Abstract
Background
Osteonecrosis of the femoral head (ONFH) is a debilitating condition affecting primarily young patients. Free vascularized fibular grafting (FVFG) may provide a durable means to preserve the femoral head. When used in the precollapse stages of ONFH, this treatment may alter the course of disease.
Questions/purposes
We asked: (1) In what percentage of patients does FVFG preserve the femoral head beyond 10 years? (2) When long-term preservation is not achieved, what is the duration of femoral head preservation? (3) Do demographic or etiologic factors predict FVFG survivorship? (4) What long-term improvements in function and activity can be anticipated?
Methods
We retrospectively reviewed 61 patients (65 hips) who underwent FVFG for precollapse ONFH. We calculated graft survivorship, SF-12 scores, activity levels, and Harris hip scores. Minimum followup was 10.5 years (mean, 14.4 years; range, 10.5–26 years).
Results Forty-nine of 65 hips (75%) had surviving FVFG for at least 10 years. At last followup, 39 of 65 hips (60%) had surviving FVFG, with a mean graft survival time of 15 years (range, 10.5–26.1 years). Twenty-six of the 65 hips with FVFG (40%) underwent conversion to THA at a mean of 8 years postoperatively. Demographic factors, lesion size, additional procedures, and low preoperative function were not associated with changes in graft survivorship. Pain and function were similar in patients with surviving FVFG and patients who had conversion to THA. Patients with surviving FVFG were more likely to engage in impact sports or active events than were patients who had conversion to THA.
Conclusions
When patients with precollapse ONFH undergo FVFG, the majority have preservation of the hip lasting for greater than 10 years with low levels of pain and reasonable function. In patients who ultimately undergo conversion surgery to THA, the mean duration of hip preservation before conversion is 8 years. We continue to use FVFG for treating patients younger than 50 years with symptomatic, precollapse ONFH.
Level of Evidence
Level IV, therapeutic study. See Instructions to Authors for a complete description of levels of evidence.
Electronic supplementary material
The online version of this article (doi:10.1007/s11999-012-2429-x) contains supplementary material, which is available to authorized users.
Introduction
Osteonecrosis of the femoral head (ONFH) is a potentially disabling condition whose natural history frequently includes collapse of the subchondral bone, progressive pain, degenerative arthrosis, and hip dysfunction [18, 20, 26]. Because ONFH primarily affects young individuals [21, 25], a biologic means of hip preservation is appealing, even if it merely delays endoprosthetic reconstruction of the hip from one decade of life to the next. There are multiple such treatment options directed toward preserving the femoral head and maintaining coxofemoral joint congruity to prevent or delay hip arthrosis [2, 9]. Although technically complex, treatment by free vascularized fibular grafting (FVFG) is reportedly a biologic option for hip preservation that may last 20 years or longer [1, 2, 7, 9, 13, 28]. It generally is accepted this intervention is more likely to result in hip preservation when performed before radiographic collapse of the femoral head [1, 2, 9, 20, 26]. At our institution, when collapse of the subchondral bone has not yet occurred, we use FVFG as a preemptive biologic reconstruction.
There are several deficiencies in the existing literature regarding FVFG treatment of ONFH. First, in reported outcomes after FVFG, precollapse and postcollapse femoral heads have been grouped together when plotting graft survival and identifying risk factors for failure [19, 22–26, 28]. Stage, size, and etiology have been identified as factors influencing the likelihood of hip preservation after FVFG [16, 22, 28], but it is not known whether these hold true in the specific subset of patients treated before bony collapse. Second, definitions of success and failure have been variable. Some studies [17, 21, 23] have described outcomes based on radiographic rather than functional assessments. Failure often is defined as conversion to THA, yet preservation of the femoral head from the fourth decade into the fifth decade of life may constitute a therapeutic success. Third, most studies describe short- (1–4 years) [17] or medium-term (4–7 years) [3, 15, 17, 22, 24, 25] findings. Two long-term studies (ie, > 10 years) [13, 28] did not focus specifically on patients with ONFH who undergo FVFG before the onset of subchondral bony collapse.
We therefore sought to define more clearly the long-term fate of FVFG in patients treated for ONFH before the onset of bony collapse. We asked the following questions: (1) In what percentage of patients does FVFG preserve the precollapse femoral head beyond 10 years? (2) When long-term preservation of the femoral head is not achieved, what is the duration of femoral head preservation? (3) What demographic or etiologic factors predict FVFG survivorship? (4) What long-term improvements in function and activity can be anticipated with this procedure?
