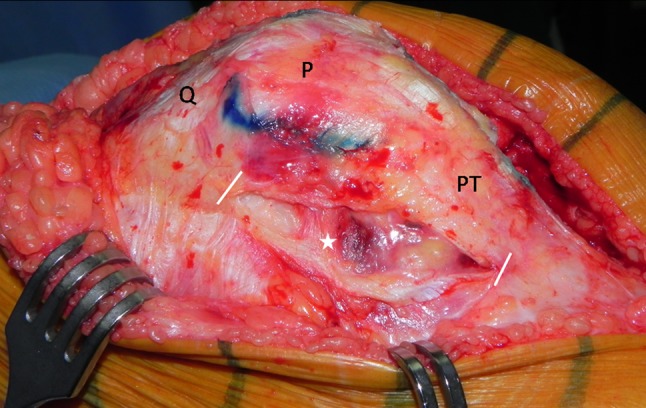
Fig. 5.
Step 1 release is shown. The two white marks show the extent of release from the midpatella to the upper tibial border. The star represents the intact synovial membrane. Q = quadriceps; P = patella; PT = patellar tendon.
Step 2 consisted of slitting the retinaculum from the starting point, and proceeding proximally to the superior patellar border (Fig. 6). These thicker fibers required stronger, sharp scissors. The SLGA, located proximal to the superior pole of the patella, thus far has been preserved. Tracking was rechecked. Only if needed, a Step 3 release was performed.
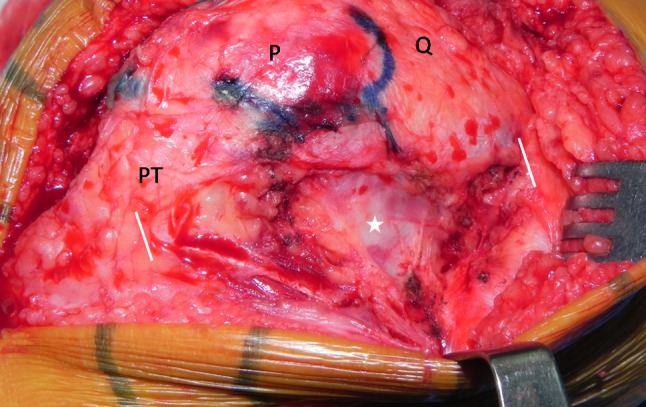
Fig. 6.
Step 2 release is shown. The release extends from the midpatella to the upper patellar border proximally. The two white marks show the extent of the Step 2 release. The star represents an intact synovial membrane. Q = quadriceps; P = patella; PT = patellar tendon.
In Step 3, the release continued further proximally from the superior patellar border, staying lateral to the vastus lateralis. This step involved splitting the SLGA. Both cut ends exhibited pulsatile bleeding, which were easily cauterized. The release was extended proximally until the thick fibers gave way to relatively thin, loose fibers (Fig. 7).
Fig. 7.
Step 3 release is shown. The release extends more proximally from the upper patellar border. The cut ends of the SLGA are cauterized. The two white marks show the full extent of the Step 3 release. The star represents intact synovial membrane. Q = quadriceps; P = patella; PT = patellar tendon.
This technique is noteworthy because it allows stepwise release (Table 2), which ensures minimum necessary release to achieve correct patellar tracking (Grade 1 or 1a). At each step, tracking must be checked to assess the need to proceed with further release. Any inadvertent synovial nick was secured with an absorbable suture.
Table 2.
