Abstract
An asthma education program for older school-age students with asthma was developed in collaboration with school personnel, health care professionals, and community partners. Feasibility and benefits were evaluated using a single-group, prospective, quasi-experimental design. The convenience sample, consisting of 28 grade 6 and 7 students with asthma, had 50% males, a diverse racial background, and a wide range of incomes. Feasibility and benefits were demonstrated by comparing pre-intervention to 1- and 12-month post-intervention evaluation of students who completed more than 70% of the 10 sessions. Statistically significant improvement sin cognitive, behavioral, psychosocial, and quality of life outcomes were seen from pre-intervention to 1-month post-intervention (all p < .03). Severity of asthma significantly improved from 1- to 12- month post-intervention (p = .04).
Keywords: Health Education, Self-care Behavior, Health Counseling, Intervention Research
Asthma prevalence in the US was estimated at 8.2% in 2009, with 24.6 million people diagnosed with the condition (Akinbami, Moorman, & Liu, 2011). Over 7 million children younger than age 18 years are diagnosed with asthma, and approximately 4 million children experience acute asthma symptoms annually. Children aged 9–14 years, hereafter referred to as students, experience higher morbidity and mortality than other age groups across the life span (Akinbami, 2007). Students with asthma are limited in engaging in life activities (e.g., Hallstrand, Curtis, Aitken, & Sullivan, 2003; Riccionietal., 2003; Strunk, Sternberg, Bacharier, & Szefler, 2002), more likely than their classmates to miss school, and often taken to the emergency room for acute exacerbation of symptoms (Akinbami et al., 2011).
Successful asthma management plans include offering health education to students with the condition. The National Guidelines for the Diagnosis and Management of Asthma (National Institutes of Health [NIH], 2007) recommended delivering education programs to students and their family caregivers in community settings including schools. Education programs for families of children with asthma have been evaluated with mixed results. Although most researchers have reported increases in knowledge (e.g., Horner & Fouladi, 2008; Magzamen, Patel, Davis, Edelstein, & Tager, 2008; Velsor-Friedrich, Pigott, & Srof, 2005), few have reported significant long-term changes in behavior or decreased morbidity (Clark et al., 2004). This lack of behavior change may be because programs rarely considered students’ cognitive, psychosocial, and behavioral needs from a developmental perspective (Kieckhefer & Trahms, 2000; Kjellman & Gustafsson, 2000; Rasmussen et al., 2002). In addition, schools have been resistant to accept non-academic asthma health education programs in the age of “No Child Left Behind” (U.S. Department of Education, 2002). Age- and grade-appropriate school-based programs are needed that can be integrated into schools’ curricula in ways that are more likely to be accepted by administrators and board members seeking to demonstrate academic outcomes. Community-based asthma awareness and education programs are also needed to address the social factors that impact asthma management in older school-age students living with the condition.
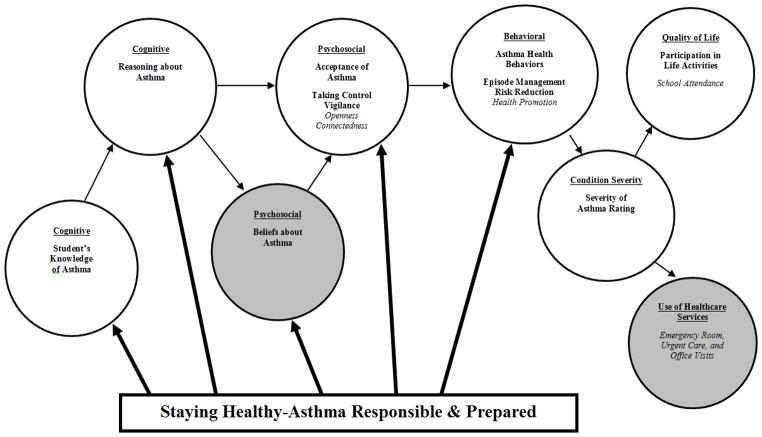
“Staying Healthy–Asthma Responsible & Prepared™”(SHARP) was designed to meet these needs (Kintner & Sikorskii, 2009) by addressing the cognitive, behavioral, and psychosocial factors that can affect asthma severity and quality of life outcomes. School personnel and asthma coalition members collaborated in the development of SHARP’s School and Community Components.
School personnel consisted of administrators, principals, office staff, and teachers who were instrumental in delivering the School Component during instructional time. Asthma coalition members consisted of dedicated and diverse individuals (i.e., pharmacists, nurses, respiratory therapists, physicians, pharmaceutical representatives, and representatives of the American Lung Association) who represented the area health/hospital system, county health department, pharmacists’ association, community college respiratory care program, tobacco reduction group, meditation center, and local restaurants. Coalition members shared the common goal of providing asthma education to improve the health status of people with asthma. These individuals were instrumental in supporting and organizing the Community Component, which was designed as an information-sharing asthma health fair.