Patients and Methods
We retrospectively reviewed our FVFG database for 1979 to 1997 and identified 642 patients who underwent 672 FVFGs for ONFH. During the study time, the indications for FVFG were (1) symptomatic ONFH, (2) age 50 years or younger, and (3) presence of an intact fibula in a well-perfused leg. The contraindications were (1) age older than 50 years, (2) hip arthrosis, and (3) bilateral lower-extremity vasculopathy based on either symptomatic claudication or absence of distal pulses. Prerequisites for inclusion in this analysis were (1) a minimum followup of 10 years postoperatively and (2) a FVFG performed before the onset of subchondral bony collapse of the femoral head, as visible on either plain radiographs or MRI (Fig. 1). All preoperative images (plain radiographs and MRI, after the availability of MR technology) were examined by one reviewer (JRU) at a weekly conference dedicated to screening candidates for FVFG. To identify radiographic collapse we used the classification system of Ficat and Arlet [9] and recorded the classification in a prospectively maintained database. Of the 672 patients undergoing FVFG, 591 had hips classified as having radiographic collapse of the femoral head. This left 81 hips (76 patients) treated with FVFG before the onset of femoral head collapse. Of these, 15 patients (16 hips) either died (nine patients, 10 hips) or were lost to followup (six patients, six hips). This left 61 patients (80%) and 65 hips (80%) available for review. There were 43 males and 18 females with a mean age at surgery of 32.1 years (range, 12–40 years). The most common etiologies of osteonecrosis were steroid-induced (n = 27), idiopathic (n = 20), posttraumatic (n = 10), and alcoholic (n = 5). According to the classification of Ficat and Arlet [9], five hips had a Stage I lesion and 60 had a Stage II lesion. When cross-sectional imaging was available, lesion volume was assessed as a percentage of femoral head volume and classified as less than 25%, 25% to 50%, or greater than 50%. The lesion volume was less than 25% in 26 hips, 25% to 50% in 15 hips, and greater than 50% in eight hips. In 16 hips, treatment was initiated before the availability of MR technology and no size assessment could be made. The minimum followup was 10.5 years (mean, 14.4 years; range, 10.5–26.1 years). No patients were recalled specifically for this study; all data were obtained from medical records. We had prior approval from the Duke University Institutional Review Board (IRB Number Pro00001803).
Fig. 1A–B.
(A) AP and (B) lateral radiographic views show the right hip in a patient with Ficat Stage II ONFH.
All procedures were performed by one of four surgeons (MJR, DSR, JMA, JRU), each of whom performed the procedure in a similar fashion. A technique previously described in detail [1] was used for all procedures. Several technical modifications have been made during the years and were used in our study. Harvesting local bone graft from the lesser trochanter was avoided as we believed this contributed to subtrochanteric fracture. An additional reamer size (17.5 mm) was added to the instrument set. The hip was prepared simultaneously during the fibular harvest. Venous couplers were used for venous anastomosis instead of a hand-sewn technique.
A bulky soft dressing was applied to the fibular harvest site. The leg then was placed into an air boot (Foot WAFFLE®; EHOB, Indianapolis, IN, USA) to prevent excessive pressure on the heel. The hip wound was covered with dressing sponges and Tegaderm™ (3M, St Paul, MN, USA). An epidural catheter was the primary means of postoperative analgesia. Physical therapy began on the first postoperative day. Patients typically were discharged home on the third postoperative day. The first followup occurred in the sixth postoperative week. During the first 6 weeks postoperatively, patients remained nonweightbearing on crutches on the operative side and performed daily strengthening and ROM exercises of the hip, knee, and ankle. For patients undergoing bilateral treatment, procedures were performed in staged fashion, with the second side being performed at least 6 weeks after the first side.
One of the four operating surgeons performed clinical evaluation at each postoperative visit. Scheduled postoperative visits typically occurred at 3, 6, 12, 18, and 24 months. In 49 patients, the considerable distance of travel necessitated portions of the followup evaluation being completed by a local orthopaedic surgeon. In these instances, a followup form was provided to the orthopaedic surgeon conducting the followup. This form and radiographs were forwarded to Duke University for review by one of the authors. Function was assessed preoperatively and postoperatively using the modified Harris hip score (HHS) [5]. Because patients were not routinely scheduled for regular followup beyond 10 years, a protocol was developed for late (> 10 years postoperatively) reassessment of patients. Patient contact information was obtained via the Duke FVFG database. When unavailable or inaccurate, contact information was sought via a variety of internet search engines, including a contracted person finder. Despite these efforts, six of the 76 patients (six of 81 hips) could not be reached by any method. All patients initially were sent a packet via standard mail at the onset of the late data collection period for this study (May 2008). This packet contained an informed consent document, a research summary, a question regarding survivorship, a question regarding overall activity levels, and the questions used to calculate the SF-12 physical component summary (PCS) and mental component summary (MCS) [27] and modified HHS (Appendix 1; Supplemental materials are available with the online version of CORR). All information was retrieved on each of the hips analyzed.