Stepwise release of the lateral retinaculum
| Step | Definition | Description |
|---|---|---|
| 1 | Release of distal part | Release of the lateral retinaculum starting from the midlevel of the patella, progressing distally to the upper tibial border (Figs. 4, 5) |
| 2 | Partial release of proximal part | Release of the lateral retinaculum starting from midlevel of the patella, progressing proximally up to the proximal border of the patella; the lateral superior genicular artery is preserved (Fig. 6) |
| 3 | Complete release of proximal part | Further release of the retinaculum from the superior border of the patella, progressing proximally, lateral to the vastus lateralis, for approximately 2 to 4 cm; this includes release of the lateral superior genicular artery tether and cauterization of the vessel (Fig. 7) |
Patients and Methods
The senior author (RNM) has been using the outside-in technique for lateral release since 2000 in preference to the inside-out technique, which he had used before 2000. We retrospectively reviewed the records of 1884 patients undergoing TKAs between February 2002 and December 2008. Preoperative and operative records of all 1884 patients were studied to note patient sex, type of surgical approach used, type of joint implant used, whether CAS was used, and the type of preoperative deformity treated. We identified 205 patients (11%) in whom lateral release was performed by the outside-in surgical technique described. The following parameters related to the technique were recorded for these 205 patients: grade of patellar maltracking, step of lateral release performed, patency of the SLGA, and the need to put in a suture for the synovial lining. During the study period, the same implant series (PFC Sigma®; DePuy Orthopaedics, Warsaw, IN, USA) was used for all patients. All implants were cemented and all patients had patellar resurfacing, using a three-lug all-polyethylene component. The surgical technique remained the same, except for two changes. We started using computer navigation in July 2004 and a midvastus approach in preference to medial parapatellar arthrotomy in August 2007. Among the 205 knees, 20 were corrected for Grade 1 patellar maltracking, 132 for Grade 2, 52 for Grade 3, and one for Grade 4. Correction by Step 1 release was performed in 17 knees, Step 2 release in 138, and Step 3 release in 50. In 132 knees with Grade 2 maltracking, 92 were corrected by Step 2 release, 30 by Step 3 release, and 10 by Step 1 release. In 52 knees with Grade 3 maltracking, 34 were corrected by Step 2 release, 16 by Step 3 release, and two by Step 1 release. The single patient with Grade 4 maltracking needed Step 3 release.
We recalled all patients who underwent a lateral release for review for the purpose of this study; 12 had died and 16 were lost to followup. These 28 exclusions left 177 patients followed clinically and radiographically. The minimum followup was 22 months (median, 48 months; range, 22–105 months). The Knee Society score (KSS) [13] was used. We specifically inquired about anterior knee pain and if present, we asked the patient to quantify the pain from 0 to 10 on a VAS scale [1], and the location of the pain was noted. Patellofemoral crepitation or clunk if detected was recorded. We performed radiographic evaluation according to The Knee Society’s radiographic evaluation scoring system [9]. Skyline views of the knee were taken in 30° flexion as described by Laurin et al. [22], maintaining the same position as in the preoperative skyline views. Two authors (RNM, SSR) assessed preoperative, immediate postoperative, and followup patellar tilt and shift [6, 10]. Because radiographs were not standardized for magnification in our study, only patellar tilt was measured quantitatively whereas patellar shift was noted for its presence. Measurements were performed by both investigators on two occasions 3 months apart. Chia et al. [6] calculated the reliability of the radiographic measurements for patellar shift and tilt by calculating the intraclass coefficient for selected parameters on 40 sets of measurements. The interobserver and intraobserver intraclass coefficients in their study, calculated using a two-way mixed model based on measures of absolute agreement, were greater than 0.9 for patellar shift and tilt. The latest followup radiographs were scrutinized for evidence of patellar avascularity. Features suggestive of patellar avascularity were defined as major changes in the radiodensity, present singly or combined with fracture, and substantial remodeling or fragmentation [33]. Patellae with no alteration in radiodensity were judged as having no evidence of avascularity.
Interobserver agreement for assessing the tracking grade was tested on 30 patients, using three observers, by Kappa statistic. The kappa statistic for interobserver agreement of patellar maltracking was 0.96 (p < 0.001).
Correlation between grade of patellar maltracking and the step of release was assessed by Spearman’s rank correlation test. The odds ratios (ORs) for lateral release were calculated with 95% CI, for intraoperative factors of surgical approach, type of joint implant, and use of CAS (Table 3). The ORs for lateral release were calculated with 95% CI for preoperative factors of sex and type of preoperative deformity (Table 3). We used SPSS® Version 10.0 (SPSS Inc, Chicago, IL, USA) for statistical analyses.