The aims of this preliminary, pilot study included evaluating the (a) feasibility of SHARP for older school-age students, their family caregivers, school personnel, and community partners; and (b) benefits to students’ cognitive, psychosocial, behavioral, asthma severity, and quality of life outcomes. Feasibility was evaluated as (a) willingness of students and caregivers to fully participate in the intervention and complete the evaluation instruments, (b) abilities of the interveners to deliver each session of the program and tail or the program to address students’ individual needs, and (c) perceptions of program and study content, format, and complexity for students, school personnel, community partners, and team members. Benefits of the program were evaluated using the following student outcomes: asthma knowledge, logical reasoning abilities for managing symptoms, acceptance of asthma as a chronic condition, and use of effective episode management and risk reduction asthma health behaviors that influence asthma severity, and participation in life activities as a measure of quality of life.
Theoretical Framework
The Acceptance of Asthma Model (Kintner, 1996, 1997, 2004, 2007) and a lifespan development perspective (e.g., Lerner, 1986; Santrock, 2010; Sugarman, 1986) guided development of the theory-driven, evidence-based SHARP program (Kintner & Sikorskii, 2009). SHARP is an age- and grade-appropriate academic and counseling asthma health education program for school-age students (aged 9–14 years) with asthma who are preparing to transition from parental dependence in elementary school to taking more personal responsibility form an aging their condition in middle or junior high schooling rades 6 or 7. Following students as they transition is the focus of this research program (Kintner & Sikorskii, 2009). Figure 1 depicts integration of SHARP into the Acceptance of Asthma Model.
Figure 1.
Depiction of how SHARP integrates into the Acceptance of Asthma Model. Factors highlighted in grey and indicators typed in italics were not evaluated as part of this study.
Method
Design and Sample
A single-group, longitudinal, prospective, quasi-experimental design was used for this preliminary, pilot study. Protection of human subjects approval was obtained through the university institutional review board. The study was in compliance with the Health Insurance Portability and Accountability Act, and Family Education Rights and Privacy Act requirements.
Eligibility criteria required that the student be diagnosed with asthma and available to engage in all class sessions, and provide verbal and written assent. Exclusion criteria included an indication of unwillingness to participate on the part of the student or lack of written consent from a parent or legal guardian for themselves or for their child. Family caregiver eligibility criteria to serve as a proxy for students included availability to complete the surveys and attend the community program, designation as caregiver of a student with asthma, and ability to understand English. Although the investigators did not seek to gain access to health or school records, school nurses had information about students who were approved to have reliever medication with them at all times.
Effect sizes were not used to determine sample size because estimates of effect sizes were not available prior to this pilot study. Effect sizes of this study were used to estimate power for subsequent studies.
A convenience sampling method was used. Recruitment letters inviting participation in SHARP were sent to caregivers of all sixth grade students (N = 387) in one school district along with brochures, response forms, and prepaid return envelopes. The highly diverse county was ranked among the top in the state for asthma incidence and prevalence. Caregivers and students who expressed interest in learning about the SHARP program and the study were instructed by school nurses to call the team using a toll free number. Two weeks after the recruitment mailing, school nurses telephoned caregivers of students diagnosed with asthma (n = 20) and invited their participation. To form one after school group at the junior high school, nurses contacted caregivers of seventh grade students with asthma (n = 10) and invited participation. Of the 397 students assessed for eligibility, 367 did not meet inclusion criteria and were excluded because they were not diagnosed with asthma and had never experienced asthma symptoms. Of the 30 students who met inclusion criteria, one family declined to participate due to lack of interest, and one family declined due to competing time commitments. Telephone numbers off a milies that agreed to be contacted (n = 28) were provided to the research team.
Appointments were scheduled for study enrollment and data collection at a time and location convenient for the participants and evaluators. At baseline, before any data were collected, pairs of trained evaluators obtained written informed consent from a parent or legal guardian and then obtained written informed as sent from the student. The recruitment period including pre-intervention data collection lasted from November 2005 through January 2006, 1-month post-intervention data were collected from April through May 2006, and 12-month follow-up data were collected from April through May 2007.
The convenience sample consisted of 28 dyads of students with asthma aged 11 to 13 years (M = 11.6, SD = .89) and their family caregivers. Table 1 provides sample demographic and clinical characteristics. Nam-Powers Socioeconomic Index Scores (Nam & Powers, 1983) ranged from 11 to 92 (M = 54.9, SD = 20.2). Severity of Illness Rating Scores (Kieckhefer, 1987) ranged from 4 to 12 (M = 5.75, SD = 1.62).
Table 1.
Sample Demographic and Clinical Characteristics (N = 28)
| Characteristic | Sample | |
|---|---|---|
| n | % | |
| Sex/Gender | ||
| Male | 14 | 50.0 |
| Female | 14 | 50.0 |
| 28 | 100.0 | |
| Grade | ||
| 6th grade | 19 | 67.9 |
| 7th grade | 9 | 32.1 |
| 28 | 100.0 | |
| Race/Ethnic Grouping | ||
| Black/African American | 15 | 53.6 |
| White/Caucasian American | 9 | 32.1 |
| Native American | 1 | 3.6 |
| Bi-racial (Black and White) | 3 | 10.7 |
| 28 | 100.0 | |
| Socioeconomic Index Scores | ||
| Lower | 10 | 35.7 |
| Low Middle | 12 | 42.9 |
| Upper Middle | 5 | 17.8 |
| Upper | 1 | 3.6 |
| 28 | 100.0 | |
| Severity of Asthma Rating | ||
| Mild Intermittent | 6 | 21.4 |
| Mild Persistent | 10 | 35.7 |
| Moderate Persistent | 10 | 35.7 |
| Severe Persistent | 2 | 7.2 |
| 28 | 100.0 | |
Two students withdrew from the study before sessions were delivered. One sixth grade student no longer attended school in the district, and one seventh grade student reported problems from diesel fumes when riding the after school bus. All enrolled students and their caregivers received the SHARP materials regardless of adherence to the intervention protocol. At 1-month post-intervention, two of the 28 families enrolled were unreachable and thus were lost to follow-up. At 12 months post-intervention, three of the 28 families were unreachable and therefore lost to follow-up. Data from 26 students were analyzed for the pre- to 1-month post-intervention comparisons, and from 25 students for the 1- to 12-month post-intervention follow-up. Attrition rate was 10.7%.