Graft survival was calculated via the Kaplan-Meier method using conversion to THA as an end point. For patients who did not have long-term (> 10 years) hip preservation, the mean duration of graft survival was calculated. To determine which variables predicted conversion to THA, we evaluated etiologic factors (etiology, stage, size), demographic factors (age, race, sex), and potential confounding factors (preoperative HHS, need for additional procedures, bilaterality) using univariate and multivariate Cox regression. The log-rank statistic was used to assess difference in survival among etiologies (idiopathic, steroids, trauma) regarding ultimate conversion to THA. We assessed long-term function and activity level via the HHS, SF-12, and an activity questionnaire (Appendix 1; Supplemental materials are available with the online version of CORR.) and reported them descriptively for patients with surviving grafts and those who underwent conversion to THA. All analyses were performed using SPSS® (Version 12.0; SPSS Inc, Chicago, IL, USA).
Results
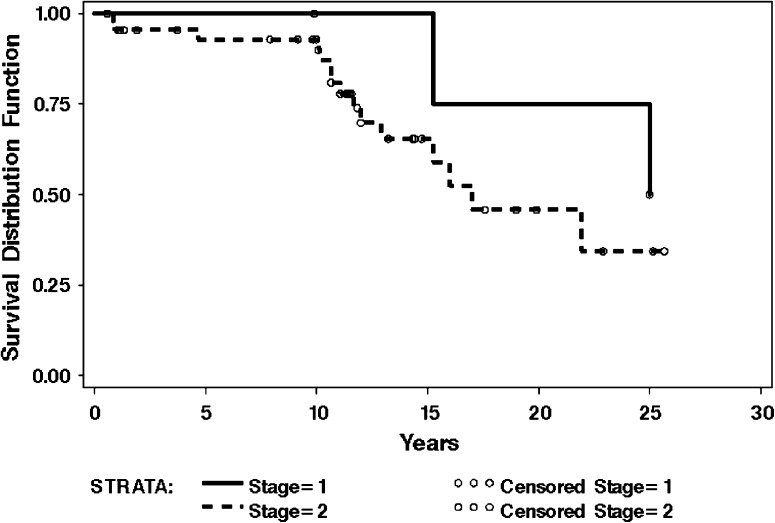
Of the 65 hips available for complete followup, 39 (60%) had surviving FVFG for the duration of followup, with a mean graft survival of 14.9 years (range, 10.5–26.1 years) (Fig. 2). Forty-nine of 65 hips (75%) had surviving FVFG at ten years postoperatively (Fig. 2).
Fig. 2.
The Kaplan-Meier survivorship curves show clinical failure (defined as conversion to THA) of FVFG for treatment of ONFH. Censored observations (the observations of each hip at the end of the study) are denoted by vertical lines. The error bars show the 95% CIs. The most common underlying etiologies (idiopathic, steroid-induced, trauma) show 60% of all hips survived 10 years or longer. Of the 40% of hips in which long-term preservation failed (≥ 10 years survival), the mean survival was 8.3 years.
Of the 26 hips (40%) that did not succeed in long-term (≥ 10 years) hip preservation, the duration of hip preservation was 8.3 years (range, 7 months to 17 years) after FVFG. After failure, all 26 hips were converted to THA (Fig. 2).
We found no association (p = 0.84) between conversion to THA and stage of disease, with two of five (40%) patients with Stage I disease and 24 of 60 (40%) with Stage II disease undergoing conversion surgery to THA (Table 1). A lower survival rate (p = 0.022) was associated with an idiopathic etiology of hip osteonecrosis when compared with other underlying etiologies (Table 1). We observed no association between lesion size (p = 0.12), anatomic side (p = 0.19), gender (p = 0.22), and conversion to THA (Table 1).
Table 1.