Table 3.
Comparison of lateral release rate in relation to implant types, approach, sex and use of navigation.
| Factor | Total number of patients | Patients with lateral release Number (%) |
Odds ratio (95% CI)* |
|---|---|---|---|
| Males | 388 | 12 (3.1%) | OR = 0.22 (0.11 to 0.39) p < 0.001 |
| Females | 1496 | 193 (12.9%) | |
| Varus | 1819 | 194 (10.7%) | OR = 0.59 (0.29 to 1.26) p = 0.11 |
| Valgus | 65 | 11 (16.9%) | |
| Fixed bearing | 1123 | 116 (10.4%) | OR = 0.87 (0.64 to 1.18) p = 0.35 |
| Mobile bearing | 761 | 89 (11.7%) | |
| High flex | 53 | 11 (20.8%) | OR = 2.22 (1.01 to 4.48) p = 0.018 |
| Standard Implant | 1831 | 193 (10.5%) | |
| Midvastus approach | 451 | 24 (5.3%) | OR = 0.39 (0.24 to 0.61) p < 0.001 |
| Medial parapatellar approach | 1433 | 181 (12.6%) | |
| CAS | 1423 | 161 (11.3%) | OR = 1.21 (0.84 to 1.76) p = 0.29 |
| Conventional | 461 | 44 (9.5%) |
* For each factor, the odds ratio (OR) was calculated with its 95% CI. If the CI included 1, the OR was not significant.
Results
Among the original 205 knees normal (Grade 1) tracking was achieved in 159 (78%) knees and near-normal (Grade 1a) tracking was achieved in 46 (22%) knees. The SLGA could be preserved in 155 knees (76%).
Tracking grade weakly correlated (ρ = 0.17; p = 0.012) with release step (Table 4). Including eight patients (4%) in whom the synovial lining was inadvertently nicked and repaired by a single stitch, no patient had any skin discoloration or abnormal swelling over the area of the lateral release.
Table 4.
Extent of release required based on prerelease tracking grade
| Prerelease tracking | Number of patients | Spearman’s rank correlation test | |||
|---|---|---|---|---|---|
| Step 1 release | Step 2 release | Step 3 release | Total | ||
| Grade 1 | 5 (25%) | 12 (60%) | 3 (15%) | 20 | p = 0.0123* ρ [rho] = 0.1746** |
| Grade 2 | 10 (7.6%) | 92 (69.7%) | 30 (22.7%) | 132 | |
| Grade 3 | 2 (3.9%) | 34 (65.4%) | 16 (30.8%) | 52 | |
| Grade 4 | 0 | 0 | 1 (100%) | 1 | |
* Significant correlation; **Spearman’s rank correlation coefficient less than 0.7 is of little importance.
All 177 patients available for clinical review continued to use their surgically treated knee and none had undergone revision. The average KSS was 96 for pain and 80 for function compared with preoperative scores of 31 for pain and 55 for function. Average postoperative flexion was 121° (range, 75°–145°). No patient had clinical evidence of patellar maltracking at latest followup. Patellofemoral crepitus was seen in 36 patients, of which only two complained of pain on inquiry. One patient of the remaining 34 pain-free patients had an arthroscopic débridement earlier for painful patellar clunk syndrome. Three patients reported anterior knee pain but had no crepitus. In all, anterior knee pain was reported in six patients (3.4%) and the average VAS scale score was 3. All patients with anterior knee pain had central patellar tracking with no shift observed on postoperative skyline views. Radiographically, preoperative skyline views showed normal placement of the patella in 107 knees, lateral shift in five, lateral tilt in 33, and lateral shift with tilt in 32. The latest followup skyline views showed lateral shift in six knees and lateral tilt in 12. In the remaining 159 patients, the patella was central in 131 and medially tilted in 28. No patient had patellar fracture. No avascular necrosis was diagnosed up to 9 years.