SHARP School and Community Components
School Component
Students met once a week for 10 weeks during 50-minute sessions (Kintner & Sikorskii, 2009). The school liaison identified two school nurses to serve as recruiters and two recently-retired, certified school teachers from the target district to serve as interveners. One intervener was designated to deliver the program, and the second intervener was available as a substitute. The substitute intervener delivered one session one time. Sixth grade students met in their schools during instructional hours. Seventh grade students met at school immediately after the last class of the day.
Students used the 100-page SHARP Student Keepsake Workbook (Kintner & Sikorskii, 2009), which was designed to be colorful, entertaining, age- and grade-appropriate, and gender, race, and culturally diverse. Academic activities that integrated biology, psychology, and sociology, complemented existing school curricula. Students were challenged with spelling words (e.g., broncho constriction), mathematical problems (e.g., doses remaining in inhaler medications), and reading and writing assignments (e.g., oral summaries of text). School Component session topics are listed in Table 2. “Students were offered a personal choice to accept responsibility for management of their asthma, and were then provided guidance to reach their goals” (Kintner & Sikorskii, 2009, p. 325). During the first half of the program, students worked on a drawing expressing what it was like to live with asthma, and during the second half students wrote stories about their experiences with asthma. The area asthma coalition invited students enrolled in SHARP to submit their drawings to a local poster contest for World Asthma Day. The posters were displayed at a mall and then were digitally scanned and projected onto the screen at the Cineplex between movies. Stories were posted on the SHARP website.
Table 2.
Session Topics for School and Community SHARP Program Components
| Session | Topics Addressed | Functioning Domain |
|---|---|---|
| 1 | Understanding anatomy and pathophysiology of asthma | Cognitive |
| 2 | Assessing asthma severity and identifying stimuli | Cognitive |
| 3 | Using medications and treatments to prevent and treat symptoms | Cognitive |
| 4 | Discussing activities for managing acute asthma episodes | Behavioral |
| 5 | Exploring how to reduce the risk of having asthma symptoms | Behavioral |
| 6 | Discussing how to stay healthy while living with asthma | Behavioral |
| 7 | Exploring how beliefs about asthma influence management of the condition | Psychosocial |
| 8 | Sharing thoughts and feelings about living with asthma | Psychosocial |
| 9 | Reasoning about what students will do if they have asthma symptoms | Capstone |
| 10 | Describing how asthma will not interfere with participation in life activities | Quality of Life |
Interveners used session-specific checklists to compile materials before delivering each session. The checklists were reviewed before and completed after delivery of each session to assure fidelity to the program. All sessions were digitally audio-recorded. The interveners and a research associate listened to a recording of the first time a session was delivered. Notes taken while listening to the recordings were reviewed and discussed during weekly meetings. Deviation from the protocol was addressed and protocols were refined as needed to strengthen the program.
Community Component
To support SHARP students, members of their social networks participated in a 3-hour information sharing program (Kintner & Sikorskii, 2009). Students personally delivered invitations to all members of their social networks. Social networks for students include parents, siblings, grandparents, aunts, uncles, cousins, friends, teachers, classmates, and club/sports/youth leaders. The program was offered on three different days to accommodate a variety of schedules. Families and invited guests selected the day and time that they could attend. Two of the programs were offered on week days during early evening hours (Tuesday and Thursday, 5:30 p.m. to 8:30 p.m.), and one program was offered on the week end in the morning (Saturday, 9:30 a.m. to 12:30 p.m.).
The program took place in a location designated by the asthma coalition members, specifically the auditorium of the local hospital. As attendees arrived, they were met by asthma coalition members. Tote bags were offered for collecting brochures, pamphlets, pens, pencils, puzzles, games, and coloring books placed on tables with display boards by asthma coalition members. Child care services were provided. Door prizes (e.g., mattress covers) were awarded to students with asthma. Following the program, hot and nutritious boxed meals were served.
During the Community Component, information about asthma was offered, as a didactic presentation with discussion and opportunities for questions, by the SHARP intervener and the chair person of the local asthma coalition. Presentations were directed toward increasing asthma knowledge and logical reasoning abilities for managing acute episodes, use of effective asthma health behaviors, and acceptance of asthma (60 minutes). The program additionally provided an overview of coalition activities in the community (30 minutes). Handouts were provided. Although not controlled for in analysis, following the formal presentation, a physician, two pulmonary nurses, a respiratory the rapist, and a pharmacist were available a tone or more of these programs to meet attendee sin an open health fair atmosphere. Attendees were encouraged to share their experiences with asthma while socially interacting with each other and healthcare professionals.