Comparison of hips converted to THA
| Variable | Number of hips | Conversion to THA (%) | p value* |
|---|---|---|---|
| Ficat stage | 0.182 | ||
| I | 5 | 2 (40%) | |
| II | 60 | 24 (40%) | |
| Total | 65 | 26 (40%) | |
| Etiology | |||
| Steroid-induced | 27 | 8 (30%) | 0.069 |
| Idiopathic | 20 | 12 (60%) | 0.022 |
| Posttraumatic | 10 | 3 (30%) | 0.731 |
| Alcoholic | 5 | 3 (60%) | 0.132 |
| Pregnancy-associated | 2 | 0 (0%) | 0.362 |
| Perthes-associated | 1 | 0 (0%) | 0.161 |
| Lesion size | |||
| < 25% | 26 | 10 (38%) | 0.124 |
| 25–50% | 15 | 6 (40%) | 0.129 |
| > 50% | 8 | 3 (38%) | 0.146 |
| Unclassified | 16 | 7 (44%) | 0.076 |
| Side | 0.19 | ||
| Right | 15 | 4 (27%) | |
| Left | 50 | 22 (44%) | |
| Gender† | 0.22 | ||
| Male | 43 | 20 (46%) | |
| Female | 18 | 6 (33%) |
Bold value indicate the significant p value.
* p ≤ 0.05 was considered significant; †gender reported as number of patients.
Preoperative HHSs were not different (p = 0.10) between patients who ultimately had conversion to THA (mean, 65.7) and patients whose FVFG was surviving at last followup (mean, 66.4) (Table 2). In hips with surviving FVFG at last followup, the mean preoperative HHS improved from 66.4 to 88.6 (range, 45.1–100), a mean improvement of 22.2 (Table 2). In hips converted to THA, the mean preoperative HHS improved from 65.7 to 89.1, a mean improvement of 23.4 (Table 2). There was no difference in either mean improvement of HHS (p = 0.30) or last HHS (p = 0.43) between hips with surviving FVFG and hips converted to THA (Table 2). There were no differences in any of the components of the HHS between hips with surviving FVFG and hips converted to THA. At last followup, higher SF-12 Mental Component Summary scores (p = 0.018) were observed for patients with surviving FVFG (mean, 54) than for patients who had undergone THA (mean, 50) (Table 2). There was no difference in SF-12 Physical Component Summary scores between patients with surviving FVFG and patients who had undergone THA (Table 2). Patients with surviving FVFG were more likely (p = 0.04) to engage in activity at a level including either impact sports (such as jogging, tennis, skiing, and ballet) or active events (such as bicycling, golf, and bowling) than patients whose FVFG was converted THA (Fig. 3). Fifty-four percent of patients with surviving FVFG regularly or occasionally participated in impact sports compared with 23% of patients with THA (Fig. 3). Patients whose FVFG was converted to THA were more likely (p = 0.04) to engage only in either mild activities (such as walking, limited housework, and limited shopping) or moderate activities (such as swimming, unlimited housework, and unlimited shopping) than patients with a surviving FVFG (Fig. 3). Forty-six percent of patients with THAs participated only in mild or moderate activities compared with 31% of patients with surviving FVFG (Fig. 3).
Table 2.
Comparison of Harris hip and SF-12 scores
| Variable | Statistic | THA (n = 26) | Surviving FVFG (n = 39) | Difference | p value* |
|---|---|---|---|---|---|
| Preoperative Harris hip score | Mean (SD) | 66 (19.5) | 66 (16.5) | 0 | 0.102 |
| Postoperative Harris hip score | Mean (SD) | 89 (28) | 89 (15) | 0 | 0.432 |
| Change in Harris hip score | Mean (SD) | +23 (19) | +23 (18) | 0 | 0.302 |
| SF-12 Physical Component Summary | Mean (SD) | 47 (9.4) | 49 (9.6) | 2 | 0.521 |
| SF-12 Mental Component Summary | Mean (SD) | 50 (7.7) | 54 (4.35) | 4 | 0.018 |
The p value less than or equal to 0.05 should be in bold.
* p value based test of mean difference equal to zero in model using generalized estimating equations to account for the correlation of multiple observations from the same subject; THA = total hip arthroplasty; FVFG = free vascularized fibular graft.
Fig. 3A–B.
The pie charts show activity levels among (A) patients with surviving FVFG and (B) patients whose FVFG was converted to THA. Patients with surviving FVFG were more likely (p = 0.04) to participate in active events or impact sports. Patients who underwent conversion to THA were more likely (p = 0.04) to participate only in mild activities (such as walking, limited housework, and limited shopping) or moderate activities (such as swimming, unlimited housework, and unlimited shopping).