The OR for lateral release was less (OR 0.39; p < 0.001) with midvastus arthrotomy and more (OR 2.22; p = 0.018) with high-flex implants (Table 3). However, we found no difference between CAS versus conventional (OR 1.21; p = 0.29) or between fixed-bearing versus mobile implants (OR 0.87; p = 0.35). The odds for release was less (OR 0.22; p < 0.001) for male gender but similar (OR 0.59; p = 0.11) for varus versus valgus knees (Table 3).
Discussion
Lateral release of a tight lateral retinaculum is performed to correct patellar maltracking. With the inside-out technique, the synovial lining has to be cut first. This creates a potential escape route for an intraarticular hematoma into the subcutaneous plane, tenting the lateral skin flap and affecting its vascularity [15]. In addition, in case of skin breakdown or the hematoma getting colonized, the joint would be directly affected. This does not happen with the outside-in technique as the synovial lining is left intact. Our primary aim was to describe our outside-in technique developed toward stepwise, titrated release, which maximizes the chances of preserving the SLGA. We then determined (1) the number of cases in which the SLGA was preserved; (2) whether there was correlation between the grade of patellar maltracking and the extent of lateral release; (3) patellofemoral function and radiographic patellar tilt, shift, avascularity, or fracture; (4) whether surgical approach, type of joint implant, and use of CAS affected the incidence, and (5) whether sex and type of preoperative deformity affected the incidence.
We acknowledge limitations of this study. First, grading of patellar maltracking and patency of the SLGA were judged by clinical observation. Ritter et al. [29] used similar observations for patency. Although postoperative angiography would allow objective evidence of patency, it was not practical to implement. Our experience suggests that the SLGA being of a larger caliber with pulsatile flow, its bleeding cannot be missed if it is transected, when the area superior to the upper patellar border is examined in flexion and extension. Second, patellar avascularity was judged on radiographic analysis rather than on scintigraphy. A temporary phase of avascularity in the early postoperative period [31] could have been missed since our review was after 2 years. Third, patellar shift could not be quantified owing to lack of standardization in magnification of the radiographs. Fourth, we have not tried to correlate intraoperative maltracking with preoperative and postoperative skyline views, which could be a subject of a separate study.
The patella is supplied by six arteries [4, 30]. The medial parapatellar approach sacrifices the supreme and two medial genicular arteries. A lateral meniscectomy and retropatellar fat excision would sacrifice the lateral inferior genicular artery and anterior tibial recurrent artery. This leaves the lateral superior genicular artery as the main patellar blood supply after TKA. We could preserve the SLGA in 76% of patients. Kusuma et al. [19] came to a similar conclusion, whereas Ritter et al. [29] reported preservation of the SLGA in only 25% of patients with lateral release (Table 5).
Table 5.
Literature review comparing patellar complications after lateral release
| Study | Type of release | Followup (months)* | Number of lateral releases (total number of patients) | Lateral release rate | % of lateral releases sacrificing SLGA | Number of lateral releases with patellar avascular necrosis/radiolucency | Number of lateral releases with patellar loosening | Number of lateral releases with patellar fracture | Number of lateral releases with anterior knee pain |
|---|---|---|---|---|---|---|---|---|---|
| Ritter and Campbell [28] | Not described | (12–120) | 84 (555) | 15% | 100% | 4 (4.8%) | 1 (1.5%) | ||
| Ritter et al. [29] | Not described | 428 (1205) | 35% | 75% | 1 (0.23%) | 10 (2.34%) | 17 (3.97%) | ||
| Kusuma et al. [19] | Not described | 56.4 | 314 (1108) | 28% | 1 | 0.3% | |||
| Strachan et al. [34] | Outside-in | 96 | ? 0% | 3 (3.1%) | |||||
| Current study | Outside-in | 54 (22–105) | 205 (1884) | 10.6% | 25% | 0 | 0 | 0 | 6 (3.4%) |
* Values are expressed as mean, with range in parentheses; SLGA = superior lateral geniculate artery.
We found a weak correlation between patellar tracking grade with release steps. A literature review does not show any study of such correlation.