Measures
Self-report measures were used. When selecting instruments for this program of research, internal consistency reliability, construct validity, readability, and age appropriateness were considered. The Knowledge of Asthma Survey, Asthma Health Behavior Survey, Acceptance of Asthma Questionnaire and Participation in Life Activities scale completed by students, and the General Health History Survey completed by caregivers are fully described in a previous manuscript (Kintner & Sikorskii, 2009). Table 3 contains internal consistency reliability estimates for this sample at baseline or Time 1.
Table 3.
Instruments, Item Numbers, Citations, and Cronbach’s and Kuder-Richardson 20 (K-R 20) Alpha Reliability Coefficients for Surveys Completed by Students and Caregivers
| Instrument | Items | Citation | Completed by | Alpha |
|---|---|---|---|---|
| Knowledge of Asthma Survey | 18 | Kintner, 1996 | Student | K-R 20 = .70 |
| Reasoning about Asthma Scenarios | 4 | Kintner, 2007 | Student | Cronbach’s = .80 |
| Asthma Health Behaviors Survey | Kintner, 2007 | Caregiver | ||
| Episode management behaviors | 6 | Cronbach’s = .73 | ||
| Risk reduction behaviors | 6 | Cronbach’s = .71 | ||
| Acceptance of Asthma Questionnaire | Kintner, 2007 | Student | ||
| Taking control | 6 | Cronbach’s = .65 | ||
| Vigilance | 6 | Cronbach’s = .69 | ||
| Participation in Life Activities | 3 | Kintner, 2008; Kintner & Sikorskii, 2008 | Student | Cronbach’s = .72 |
| Severity of Illness Rating Scheme | 4 | Kieckhefer, 1987 | Caregiver | Cronbach’s = .71 |
| General Health History Survey | 36 | Kintner, 1996 | Caregiver | Not applicable |
SHARP Program Satisfaction Survey
Students also completed a 10-item, 5-point Likert-type scale that measured satisfaction with overall aspects of the SHARP program (e.g. learning activities, meeting locations, and intervener effectiveness). Mean scores were computed.
Reasoning about Asthma Scenarios
Completed by students, this is a process-learning instrument measuring how students use knowledge and experience to make decisions, solve problems, and draw conclusions related to management of their asthma (Kintner, 2007; Kintner & Sikorskii, 2009). Scoring of this instrument was re-conceptualized for this study. The instrument contains four scenarios with seven questions per scenario addressing: symptom recognition, severity classification, stimuli identification, helper selection, medication consideration, management technique usage, and summary of experiential learning. Mean scores were computed for responses to the seven questions on a three-point scale ranging from 0 (less logical reasoning) to 1 (more logical reasoning) and 2 (most logical reasoning). Question scores were then used to compute composite mean scores for each of the four scenarios. A final grand mean score was computed across the four scenarios. Higher scores were reflective of increased logical reasoning ability.
The Severity of Illness Rating Scale (Kieckhefer, 1987) was completed by caregivers. Using a sample of 206 students with asthma similar to that of our current study, scores for the SIRS were correlated (r = .63, p < .001) with the Severity of Chronic Asthma (SCA) scale (Horner, Kieckhefer, & Fouladi, 2006) designed to be consistent with the national guidelines for diagnosis and management of asthma (NIH, 2007).
Data Collection and Analysis
File Maker Pro® (File Maker Pro, 2005) was used by caregivers and students to complete their surveys. Data were electronically entered by participants into an audio-linked data base prepared by the research team for this purpose. Trained evaluators working in pairs used password-protected and encrypted laptop computers to assist with data collection in the homes of students with asthma at three time points: baseline (Time 1), 1 month post-intervention (Time 2), and 12 months post-intervention (Time 3). Evaluators were multi-lingual male and female professionals identified by coalition members. One evaluator was designated to read the consent and assent forms, answer questions, and obtain written consent and assent from caregivers and students. This evaluator also supported the caregiver’s completion of the survey by assisting with computer use and monitoring other children in the home under the supervision of the caregiver. The other evaluator attended to the needs of the student.
To acknowledge participants for the time and effort involved in completing surveys, at each time point, both students and caregivers were offered a cash award of $15. Healthcare professionals who work with low socioeconomic populations understand that certificates and gift cards are not as useful as monetary awards. Store certificates are difficult to redeem when participants live two or more bus transfers from store locations. Participants who lack access to banking services are prevented from cashing checks and exchanging money orders. Although some participants may receive government support for food items, many in this population remain cash poor and have a need to cover daily necessities such as utilities and rent.
Based on ethical principles of respect for person, autonomy, and self-determination, offering a cash gratuity promotes human dignity and independence. Some participants may use the funds for food to feed their family, and others may purchase clothing, medications, school supplies, or pay for transportation to healthcare appointments. Students and caregivers who participated in all three data collection time points were awarded a total of $45 each or $90 per dyad.