We recorded numerous complications, most of which either were treated and resolved or did not remain symptomatic. However, four patients had persistent symptoms related to complications: one symptomatic flexor hallucis longus contracture, one symptomatic ankle pain, one symptomatic heterotopic ossification, and one recurrent trochanteric bursitis (Table 3).
Table 3.
Summary of donor site and graft site complications.
| Complication | Number symptomatic at early followup (percentage) | Number symptomatic at final followup (percentage) |
|---|---|---|
| Donor site (leg) | ||
| Great toe flexion contracture | 3 (4.6%) | 1 (1.5%) |
| Ankle pain or tenderness | 3 (4.6%) | 1 (1.5%) |
| Altered sensation | 1 (1.5%) | 0 (0%) |
| Superficial infection | 2 (3%) | 0 (0%) |
| Deep infection | 1 (1.5%) | 0 (0%) |
| Graft site (hip) | ||
| Pin migration | 5 (7.7%) | 0 (0%) |
| Heterotopic ossification | 3 (4.6%) | 1 (1.5%) |
| Femoral fracture | 3 (4.6%) | 0 (0%) |
| Superficial infection | 1 (1.5%) | 0 (0%) |
| Deep infection | 0 (0%) | 0 (0%) |
| Trochanteric bursitis | 2 (3%) | 1 (1.5%) |
Discussion
In the search for a definitive biologic treatment for ONFH, various studies have described variable results after FVFG [3, 6–9, 11, 15–17, 21, 23, 25]. The literature lacks long-term reports (there are two with 10-year followup or longer [13, 28]) and specific focus on patients treated with FVFG before the onset of femoral head collapse. We sought to better define the typical long-term results after FVFG specifically in patients with precollapse ONFH. In so doing, we sought to answer four specific questions: (1) In what percentage of patients does FVFG preserve the precollapse femoral head beyond 10 years? (2) When long-term preservation of the femoral head is not achieved, what is the duration of femoral head preservation? (3) What demographic or etiologic factors predict FVFG survivorship? (4) What long-term improvements in function and activity can be anticipated with this procedure?
Limitations of our study must be addressed. First, FVFG is the preferred treatment at our institution for symptomatic, early-stage ONFH in patients younger than 50 years. Our referral population includes few patients with small Ficat Stage I lesions and we do not intend to imply that we would recommend FVFG broadly for such patients. As such, our study lacks a control group treated with either nonoperative treatment, an alternative femoral head-preserving procedure, or arthroplasty. Second, we lacked long-term radiographic analysis, owing to the lack of consistent availability of high-quality radiographs. As the focus of our study was functional outcomes and functional outcomes do not correlate with specific radiographic parameters [25, 26], we believe radiographic analysis does not substantially contribute to our findings. Twenty percent of hips in our series were not available for complete followup. Although the majority of patients lost to followup (nine of 15 patients) were not available because of death unrelated to the procedure, it is possible that nonresponders are substantially different from responders. This leaves the potential for different outcomes and conclusions, had these additional patients been available for review. Finally, a large number of FVFG are performed at our institution annually and there are specialized surgical, nursing, and perioperative support teams. This procedure is technically complex and our results may not be applicable if performed in a less highly specialized setting.
Reported rates of overall FVFG survivorship range from 61% to 96% [3, 6, 7, 9, 11, 15–17, 23]. With one exception [28], studies showing survivorship in excess of 75% have followups of 5 years or less [3, 6, 7, 9, 11, 15–17, 23]. The survivorship of 60% in our study likely reflects the long followup period and relative frequency of patients with idiopathic ONFH (in whom we have identified a higher rate of late disease progression). Because FVFG is a relatively complex operation, it is important to consider rates and duration of long-term hip preservation after technically simpler interventions. Fairbank et al. [8] reported an 88% rate of salvage in Ficat Stage I hips and a 72% rate of salvage in Ficat Stage II hips treated by core decompression. Bozic et al. [4] reported a 44% rate of salvage among all precollapse hips treated by core decompression at a mean followup of 10 years. Half of the failures in the study by Bozic et al. occurred in patients with cystic changes in the femoral head, suggesting that core decompression alone is not ideal for these patients [4]. Another technically simpler operation to consider is treatment of ONFH with a nonvascularized cortical graft. Our results compare favorably with results of this technique where survivorship has been reported to be 59% at 5 years [14]. Plakseychuk et al. [22] have published the only direct comparison of vascularized versus nonvascularized fibular grafting of ONFH. In their study, the FVFG survival rate was 86% at 7 years compared with 30% at 7 years for the nonvascularized fibular grafts. We compared our results with those in the literature (Table 4), although only one other study, that of Yoo et al. [28], exclusively evaluated precollapse femoral heads.