At last followup the incidence of anterior knee symptoms was low (3.4%). No patient had avascular necrosis or fracture of the patella. Our technique involves release being performed 1 cm away from the lateral patellar border, which preserved the collateral circulation [4, 16]. Ritter et al. [29] reported a higher incidence of patellar fractures with lateral release (Table 5).
The incidence of lateral release during TKA is reported between 3.8% to 45% in the literature (Table 6). In our study encompassing a large number of TKAs (n = 1884) during a 6-year period, the lateral release incidence was 11%. However, our indications for lateral release erred more toward doing the procedure. In addition to performing release for all Grades 2, 3, and 4 patellar tracking cases, it also was performed in 1% of patients (20 knees) who had normal tracking (Grade 1 and 1a), for substantial anterolateral overhang of the femoral component tenting the retinaculum. The lateral release rate was lower when a midvastus arthrotomy was used (5%) compared with a medial parapatellar arthrotomy (13%). Kelly et al. [18] and Engh et al. [8] reported similar findings (Table 6). With a midvastus arthrotomy, the pull of the still-attached vastus medialis negates the pull of the laterally attached vastus lateralis and rectus femoris. This leads to better extensor mechanism centralization and lesser need for lateral release. Some surgeons therefore no longer use the no-thumb technique with a medial parapatellar arthrotomy whereas some use a temporary single stitch to hold the vastus medialis obliquus to the patella while assessing tracking [2]. The literature is divided regarding whether mobile-bearing implants lower the incidence of lateral release owing to bearing rotation and a better centralized extensor mechanism. Yang et al. [37] reported fewer lateral releases in mobile bearing group while Pagnano et al. [27] found no difference (Table 6). We also found no difference in the incidence between fixed- and mobile-bearing knees. However, the lateral release rate was higher with high-flex components (11 of 53 knees, 21%) than with standard components in our study. In five high-flex knees, although patellar tracking was Grade 1, lateral release was performed for tenting of the lateral retinaculum by the overhanging femoral component in full flexion. If these patients are excluded, the lateral release rate was comparable with the rate for standard knees.
Table 6.
Literature review of surgical factors influencing incidence of lateral release
| Study | Type of release | Lateral release rate (number of lateral releases/total patients) | Number of lateral releases (total number of patients) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Approach | Tibial bearing | Navigation | |||||||||
| Midvastus | Medial parapatellar | p value | Mobile | Fixed | p value | Navigated | Nonnavigated | p value | |||
| Engh et al. [8] | Not described | 5.1% (6/118) |
2 (61) (3.3%) |
4 (57) (7%) |
0.258 | ||||||
| Keating et al. [17] | Not described | 15.5% (51/200) |
25 (100) (2.5%) |
26 (100) (2.6%) |
0.871 | ||||||
| Kelly et al. [18] | Not described | 27.5% (14/51) |
1 (22) (4.5%) |
13 (29) (45%) |
< 0.01 | ||||||
| Pagnano et al. [27] | Inside-out | 3.8% (9/240) |
3 (80) (3.75%) |
6 (160) (3.75%) |
* | ||||||
| Yang et al. [37] | Inside-out | 7.9% (104/1318) |
50 (940) (5.3%) |
54 (378) (14.3%) |
< 0.001 | ||||||
| Current study | Outside-in | 10.6% (205/1884) |
24 (451) (5.3%) |
181 (1433) (12.6%) |
< 0.001 | 89 (761) (11.7%) |
116 (1123) (10.4%) |
0.35 | 161 (1423) (11.3%) |
44 (461) (9.5%) |
0.29 |
* No statistical evaluation reported.
The incidences reported by Laskin [21] and Kusuma et al. [19] were higher in valgus than varus knees (Table 7). In our study, the incidence was 16.9% in valgus and 10.7% in varus knees with no statistical difference in rate of releases. Valgus deformity is associated with a tight lateral retinaculum and lateral patellar subluxation. In addition, there is difficulty in achieving proper femoral component rotation in a valgus deformity, which may necessitate lateral release more often.
Table 7.