Following encryption, data were electronically transferred to the study-dedicated password and firewall protected server. Raw data were processed from the data entry file into SAS 9.1 (SAS, 2002–2003) for analysis. To assess the quality of the data and to evaluate the potential violation of statistical assumptions, descriptive statistics were computed for all variables. Internal consistency reliability for this sample was assessed at Time 1 using Cronbach’s or Kuder-Richardson-20 alpha correlation coefficients. A one sample t-test was used to examine change and stability in target variables from (a) baseline (Time 1) to 1 month post-intervention (Time 2), and (b) 1 month post-intervention (Time 2) to 12 months post-intervention (Time 3).
Results
Feasibility
Students and caregivers demonstrated willingness to fully participate in the intervention
This was evidenced by subject accrual and attendance in both the School and Community components. All sixth grade students (n = 19, 100%) attended each school session offered during school hours; however, one student required one make-up session. Sixty-six percent of the seventh grade students (n = 6) attended all the after school sessions, 33% (n = 3) occasionally forgot, and 11% (n = 1) was unable to attend due to transportation issues. Of the three seventh grade students who occasionally forgot, two students missed two sessions and one student missed three sessions. The students immediately called to report that they had forgot ten to attend the after school program. To address content covered in the missed after school sessions, the intervener reviewed previous content before introducing new material.
The majority of caregivers (n = 19, 67.9%) attended the Community component program, which had total attendance of 74 individuals. Participation in the Community component increased after students were introduced to their stethoscopes during the School component. Taking home a stethoscope from the community program was a strong motivator for students to convince their caregivers to attend.
All caregivers (100%) who attended the community component strongly agreed that they learned something new about asthma, had a better understanding of the SHARP program, learned of new asthma resources in the community, and appreciated the convenient location of the Community component. Caregivers expressed appreciation for being able to socially interact with their students’ physicians, school teachers, nurses, respiratory therapists, and pharmacists during the Community program. Caregivers found the handouts very informative. Examples of caregiver comments included the following: “This program has opened my son’s mind to accept that he has asthma so that he can live with the condition daily throughout his life.” “Thank you for helping my child and me better understand asthma.” “My son’s interest in taking care of his asthma has improved.” “I am really happy that my daughter understands her asthma; the program has helped our family in many ways. Now we know what to look for and how to help.” “The SHARP Community component is a wonderful program = A+.”
Students and caregivers were willing to complete the evaluation instruments
Collecting data in the homes of the student/caregiver dyads at a convenient time in the early evening hours or during weekends was feasible and preferred by families for convenience, childcare, transportation, and time commitments. Three dyads (10.7 %) requested to meet with evaluators at a location other than their homes, in a small conference room at the centrally-located hospital. Students and caregivers reported that they had fun and enjoyed completing the surveys using the audio-linked, data entry systems. Encouraging participants to take a break addressed the potential for response burden. Approximately, 75% of the caregivers completed their five surveys in 25–120 minutes (Mode ≤65), and 75% of the students completed their five surveys in 40–150 minutes (Mode ≤90) with at least one 10-minute break.
Interveners demonstrated ability to deliver each session
This was evidenced by implementation of the program. The interveners were able to deliver 100% of the required components as prescribed for each of the 50-minute sessions. Review of the audio-recordings by the interveners and the research associate, and discussions during the weekly meetings with the PI substantiated the quality of content being delivered. Interveners were able to tailor the curriculum to meet the needs of individual students.
Perceptions of students
All student participants (100%) strongly agreed that they appreciated that their school offered SHARP, and that they were glad they had participated in the program. Over 95% strongly agreed that they had learned something new about asthma, found the SHARP Keepsake Student Workbook to be useful, and had enjoyed sharing their beliefs with other students during the Asthma Beliefs Ungame. Students appreciated practicing potential actions they could take when experiencing breathing problems, expressed confidence in their ability to appropriately respond should breathing problems occur, and reported that by the end of the program they knew what to do during an acute asthma episode. Students enjoyed drawing pictures and writing stories about what it is like to live with asthma. When provided the opportunity to offer suggestions for improving the program, one student emphasized the importance of “educating all students in all grades with and without asthma in their school and throughout the community, and around the world about asthma.”
Perceptions of school personnel
Pressured to demonstrate academic outcomes, school personnel embraced the developmentally age- and grade-appropriate program designed to meet the academic and counseling needs of older school-age students. In a community with high incidence and prevalence of asthma, school personnel were seeking ways to address cognitive, behavioral, psychosocial, and quality of life outcomes of older school-age students with asthma. The director of health and human services for the district served as the school liaison and negotiated entry into the schools with ease. School personnel understood that the academic and counseling program had to be delivered during instructional time. Enrichment periods, which were built into the school day for students to work on academic projects to meet their individual needs, were identified for this purpose. School personnel collaborated in refinement of the program throughout the study. When school principals, office staff, school nurses, and homeroom teachers quizzed students about what they had learned, school personnel were impressed by students’ knowledge gained and engagement in the program.
Perceptions of community partners
Coalition members expressed willingness and readiness to engage in all aspects of the study. Coalition members deemed the purpose of the program to be achievable in improving the health status and meeting the needs of students with asthma. They believed the innovative program was comprehensive, valuable, and meaningful. Coalition members found implementation of the program possible, practical, and worthwhile with realistic potential for long-term health benefits and cost savings.