Table 4.
Comparison of results in the current study with those reported in the literature.
| Study | Number of hips | Mean patient age (years) | Mean followup (years) | Graft survival at final followup (%) | Mean final Harris hip score* | Factors associated with failure (other than advanced stage) |
|---|---|---|---|---|---|---|
| Berend et al. [3] | 121 | 34 | 4.3 | 64.5 | 81 | Idiopathic, alcoholic, and posttraumatic etiologies |
| Judet and Gilbert [13] | 68 | NR | 18 | 73.5 | 52% > 80* | Age > 40 years |
| Louie et al. [15] | 59 | 34 | 4.2 | 73 | 83.6 | Age > 40 years |
| Malizos et al. [17] | 40 | NR | 2.7 | 92.5 | 88% > 80* | Large lesion size |
| Marciniak et al. [19] | 101 | 37 | 5 | 61 | 80 | No significant associations |
| Plakseychuk et al. [22] | 50 | 44 | 5 | 86 | 78 | No significant associations |
| Soucacos et al. [24] | 184 | NR | 4.7 | 92.4 | 88.1 | No significant associations |
| Urbaniak et al. [25] | 103 | 34 | 7 | 70 | 80 | Age > 30 years |
| Yoo et al. [28] | 124 | 35.5 | 13.9 | 89.6 | 88 | Age > 35 years |
| Current study | 65 | 32 | 14.4 | 60 | 89 | Idiopathic etiology |
* Mean Harris hip score of patients with surviving FVFG at final followup. In some instances, the Harris hip score was reported as a percentage deemed good or excellent (ie, > 80); NR = not reported.
Perhaps the more important question regarding graft survivorship concerns the duration of femoral head preservation when it does not meet the accepted definition of long term (10 years). With a mean patient age of 32.1 years at the time of surgery and a mean graft survival of 8.3 years, the average patient for whom long-term femoral head preservation failed would still experience a substantial extension of the life of the femoral head and hip (from the fourth decade of life to the fifth decade of life). This benefit is in contrast to nonoperative treatment, wherein rates of femoral head preservation are low and progression to collapse is rapid [18, 26]. This duration of preservation among patients with failed femoral head preservation compares favorably with results seen after core decompression. In Ficat Stage I hips, Fairbank et al. reported a mean 9.8 years to failure after core decompression but for Ficat Stage II hips the mean time to failure was 4.8 years [8]. Bozic et al. did not report mean survival times but most failures occurred within the first 6 years postoperatively [4]. Advanced stage of disease is consistently associated with poorer outcomes [3, 13, 15, 17, 19, 22, 24, 25, 28]. Independent of stage, various other factors have been associated with failure but have not been replicated consistently across different studies [3, 13, 15, 17, 19, 22, 24, 25, 28]. In our study, patients with idiopathic ONFH experienced a progressive decline in survivorship, even beyond the 10-year mark. Yoo et al. [28], and a prior study at our institution [25] found no association between etiology and graft survival. We speculate that idiopathic cases of ONFH may be attributable to a progressive underlying disorder such as intraosseous hypertension, which could result in late changes to the femoral head despite treatment with a vascularized bone graft. Some authors have reported patient age at the time of surgery predicts graft survival [4, 7, 25, 28]. Yoo et al. [28] and Judet and Gilbert [13] reported graft survival is more likely in patients younger than 35 and 40 years, respectively. Other authors [4, 7, 25] have refuted this in medium-term followup. We found no association between age and either graft survival or functional outcomes. This may be because our study included only hips with precollapse ONFH. Failure to control for this may result in an apparent age effect, as rates of collapse increase with patient age [26]. In general, HHSs reported in the literature after FVFG and THA are frequently in excess of 80 and our mean HHS of 88.6 compares favorably [3, 4, 13–15, 17, 19, 22, 24, 25, 28]. Long-term HHSs are not well described for nonoperative management, core decompression, or nonvascularized fibular grafting. Our patients with successful femoral head preservation also were likely to participate in impact sports and active events. This query of specific activities after treatment of ONFH has not been reported previously for patients undergoing FVFG, core decompression, or nonoperative treatment. Whether patients with surviving FVFG actually had a superior capacity for such activities is not clear. It is possible patients in whom hip preservation failed either chose or were instructed not to participate in such activities to protect their arthroplasties. Johansson et al. [12] reported that a lower preoperative HHS correlates with greater postoperative pain and poorer postoperative function. We found lower preoperative HHS did not predict either conversion to THA or poorer postoperative function. Complications, mostly transient, were consistent with those previously described [10] and did not generally affect functional outcomes.