Literature review of preoperative factors influencing incidence of lateral release
| Study | Type of release | Lateral release rate (number of lateral releases/total patients) | Number of lateral releases (total number of patients) | |||||
|---|---|---|---|---|---|---|---|---|
| Deformity | Sex | |||||||
| Varus | Valgus | p value | Male | Female | p value | |||
| Laskin [21] | Outside-in | 6% (12/178) |
1 (134) (1%) |
11 (24) 46% |
||||
| Ritter et al. [29] | Not described | 35% (428/1205) |
141 (469) (30.1%) |
287 (736) (40%) |
* | |||
| Kusuma et al. [19] | Not described | 28% (314/1108) |
249 (930) (26.7%) |
65 (178) (36.5%) |
0.02 | |||
| Current study | Outside-in | 10.6% (205/1884) |
194 (1819) (10.7%) |
11 (65) (16.9%) |
0.1113 | 12 (388) (3.1%) |
193 (1496) (12.9%) |
< 0.001 |
* No statistical evaluation reported.
Using an outside-in technique for lateral release has the benefit of preserving the synovial covering of the joint, thus providing additional protection. Our surgical technique of outside-in release is simple to perform and has the added advantage of allowing stepwise, titrated release so that minimum necessary slackening of the retinaculum can be done. Such a stepwise release maximized the chances of preservation of the SLGA (155 patients, 75.6%). For 2 to 9 years, the corrected patellar tracking is maintained without compromise to the patellar vascularity. The incidence of anterior knee pain was low (six of 177 patients, 3.4%). Patellofemoral crepitus was detected in 36 of 177 patients (20.3%) but was asymptomatic in 33 patients (19%). This technique could be a useful alternative to the inside-out technique, which disrupts the synovial covering of the joint.
Acknowledgments
We thank Arun Nanivadekar MD MSc, Medical Research Consultant, Lilavati Hospital, Mumbai, India, for assistance with statistical evaluation. We also thank Parul Maniar MS, FRCO, for assistance with editing the manuscript.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Lilavati Hospital, Mumbai, Maharashtra, India.
References
- 1.Bijur PE, Silver W, Gallagher EJ. Reliability of the visual analog scale for measurement of acute pain. Acad Emerg Med. 2001;8:1153–1157. doi: 10.1111/j.1553-2712.2001.tb01132.x. [DOI] [PubMed] [Google Scholar]
- 2.Bindelglass DE, Vince KG. Patellar tilt and subluxation following subvastus and parapatellar approach in total knee arthroplasty: implication for surgical technique. J Arthroplasty. 1996;11:507–511. doi: 10.1016/S0883-5403(96)80101-X. [DOI] [PubMed] [Google Scholar]
- 3.Boyd AD, Jr, Ewald FC, Thomas WH, Poss R, Sledge CB. Long-term complications after total knee arthroplasty with or without resurfacing of the patella. J Bone Joint Surg Am. 1993;75:674–681. doi: 10.2106/00004623-199305000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Brick GW, Scott RD. Blood supply to the patella: significance in total knee arthroplasty. J Arthroplasty. 1989;4(suppl):S75–S79. doi: 10.1016/S0883-5403(89)80011-7. [DOI] [PubMed] [Google Scholar]
- 5.Chan KS, Gill GS. Postoperative patellar tilt in total knee arthroplasty. J Arthroplasty. 1999;14(3):300–304. doi: 10.1016/S0883-5403(99)90055-4. [DOI] [PubMed] [Google Scholar]
- 6.Chia SL, Merican AM, Devadasan B, Strachan RK, Amis AA. Radiographic features predictive of patellar maltracking during total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2009;17:1217–1224. doi: 10.1007/s00167-009-0832-y. [DOI] [PubMed] [Google Scholar]