Perceptions of team members
The area asthma coalition assisted in identifying the pilot program’s medical consultant, project director, and evaluators. The medical consultant reviewed and approved student and community component materials, deemed the material to be accurate and comprehensive, and attended one of the community programs. The project director coordinated all aspects of the study according to written protocols. The project director was confident in her ability to coordinate all activities. Evaluators (e.g., physicians, respiratory therapists, school teachers, and counselors) responsible for in-home data collection expressed that they had gained knowledge and experience by collecting data in settings beyond their usual scope of practice.
Changes in Asthma Knowledge, Behaviors, and Symptoms
Pre- to 1-month post-intervention (Time 1 to Time 2) comparisons of outcomes for this pilot study, adjusted for within-school clustering, are presented in Table 4. Scores for knowledge of asthma, logical reasoning abilities for managing acute episodes of symptom exacerbation, use of effective risk reduction and episode management behaviors, acceptance of asthma as a chronic condition in taking control and vigilance, and participation in life activities demonstrated statistically significant increases (p < .05).
Table 4.
Pre- to 1-month Post-Intervention Comparisons of Outcomes Adjusted for Clustering within School (N =26)
| Pre-Intervention | Post-Intervention | Effect size | df | p-value | |||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Mean | SD | Mean | SD | ||||
| Student Knowledge | 8.14 | 2.52 | 10.63 | 2.25 | 1.04 | 19 | <.01 |
| Reasoning About Asthma | 1.10 | 0.23 | 1.46 | 0.24 | 1.35 | 19 | <.01 |
| Risk Reduction Behaviors | 1.94 | 0.75 | 2.70 | 0.73 | 1.15 | 18 | <.01 |
| Episode Management Behaviors | 1.19 | 0.82 | 1.76 | 1.01 | .29 | 18 | .03 |
| Taking Control | 3.60 | 0.71 | 4.04 | 0.54 | .52 | 19 | .01 |
| Vigilance | 3.41 | 0.61 | 3.71 | 0.62 | .46 | 19 | .03 |
| Participation in Activities | 1.57 | 0.92 | 1.98 | 0.62 | .44 | 19 | .03 |
Stability and change in scores from 1 month to 12 months post-intervention (Time 2 to Time 3) are presented in Table 5. Scores for knowledge of asthma and reasoning about asthma, use of effective episode management behaviors, acceptance of asthma in taking control and vigilance, and participation in life activities remained stable overtime (p > .05). Statistically significant changes were observed indicating improvement in asthma severity (p = .04), despite a decrease in the use of effective risk reduction behaviors (p = .02).
Table 5.
Paired t-test for Stability and Change over Time (N = 25) from 1-month Post-Intervention (Time 2) to 12-months Post-Intervention (Time 3) Follow-up (df = 24)
| Time 2 at 1-month post | Time 3 at 12-month post | t-test | p-value | |||
|---|---|---|---|---|---|---|
|
| ||||||
| Mean | SD | Mean | SD | |||
| Student Knowledge | 10.73 | 2.23 | 10.90 | 2.20 | −.590 | .56 |
| Reasoning about Asthma | 1.46 | .24 | 1.43 | .21 | .823 | .42 |
| Risk Reduction Behaviors | 2.68 | .77 | 2.42 | .79 | 2.662 | .02 |
| Episode Management Behaviors | 1.77 | 1.03 | 1.81 | 1.05 | −.336 | .74 |
| Taking Control | 4.01 | .56 | 3.87 | .59 | 1.379 | .18 |
| Vigilance | 3.71 | .62 | 3.90 | .54 | −1.739 | .10 |
| Severity of Illness Rating | 5.92 | 1.96 | 5.28 | 1.49 | 2.222 | .04 |
| Participation in Activities | 1.99 | .62 | 1.94 | .77 | .389 | .70 |
Discussion
Feasibility and benefits of SHARP were demonstrated as evidenced by willingness of students, caregivers, school personnel, and community partners to fully participate in the program, and by significant improvements in student knowledge, acceptance of the condition, and reasoning abilities concerning their asthma. School personnel were able to identify and recruit students with asthma into the program. Students and members of their social networks attended the school and community components, respectively. Interveners were able to deliver each session of the school and community components while tailoring the intervention to meet individual’s needs. Research team members implemented SHARP according to designed protocols. Students and caregivers completed evaluation instruments. Students reported high levels of satisfaction with the program. Observing students’ knowledge and engagement, school personnel embraced the idea of delivering the academic program during instructional time. Seeking to increase asthma awareness and decrease asthma morbidity, community partners demonstrated commitment to all aspects of the program.
Positive outcomes for knowledge of asthma and reasoning about asthma, use of effective episode management and risk reduction behaviors, acceptance of asthma in taking control and vigilance, and participation in life activities demonstrated moderate to large effect sizes from baseline to 1-month post-intervention indicating clinical significance of the intervention. Improvements in knowledge of asthma, reasoning about asthma, use of effective episode management behaviors, acceptance of asthma in taking control and vigilance, and participation in life activities were sustained over a 12-month period. Although use of effective risk reduction behaviors decreased somewhat overtime, asthma severity improved as hypothesized.