We conclude that more than half of patients with precollapse ONFH treated with FVFG can expect long-term preservation of the hip. Patients can expect levels of hip function comparable to that of THA and with a greater likelihood of participating in high-demand or impact sports. Patients for whom long-term preservation ultimately failed had a mean time to failure of 8 years. At our institution, where this technically demanding procedure is performed routinely, we regard FVFG as the treatment of choice for patients younger than 50 years with symptomatic, precollapse ONFH, especially for individuals who wish to maintain a high level of athletic activity.
Electronic supplementary material
Acknowledgments
We thank Mack Aldridge (JMA) MD for his dedicated care given to many of the patients included in this analysis, to Sandra Stinnett for statistical analysis of data, and to Jennifer Friend for her invaluable contributions to data collection and review.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Duke University Medical Center, Durham, NC, USA.
References
- 1.Aldridge JM, 3rd, Berend KR, Gunneson EE, Urbaniak JR. Free vascularized fibular grafting for the treatment of postcollapse osteonecrosis of the femoral head: surgical technique. J Bone Joint Surg Am. 2004;86(suppl 1):87–101. doi: 10.2106/00004623-200403001-00012. [DOI] [PubMed] [Google Scholar]
- 2.Aldridge JM, 3rd, Urbaniak JR. Avascular necrosis of the femoral head: role of vascularized bone grafts. Orthop Clin N Am. 2007;38:13–22. doi: 10.1016/j.ocl.2006.10.012. [DOI] [PubMed] [Google Scholar]
- 3.Berend KR, Gunneson EE, Urbaniak JR. Free vascularized fibular grafting for the treatment of postcollapse osteonecrosis of the femoral head. J Bone Joint Surg Am. 2003;85:987–993. doi: 10.2106/00004623-200306000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Bozic KJ, Zurakowski D, Thornhill TS. Survivorship analysis of hips treated with core decompression for nontraumatic osteonecrosis of the femoral head. J Bone Joint Surg Am. 1999;81:200–209. doi: 10.2106/00004623-199902000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Byrd TJ, Jones KS. Prospective analysis of hip arthroscopy with 2-year follow-up. Arthroscopy. 2000;16:578–587. doi: 10.1053/jars.2000.7683. [DOI] [PubMed] [Google Scholar]
- 6.Chillag KJ. Survival analysis of hips treated with core decompression or vascularized fibular grafting because of avascular necrosis. J Bone Joint Surg Am. 2000;82:289–290. [PubMed] [Google Scholar]
- 7.Cho BC, Kim SY, Lee JH, Ramasastry SS, Weinzweig N, Baik BS. Treatment of osteonecrosis of the femoral head with free vascularized fibular transfer. Ann Plast Surg. 1998;40:586–593. doi: 10.1097/00000637-199806000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Fairbank AC, Bhatia D, Jinnah RH, Hungerford DS. Long-term results of core decompression for ischaemic necrosis of the femoral head. J Bone Joint Surg Br. 1995;77:42–49. [PubMed] [Google Scholar]
- 9.Ficat RP, Arlet J. Functional investigation of bone under normal conditions. In: Hungerford DS, editor. Ischemia and Necrosis of Bone. Baltimore, MD: Williams and Wilkins; 1980. pp. 29–52. [Google Scholar]
- 10.Gaskill TR, Urbaniak JR, Aldridge JM., 3rd Free vascularized fibular transfer for femoral head osteonecrosis: donor and graft site morbidity. J Bone Joint Surg Am. 2009;91:1861–1867. doi: 10.2106/JBJS.H.01105. [DOI] [PubMed] [Google Scholar]
- 11.Goodman SB. Survival analysis of hips treated with core decompression or vascularized fibular grafting because of avascular necrosis. Comment on: J Bone Joint Surg Am. 1998;80:1270–1275. J Bone Joint Surg Am. 2000;82:289. [PubMed] [Google Scholar]
- 12.Johansson HR, Bergschmidt P, Skripitz R, Finze S, Bader R, Mittelmeier W. Impact of preoperative function on early postoperative outcome after total hip arthroplasty. J Orthop Surg (Hong Kong). 2010;18:6–10. doi: 10.1177/230949901001800102. [DOI] [PubMed] [Google Scholar]