- 7.Clayton ML, Thirupathi R. Patellar complications after total condylar arthroplasty. Clin Orthop Relat Res. 1982;170:152–155. [PubMed] [Google Scholar]
- 8.Engh GA, Parks NL, Ammeen DJ. Influence of surgical approach on lateral retinacular releases in total knee arthroplasty. Clin Orthop Relat Res. 1996;331:56–63. doi: 10.1097/00003086-199610000-00008. [DOI] [PubMed] [Google Scholar]
- 9.Ewald FC. The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res. 1989;248:9–12. [PubMed] [Google Scholar]
- 10.Grelsamer RP, Bazos AN, Procter CS. Radiographic analysis of patellar tilt. J Bone Joint Surg Br. 1993;75:822–824. doi: 10.1302/0301-620X.75B5.8376449. [DOI] [PubMed] [Google Scholar]
- 11.Healy WL, Iorio R, Warren P. Mesh expansion release of the lateral patellar retinaculum during total knee arthroplasty. J Bone Joint Surg Am. 2003;85:1909–1913. doi: 10.2106/00004623-200310000-00007. [DOI] [PubMed] [Google Scholar]
- 12.Husted H, Toftgaard Jensen T. Influence of the pneumatic tourniquet on patella tracking in total knee arthroplasty: a prospective randomized study in 100 patients. J Arthroplasty. 2005;20:694–697. doi: 10.1016/j.arth.2004.11.016. [DOI] [PubMed] [Google Scholar]
- 13.Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;248:13–14. [PubMed] [Google Scholar]
- 14.Insall JN, Windsor RE, Scott WN, Kelly MA, Aglietti P, editors. Surgery of the Knee. 2. New York, NY: Churchill Livingstone; 1993. [Google Scholar]
- 15.Johnson DP, Eastwood DM. Lateral patellar release in knee arthroplasty: effect on wound healing. J Arthroplasty. 1992;7(suppl):427–431. doi: 10.1016/S0883-5403(07)80035-0. [DOI] [PubMed] [Google Scholar]
- 16.Kayler DE, Lyttle D. Surgical interruption of patellar blood supply by total knee arthroplasty. Clin Orthop Relat Res. 1988;229:221–227. [PubMed] [Google Scholar]
- 17.Keating EM, Faris PM, Meding JB, Ritter MA. Comparison of the midvastus muscle-splitting approach with the median parapatellar approach in total knee arthroplasty. J Arthroplasty. 1999;14:29–32. doi: 10.1016/S0883-5403(99)90198-5. [DOI] [PubMed] [Google Scholar]
- 18.Kelly MJ, Rumi MN, Kothari M, Parentis MA, Bailey KJ, Parrish WM, Pellegrini VD., Jr Comparison of the vastus-splitting and median parapatellar approaches for primary total knee arthroplasty: a prospective, randomized study. J Bone Joint Surg Am. 2006;88:715–720. doi: 10.2106/JBJS.E.00107. [DOI] [PubMed] [Google Scholar]
- 19.Kusuma SK, Puri N, Lotke PA. Lateral retinacular release during primary total knee arthroplasty: effect on outcomes and complications. J Arthroplasty. 2009;24:383–390. doi: 10.1016/j.arth.2007.11.004. [DOI] [PubMed] [Google Scholar]
- 20.Larson CM, Lachiewicz PF. Patellofemoral complications with the Insall-Burstein II posterior-stabilized total knee arthroplasty. J Arthroplasty. 1999;14:288–292. doi: 10.1016/S0883-5403(99)90053-0. [DOI] [PubMed] [Google Scholar]
- 21.Laskin RS. Lateral release rates after total knee arthroplasty. Clin Orthop Relat Res. 2001;392:88–93. doi: 10.1097/00003086-200111000-00011. [DOI] [PubMed] [Google Scholar]
- 22.Laurin CA, Levesque HP, Dussault R, Labelle H, Peides JP. The abnormal lateral patellofemoral angle: a diagnostic roentgenographic sign of recurrent patellar subluxation. J Bone Joint Surg Am. 1978;60:55–60. [PubMed] [Google Scholar]