The theory-guided and evidence-based SHARP offers education to improve student knowledge of asthma, reasoning abilities for managing asthma symptoms, and use of effective asthma health behaviors. The program also provides health counseling to improve acceptance of asthma, and ultimately impacts overall quality of life as reflected in participation in life activities. A program similar to SHARP was implemented as a 15-lesson integrated curriculum for the elementary classroom (Pike et al., 2011) using theoretical concepts reflective of this program of research (Kintner & Sikorskii, 2009). Findings of the academic program (Pike et al., 2011) were similar to feasibility and benefits reported for this study. Teachers indicated strong acceptance for the academic program, indicating that they would continue to incorporate the lessons into future teaching. Students demonstrated increases in asthma knowledge.
We acknowledge the inherent limitations of self-report data. In addition, we caution about generalizing findings from this pilot study to larger populations. Evaluating efficacy, effectiveness, and impact of the SHARP program requires larger and more diverse students with asthma, their caregivers, and members of their social networks.
Future research is needed to fully evaluate the SHARP program. A larger and more diverse sample is needed. Efficacy could be demonstrated by using a randomized control design with intervention and usual care or attention control groups. Effectiveness and impact of SHARP over time could be evaluated by using individual and community outcomes, specifically enhanced caregiver and school personnel knowledge of asthma, appropriate use of healthcare services, improved school attendance, and decreased morbidity and mortality rates. Once efficacy, effectiveness, and impact of SHARP are demonstrated, school personnel and community members will have a program with features that will foster acceptance by school personnel and community coalitions.
The National Guidelines for the Diagnosis and Management of Asthma (NIH, 2007) recommended development and evaluation of asthma health education programs for community settings including schools. SHARP was developed to meet the age- and grade-appropriate cognitive, behavioral, and psychosocial aspects of asthma management of older school-age students with asthma. The program also was designed to complement existing school curriculum so that it is more likely to be accepted and adopted by administrators seeking to meet academic outcomes. Findings offer insight into the feasibility of SHARP as well as multiple benefits for adolescents, leading to improved quality of life.
Acknowledgments
This research was funded by a grant from the National Institutes of Health, R21 NR009517 Staying Health —Asthma Responsible and Prepared, National Institute of Nursing Research (Primary); National Heart, Lung, and Blood Institute; National Institute of Allergy and Infectious Diseases; and National Institute of Child Health and Human Development. The authors wish to acknowledge Dr. A. Sikorskii for serving as our statistician as well as members of the Jackson Asthma Coalition and personnel of the Jackson Public School District in Michigan for their assistance and support. We also recognize participants for sharing their experiences by being part of the SHARP program.
Contributor Information
Eileen Kintner, Email: ekintner@mail.nur.utexas.edu, The University of Texas at Austin, School of Nursing, D0100, 1700 Red River Street, NUR 3.446, Austin, TX 78701-1499, Phone: 512-358-4717, FAX: 512-475-8755.
Gwendolyn Cook, The University of Texas at Austin, School of Nursing.
April Allen, Cardio pulmonary Rehabilitation, Allegiance Health, Jackson, MI
Linda Meeder, Michigan Department of Community Health, Lansing, MI.
Janell Bumpus, Jackson Public Schools, Jackson, MI.
Kimberly Lewis, The University of Texas at Austin, School of Nursing.
References
- Akinbami LJ. Asthma prevalence, health care use and mortality: United States, 2003–2005. Center for Disease Control and Prevention; 2007. Retrieved from http://www.cdc.gov/nchs/products/pubs/pubd/hestats/ashtma03-05/asthma03-05.htm. [Google Scholar]
- Akinbami LJ, Moorman JE, Liu X. Asthma prevalence, health care use, and mortality: United States, 2005–2009. National Health Statistics Reports. 2011;32:1–14. [PubMed] [Google Scholar]
- Clark NM, Brown R, Joseph CL, Anderson EW, Liu M, Valerio MA. Effects of a comprehensive school-based asthma program on symptoms, parent management, grades, and absenteeism. Chest. 2004;125:1674–1679. doi: 10.1378/chest.125.5.1674. [DOI] [PubMed] [Google Scholar]
- FileMaker Pro. FileMaker Pro Developer 7. Santa Clara, CA: FileMaker, Inc; 2005. [Google Scholar]
- Hallstrand TS, Curtis JR, Aitken ML, Sullivan SD. Quality of life in adolescents with mild asthma. Pediatric Pulmonology. 2003;36:536–543. doi: 10.1002/ppul.10395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horner SD, Fouladi RT. Improvement of rural children’s asthma self-management by lay health educators. The Journal of School Health. 2008;78:506–513. doi: 10.1111/j.1746-1561.2008.00336.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horner SD, Kieckhefer GM, Fouladi RT. Measuring asthma severity: Instrument refinement. Journal of Asthma. 2006;43:533–538. doi: 10.1080/02770900600857192. [DOI] [PubMed] [Google Scholar]