- 13.Judet H, Gilbert A. Long-term results of free vascularized fibular grafting for femoral head necrosis. Clin Orthop Relat Res. 2001;386:114–119. doi: 10.1097/00003086-200105000-00015. [DOI] [PubMed] [Google Scholar]
- 14.Keizer SB, Kock NB, Dijkstra PD, Taminiau AH, Nelissen RG. Treatment of avascular necrosis of the hip by a non-vascularised cortical graft. J Bone Joint Surg Br. 2006;88:460–466. doi: 10.1302/0301-620X.88B4.16950. [DOI] [PubMed] [Google Scholar]
- 15.Louie BE, McKee MD, Richards RR, Mahoney JL, Waddell JP, Beaton DE, Schemitsch EH, Yoo DJ. Treatment of osteonecrosis of the femoral head by free vascularized fibular grafting: an analysis of surgical outcome and patient health status. Can J Surg. 1999;42:274–283. [PMC free article] [PubMed] [Google Scholar]
- 16.Malizos KN, Quarles LD, Dailiana ZH, Rizk WS, Seaber AV, Urbaniak JR. Analysis of failures after vascularized fibular grafting in femoral head necrosis. Orthop Clin North Am. 2004;35:305–314. doi: 10.1016/j.ocl.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 17.Malizos KN, Soucacos PN, Beris AE. Osteonecrosis of the femoral head: hip salvaging with implantation of a vascularized fibular graft. Clin Orthop Relat Res. 1995;314:67–75. [PubMed] [Google Scholar]
- 18.Mankin HJ. Nontraumatic necrosis of bone (osteonecrosis) N Engl J Med. 1992;326:1473–1479. doi: 10.1056/NEJM199205283262206. [DOI] [PubMed] [Google Scholar]
- 19.Marciniak D, Furey C, Shaffer JW. Osteonecrosis of the femoral head: a study of 101 hips treated with vascularized fibular grafting. J Bone Joint Surg Am. 2005;87:742–747. doi: 10.2106/JBJS.D.02004. [DOI] [PubMed] [Google Scholar]
- 20.Merle D’Aubigné R, Postel M, Mazabraud A, Mazabraud A, Massias P, Gueguen J, France P. Idiopathic necrosis of the femoral head in adults. J Bone Joint Surg Br. 1965;47:612–633. [PubMed] [Google Scholar]
- 21.Mont MA, Jones LC, Hungerford DS. Survival analysis of hips treated with core decompression or vascularized fibular grafting because of avascular necrosis. J Bone Joint Surg Am. 2000;82:290–291. doi: 10.1302/0301-620X.82B2 .9819. [DOI] [PubMed] [Google Scholar]
- 22.Plakseychuk AY, Kim SY, Park BC, Varitimidis SE, Rubash HE, Sotereanos DG. Vascularized compared with nonvascularized fibular grafting for the treatment of osteonecrosis of the femoral head. J Bone Joint Surg Am. 2003;85:589–596. doi: 10.2106/00004623-200304000-00001. [DOI] [PubMed] [Google Scholar]
- 23.Scully SP, Aaron RK, Urbaniak JR. Survival analysis of hips treated with core decompression or vascularized fibular grafting because of avascular necrosis. J Bone Joint Surg Am. 1998;80:1270–1275. doi: 10.2106/00004623-199809000-00004. [DOI] [PubMed] [Google Scholar]
- 24.Soucacos PN, Beris AE, Malizos K, Koropilias A, Zalavras H, Dailiana Z. Treatment of avascular necrosis of the femoral head with vascularized fibular transplant. Clin Orthop Relat Res. 2001;386:120–130. doi: 10.1097/00003086-200105000-00016. [DOI] [PubMed] [Google Scholar]
- 25.Urbaniak JR, Coogan PG, Gunneson EB, Nunley JA. Treatment of osteonecrosis of the femoral head with free vascularized fibular grafting: a long-term follow-up study of one hundred and three hips. J Bone Joint Surg Am. 1995;77:681–694. doi: 10.2106/00004623-199505000-00004. [DOI] [PubMed] [Google Scholar]
- 26.Vail TP, Covington DB. The incidence of osteonecrosis. In: Urbaniak JR, Paul JP, editors. Osteonecrosis: Etiology, Diagnosis, and Treatment. Rosemont, IL: American Academy of Orthopaedic Surgeons; 1997. pp. 43–49. [Google Scholar]
- 27.Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 28.Yoo M, Kim K, Hahn C, Parvizi J. Long-term followup of vascularized fibular grafting for femoral head necrosis. Clin Orthop Relat Res. 2008;466:1133–1140. doi: 10.1007/s11999-008-0204-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.