- 23.Lynch AF, Rorabeck CH, Bourne RB. Extensor mechanism complications following total knee arthroplasty. J Arthroplasty. 1987;2:135–140. doi: 10.1016/S0883-5403(87)80020-7. [DOI] [PubMed] [Google Scholar]
- 24.McMahon MS, Scuderi GR, Glashow JL, Scharf SC, Meltzer LP, Scott WN. Scintigraphic determination of patellar viability after excision of infrapatellar fat pad and/or lateral retinacular release in total knee arthroplasty. Clin Orthop Relat Res. 1990;260:10–16. [PubMed] [Google Scholar]
- 25.Merkow RL, Soudry M, Insall JN. Patellar dislocation following total knee replacement. J Bone Joint Surg Am. 1985;67:1321–1327. [PubMed] [Google Scholar]
- 26.Mochizuki RM, Schurman DJ. Patellar complications following total knee arthroplasty. J Bone Joint Surg Am. 1979;61:879–883. [PubMed] [Google Scholar]
- 27.Pagnano MW, Trousdale RT, Stuart MJ, Hanssen AD, Jacofsky DJ. Rotating platform knees did not improve patellar tracking: a prospective, randomized study of 240 primary total knee arthroplasties. Clin Orthop Relat Res. 2004;428:221–227. doi: 10.1097/01.blo.0000148892.31464.81. [DOI] [PubMed] [Google Scholar]
- 28.Ritter MA, Campbell ED. Postoperative patellar complications with or without lateral release during total knee arthroplasty. Clin Orthop Relat Res. 1987;219:163–168. [PubMed] [Google Scholar]
- 29.Ritter MA, Herbst SA, Keating EM, Faris PM, Meding JB. Patellofemoral complications following total knee arthroplasty: effect of a lateral release and sacrifice of the superior lateral geniculate artery. J Arthroplasty. 1996;11:368–372. doi: 10.1016/S0883-5403(96)80024-6. [DOI] [PubMed] [Google Scholar]
- 30.Scapinelli R. Blood supply of the human patella: its relation to ischaemic necrosis after fracture. J Bone Joint Surg Br. 1967;49:563–570. [PubMed] [Google Scholar]
- 31.Scuderi G, Scharf SC, Meltzer LP, Scott WN. The relationship of lateral releases to patella viability in total knee arthroplasty. J Arthroplasty. 1987;2:209–214. doi: 10.1016/S0883-5403(87)80039-6. [DOI] [PubMed] [Google Scholar]
- 32.Shaw JA. Patellar retinacular peel: an alternative to lateral retinacular release in total knee arthroplasty. Am J Orthop (Belle Mead NJ). 2003;32:189–192. [PubMed] [Google Scholar]
- 33.Smith PN, Parker DA, Gelinas J, Rorabeck CH, Bourne RB. Radiographic changes in the patella following quadriceps turndown for revision total knee arthroplasty. J Arthroplasty. 2004;19:714–719. doi: 10.1016/j.arth.2004.03.007. [DOI] [PubMed] [Google Scholar]
- 34.Strachan RK, Merican AM, Devadasan B, Maheshwari R, Amis AA. A technique of staged lateral release to correct patellar tracking in total knee arthroplasty. J Arthroplasty. 2009;24:735–742. doi: 10.1016/j.arth.2008.02.005. [DOI] [PubMed] [Google Scholar]
- 35.Tria AJ, Jr, Harwood DA, Alicea JA, Cody RP. Patellar fractures in posterior stabilized knee arthroplasties. Clin Orthop Relat Res. 1994;299:131–138. [PubMed] [Google Scholar]
- 36.Wetzner SM, Bezreh JS, Scott RD, Bierbaum BE, Newberg AH. Bone scanning in the assessment of patellar viability following knee replacement. Clin Orthop Relat Res. 1985;199:215–219. [PubMed] [Google Scholar]
- 37.Yang CC, McFadden LA, Dennis DA, Kim RH, Sharma A. Lateral retinacular release rates in mobile- versus fixed-bearing TKA. Clin Orthop Relat Res. 2008;466:2656–2661. doi: 10.1007/s11999-008-0425-y. [DOI] [PMC free article] [PubMed] [Google Scholar]