- Kieckhefer GM. Testing self-perception of health theory to predict health promotion and illness management behavior in children with asthma. Journal of Pediatric Nursing. 1987;2:381–391. [PubMed] [Google Scholar]
- Kieckhefer GM, Trahms CM. Supporting development of children with chronic conditions: from compliance toward shared management. Pediatric Nursing. 2000;26:354–363. [PubMed] [Google Scholar]
- Kintner EK. Doctoral Dissertation. The University of Arizona; Tucson, AZ: 1996. Testing of the School-aged Child and Adolescent Acceptance of Asthma Model. [Google Scholar]
- Kintner EK. Adolescent process of coming to accept asthma: A phenomenological study. Journal of Asthma. 1997;34:547–561. doi: 10.3109/02770909709055399. [DOI] [PubMed] [Google Scholar]
- Kintner EK. Lack of relationship between acceptance and knowledge of asthma in school-age children and early adolescents. Journal for Specialists in Pediatric Nursing: JSPN. 2004;9:5–14. doi: 10.1111/j.1088-145x.2004.00005.x. [DOI] [PubMed] [Google Scholar]
- Kintner EK. Testing the Acceptance of Asthma Model with children and adolescents. Western Journal of Nursing Research. 2007;29:410–431. doi: 10.1177/0193945907299657. [DOI] [PubMed] [Google Scholar]
- Kintner EK. Development and preliminary evaluation of the Participation in Life Activities scale for children and adolescents with asthma: An instrument development study. Health & Quality of Life Outcomes. 2008;6:1–11. doi: 10.1186/1477-7525-6-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kintner EK, Sikorskii A. Reliability and construct validity of the Participation in Life Activities scale for children and adolescents with asthma: An instrument evaluation study. Health and Quality of Life Outcomes. 2008;6:1–10. doi: 10.1186/1477-7525-6-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kintner EK, Sikorskii A. Randomized clinical trial of a school-based academic and counseling program for older school-age students. Nursing Research. 2009;58:321–331. doi: 10.1097/NNR.0b013e3181b4b60e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kjellman B, Gustafsson PM. Asthma from childhood to adulthood: Asthma severity, allergies, sensitization, living conditions, gender influence and social consequences. Respiratory Medicine. 2000;94:454–465. doi: 10.1053/rmed.1999.0764. [DOI] [PubMed] [Google Scholar]
- Lerner RM. Concepts and theories of human development. 2. New York, NY: McGraw-Hill; 1986. [Google Scholar]
- Magzamen S, Patel B, Davis A, Edelstein J, Tager IB. Kickin’ Asthma: School-based asthma education in an urban community. The Journal of School Health. 2008;78:655–665. doi: 10.1111/j.1746-1561.2008.00362.x. [DOI] [PubMed] [Google Scholar]
- Nam CB, Powers MG. The socioeconomic approach to status measurement. Houston, TX: Cap & Gown Press; 1983. [Google Scholar]
- National Institutes of Health [NIH] National Institutes of Health, National Heart, Lung, and Blood Institute Expert Panel Report 3: Guidelines for diagnosis and management of asthma. U.S. Department of Health and Human Services; 2007. Retrieved from http://www.nhlbi.nih.gov/guidelines/asthma/asthgdln.htm. [Google Scholar]
- Pike EV, Richmond CM, Hobson A, Kleiss J, Wottowa J, Sterling DA. Development and evaluation of an integrated asthma awareness curriculum for the elementary school classroom. Journal of Urban Health: Bulletin of the New York Academy of Medicine. 2011;88(Suppl 1):61–67. doi: 10.1007/s11524-010-9477-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasmussen F, Taylor DR, Flannery EM, Cowan JO, Greene JM, Herbison GP, Sears MR. Risk factors for hospital admission for asthma from childhood to young adulthood: A longitudinal population study. Journal of Allergy & Clinical Immunology. 2002;110:220–227. doi: 10.1067/mai.2002.125295. [DOI] [PubMed] [Google Scholar]
- Riccioni G, D’Orazio N, Di Ilio C, Della Vecchia R, Ballone E, Menna V, Guagnano MT. Bronchial hyper responsiveness and quality of life in asthmatics. Respiration. 2003;70:496–499. doi: 10.1159/000074206. [DOI] [PubMed] [Google Scholar]
- Santrock JW. Adolescence. 13. Boston, MA: McGraw-Hill; 2010. [Google Scholar]
- SAS. SAS® Software Version 9 of the SAS System for Windows (Version 9.3.1) Cary, NC: SAS Institute, Inc; 2002–2003. [Google Scholar]
- Strunk RC, Sternberg AL, Bacharier LB, Szefler SJ. Nocturnal awakening caused by asthma in children with mild-to-moderate asthma in the childhood asthma management program. Journal of Allergy & Clinical Immunology. 2002;110:395–403. doi: 10.1067/mai.2002.127433. [DOI] [PubMed] [Google Scholar]
- Sugarman L. Life-span development concepts, theories, and interventions. New York, NY: Routledge; 1986. [Google Scholar]
- U.S. Department of Education. No Child Left Behind. 2002 Retrieved 1/2/2007, from http://www.ed.gov/nclb/landing.jhtml.
- Velsor-Friedrich B, Pigott T, Srof B. A practitioner-based asthma intervention program with African American inner-city school children. Journal of Pediatric Health Care. 2005;19:163–171. doi: 10.1016/j.pedhc.2004.12.002. [DOI] [PubMed] [Google Scholar]